Abstract
Context:
Zoonotic sexual transmission.
Aims:
Identification of unknown microorganisms causing sexually transmitted zoonotic infection was a common effort of clinicians and the laboratory.
Settings and Design:
A male patient had recurring urethritis and balanitis after having repeated unprotected penetrative sexual intercourse with female piglets. He claimed allergy to metals and plastics. Routine microbiological tests were carried out.
Materials and Methods:
Specimens from the urethra, glans, rectum, throat, urine, and blood were cultured. Subsequently, isolates were tested for their biochemical activity and antibiotic susceptibility.
Results:
Kurthia gibsonii was isolated from both urethra and glans. No other concomitant infection was detected. The patient was cured with oral cefuroxime for 15 days and topical gentamicin cream for 2 months.
Conclusion:
This is the first reported zoophilic infection by Kurthia spp. Fecal contamination of animals' genital tract was the possible source of infection. Immune disturbance of the patient might predispose to opportunistic Kurthia infection.
Keywords: Antibiotic treatment, balanitis, Kurthia gibsonii, sexual abuse of piglets, Ukrainian gonorrhea, urethritis
INTRODUCTION
Sexual abuse of animals has been known since ancient times. Its designation (recently: Sex with animals [SWA]), range of animal species, and acceptance by the public have been varied depending on historical times, geographical locations, demographic characteristics, and related sexual behaviors.[1] Direct contact of genital organs between humans and animals predisposes to mutual transmission of microbes being present either as members of the normal flora or pathogens. However, data on zoophilic sexual transmission of nonhuman pathogens are scarcely available in the literature. In our laboratory, a bacterial species was identified, causing sexually transmitted zoonosis.
MATERIALS AND METHODS
A 36-year-old male was referred to the National Institute of Dermato-Venereology (NIDV), Budapest, with the accompanying diagnosis, “query zoonosis?” by his local dermato-venereologist from a remote small town. The symptoms of the patient had started with urethritis and acute prostatitis 3 years ago. On unknown antibiotic treatment, these symptoms ceased. Six months later, prostatitis relapsed once, while urethritis relapsed several times. At the time of the first episode of urethritis, he also experienced balanitis that became chronic. During 3 years of supervision, no specimen was taken for microbiological diagnosis, but urethritis of the patient was treated with several courses of various antibiotics. Balanitis was treated either with the glans rinsed twice daily with chlorogene (1 g tablet dissolved in 1 L of tap water) or 10% (w/w) povidone-iodine antiseptic cream applied twice a day; both treatments were unsuccessful. Before admission, his glans was treated with another antiseptic cream (10 mg hydrocortisone, 10 mg natamycin, and 3.5 mg neomycin/g) twice a day. The latter regimen resulted in a mild improvement of the inflammation.
On admission, the patient was in good physical and mental health without any general symptoms. He had no history of chronic disease, did not experience fever or rigor at any time during the infection but claimed allergies to nickel, rubber, adhesive tape, and cosmetic perfumes. He complained of urethral pain and burning during urination. Physical examination revealed mild balanitis with soreness and central induration in a 5 mm diameter spot. Biopsy was recommended, but he refused it. The absence of regional lymphadenopathy and lymphangitis was established. He denied any sexual contact with female or male partners in the preceding 3 years but had occasional unprotected penetrative intercourse with female piglets.
Specimens were taken from his urethra, glans, throat, rectum, midstream urine, and subsequently inoculated into different media routinely used in the laboratory. Standardized test tube biochemical methods were used to identify the bacteria. Venous blood was drawn for routine chemistry, blood culture, and serology. Antibiotic susceptibility was tested by standard disc diffusion technique (Oxoid Ltd., Cambridge, UK). Other quantitative susceptibility methods were not available for routine use in this laboratory.
RESULTS
According to standard references,[2] the isolates from the urethra and glans were identified as Kurthia gibsonii. Differentiation from other microbes of porcine origin as L. monocytogenes (e.g., nonhemolytic, carbohydrate fermenter) or E. rhusiopathiae (e.g., nonhemolytic, catalase and esculin hydrolysis negative) was considered. No pathogenic microbes were obtained from any specimen [Table 1].
Table 1.
Major characteristics of Kurthia gibsonii isolates obtained from our patient and differential diagnostic procedures
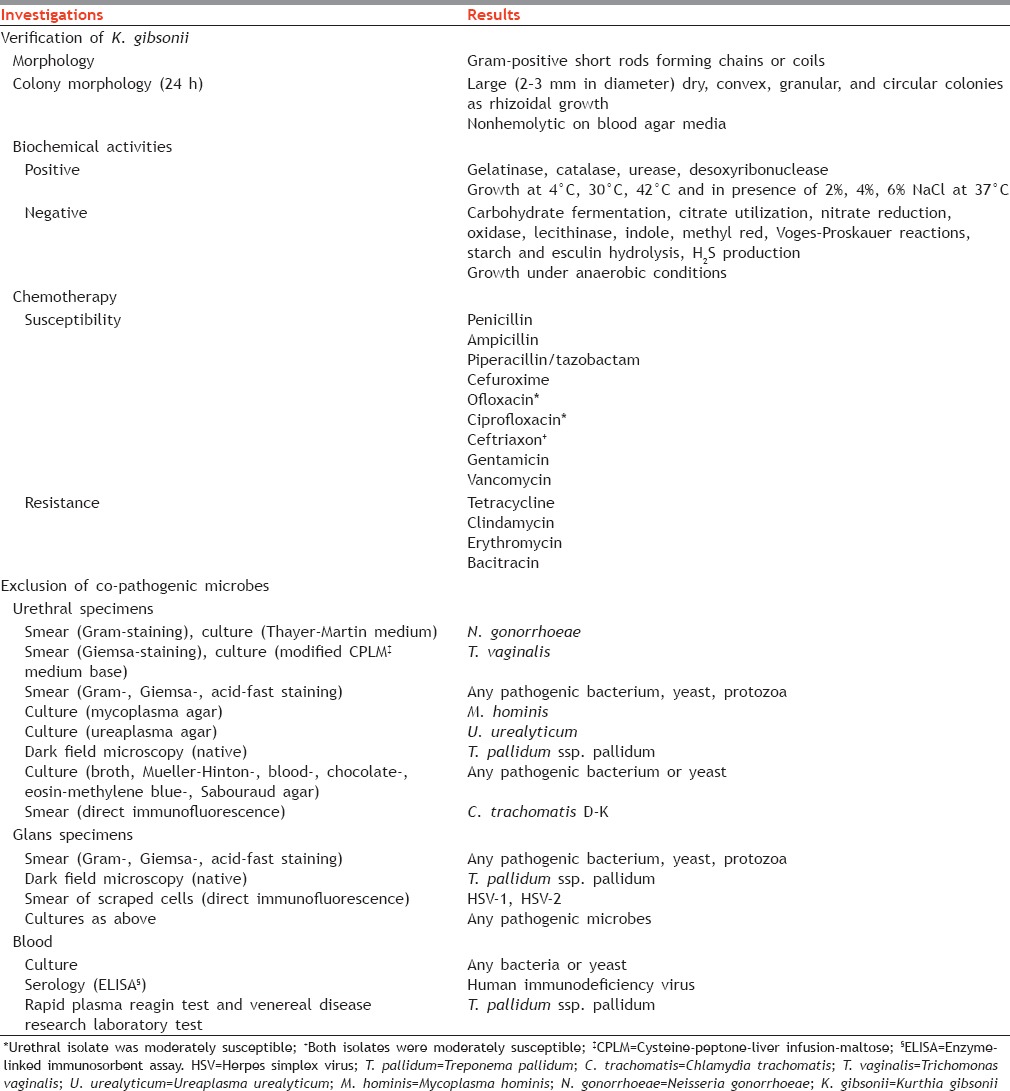
Antibiotic sensitivity of isolates was almost identical [Table 1]. The patient was treated with oral cefuroxime axetil (500 mg twice a day for 15 days). He rinsed the surface of the glans with 10% (w/w) povidone-iodine solution daily twice in his home without success for 10 days, so consequently treatment with 0.1% (w/w) gentamicin sulfate topical cream to be applied twice daily was prescribed. After 2 months of treatment, K. gibsonii was not recovered from repeat specimens taken from the urethra and glans. Urethral pain and inflammation on the glans disappeared. The patient was cured and has not returned in the following 14 months while authors worked at NIDV.
DISCUSSION
The genus Kurthia contains three recognized species: K. zopfii, K. gibsonii, and K. sibirica. Additional species are mentioned in the literature but have not been validated.[2] K. gibsonii and K. zopfii are frequently found in the environment, decomposing organic materials, swine carcasses,[3] feces of farmyard animals,[4] spoiled pork, and other food;[4,5] consequently, they might cause gastroenteral infections. Different Kurthia species have been isolated from the human feces including from cases of acute diarrhea.[6] K. massiliensis sp. nov. was isolated from the feces of a healthy adult.[7] They are not part of the normal flora, and in the majority of cases, they have not normally been regarded as pathogenic.[8] Kurthia infections rarely become systemic. K. zopfii was isolated from the blood of an infant with septicemia.[9] A 31-year-old male intravenous drug user had endocarditis due to K. bessonii infection.[10] Kurthia species very rarely cause bacteremia in immunocompromised patients with indwelling catheters or penetrating injuries.[8] Kurthia sp. might spread to humans via dog bite.[11] This suggests possible zoonotic spread. The clinical evidence of the pathogenicity of Kurthia has never been confirmed and the virulence factors are unknown: It probably has low virulence.[8]K. gibsonii might damage mucous membrane surfaces.[6]
Kurthia spp. have no validated testing methods by the Clinical and Laboratory Standards Institute (CLSI, formerly NCCLS, Wayne, PA, USA) or other organization.[2,8] The complete microbiological diagnostic procedures and comparison of sensitivity to chemotherapeutic agents tested so far in the case of other Kurthia species as well have been described lately.[12] The complete spectrum of their susceptibility to chemotherapeutics is unknown; no definitive treatment guidelines have been suggested.[8]
Our case is the first to show that K. gibsonii can spread from an animal to a human by zoophilic sexual intercourse, and the mucous membranes of the human genital tract can support bacterial survival. Fecal contamination of piglets' genital tract might have been the source of his infection. On this occasion, K. gibsonii did not cause disseminated infection. To what extent this patient's allergy might have contributed to the development of his infection with K. gibsonii is unknown. This could be a warning sign to those who suffer from any form of immunosuppression.
Persons who contract infection from animals can forward microbes to their human sexual partners. At the end of World War II when the Soviet Red Army invaded Hungary, several females raped by Ukrainian soldiers suffered from a gonorrhea-like disease. No known pathogen was found, and the public denoted this disease as “Ukrainian gonorrhea” (Prof. J. Sinkovics, University of South Florida, Tampa, FL, USA, personal communication). Cases of SWA among soldiers were suspected; consequently, animal microbes could be transmitted to females. Due to disintegrated wartime health system, such cases have never been studied. Since the “sexual revolution” in the 60s, both clinicians and the microbiology laboratories have to be prepared for diagnosing unusual pathogens. Subjects who report SWA also report more venereal diseases.[1] In our laboratories, all procedures were carried out manually; consequently, discordant biochemical results were noticed early. Using automated diagnostic tools not programed for animal or environmental microbes, such pathogens could be misinterpreted.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
REFERENCES
- 1.Zequi Sde C, Guimarães GC, da Fonseca FP, Ferreira U, de Matheus WE, Reis LO, et al. Sex with animals (SWA): Behavioral characteristics and possible association with penile cancer. A multicenter study. J Sex Med. 2012;9:1860–7. doi: 10.1111/j.1743-6109.2011.02512.x. [DOI] [PubMed] [Google Scholar]
- 2.Stackebrandt E, Keddie RM, Jones D. The genus Kurthia. In: Dworkin M, Falkow S, Rosenberg E, Schleifer KH, Stackebrandt E, editors. The Prokaryotes. New York, US: Springer Science and Business Media LLC; 2006. pp. 519–29. [Google Scholar]
- 3.Howard GT, Duos B, Watson-Horzelski EJ. Characterization of the soil microbial community associated with the decomposition of a swine carcass. Int Biodeterior Biodegradation. 2010;64:300–4. [Google Scholar]
- 4.Shaw S, Keddie RM. A numerical taxonomic study of the genus Kurthia with a revised description of Kurthia zopfii and a description of Kurthia gibsonii sp. nov. Syst Appl Microbiol. 1983;4:253–76. doi: 10.1016/S0723-2020(83)80054-X. [DOI] [PubMed] [Google Scholar]
- 5.Pin C, Baranyi J. Predictive models as means to quantify the interactions of spoilage organisms. Int J Food Microbiol. 1998;41:59–72. doi: 10.1016/s0168-1605(98)00035-x. [DOI] [PubMed] [Google Scholar]
- 6.Jarumilinta R, Miranda M, Villarejos VM. A bacteriological study of the intestinal mucosa and luminal fluid of adults with acute diarrhoea. Ann Trop Med Parasitol. 1976;70:165–79. doi: 10.1080/00034983.1976.11687109. [DOI] [PubMed] [Google Scholar]
- 7.Roux V, El Karkouri K, Lagier JC, Robert C, Raoult D. Non-contiguous finished genome sequence and description of Kurthia massiliensis sp. nov. Stand Genomic Sci. 2012;7:221–32. doi: 10.4056/sigs.3206554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Forbes BA, Sahm DF, Weissfeld AS. Diagnostic Microbiology. 10th ed. St. Louis, MO, US: Mosby; 1988. [Google Scholar]
- 9.Yang M, Sun Y, Ge P, Dong QY, Ma ZX. A case of infant septicemia caused by Kurthia zopfii. Chin J Microbiol Immunol. 1985;5:485. [Google Scholar]
- 10.Pancoast SJ, Ellner PD, Jahre JA, Neu HC. Endocarditis due to Kurthia bessonii. Ann Intern Med. 1979;90:936–7. doi: 10.7326/0003-4819-90-6-936. [DOI] [PubMed] [Google Scholar]
- 11.Wunder JA, Briner WW, Calkins GP. Identification of the cultivable bacteria in dental plaque from the beagle dog. J Dent Res. 1976;55:1097–102. doi: 10.1177/00220345760550061601. [DOI] [PubMed] [Google Scholar]
- 12.Ongrádi J, Stercz B, Kövesdi V, Nagy K, Chatlynne L. Isolation of Kurthia gibsonii from non-gonorrheal urethritis: Implications for the pathomechanism upon surveying the literature. Acta Microbiol Immunol Hung. 2014;61:79–87. doi: 10.1556/AMicr.61.2014.1.8. [DOI] [PubMed] [Google Scholar]


