Abstract
Crusted scabies is a rare manifestation of scabies characterized by uncontrolled proliferation of mites in the skin. It is common in patients with sensory neuropathy, mentally retarded persons and in patients who are immunosuppressed. Further, crusted scabies can rarely present as erythroderma (<0.5% cases) necessitating a high index of suspicion for its diagnosis. Because of its rare occurrence, we are reporting a case of crusted scabies presenting as erythroderma, in a human immunodeficiency virus seropositive patient.
Keywords: Crusted scabies, erythroderma, human immunodeficiency virus, immunosuppression
INTRODUCTION
Crusted scabies was described by Boeck and Danielssen among lepers in Norway in 1848, and named as “Scabies Norvegi Boeki” by von Hebra in 1862. Crusted scabies is characterized by hyperkeratosis and crusting of the skin due to the profuse proliferation of mites resulting from an altered host response to the infestation. Various cutaneous, neurologic, and immunologic diseases, which predispose to crusted scabies, have been described.[1] Crusted scabies can rarely present as erythroderma (<0.5% cases) requiring high index of suspicion for its diagnosis.[2] Because of heavy infestation, patients with crusted scabies are capable of triggering an epidemic of scabies. Early recognition and treatment are necessary to avoid complications and an outbreak of scabies.[3]
CASE REPORT
A 71-year-old male HIV seropositive patient came to skin outpatient department with complaints of itching and scaling over neck followed by hands, feet, and eyes, and then gradually progressing to the whole body since 3 months. The symptoms had increased in severity in the last 1 week, which aggravated during nights. History of generalized pruritus with night aggravation was present in son and wife.
The patient had associated complaints of generalized weakness and mild fever since 2 months, recurrent diarrhea since 1 month and breathlessness for 2 days.
He was on antiretroviral therapy (ART) – (tablet [emtricitabine 100 mg + efavirenz 600 mg + tenofovir 300 mg], both once daily) along with (tablet [trimethoprim 160 mg + sulfamethoxazole 800 mg] since 1.5 years). He was also on Cat-1 antitubercular treatment (AKT) since 6 months for tubercular lymphadenitis.
General examination revealed conjunctival pallor. Bilateral inguinal and axillary lymph nodes were palpable, nontender, multiple, firm, and discrete. Cutaneous examination revealed diffuse scaling on the scalp, whitish plaque on buccal mucosa suggestive of oral candidiasis. Bilateral multiple yellowish crusted plaques were present on the face, chest, back, abdomen, both upper limbs, and lower limbs including palms and soles [Figure 1a and b]. Nails showed longitudinal ridging. Systemic examination findings were within normal limits.
Figure 1.

(a) Thick yellowish-white crusted plaques on the face (periorbital region), on admission. (b) Thick yellowish-white crusted plaques on trunk, on admission
Differential diagnoses considered were psoriasis, eczema, and cutaneous lymphoma. Complete blood count, peripheral blood smear, urine routine and microscopy, blood sugar and liver function tests were within normal limits. CD4 count was 115 cells/cu.mm. Renal function tests showed elevated blood urea (162 mg/dl), serum creatinine (4.7 mg/dl), and serum potassium levels (6.06 mmol/L) as patient had reduced oral intake for past 2 days, which normalized with fluid and electrolyte supplementation. Ultrasonography (USG) abdomen showed fatty changes (Grade 2) in liver. USG chest showed mild to moderate pleural effusion on the right side and mild pleural effusion on the left side. Chest X-ray (posteroanterior view) revealed blunting of right cardiopulmonary angle. Sputum acid-fast bacilli were negative.
10% potassium hydroxide examination of the crust revealed scabies mite [Figure 2]. Histopathological study revealed the presence of transverse section of mites in stratum corneum, hyperkeratosis, acanthosis, elongated rete ridges, and dermal inflammatory infiltrate consisting of mononuclear cells and eosinophils [Figure 3].
Figure 2.

Potassium hydroxide examination of crust showing scabies mite
Figure 3.
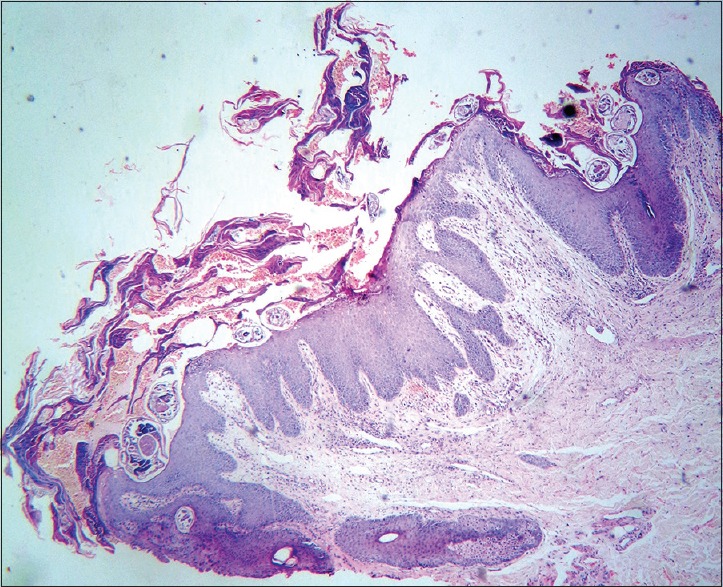
Transverse section showing multiple scabies mites seen in stratum corneum (H and E)
Treatment included patient isolation, parenteral antibiotic (injection cefotaxime 1 g IV 8thh for 7 days), tablet ivermectin 12 mg stat dose (repeated after 1 week), tablet hydroxyzine 25 mg twice daily, topical permethrin 5% cream once weekly night application for 2 weeks, (urea 10% + lactic acid 10% + propylene glycol 10% + liquid paraffin 10%) cream twice daily. Previous ART and AKT were continued as per the physician's advice (as the patient was not in clinical or immunological failure with the present ART). For altered renal parameters and elevated serum potassium, intravenous fluid supplementation (500 ml normal saline every 8 h) and potassium correction were given, until normalization over 4 days. As per chest physician's advice, with continued AKT and salbutamol nebulization, breathlessness was relieved. Patient improved within 10 days without any complications [Figure 4a and b]. Skin scrapings done at 1 week and 4 weeks were negative. Topical permethrin was prescribed to family members.
Figure 4.

(a) Reduced crusting on face after oral ivermectin, two applications of topical permethrin (5%) cream, and topical keratolytics. (b) Reduced crusting on trunk after oral ivermectin, two applications of topical permethrin (5%) cream and topical keratolytics
DISCUSSION
Clinical features, investigations, and prompt response to treatment confirmed that the cause for erythroderma in our patient was crusted scabies. Furthermore, the outbreak of scabies in the family members gave a hint to the diagnosis.
Crusted scabies typically develops in patients with a defective T-cell immune response or decreased cutaneous sensation or reduced ability to mechanically debride the mites.[3]
In human immunodeficiency virus (HIV) infection, crusted scabies is seen usually at CD4 counts <150 cells/cu.mm.[4] Dia et al. found that HIV infection was the most commonly associated disease, seen in 45% of the patients.[5]
Clinically, the lesions may be asymptomatic or mildly itchy, erythematous localized hyperkeratotic plaques, distributed on the extremities, back, face, scalp, and nail folds.[6] Firmly adherent crusts are creamy, gray, yellow-brown, or yellow-green in color. It can also present as warty dermatosis of the hands and feet, dystrophic nails with subungual hyperkeratosis and debris.[3]
Complications include secondary bacterial infection, generalized lymphadenopathy, and sepsis.[3]
Crusted scabies should always be suspected in any crusted lesion in acquired immune deficiency syndrome patients. It can mimic various conditions such as psoriasis, eczema, seborrheic dermatitis, Darier disease, pityriasis rubra pilaris, lichen planus, and cutaneous lymphoma.
Demonstration of mite with direct microscopic examination of the skin scrapings, with noninvasive techniques such as standard dermoscopy, epiluminescence microscopy, and high-resolution videodermatoscopy; or histopathology can be used for diagnosis.[3] On dermoscopy, “triangle sign,” “the delta wing jet with contrail” sign corresponding to the “head” portion of the mite and the head of mite with trailing burrow, respectively, are suggestive of scabies.[7] Eosinophilia and elevated serum IgE levels may be seen. DNA fingerprinting system for mite is useful to know if the patient is really cured.[3]
Treatment includes isolation, clipping of nails, and laundering of clothes. Due to resistant nature of the disease, concomitant oral and topical treatment is preferred such as oral ivermectin (200 mcg/kg) with permethrin 5% cream/benzyl benzoate 25% emulsion.[3] Efficacy of permethrin single application is maximum among various antiscabitic topicals available, i.e. 97.8%.[8] Oral ivermectin has the efficacy of 50% after 24 h, 85% after 72 h, and 94% by 1 week.[9] We had given a combination of topical permethrin and oral ivermectin.
Symptomatic treatment includes antihistamines and emollient application. Keratolytic agents such as 5–10% salicylic acid, 40% urea or soaking in a hot water bath for thick crusts removal can be used. Broad-spectrum antibiotics are indicated for sepsis.
CONCLUSION
Crusted scabies should be considered in a HIV-seropositive patient presenting with erythroderma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
REFERENCES
- 1.Bumb RA, Mehta RD. Crusted scabies in a patient of systemic sclerosis. Indian J Dermatol Venereol Leprol. 2000;66:143–4. [PubMed] [Google Scholar]
- 2.Das A, Bar C, Patra A. Norwegian scabies: Rare cause of erythroderma. Indian Dermatol Online J. 2015;6:52–4. doi: 10.4103/2229-5178.148951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karthikeyan K. Crusted scabies. Indian J Dermatol Venereol Leprol. 2009;75:340–7. doi: 10.4103/0378-6323.53128. [DOI] [PubMed] [Google Scholar]
- 4.Mendiratta V, Mittal S, Jain A, Chander R. Mucocutaneous manifestations in children with human immunodeficiency virus infection. Indian J Dermatol Venereol Leprol. 2010;76:458–66. doi: 10.4103/0378-6323.69041. [DOI] [PubMed] [Google Scholar]
- 5.Dia D, Dieng MT, Ndiaye AM, Ndiaye B, Develoux M. Crusted scabies in Dakar apropos of 11 cases seen in a year. Dakar Med. 1999;44:243–5. [PubMed] [Google Scholar]
- 6.Perna AG, Bell K, Rosen T. Localised genital Norwegian scabies in an AIDS patient. Sex Transm Infect. 2004;80:72–3. doi: 10.1136/sti.2003.002048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fox G. Diagnosis of scabies by dermoscopy. BMJ Case Rep. 2009;10:1136. doi: 10.1136/bcr.06.2008.0279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krishnan SS, Lockshin BN. Topical antiparasitic agents. In: Wolverton SE, editor. Comprehensive Dermatologic Drug Therapy. 3rd ed. Edinburgh Elsevier Publications; 2013. pp. 481–6. [Google Scholar]
- 9.Elston D. Systemic antiparasitic agents. In: Wolverton SE, editor. Comprehensive Dermatologic Drug Therapy. 3rd ed. Edinburgh Elsevier Publications; 2013. pp. 135–41. [Google Scholar]


