Abstract
Background:
National AIDS Control Organization guidelines on enhanced syndromic case management of sexually transmitted infections (STIs) and reproductive tract infections (RTIs) require per speculum (P/S) and per vaginal (P/V) examinations for diagnosis of STIs. However, it is not known if the addition of P/S and P/V examinations to self-reported symptomatic assessment adds any value for the diagnosis of STI/RTI.
Objective:
To assess the diagnostic accuracy of P/S and P/V examinations compared with self-reported symptomatic assessment in a cohort of female sex workers (FSWs).
Methods:
We performed a cross-sectional study from August 2009 to June 2010, among 519 FSWs in Surat city, Gujarat, India. Symptomatic assessment for the presence or absence of vaginal/cervical discharge (VCD) or lower abdominal pain (LAP) was done using a self-administered questionnaire. After completion of the questionnaire, all participants underwent P/S and P/V examinations. Summary diagnostic accuracy measures were calculated.
Results:
Five hundred and nineteen FSWs between the ages of 18–49 years participated in the study. The median age of participants was 31 years. The prevalence of VCD and LAP syndromes based on vaginal discharge, LAP, or both was 56%, 5,–10%, respectively. The sensitivity of P/S and P/V examinations depending on symptomatic assessment ranged from 47% to 76%. The specificity ranged from 73% to 93%. The positive predictive value ranged from 25% to 83%, and the negative predictive value ranged from 56% to 98%.
Conclusion:
Symptomatic assessment alone is not adequate for the diagnosis of VCD and LAP syndromes and can lead to a significant number of missed cases (36%). A P/S and P/V examinations is critical for assessment of VCD and LAP syndromes and subsequent treatment.
Keywords: Diagnostic accuracy, lower abdominal pain, reproductive tract infections, sexually transmitted infections, vaginal discharge
INTRODUCTION
In 2008, the National AIDS Control Organization (NACO) in India introduced guidelines on enhanced syndromic case management of sexually transmitted infections (STIs)/reproductive tract infections (RTIs).[1] The NACO guidelines recommend per speculum (P/S) and per vaginal (P/V) examinations for diagnosis of STIs in subjects who are at high risk for STIs, which includes female sex workers (FSWs).[2] Before the introduction of enhanced NACO guidelines, the diagnosis of STI/RTI for FSWs was based on only symptomatic assessment at field level STI clinic as per targeted intervention guidelines, which included asking patients about the presence or absence of vaginal discharge and lower abdominal pain (LAP).[3] However, it is not known if the addition of P/S and P/V examinations to symptomatic assessment of high-risk patients suspected of STI/RTI adds any diagnostic value. Therefore, we performed a cross-sectional analytic study to assess the diagnostic accuracy of P/S and P/V over symptomatic assessment in a cohort of FSWs.
METHODS
Participants
Any FSWs between the ages of 18–49 years were eligible for inclusion in the study. FSWs menstruating at the time of study and with a history of prior hysterectomy were excluded. All consecutive FSWs who attended the field level STI clinic in Surat city, Gujarat, India, for routine medical checkup were asked to participate in the study. All participants who agreed to participate were asked to give signed informed consent. The study was approved by the local Institutional Review Board.
Test methods
For symptomatic assessment, all enrolled participants completed a semi-structured, pretested questionnaire that included questions related to the presence or absence of vaginal discharge or/and LAP. The following definitions specified by the NACO guidelines for these symptoms were used: Vaginal/cervical discharge (VCD) - symptomatic vaginal discharge or asymptomatic vaginal discharge seen on examination and cervical discharge seen on speculum examination. LAP-LAP with tenderness, or cervical motion tenderness.
Any participant with complaints of LAP underwent per abdominal examination. All participants also underwent P/S and P/V examinations. The administration of the questionnaire, physical examination, per abdominal examination, and the P/S and P/V examinations were performed by trained clinicians. After the questionnaire, abdominal examination (where applicable) and P/S and P/V examinations were completed, the physician recorded his/her assessment of whether the participants did or did not have an STI/RTI. The clinician performing the P/S and P/V examinations or per abdominal examination were not blinded to the results of the questionnaire.
Reference standard
We used the following a priori developed rules to categorize participants as being true/false positive or negative for VCD and LAP syndromes. True positive for VCD and LAP syndromes. positive on questionnaire, and positive on P/S and P/V or per abdominal examination (where applicable). True negative for VCD and LAP syndromes: Negative on questionnaire, and negative on P/S and P/V or per abdominal examination (where applicable). If a participant was positive for VCD and LAP syndromes on the questionnaire and negative on P/S and P/V examinations or per abdominal examination, the result was categorized as false positive. Likewise, if the participant was negative for VCD and LAP syndromes on the questionnaire and positive on P/S and P/V examinations or per abdominal examination, the result was considered false negative. However, the clinician performing the P/S and P/V examinations or per abdominal examination were not blinded to the findings of symptomatic assessment as the clinician single-handedly collected history and performed a clinical examination.
Statistical methods
Diagnostic accuracy measures of sensitivity, specificity, positive predictive value, negative predictive value, and positive and negative likelihood ratios along with 95% confidence intervals (95% CIs) were calculated. All statistical analysis was performed using MedCalc statistical analysis software, Version 16.2 developed by Microsoft Partner, Silver Application Development.[4] The study was performed and reported as per the Standards for Reporting of Diagnostic Accuracy guidelines.[5]
RESULTS
Participant characteristics
Five hundred and nineteen FSWs between the ages of 18–49 years participated in the study and were included the final analysis. The study was performed from August 2009 to June 2010. The median age of participants was 31 years (range 18–49 years). The median age of participants presenting with self-reported STI/RTI symptoms on the questionnaire was 32.5 years (range 18–45 years) compared 31 years (range 18–49 years) in the group presenting without symptoms on the questionnaire. Of the 519 patients, 32% (166/519) reported vaginal discharge and 68% (353/519) reported no vaginal discharge on the self-reported questionnaire. The prevalence of VCD and LAP syndromes as determined by P/V and P/S examinations was 81.9% (136/166) in the group who reported vaginal discharge and 43.9% (155/353) in the group who reported no vaginal discharge.
Test results
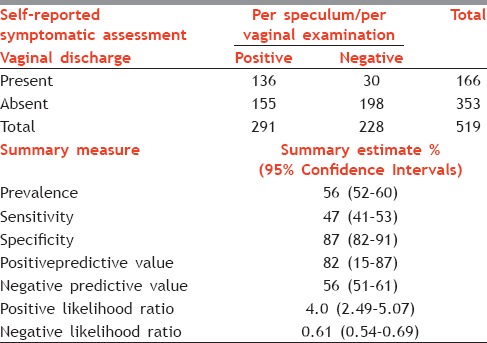
Symptom: Vaginal discharge on self-reported questionnaire
As illustrated in Table 1, the prevalence of VCD based on self-reported vaginal discharge was 56% (95% CI: 52–60%). The sensitivity of P/S and P/V examinations was 47% (95% CI: 41–53%) and specificity was 87% (95% CI: 82–91%). The positive predictive value for P/S and P/V examinations was 82% (95% CI: 15–87%), and negative predictive value was 56% (95% CI: 51–61%). The positive likelihood ratio was 4.0 (95% CI: 2.49–5.07), and the negative likelihood ratio was 0.61 (95% CI: 0.54–0.69).
Table 1.
Test performance characteristics using per speculum/per vaginal examination among female sex workers with self-reported vaginal discharge
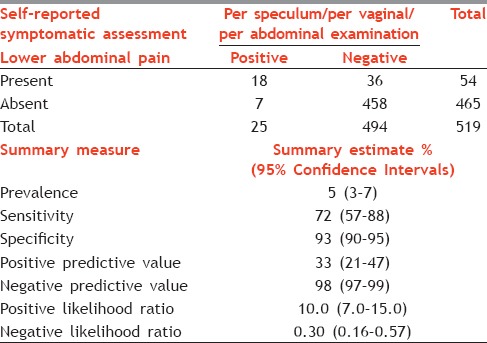
Symptom: Lower abdominal pain on self-reported questionnaire
As shown in Table 2, the prevalence of LAP based on self-reported LAP was 5% (95% CI: 3–7%). The sensitivity of the P/S and P/V examinations was 72% (95% CI: 57–88%) and the specificity was 93% (95% CI: 90–95%). The positive predictive value was 33% (95% CI: 21–47%) and negative predictive value was 98% (95% CI: 97–99%). The positive likelihood ratio was 10.0 (95% CI: 7.0–15.0), and negative likelihood ratio was 0.30 (95% CI: 0.16–0.57).
Table 2.
Test performance characteristics using per speculum/per vaginal/per abdominal examination among female sex workers with self-reported lower abdominal pain
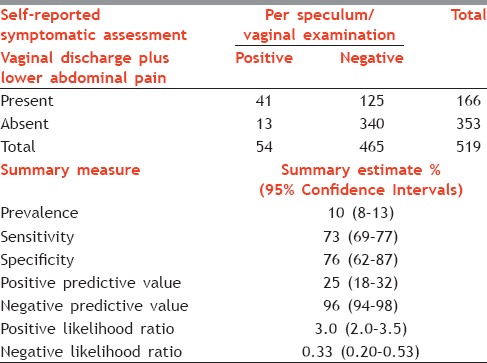
Symptom: Vaginal discharge and abdominal pain on self-reported questionnaire
As shown in Table 3, the prevalence of VCD and LAP syndromes based on symptom of vaginal discharge plus LAP on self-reported questionnaire was 8% (95% CI: 8–13%). The sensitivity of P/S and P/V examinations was 76% (95% CI: 62–87%) and the specificity was 73% (95% CI: 69–77%). The positive predictive value was 25% (95% CI: 18–32%) and negative predictive value was 96% (95% CI: 94–98%). The positive likelihood ratio was 3.0 (95% CI: 2.0–3.5), and negative likelihood ratio was 0.33 (95% CI: 0.2–0.53).
Table 3.
Test performance characteristics using per speculum/per vaginal/per abdominal examination among female sex workers with self-reported vaginal discharge plus lower abdominal pain
DISCUSSION
The results from this cross-sectional analytic study show that the PS/PV examination is helpful to rule in the diagnosis of VCD syndrome in patients who present with vaginal discharge as indicated by high specificity (87%). The sensitivity of the PS/PV examination was low (47%) which indicates that PS/PV may not be of value in ruling out the diagnosis of VCD syndrome. However, given the high prevalence of vaginal discharge, the PS/PV examination may be useful in establishing a diagnosis of VCD syndrome as indicated by high positive predictive value (82%). The findings also show that diagnosis of VCD syndrome based on symptomatic assessment of vaginal discharge alone may lead to over diagnosis with a false positive rate of 34%. However, the rate of underdiagnosis was low with a false negative rate of 6%.
Furthermore, the P/S and P/V examinations are also useful for ruling in as well as ruling out the diagnosis of LAP syndrome in subjects who present with LAP as indicated by high sensitivity (72%) and specificity (93%). However, given the low prevalence of LAP in our cohort, the positive predictive value (33%) was lower than the negative predictive value (98%). Nevertheless, the P/S and P/V examinations should be recommended in high-risk subjects presenting with abdominal pain as the likelihood ratio was very strong (>10). In addition, use of abdominal pain for symptomatic assessment resulted in a very low incidence of false positive (1%) and negative rates (7%) of LAP syndrome.
There have been other studies assessing the value of P/S and P/V examinations following the symptomatic assessment.[6,7,8,9] However, these studies mostly involved reference standard of laboratory-based confirmation.[6,7,8,9] Therefore, the results from other studies are not entirely comparable to ours. Nevertheless, all these studies concluded that P/S and P/V examinations does increase the posttest probability for diagnosing STI/RTI compared with symptomatic assessment alone.[6,7,8,9]
The findings from this study have several practical applications. For example, the objective of the STI/RTI examination is to accurately identify individuals who have asymptomatic or unrecognized STIs that are associated with serious morbidities and to initiate early treatment. Screening asymptomatic individuals (especially women) who are at high risk for STI/RTI such as FSWs is critical for limiting the transmission of STI/RTI. Routine medical screening for STI/RTI using the PS/PV examination will assist in early diagnosis of STI/RTI and may provide opportunities for early treatment and reduce overtreatment, thereby significantly reducing mortality and morbidity.
There are some limitations in this study. First, the clinicians performing the P/S and P/V examinations were not blind to the questionnaire results and therefore may have been biased in their evaluation. Second, due to lack of resources, we were not able to confirm the presence or absence of STI/RTI using objective laboratory methods. However, we used predefined rules for establishment of STI/RTI using the P/S and P/V examinations and therefore the findings reflect the real-world scenario of a resource-limited setting where laboratory confirmation of STI/RTI is not always possible.
In summary, these findings suggest that diagnosing STI/RTI by P/S and P/V examinations is more specific than diagnosing based on self-reported symptoms. In this resource-limited setting, the P/S and P/V examinations were superior to solely relying on patients' complaints of vaginal discharge (PPV of vaginal discharge by P/S examination: 81% and NPV of vaginal discharge by P/S examination: 56%). Potentially, 30% of the VCD cases may be missed if the providers rely solely on the patients' narrative of vaginal discharge symptoms. Similarly, to establish a clinical diagnosis of LAP syndrome based on LAP in a resource-limited setting, a comprehensive examination strategy that includes a thorough per abdominal physical examination in addition to P/S and P/V appears to be superior to solely relying on per abdominal examination.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Acknowledgments
Authors acknowledge the resources and support received from the Fogarty International Grant/USNIH: Grant # 1D43TW006793-01A2-AITRP.
We are thankful to team members of PARAS - PSM NACP III, Sahyog Mahila Mandal, and Ekta Mahila Mandal for all their assistance throughout the research study.
REFERENCES
- 1.National Guidelines on Prevention, Management and Control of Reproductive Tract Infections including Sexually Transmitted Infections. New Delhi: National Institute for Research in Reproductive Health (Indian Council of Medical Research) Ministry of Health and Family Welfare, Government of India, editors; 2007. pp. 4–5. [Google Scholar]
- 2.National Behavioural Surveillance Survey (BSS) New Delhi: National AIDS Control Organization MoHaFW, Government of India; 2006. Female sex workers (FSWs) and their clients. [Google Scholar]
- 3.Guidelines on STI/RTI service delivery for high risk groups and bridge popultaion in TI NGOs, NACO STI TEAM; National AIDS Control Organization MoHaFW, Government of India. 2010 Apr;:2. [Google Scholar]
- 4.MedCalc for Windows [computer program]. Version 12.5. Ostend, Belgium: MedCalc Software; [Last modified: February 4, 2016]. Available from: https://www.medcalc.org . [Google Scholar]
- 5.Bossuyt PM, Reitsma JB, Bruns DE, et al. Towards complete and accurate reporting of studies of diagnostic accuracy: The STARD initiative. BMJ: British Medical Journal. 2003;326(7379):41–44. doi: 10.1136/bmj.326.7379.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cornier N, Petrova E, Cavailler P, Dentcheva R, Terris-Prestholt F, Janin A, et al. Optimising the management of vaginal discharge syndrome in Bulgaria: Cost effectiveness of four clinical algorithms with risk assessment. Sex Transm Infect. 2010;86:303–9. doi: 10.1136/sti.2009.040832. [DOI] [PubMed] [Google Scholar]
- 7.Goyal M, Hayes K, Mollen C. Sexually transmitted infection prevalence in symptomatic adolescent emergency department patients. Pediatr Emerg Care. 2012;28:1277–80. doi: 10.1097/PEC.0b013e3182767d7c. [DOI] [PubMed] [Google Scholar]
- 8.Msuya SE, Mbizvo EM, Stray-Pedersen B, Sundby J, Sam NE, Hussain A. Risk assessment at the primary health care level in Moshi, Tanzania: Limits in predicting sexually transmitted infections among women. Cent Afr J Med. 2006;52:97–104. doi: 10.4314/cajm.v52i9-12.62593. [DOI] [PubMed] [Google Scholar]
- 9.Vishwanath S, Talwar V, Prasad R, Coyaji K, Elias CJ, de Zoysa I. Syndromic management of vaginal discharge among women in a reproductive health clinic in India. Sex Transm Infect. 2000;76:303–6. doi: 10.1136/sti.76.4.303. [DOI] [PMC free article] [PubMed] [Google Scholar]


