Abstract
Hamartoma of the bladder is an unusual entity described in only eleven patients to date. It may present as painless hematuria, irritative urinary tract symptoms, or inability to void or it may be diagnosed incidentally. Hamartoma of the bladder may be isolated or occur as part of a syndrome. No isolated bladder hamartoma to date has shown malignant potential. We describe here a bladder hamartoma in a 15-year-old boy.
Keywords: Hamartoma of bladder, hematuria, pediatric
Introduction
Hamartoma of the urinary bladder, especially in children, is an unusual type of benign tumor. It consists of a mixture of tissues resembling Von Brunn’s nests, cystitis cystica and cystitis glandularis. The stroma may be muscular, fibrous or edematous. Conventional methods, such as cystoscopy and excretory urography, are helpful in locating the lesions but they cannot distinguish hamartoma from a malignant mesenchymal bladder tumor or demonstrate extraluminal extension. Ultrasonography and computerized tomography (CT) can provide excellent means for identifying extravesical tumor extension and can be used as a complementary diagnostic modality to endoscopy in patients affected by hamartoma of the bladder. However, only histopathologic examination enables a definitive diagnosis.
To the best of our knowledge, only eleven cases diagnosed as hamartoma of the urinary bladder have been reported previously. We present an additional case of this rare tumor in a 15 year-old boy and briefly review the literature.
Case presentation
A 15-year-old boy presented to our clinic with urinary frequency, urgency and hesitancy of two months’ duration. He had no history of dysuria, fever, or abdominal pain. However, he experienced an episode of painless hematuria one year earlier that resolved spontaneously. Medical history revealed asthma not requiring regular medication. He was not a smoker and his family history was unremarkable.
A physical examination showed nothing unusual. All laboratory investigations, including blood count, coagulation profile and urine cytology were normal. Urine culture showed no evidence of infection. CT scan with intravenous contrast material showed a polypoidal growth arising from the left lateral wall of the bladder, with uptake of contrast in the arterial phase. The bladder was well delineated, with no evidence of extravesical extension or hydronephrosis, and his ureters were of normal caliber (Figure 1).
Figure 1.
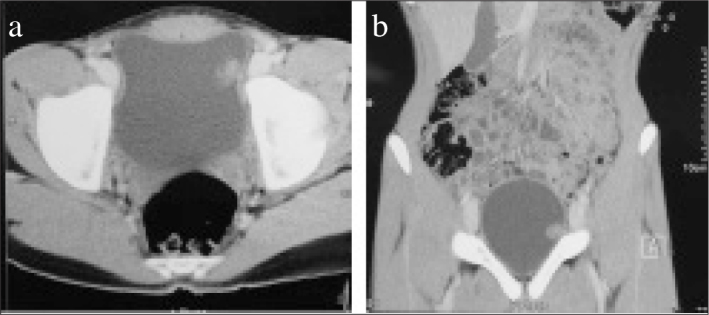
a, b. Computerized tomography of the abdomen and pelvis with intravenous contrast material. (a) Cross sectional images of the bladder following injection of intravenous contrast material showed a vascular exophytic growth coming off from the left lateral bladder wall. (b) Only intraluminal extension was observed
Cystoscopic examination showed a 5 cm polypoidal pedunculated, partly cystic mass arising from the left lateral wall of the bladder (Figure 2). Transurethral resection of the bladder tumor was performed. Histopathological examination revealed a benign urothelial lining with numerous round to oval variably sized urothelial nests, appearing as “Von Brunn’s nests”. Some of these nests showed central cystic dilatation with amorphous eosinophilic secretions, while others showed columnar cell lining with goblet cells forming both cystitis cystica and glandularis, and irregular distribution. In some areas, intersecting loose smooth muscle fibers were present among the glands. The stroma has a fibromyxoid structure with plump benign fibroblasts and congested, dilated capillaries. No mitosis, necrosis or atypical features was seen in the epithelium or stroma (Figure 3).
Figure 2.
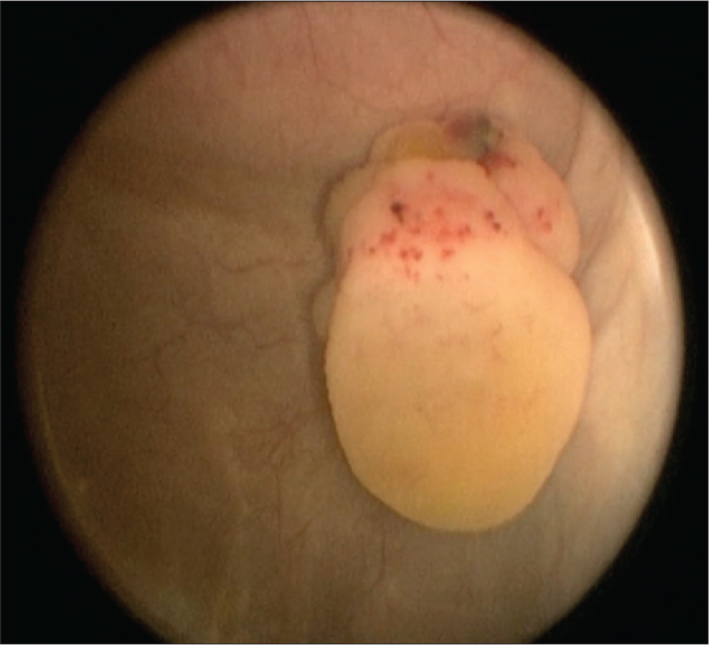
Intraoperative findings on cystoscopy, showing a 5 x 5 cm polypoidal partly cystic pedunculated bladder mass arising from the left lateral bladder wall and sparing the trigone
Figure 3.
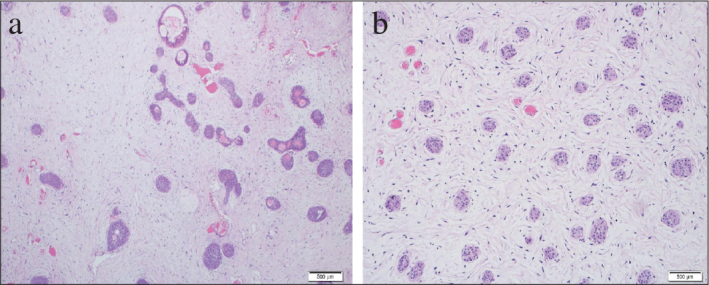
a, b. Histologic examination of tumor tissue. H&E slide showing; (a) florid nests of urothelial cells in a background of fibromyxoid stroma and (b) congested capillaries
The differential diagnosis initially included florid Von Brunn’s nests, but the size, depth and growth pattern of the lesion favored the diagnosis of hamartoma. This diagnosis was supported by findings of fibromyxoid stroma with occasional fascicles of smooth muscle. No features suggested the nested variant of urothelial carcinoma or inverted papilloma. Long-term follow-up, including regular urinalysis and ultrasound examination was recommended to the patient.
Discussion
Hamartoma is a benign tumor-like malformation made of abnormal mixtures of cells and tissues and found in areas of the body where cellular proliferation occurs. Hamartomas have been often reported in the gastrointestinal tract, bronchial tree, brain and bone, but they are very rare in the urinary bladder.[1] Since the first reported case in 1949,[2] to our best of knowledge, only 11 cases have been reported in the literature so far.[3]
Most of the patients had similar clinical presentations, with gross hematuria, dysuria, and mild suprapubic discomfort.[1,4] The size of the lesions may range from tiny growths to large masses. They are always solitary and may be located anywhere, although they favor the bladder dome or its posterolateral walls. Tumors larger than 8 cm in diameter have not been reported. Alternatively, bladder hamartomas may be asymptomatic and be discovered incidentally on autopsy.[5]
Bladder hamartomas might take place as an isolated entity or as part of a syndrome, including Goldenhar syndrome,[4] multiple hamartomatous syndrome or Cowden disease,[6] Peutz-Jeghers syndrome[7] or Beckwith-Wiedemann syndrome.[8] Most of these hamartomas arise from the bladder wall. They can also arise from the trigone,[9] extravesically from the intramural part of the urachal remnant,[10] and from the urethra.[11]
Bladder hamartomas are generally benign and can be resected transurethrally or by partial cystectomy. Any disease recurrence has not been observed on follow-up extending to a maximum 17 months.[9] It is important, however, to distinguish between isolated bladder hamartomas and the presence of hamartomas in other systems. Malignancy of the bladder, in the form of papillary carcinoma, has been reported in patients with familial hamartomas (i.e. Cowden disease).[6] One patient with a recurrent bladder cancer was found to have a polypoidal lesion at the dome, and histopathological examination of transurethral resection material revealed superficial cells with dysplastic tumor suspicious of hamartoma.[5] Another patient had transitional cell carcinoma of the bladder.[6] Isolated bladder hamartomas, including invasive hamartomas, have shown no evidence of recurrence or malignant potential after partial cystectomy.[12]
General experience with bladder hamartomas is limited, but patients who have undergone tumor resection are advised to undergo long-term periodic cystoscopy as surveillance for recurrence.[12]
Footnotes
Informed Consent: Written informed consent was obtained from patient’s family who participated in this case.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - N.A.S.; Design - N.A.S.; Supervision - A.R.A.; Resources - A.A.; Materials - E.M.A.; Data Collection and/or Processing - A.A.; Analysis and/or Interpretation - E.M.A.; Literature Search - N.A.S.; Writing Manuscript - N.A.S.; Critical Review - A.R.A.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Ota T, Kawai K, Hattori K, Uchida K, Akaza H, Harada M. Hamartoma of the urinary bladder. Int J Urol. 1999;6:211–4. doi: 10.1046/j.1442-2042.1999.06434.x. http://dx.doi.org/10.1046/j.1442-2042.1999.06434.x. [DOI] [PubMed] [Google Scholar]
- 2.Davis TA. Hamartoma of the urinary bladder. Northwest Med. 1949;48:182–5. [PubMed] [Google Scholar]
- 3.McCallion WA, Herron BM, Keane PF. Bladder hamartoma. Br J Urol. 1993;72:382–3. doi: 10.1111/j.1464-410x.1993.tb00741.x. http://dx.doi.org/10.1111/j.1464-410X.1993.tb00741.x. [DOI] [PubMed] [Google Scholar]
- 4.Adam A, Gayaparsad K, Engelbrecht MJ, Moshokoa EM. Bladder hamartoma: a unique cause of urinary retention in a child with Goldenhar syndrome. Saudi J Kidney Dis Transpl. 2013;24:89–92. doi: 10.4103/1319-2442.106296. http://dx.doi.org/10.4103/1319-2442.106296. [DOI] [PubMed] [Google Scholar]
- 5.Romanelli R, Borghesi MR. Two unusual tumors of the urinary bladder. Pathologica. 1987;79:641–5. [PubMed] [Google Scholar]
- 6.Hauser H, Ody B, Plojoux O, Wettstein P. Radiological findings in multiple hamartoma syndrome (Cowden disease): a report of three cases. Radiology. 1980;137:317–23. doi: 10.1148/radiology.137.2.7433661. http://dx.doi.org/10.1148/radiology.137.2.7433661. [DOI] [PubMed] [Google Scholar]
- 7.Keating MA, Young RH, Lillehei CW, Retik AB. Hamartoma of the bladder in a 4-year-old girl with hamartomatous polyps of the gastrointestinal tract. J Urol. 1987;138:366–9. doi: 10.1016/s0022-5347(17)43148-x. [DOI] [PubMed] [Google Scholar]
- 8.Williams MP, Ibrahim SK, Rickwood AM. Hamartoma of the urinary bladder in an infant with Beckwith-Wiedemann syndrome. Br J Urol. 1990;65:106–7. doi: 10.1111/j.1464-410x.1990.tb14671.x. http://dx.doi.org/10.1111/j.1464-410X.1990.tb14671.x. [DOI] [PubMed] [Google Scholar]
- 9.Borski AA. Hamartoma of the bladder. J Urol. 1970;104:718–9. doi: 10.1016/s0022-5347(17)61819-6. [DOI] [PubMed] [Google Scholar]
- 10.Park C, Kim H, Lee YB, Song JM, Ro JY. Hamartoma of the urachal remnant. Arch Pathol Lab Med. 1989;113:1393–5. [PubMed] [Google Scholar]
- 11.Krege S, Kropfl D, Brenneke HJ. Hamartoma polyps of the urethra. Urologe A. 1992;31:315–6. [PubMed] [Google Scholar]
- 12.Brancatelli G, Midiri M, Sparacia G, Martino R, Rizzo G, Lagalla R. Hamartoma of the urinary bladder: case report and review of the literature. Eur Radiol. 1999;9:42–4. doi: 10.1007/s003300050624. http://dx.doi.org/10.1007/s003300050624. [DOI] [PubMed] [Google Scholar]


