Abstract
Objectives:
The present study evaluated the changes in serology and human immunodeficiency virus (HIV) testing behaviors over a 10-year period in a center in India.
Methods:
We used clinical data collected at the antenatal clinic from 2002 to 2011. The key outcomes were: (1) Proportion of women who opted for HIV test and those who tested positive; (2) proportion of male partners who came in for HIV test and those who tested positive; and (3) proportion of women who opted for continuation of pregnancy or for medical termination of pregnancy.
Results:
We tested 11,452 women for HIV over the 10-year period from 2002 to 2011. The proportion of women who opted for HIV testing was 72.0% (95% confidence interval [CI]: 70.7–73.4%). The acceptance of test increased from 35.9% (95% CI: 31.7–40.4%) in 2002 to the peak of 82.6% (95% CI: 78.6–86.8%) in 2009 (P < 0.001). The overall HIV prevalence over the decade was 0.70% (95% CI: 0.55–0.87%). The prevalence high at 1.11% (95% CI: 0.23–3.24%) in 2002 and reduced to 0.37% (95% CI: 0.12–0.87%) in 2011 (P < 0.001). Only 0.57% of male partners tested for HIV over this time period.
Conclusion:
Strategies to improve acceptance of testing in pregnant women should be included in the Indian guidelines. The male partners do not get tested. Thus, this component needs to be strengthened - by targeted interventions for male spouses - to make the program more effective.
Keywords: Human immunodeficiency virus, prevention of parent to child transmission, spouses, trends
INTRODUCTION
It is estimated that about India has about 2.09 million cases of people living with human immunodeficiency virus (HIV)/AIDS in 2011. Even though the incidence of new cases has reduced over the past few years, the total number of cases is relatively high.[1] India predominantly has a concentrated HIV epidemic. Thus, although the overall HIV adult prevalence in 2011 was 0.27%, in certain high-risk groups the estimated prevalence was very high. For instance, in the year 2010–2011, the prevalence was 2.67% in female sex workers was 2.67%, 4.43% in men who have sex with men, 7.14% in people who injected drugs, and 8.82% in male-to-female transgendered people.[1] The main route of transmission - unprotected sex - accounts for nearly 89% of the total new infections. The second most common route of transmission, accounting for 5% of the cases is a parent to child transmission.[2]
The first National AIDS Control Programme (NACP) in was launched in 1992 for prevention and control of HIV in India. The Prevention of Parent to Child Transmission (PPTCT) was initiated in 2002 under NACP-II.[1,2] The main components of the program were aimed at (1) Primary prevention of HIV in women; (2) avoid unintended pregnancies in HIV-infected women; (3) prevent transmission of HIV infection to the baby; and (4) support women and children living with HIV.[3] Even though the initial treatment strategy was single dose nevirapine, the current recommendations include providing antiretroviral therapy (ART) to all infected women).[1,3] In fact, the NACP has converged its program with the National Health Mission (NHM) to improve the reach to all pregnant women. The current recommendations include an essential package for PPTCT services; some of the components are: Counseling; “family centric approach;” provision of ART; institutional delivery; counseling and support post delivery; follow-up and care of the baby; and treatment of associated conditions (such as sexually transmitted infections).[3]
India, with more than 15,000 PPTCT centers, tests about 8.83 million women annually, and the program was integrated with the NHM to provide HIV testing services to all antenatal women.[3] However, only 53% of pregnant women use skilled child care, and the total estimated proportion of coverage of the pregnant women who have been tested for HIV was 23% in 2010.[3,4] Even though, there has been an improvement in women availing the Integrated Counselling and Testing Centres,[5] studies have identified certain shortcomings such as low coverage of the PPTCT program, poor follow-up of the mother and baby, low proportion of institutional deliveries, inadequate counseling services, poor laboratory facilities, and resistance to medications.[6,7,8,9,10]
The present study was designed to study the changes in serology and HIV testing behaviors over a 10-year period in a PPTCT center in a tertiary care center in India. We also assessed the public health implications of these changes on the PPTCT program in the country.
METHODS
The present study is a secondary analysis of clinical data collected at the antenatal clinic (ANC) from 2002 to 2011.
Study site
The study was conducted the Mahatma Gandhi Mission's Medical College and Hospital, Aurangabad, Maharashtra, India. It is situated at a distance of about 350 km from the state capital Mumbai and has experienced rapid urbanization over the past decade. The hospital has all specialty and subspecialty departments and caters mostly to low-middle and low-income patients.
Study procedures and population
The PPTCT program at the MGM Medical College and Hospital was started in the year 2002. Aurangabad was classified a Category A (>1% prevalence in ANC) district based on the surveillance data.[11] In concordance with the National AIDS Control Organisation (NACO) program, we implemented the opt-out policy of HIV testing. All women accessing antenatal care in the hospital were counseled about HIV testing using the group counseling method. We tested HIV in all consenting women. The posttest counseling was done in these women using one-to-one counseling technique. All women were also asked to discuss HIV with their spouses and get them tested in the center.
We discussed all the treatment and care options with HIV-infected women. These included various options - continuation of pregnancy or medical termination of pregnancy (MTP). In women who opted for continuation of pregnancy, we offered them therapy according to the NACO guidelines. These included: Single dose of nevirapine to the mother; elective caesarean section with no milking of cord; choice of feeding options; a single dose of nevirapine to the baby; and follow-up of all children in the hospital.
Statistical analysis
The key outcomes in our analysis were: (1) Proportion of women who opted for HIV test (total number of women who had an HIV test/total number of women who attended the ANC) and proportion of women who tested HIV positive (total number of women who tested HIV positive/total number of women tested); (2) proportion of male partners who came in for HIV test (total number of male partners tested/total number of women tested) and proportion who tested HIV positive (proportion of male partners who tested HIV positive/total number of male partners tested); and (3) proportion of women who opted for continuation of pregnancy or MTP (total number of women who continued with the pregnancy or opted for MTP/total number of women who tested HIV positive). We calculated the proportions and their 95% confidence intervals (CIs) for each year and the trends were assessed using the Chi-square test for trend. Data were analyzed using Stata Version 13 (StataCorp, College Station, Texas, USA).
The study was approved by the Ethics Committee at MGM Medical College, Aurangabad.
RESULTS
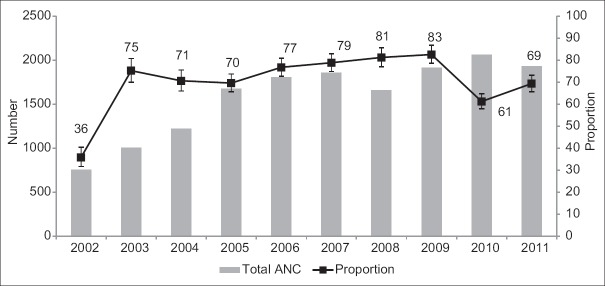
We tested 11452 women for HIV over the 10-year period from 2002 to 2011. The total ANC attendance over the 10-year period was 15901; thus, the total proportion of women who opted for HIV testing was 72.0% (95% CI: 70.7–73.4%). The acceptance of test increased from 35.9% (95% CI: 31.7–40.4%) in 2002 to the peak of 82.6% (95% CI: 78.6–86.8%) in 2009; the trend was statistically significant (Chi-square for trend P < 0.001) [Figure 1]. However, there was a reduction in the proportion from 2009 to 2011 [Figure 1]; this trend was also statistically significant (Chi-square for trend P < 0.001).
Figure 1.
Trends of the total antenatal attendance (ANC) and proportion of women who opted for HIV testing, 2002-11, Aurangabad, India
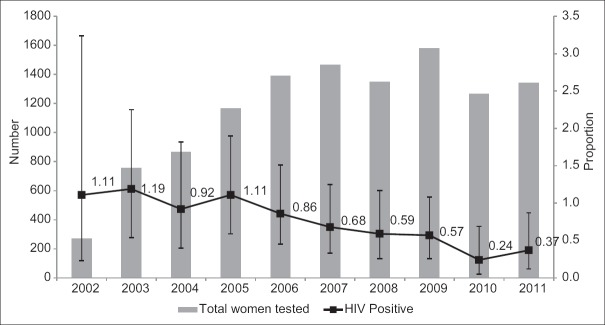
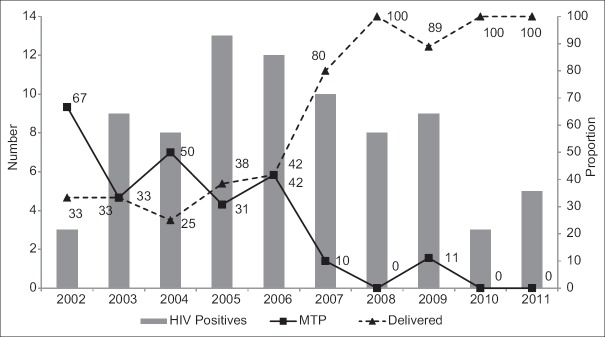
The overall HIV prevalence over the decade was 0.70% (95% CI: 0.55–0.87%). The prevalence was as high as 1.11% (95% CI: 0.23–3.24%) in 2002. It reduced over time: It was 0.86% (95% CI: 0.45–1.51%) in 2006 and as low as 0.37% (95% CI: 0.12–0.87%) in 2011 [Table 1]. This reduction in proportion was statistically significant (Chi-square for trend P < 0.001) [Figure 2]. In the year 2002, two of the three women who tested positive for HIV opted for MTP. However, the proportion of women who opted for MTP reduced over the 10-year period. None of the women opted for MTP in the year 2011 [Figure 3]. This reduction was statistically significant (Chi-square for trend, P = 0.001). Only one woman (of three positive women) opted for delivery in the year 2002. However, all HIV-infected women opted for delivery in the year 2011 [Figure 3]; this trend was statistically significant (P = 0.001).
Table 1.
The HIV testing behaviours of women and spouses, and HIV serology in women, 2002-11, Aurangabad, India
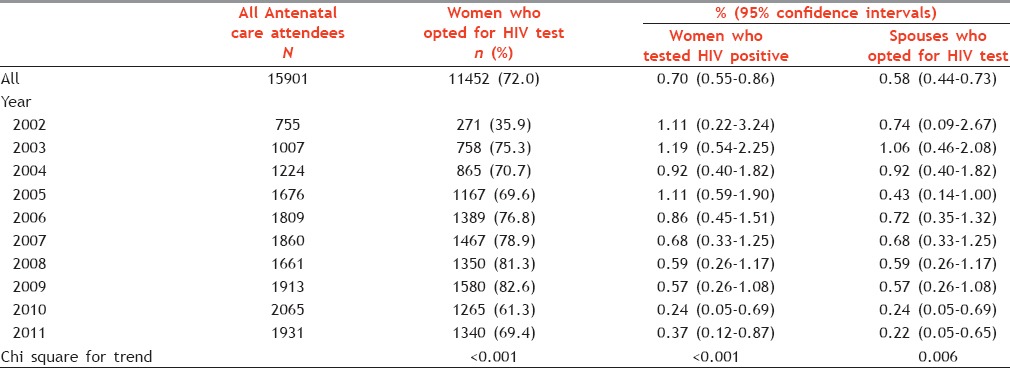
Figure 2.
Trends of the total antenatal women who opted for HIV test and proportion of women who were HIV infected, 2002-11, Aurangabad, India
Figure 3.
Trends of the total antenatal women were HIV infected, and proportion of those who opted for medical termination of pregnancy and continuation of pregnancy, 2002-11, Aurangabad, India
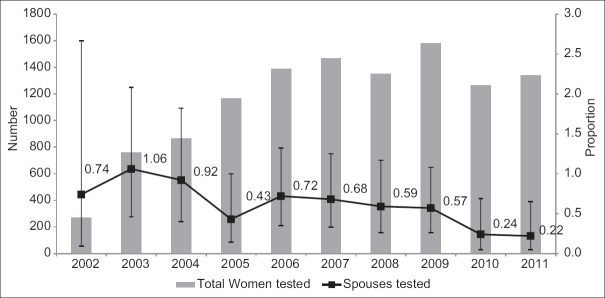
Only 0.57% of male partners tested for HIV over this time period. The proportion of male partners who opted for HIV testing was 0.73% (95% CI: 0.09–2.67%) in 2002. There was a gradual reduction in this proportion over the 10-year period [Figure 4]. The proportion of male partners who tested for HIV was as low as 0.22% (95% CI: 0.05–0.65%) in 2011; this reduction was statistically significant (Chi-square for trend, P = 0.006).
Figure 4.
Trends of the total antenatal women who opted for HIV test and proportion of spouses who tested for HIV, 2002-11, Aurangabad, India
Of the total 80 HIV-infected women, 48 have delivered. Of these, 27 children have completed their 18 months of follow-up (until the end of 2011); all of these children tested negative for HIV. Furthermore, seven children were still being followed up until the end of 2011.
DISCUSSION
Thus, in our study, the prevalence of HIV among antenatal women reduced over the 10-year period. Though, a high proportion of antenatal women opted for HIV testing; there was a decline in the proportion in the latter years. The proportion of spouses who underwent HIV testing was very low in our population.
In general, the trends of HIV prevalence have been similar to the overall state prevalence. For instance, the sentinel surveillance data show that the HIV prevalence in the ANC clinics in Maharashtra was 1.15% in 2003. However, the proportion had reduced to 0.42% in the year 2010–11.[12] Even though these findings are encouraging, an important area of concern is the reduction in the proportion of women who opted for HIV testing. Such reductions in the proportion of ANC women opting for HIV test have also been reported from other parts of India.[8] The overall, however, of the proportion of women who opted for HIV testing was similar to that observed in other parts of the country.[7,13] It has been suggested that, though testing and management facilities are available in the PPTCT centers, many women experience discrimination by various stakeholders (such as healthcare personnel, family members, and the larger community).[14] In addition, women may feel that HIV-positive status may bring shame to them or their family;[14] thus, they may be reluctant to undergo HIV test or access PPTCT services. Though counselors address individual level stigma and discrimination, systematic discrimination in healthcare settings needs to be addressed by incorporating various components of stigma and discrimination in HIV-infected individuals and means to address them in the guidelines for PPTCT programs in India.
Another important finding observed in this study is that all HIV-infected women opted for continuation of pregnancy in the latter years, whereas all HIV-infected women had opted for MTP in earlier years. Though some pregnancies in HIV-infected women may be unintended, it has also been observed that a high proportion of HIV women desires to have a child even if they already have children.[15,16,17] Tibrewal and Goswami found that HIV-infected women opted for MTP due to fear of transmission to the child.[18] Thus, increased awareness about HIV, availability of treatment for prevention of transmission, and availability of treatment options (including antiretroviral therapy) through government program for HIV care of infected children may have contributed to this change. Other issues that determine choices about pregnancy are the duration of HIV infection, economic status, and support from the family members.[16,18,19] For instance, Kanniappan et al. reported that women who were assured of family support and care of their infected children were more likely to opt to have a child.[19] Thus, pregnancy related choice in HIV-infected women is as much a socioeconomic issue as it is a clinical issue; these areas should form an important component of the PPTCT policy.
One of the most significant findings from our study was the poor attendance of the male partners in the PPTCT clinic. Less than 1% of male partners were tested in the PPTCT clinic; the proportion had significantly reduced over the past 10 years. Though, low male involvement has been reported globally,[20,21,22,23] none of these studies found the involvement to be as low as our study. In general, HIV testing among male partners has been reported to be significantly higher in HIV-infected women and in those whose men who had tested for HIV earlier.[24] A systematic review by Morfaw et al. found that reluctance to learn one's HIV status and lack of time were two main barriers to access these services.[25] Apart from these factors, cultural norms that pregnancy is only woman's affair and assuming that one's status is same as that of the partner were important factors that prevented men from attending the ANC.[25] Interestingly, knowledge about routes of HIV transmission and HIV testing facilities in government hospitals were found to be associated with a willingness to test by male partners.[26] In addition, women themselves may be disinclined to discuss HIV testing and HIV status with the male partners; this may be due to fear of stigma, adverse labels, or domestic violence.[25,27] Thus, effective programs (such as couple counseling) to encourage male participation should be designed and included in the PPTCT centers. It was earlier pointed out that the Indian PPTCT programs did not have specific strategies to include fathers in these centers. Though, a new strategy and policy document were released in 2013, it still does have any specific guidelines or methods for involving men in the PPTCT centers. It is quite possible that male partners may get tested at other sites (such as private clinics); but, there are no existing mechanisms to track these tests. Even the ANC data collected for regular monitoring do not reflect the male attendance in these centers. Thus, the program strategies need to be upgraded to include male partners and truly make it a prevention of “Parent” to child transmission.
We have not analyzed individual-level data, and the variables were group level or ecologic level analysis. Thus, we could have individual level predictors - a limitation of these analyses. Nonetheless, this study presents interesting trends over a 10-year period. To the best of our knowledge, the data analyzed in the study are from the longest follow-up period in an ANC after the initiation of the PPTCT program in India. The study has useful suggestions to improve the public health interventions in India. The PPTCT program, which provides probably the only chance for many women to get tested for HIV, needs to move beyond the clinical components and improve the psychosocial and counseling components. Strategies to improve acceptance of testing in pregnant women should be included in the PPTCT guidelines. In addition, even though focusing on the family is an important part of a package of essential services, there are no explicit guidelines on these.
CONCLUSION
Our data highlight that men do not get tested - at least in the PPTCT program. Thus, lack of their inclusion is one of the main shortcomings of the program and needs to be strengthened - by having specific targeted interventions for them and including the male partners in all the mass media campaigns to make the program more effective.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Acknowledgments
We would like to acknowledge the support by the Dean, Dr. A. Shroff and the contribution of Mr. Shafiq Baig, Counselor, MGM Medical College, Aurangabad, India.
REFERENCES
- 1.Annual Report 2013-14. New Delhi, India: Department of AIDS Control, Ministry of Health and Family Welfare, Government of India; 2014. National AIDS Control Organisation. [Google Scholar]
- 2.Annual Report 2010-11. New Delhi, India: Department of AIDS Control, Ministry of Health and Family Welfare, Government of India; 2012. National AIDS Control Organisation. [Google Scholar]
- 3.Updated Guidelines for Prevention of Parent to Child Transmission (PPTCT) of HIV Using Multi Drug Anti-Retroviral Regimen in India. New Delhi, India: Department of AIDS Control Basic Services Division, Ministry of Health and Female Welfare, Government of India; 2013. National AIDS Control Organisation. [Google Scholar]
- 4.World Health Organization. Global Health Observatory Data Repository: Prevention of Mother-to-child Transmission: Data by Country. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 5.Kwatra A, Bangal VB, Shinde K, Padaliya K. HIV seroprevalence among the pregnant population and utilisation of integrated counselling and training centre facilities at a teaching hospital in rural Maharashtra. Australas Med J. 2011;4:566–70. doi: 10.4066/AMJ.2011.714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dash M, Padhi S, Panda P, Pattnaik D, Parida B. PPTCT of HIV: Two and a half year experience at MKCG medical college, Berhampur, India. Indian J Med Microbiol. 2009;27:276–7. doi: 10.4103/0255-0857.53219. [DOI] [PubMed] [Google Scholar]
- 7.Joshi U, Kadri A, Bhojiya S. Prevention of parent to child transmission services and interventions – Coverage and utilization: A cohort analysis in Gujarat, India. Indian J Sex Transm Dis. 2010;31:92–8. doi: 10.4103/2589-0557.74983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mukherjee S, Ghosh S, Goswami DN, Samanta A. Performance evaluation of PPTCT (Prevention of parent to child transmission of HIV) programme: An experience from West Bengal. Indian J Med Res. 2012;136:1011–9. [PMC free article] [PubMed] [Google Scholar]
- 9.Goswami S, Chakravorty PS. Prevention of parent to child transmission of HIV (PPTCT): An effort of 4 years in a tertiary centre. J Obstet Gynaecol India. 2011;61:394–8. doi: 10.1007/s13224-011-0056-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sinha A, Roy M. An ICMR task force study of prevention of parent to child transmission (PPTCT) service delivery in India. Indian J Public Health. 2008;52:200–2. [PubMed] [Google Scholar]
- 11.National AIDS Control Organisation. Prioritisation of Districts for Programme Implemention. 2006. [Last cited on 2015 Feb 07]. Available from: http://www.naco.gov.in/upload/NACO%20PDF/District%20Categorisation%20for%20Priority%20Attention.pdf .
- 12.HIV Sentinel Surveillance 2012-13: A Technical Brief. New Delhi, India: Department of AIDS Control, Ministry of Health and Family Welfare, Government of India; 2014. National AIDS Control Organisation. [Google Scholar]
- 13.Kumar R, Virdi NK, Lakshmi PV, Garg R, Bhattacharya M, Khera A. Utility of prevention of parent-to-child transmission (PPTCT).Programme data for HIV surveillance in general population. Indian J Med Res. 2010;132:256–9. [PubMed] [Google Scholar]
- 14.Rahangdale L, Banandur P, Sreenivas A, Turan JM, Washington R, Cohen CR. Stigma as experienced by women accessing prevention of parent-to-child transmission of HIV services in Karnataka, India. AIDS Care. 2010;22:836–42. doi: 10.1080/09540120903499212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loutfy M, Raboud J, Wong J, Yudin M, Diong C, Blitz S, et al. High prevalence of unintended pregnancies in HIV-positive women of reproductive age in Ontario, Canada: A retrospective study. HIV Med. 2012;13:107–17. doi: 10.1111/j.1468-1293.2011.00946.x. [DOI] [PubMed] [Google Scholar]
- 16.Oladapo OT, Daniel OJ, Odusoga OL, Ayoola-Sotubo O. Fertility desires and intentions of HIV-positive patients at a suburban specialist center. J Natl Med Assoc. 2005;97:1672–81. [PMC free article] [PubMed] [Google Scholar]
- 17.Finocchario-Kessler S, Sweat MD, Dariotis JK, Trent ME, Kerrigan DL, Keller JM, et al. Understanding high fertility desires and intentions among a sample of urban women living with HIV in the United States. AIDS Behav. 2010;14:1106–14. doi: 10.1007/s10461-009-9637-8. [DOI] [PubMed] [Google Scholar]
- 18.Tibrewal R, Goswami S. Impact of HIV positive status on reproductive decision making. J South Asian Fed Obstet Gynaecol. 2011;3:82–5. [Google Scholar]
- 19.Kanniappan S, Jeyapaul MJ, Kalyanwala S. Desire for motherhood: Exploring HIV-positive women's desires, intentions and decision-making in attaining motherhood. AIDS Care. 2008;20:625–30. doi: 10.1080/09540120701660361. [DOI] [PubMed] [Google Scholar]
- 20.Byamugisha R, Tumwine JK, Semiyaga N, Tylleskär T. Determinants of male involvement in the prevention of mother-to-child transmission of HIV programme in Eastern Uganda: A cross-sectional survey. Reprod Health. 2010;7:12. doi: 10.1186/1742-4755-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Katz DA, Kiarie JN, John-Stewart GC, Richardson BA, John FN, Farquhar C. Male perspectives on incorporating men into antenatal HIV counseling and testing. PLoS One. 2009;4:e7602. doi: 10.1371/journal.pone.0007602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Msuya SE, Mbizvo EM, Hussain A, Uriyo J, Sam NE, Stray-Pedersen B. Low male partner participation in antenatal HIV counselling and testing in northern Tanzania: Implications for preventive programs. AIDS Care. 2008;20:700–9. doi: 10.1080/09540120701687059. [DOI] [PubMed] [Google Scholar]
- 23.Haile F, Brhan Y. Male partner involvements in PMTCT: A cross sectional study, Mekelle, Northern Ethiopia. BMC Pregnancy Childbirth. 2014;14:65. doi: 10.1186/1471-2393-14-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brou H, Djohan G, Becquet R, Allou G, Ekouevi DK, Viho I, et al. When do HIV-infected women disclose their HIV status to their male partner and why. A study in a PMTCT programme, Abidjan? PLoS Med. 2007;4:e342. doi: 10.1371/journal.pmed.0040342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morfaw F, Mbuagbaw L, Thabane L, Rodrigues C, Wunderlich AP, Nana P, et al. Male involvement in prevention programs of mother to child transmission of HIV: A systematic review to identify barriers and facilitators. Syst Rev. 2013;2:5. doi: 10.1186/2046-4053-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Das A, Babu GR, Ghosh P, Mahapatra T, Malmgren R, Detels R. Epidemiologic correlates of willingness to be tested for HIV and prior testing among married men in India. Int J STD AIDS. 2013;24:957–68. doi: 10.1177/0956462413488568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rujumba J, Neema S, Byamugisha R, Tylleskär T, Tumwine JK, Heggenhougen HK. “Telling my husband I have HIV is too heavy to come out of my mouth”: Pregnant women's disclosure experiences and support needs following antenatal HIV testing in Eastern Uganda. J Int AIDS Soc. 2012;15:17429. doi: 10.7448/IAS.15.2.17429. [DOI] [PMC free article] [PubMed] [Google Scholar]