Abstract
Context:
Prevention with a positive approach has been advocated as one of the main strategies to diminish the new instances of HIV and the target are those who are engaged in high-risk sexual behavior. Therefore, understanding the risky behaviors of the HIV-infected individual is important.
Aims:
This study aimed to assess the prevalence and the predictors of high-risk sexual behavior among people living with HIV/AIDS (PLHA).
Settings and Design:
A hospital-based cross-sectional study was conducted at antiretroviral therapy centers of two tertiary care hospitals in Lucknow.
Materials and Methods:
A total of 322 HIV-positive patients were interviewed about their sexual behaviors during last 3 months using a pretested questionnaire.
Statistical Analysis Used:
Probability (p) was calculated to test for statistical significance at 5% level of significance. Association between risk factors and high-risk sexual behavior was determined using bivariate analysis followed by multivariate logistic regression.
Results:
Prevalence of high-risk sexual behavior was 24.5%. Of these patients, multiple sexual partners were reported by 67.3% whereas about 46.9% were engaged in unprotected sex. Multivariate logistic regression analysis revealed that high-risk sexual behavior was significantly associated with nonsupporting attitude of spouse (odds ratio [OR]: 18; 95% confidence interval [CI]: 1.4–225.5; P = 0.02) and alcohol consumption (OR: 9.3; 95% CI: 2.4–35.4; P = 0.001).
Conclusions:
Specific intervention addressing alcohol consumption and encouragement of spouse and family support should be integrated in the routine HIV/AIDS care and treatment apart from HIV transmission and prevention knowledge.
Keywords: HIV/AIDS, people living with HIV/AIDS, sexual behavior, spouse support, Uttar Pradesh
INTRODUCTION
Since the beginning of the epidemic, almost 78 million people have been infected with HIV virus and about 39 million people have died of HIV. Globally, 35.0 million (33.2–37.2 million) people were living with HIV at the end of 2013.[1] The Government of India estimates that about 2.40 million Indians are living with HIV (1.93–3.04 million) with an adult prevalence of 0.27% (2011).[2] Antiretroviral therapy (ART) along with sustainable prevention interventions (such as condom provision and health promotion including counseling services) is provided under National AIDS Control Programme. Recent evidence indicates a significant increase in the number of sexual partners in some countries among HIV positives as well as a decline in condom use.[3] This risky sexual behavior among HIV-positive individuals remains the most effective driver of the HIV epidemic. Sexual behavior among people receiving ART is a major public health concern not only because of risks of HIV transmission but also the potential risk of transmission of resistant strains.[3]
HIV prevention strategies have been criticized in the past for focusing too much on HIV-negative people and failing to utilize the ways in which people living with HIV/AIDS (PLHA) could contribute to HIV prevention.[4] This has recently called for the prevention with a positive approach of HIV transmission. Positive prevention approach focuses on the notion that appropriate treatment reduces viral load and hence reduces transmission probability.[5] Positive prevention is not only about stopping the forward transmission of HIV but also involves behavior change among HIV positives and confidence to make decisions to take care of their health and reduce possible harm to their sexual partners.[4] Although several surveys[6] have examined the magnitude of risky sexual behaviors among general population but limited studies are available in the context of high-risk sexual behavior among PLHA. Understanding the magnitude and predictors of such high-risk sexual behavior remains a priority as this information will inform efforts to include prevention with positive messages in the routine HIV/AIDS care and treatment. Therefore, this study intends to describe the prevalence and predictors of high-risk sexual behaviors of PLHA attending ART centers at two tertiary care hospitals of Lucknow.
MATERIALS AND METHODS
Study design
The present study is a hospital-based cross-sectional study.
Study settings
The study was conducted at the ART center of King George's Medical University and Ram Manohar Lohia Institute of Medical Sciences, two tertiary care hospitals in Uttar Pradesh, India. Both these centers provide ART free of charge and have the relevant resources for CD4 count estimation, counseling sessions (adherence to treatment, healthy sexual behavior, condom use, etc.) and regular checkups.
Study participants
All PLHA patients from this center aged ≥ 18 years, and who have been receiving ART for at least 6 months were included in the study.
Sample selection
During the study period, data were collected on 3 (alternate) days every week. Days of data collection were varied in consecutive weeks to reduce the bias for day-specific outpatient department attendance. Every sixth patient from the registration on that day was interviewed, if the patient was not eligible for this study next consecutive patient was interviewed in private. A total of 322 patients were included in the study. Nonwilling patients, patients who were unable to communicate, and seriously ill patients were excluded from the study.
Ethical clearance
This study was approved by the Ethics Committee of King George's Medical University. Patients were first briefed about the purpose of the study and assured regarding the confidentiality of the data given. After written consent was obtained from the participants, they were interviewed.
Data collection tool
Patients were interviewed with the help of a predesigned and pretested schedule. Data on sociodemographic characteristics, sexual behaviors, adherence to treatment, psychosocial factors such as family support and perceived health status were collected from all participants.
Assessment of depression
Becks Depression Inventory[7] (Hindi) was used to assess depression in patients. The Beck Depression Inventory is a 21-item, self-report rating inventory that measures characteristic attitudes and symptoms of depression.[7] Higher scores on the scale indicated a greater number of depressive symptoms or a greater probability of major depressive disorder. The score ranges from 0 to 63. For the purpose of analysis, the score was dichotomized, with ≥ 17 being indicative of depression.
Assessment of nonadherence to ART
Adherence percentage (A) was assessed using pill count method. A = (Number of tablets or doses actually taken by a patient for a particular time period) ÷ (Number of tablets or doses the patient should have taken during this time period). All patients with poor adherence percentage < 95% of treatment adherence were denoted as “nonadherent.”[8]
High-risk sexual behavior
High-risk sexual behavior in the present study is defined as having multiple sexual partners or unprotected sex within last 3 months.
Duration of treatment
Duration of treatment means the time since the patient was on ART.
Spousal support
Spousal support means the spouse resides with their HIV-positive partner and encourages getting and staying on ART.
Data management
Data were compiled and analyzed using the statistical software. The association between different variables in relation to high-risk sexual behavior was determined using Pearson's Chi-square test; Yates-corrected Chi-square and Fisher's exact test were applied in appropriate cases. Independent variables that were found to be statistically significant in bivariate analysis were considered for application in the logistic regression model to determine the important predictors of high-risk sexual behavior, with high-risk sexual behavior as the dependent variable. A P ≤ 0.05 was considered statistically significant.
RESULTS
Biosocial characteristics of PLHA
In total, 322 PLHA on ART were interviewed. None of the patients falling in sampling refused to participate in study. Among them, 201 (62.4%) were males. The mean age of respondents was 38.3 ± 9.3 (range: 18–67 years). The majority of patients were more than 35 years old (55.3%), about 63.4% were married, and 60.9% were having at least senior secondary level of education (60.9%). Among 204 married patients, about two-third (66.7%) patient's spouse were sero-discordant [Table 1].
Table 1.
Bio-social profile of the patients attending ART center
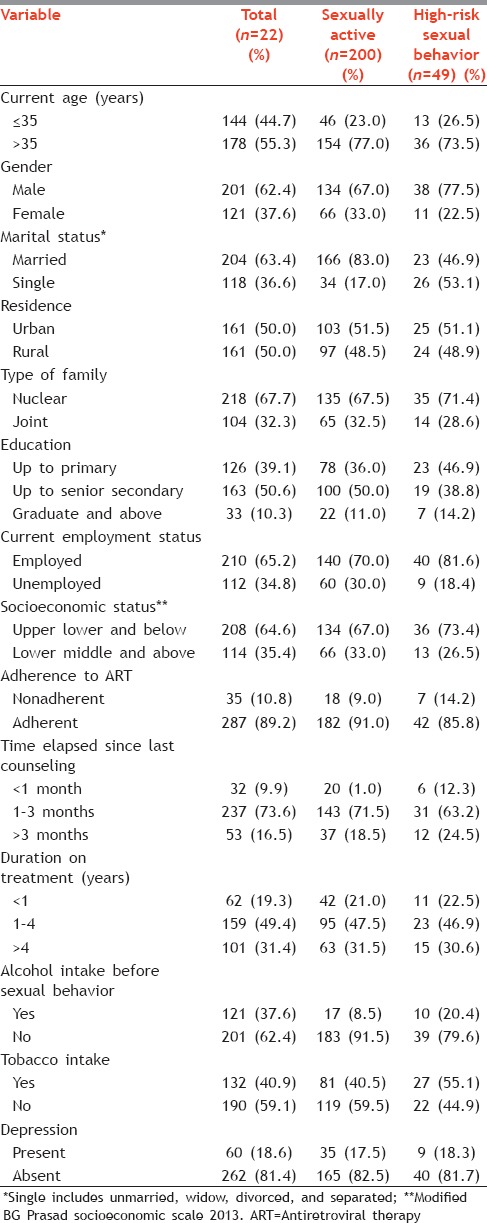
Biosocial characteristics of sexually active PLHA
With regards to sexual behavior, 200 (62.1%) PLHA surveyed were sexually active during last 3 months. Majority (71.7%) of the patients with age less than 35 years were engaged in high-risk sexual activities. High-risk sexual behavior was more among female as compared to males. Among 166 sexually active married patients, about one-fifth (19.8%) patient's spouse were sero-discordant. Although only one patient with spouse sero-discordant status showed high-risk sexual behavior.
Sexual behavior of sexually active PLHA
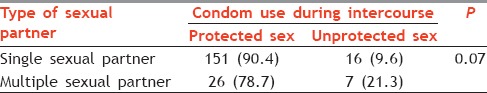
High-risk sexual behavior was reported in 49 (24.5%) patients among 200 sexually active patients [Table 1]. Although the proportion of noncondom users was high among the PLHA having multiple sexual partners, but the association was found to be statistically insignificant. Almost all (98.0%) noncondom users had unprotected sex with a partner of negative or unknown HIV status [Table 2].
Table 2.
Condom use and type of sexual partner in study participants during last 3 months (n=200)
Determinants of high-risk sexual behavior
Table 3 describes the univariate and multivariate logistic regression of the factors related to high-risk sexual behavior among sociodemographic factors, on univariate analysis marital status (P = 0.00), current employment status (P = 0.04), spouse support (P = 0.00), alcohol intake (P = 0.01), and tobacco consumption (P = 0.01) were significantly associated with high-risk sexual behavior. About 38.3% of the nonadherent patient showed risky sexual behavior.
Table 3.
Univariate and multivariate analysis of factors associated with high-risk sexual behavior
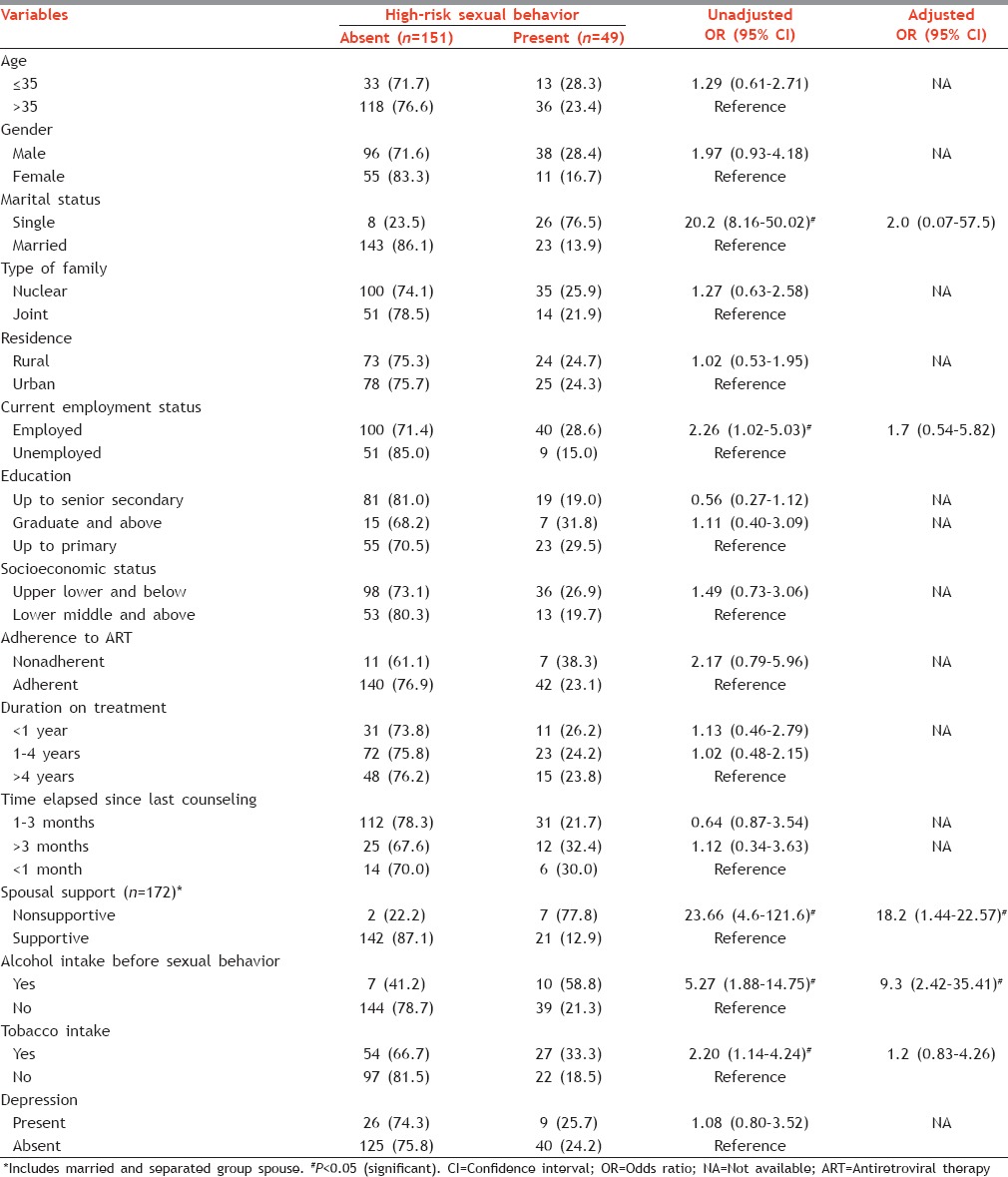
On multivariate analysis, nonsupporting attitude of spouse was significantly associated with high risk (odds ratio [OR]: 18; 95% confidence interval [CI]: 1.4–225.5; P = 0.02). Patients who did not have spouse support were 18 times more likely to be engaged in high-risk sexual activities. Furthermore, high-risk sexual behavior was 9 times more among patients addicted to alcohol as compared to nonalcoholics (OR: 9.3; 95% CI: 2.4–35.4; P = 0.001). Marital status, current employment status, and tobacco intake were found nonsignificant during multivariate analysis.
DISCUSSION
Currently, limited studies are available in Indian context related to the high-risk sexual behavior of PLHA. This study therefore aimed to explore the prevalence and determinants of high-risk sexual behavior among the HIV patients on ART attending ART centre.
In our study, 62.1% of the PLHA on ART were sexually active. This proportion is lower as reported by Yaya et al.[9] in Togo (74.6%), but higher than those reported by Bajunirwe et al.[10] in Uganda (51.4%). Furthermore, of the 200 PLHA, who were sexually active, nearly one-fourth (24.5%) had risky sexual behavior. Almost all (98.0%) noncondom users had unprotected sex with a partner of negative or unknown HIV status. Our finding showed a high prevalence of risky sexual behavior similar to studies[11,12,13,14,15] in other developing countries. This poses a risk of spread of HIV infection in the general population.
Similar to Saha et al.,[16] we found no significant association between adherence to ART and high-risk sexual behavior among PLHA. However, studies[9,17] in African countries showed significant association between nonadherence to ART and high-risk sexual behavior. The reported ART initiation actually promoted safe sexual behavior among PLHA.
Berhan and Berhan[17] found relaxation in the observance of preventive behavior overtime by PLHA on ART. They reported increased risk of sexual behavior with duration of ART. Contrary to this, our study showed no significant association between duration of ART and high-risk sexual behavior.
In the present study, alcohol consumption by the person was found to be significantly associated with their high-risk sexual behavior. A similar finding was also reported in a meta-analysis by Shuper et al.[18] in HIV positives. In India, researchers[19,20] reported a significant association between alcohol consumption and occurrence of unprotected sex and involvement of multiple sexual partner in studies conducted among the general population and persons having sexually transmitted infection. The relationship between alcohol consumption and high-risk sexual behavior can be explained by the rationale that alcohol consumption impairs person judgment skills and modesty which may be responsible for their risky sexual behavior.
The UNFPA states that psychological support provided by family members, especially spouse to PLHA, could be an opportunity for prevention of further HIV infection and transmission.[21]
Mhalu et al.[6] opined that spousal support plays a significant role in reducing behavior for multiple sexual partner and secondary abstinence following HIV diagnosis. Similarly, this study also showed that PLHAs, who had spousal support, significantly had lower high-risk sexual behavior. This shows there is a need to take intervention measures to enhance spousal support to PLHAs. A study by Jones et al.[22] had illustrated the positive effect of group cognitive behavior intervention strategy to change inconsistent condom use to consistent use and also the enhancement in self-efficacy and improvement in communication among high-risk sex couples in India.
Limitations
The findings of this study must be interpreted in light of its limitations. The study was conducted at only two sites in the country among the patients on ART; the findings may not be generalizable to other clinical settings. Furthermore, since the study conducted was cross-sectional, causal inferences cannot be made. Second, issues like alcohol use and sexual behavior are quite personal. Thus, any self-reported measures are subject to recall bias including deliberate concealment. Although significant, CI for spousal support was quite broad. This might be because the estimates are based on the number of participants enrolled in the study included in the study. More precise results could be obtained by increasing the sample size.
CONCLUSIONS AND RECOMMENDATIONS
Nonsupporting status of spouse and alcohol consumption was found to be the independent predictors of high-risk sexual behavior. Based on the current results, it is recommended to enhance the efforts in the direction of advocacy of safe sex behaviors at ART centers. Nonetheless, findings from the study have implication for future harm curtailment programs targeting alcohol use and encouragement of spouse and family support to eliminate discrimination with their closest social environment. The significant association between alcohol use and high-risk sexual behavior with low condom use rate underscores the importance of enhanced condom promotion programs. Periodic evaluation of the patient for assessing their sexual behavior along with special counseling session with their sexual partner has to be done, so as, to negotiate their partner for condom use.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Acknowledgment
We are thankful to Dr Neetu Gupta, Dr Suman Shukla, Medical Officer ART centre, Mrs Rajnigandha, Counselor, ART Centre, King George's Medical University Lucknow, Dr Abhishek Gupta, Dr Pallavi Shukla, Dr Ravikant and my dear juniors Dr Kriti, Dr Hossain, and Dr Naro for their constant encouragement and motivation in bringing out this manuscript.
REFERENCES
- 1.WHO | HIV/AIDS: HIV/AIDS. Global Situation and Trends. 2013. [Last accessed on 2014 Dec 30]. Available from: http://www.who.int/gho/hiv/en/
- 2.National AIDS Control Organisation. NACO Annual Report. 2013-14. [Last accessed on 2014 Dec 30]. Available from: http://www.naco.gov.in/upload/2014%20mslns/NACO_English%20-2013-14.pdf .
- 3.UNAIDS Report on the Global AIDS Epidemic. 2013. [Last accessed on 2015 Jan 30]. Available from: http://www.unaids.org/sites/default/files/media_asset/UNAIDS_Global_Report_2013_en_1.pdf .
- 4.National Family Health Survey (NFHS-3) [Last accessed on 2015 Mar 20]. Available from: http://www.rchiips.org/nfhs/nfhs3.shtml .
- 5.Managing Your Health: A Guide for People Living with HIV. Toronto: CATIE; 2009. Canadian AIDS Treatment Information Exchange. [Google Scholar]
- 6.Mhalu A, Leyna GH, Mmbaga EJ. Risky behaviours among young people living with HIV attending care and treatment clinics in Dar Es Salaam, Tanzania: Implications for prevention with a positive approach. J Int AIDS Soc. 2013;16:17342. doi: 10.7448/IAS.16.1.17342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 8.Jean-Baptiste R. Operations Research Results. Published for the U.S. Agency for International Development (USAID) by the Quality Assurance Project. Bethesda, MD: University Research Co., LLC; 2008. Factors Associated with Adherence to Antiretroviral Therapy in Rwanda: A Multi-site Study. [Google Scholar]
- 9.Yaya I, Saka B, Landoh DE, Patchali PM, Makawa MS, Senanou S, et al. Sexual risk behavior among people living with HIV and AIDS on antiretroviral therapy at the regional hospital of Sokodé, Togo. BMC Public Health. 2014;14:636. doi: 10.1186/1471-2458-14-636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bajunirwe F, Bangsberg DR, Sethi AK. Alcohol use and HIV serostatus of partner predict high-risk sexual behavior among patients receiving antiretroviral therapy in South Western Uganda. BMC Public Health. 2013;13:430. doi: 10.1186/1471-2458-13-430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Luchters S, Sarna A, Geibel S, Chersich MF, Munyao P, Kaai S, et al. Safer sexual behaviors after 12 months of antiretroviral treatment in Mombasa, Kenya: A prospective cohort. AIDS Patient Care STDS. 2008;22:587–94. doi: 10.1089/apc.2007.0247. [DOI] [PubMed] [Google Scholar]
- 12.Ncube NM, Akunna J, Babatunde F, Nyarko A, Yatich NJ, Ellis W, et al. Sexual risk behaviour among HIV-positive persons in Kumasi, Ghana. Ghana Med J. 2012;46:27–33. [PMC free article] [PubMed] [Google Scholar]
- 13.Ragnarsson A, Ekström AM, Carter J, Ilako F, Lukhwaro A, Marrone G, et al. Sexual risk taking among patients on antiretroviral therapy in an urban informal settlement in Kenya: A cross-sectional survey. J Int AIDS Soc. 2011;14:20. doi: 10.1186/1758-2652-14-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olley BO. Higher-risk sexual behaviour among HIV patients receiving antiretroviral treatment in Ibadan, Nigeria. Afr J AIDS Res. 2008;7:71–8. doi: 10.2989/AJAR.2008.7.1.8.436. [DOI] [PubMed] [Google Scholar]
- 15.Eisele TP, Mathews C, Chopra M, Lurie MN, Brown L, Dewing S, et al. Changes in risk behavior among HIV-positive patients during their first year of antiretroviral therapy in Cape Town South Africa. AIDS Behav. 2009;13:1097–105. doi: 10.1007/s10461-008-9473-2. [DOI] [PubMed] [Google Scholar]
- 16.Saha R, Saha I, Sarkar AP, Das DK, Misra R, Bhattacharya K, et al. Adherence to highly active antiretroviral therapy in a tertiary care hospital in West Bengal, India. Singapore Med J. 2014;55:92–8. doi: 10.11622/smedj.2014021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berhan A, Berhan Y. Is the sexual behaviour of HIV patients on antiretroviral therapy safe or risky in Sub-Saharan Africa. Meta-analysis and meta-regression? AIDS Res Ther. 2012;9:14. doi: 10.1186/1742-6405-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shuper PA, Joharchi N, Irving H, Rehm J. Alcohol as a correlate of unprotected sexual behavior among people living with HIV/AIDS: review and meta-analysis. AIDS Behav. 2009;13:1021–36. doi: 10.1007/s10461-009-9589-z. [DOI] [PubMed] [Google Scholar]
- 19.Pandey A, Mishra RM, Reddy DC, Thomas M, Sahu D, Bharadwaj D. Alcohol use and STI among men in India: Evidences from a National Household Survey. Indian J Community Med. 2012;37:95–100. doi: 10.4103/0970-0218.96094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Apondi R, Bunnell R, Ekwaru JP, Moore D, Bechange S, Khana K, et al. Sexual behavior and HIV transmission risk of Ugandan adults taking antiretroviral therapy: 3 year follow-up. AIDS. 2011;25:1317–27. doi: 10.1097/QAD.0b013e328347f775. [DOI] [PubMed] [Google Scholar]
- 21.UNFPA. The greatest hope for turnings the tide, a safe and supportive environment. New York, USA: UNFPA; 2007. Preventing HIV/AIDS, young people. [Google Scholar]
- 22.Jones D, Bagga R, Nehra R, Deepika, Sethi S, Walia K, et al. Reducing sexual risk behavior among high-risk couples in Northern India. Int J Behav Med. 2013;20:344–54. doi: 10.1007/s12529-012-9235-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


