Abstract
Social stigma is common among men who have sex with men (MSM) across Sub-Saharan Africa, and may influence risks for HIV and sexually transmitted infections (STIs) via its association with depression. We conducted a cross-sectional study of 530 MSM in Lesotho accrued via respondent-driven sampling. Using generalized structural equation models we examined associations between stigma, social capital, and depression with condom use and testing positive for HIV/STIs. Depression was positively associated with social stigma experienced or perceived as a result of being MSM. In contrast, increasing levels of social cohesion were negatively associated with depression. Social stigma was associated with testing positive for HIV; however, this association did not appear to be mediated by depression or condom use. These data suggest a need for integrated HIV and mental health care that addresses stigma and discrimination and facilitates positive social support for MSM.
Keywords: Depression, social stigma, MSM, HIV, Africa
Introduction
There is increasing evidence that the prevalence of depression among men who have sex with men (MSM) is higher than that of non-MSM in many parts of the world, with studies citing discrimination, stigma, and minority stress as potential contributing factors (1-7). Moreover, studies also suggest that the lack of social support, feelings of isolation, and frequent stressful life events are contributors to adverse mental health conditions (8-10). For example, MSM may experience discrimination across multiple aspects of day-to-day life such as school, work, and accessing healthcare, which can contribute to chronic stress and internalized homophobia (6). Internalized homophobia, or self-stigma, may further facilitate psychological distress (6).
In southern Africa, where the prevalence of screening positive for depression among MSM ranges 44-58% (1, 11, 12), homoprejudice (anti-homosexual responses towards gays and lesbians) may play a major role in influencing depression because homosexuality is heavily stigmatized and in some cases criminalized (13, 14). Studies have consistently demonstrated a high prevalence of homoprejudice, with over 20% of MSM perceiving or experiencing various types of stigma in Malawi (15), 44% experiencing stigma in Swaziland (12), 76% experiencing at least one form of discrimination in Lesotho (16), and up to 40% experiencing at least one discrimination event in Malawi, Botswana, and Namibia (17, 18). However, there is still much to be learned about the consequences of stigma on psychological outcomes for African MSM.
In addition to depression, HIV remains an important public health issue across Sub-Saharan Africa especially given the broadly generalized HIV epidemics of Southern and Eastern Africa. Within these widespread HIV epidemics, there have been consistent epidemiologic studies highlighting the importance of key populations such as MSM and their unmet HIV prevention, treatment, and care needs (13, 19, 20). Moreover, risks for other sexually transmitted infections (STIs) such as syphilis are also of concern, with a prevalence of active syphilis infections of up to 5.3% (15, 21-24) among MSM in parts of southern Africa. As a result, recent efforts to reduce the spread of HIV/STIs among MSM in this region have called for a better understanding of HIV/STI correlates among these men.
Previous studies have linked HIV/STIs with sexual risk behaviors such as inconsistent condom use for anal intercourse and multiple and concurrent sexual partnerships (22, 25). However, although sexual behavior change is an important consideration for HIV/STIs, the epidemic of HIV among MSM is driven substantially by other factors including the social and structural factors that underlie high risk sexual practices (26). For example, stigma and discrimination affecting MSM can impact psychosocial determinants, which may influence behavior by inhibiting the ability of MSM to think or act in ways promoting good health (27). In particular, depression is thought to increase risk for HIV by decreasing self-efficacy and increasing sexual risk behaviors such as unprotected anal intercourse (11, 28, 29) and by affecting the desire or ability of MSM to engage in health care (30).
In contrast, social capital may improve mental health and reduce HIV risk behaviors by increasing resources or encouraging individuals to seek care (31, 32). Although it has many definitions, Woolcock & Narayan define social capital as “the norms and networks that enable people to act collectively.” (33). In particular, “bonding” social capital is social capital that exists within a group that has similar characteristics, such as MSM (33). In addition, “cognitive” social capital consists of the individual's perceptions of the trustworthiness of other people and institutions, as well as the norms around working together to solve problems (34-36). Both forms may have an impact on the mental health and HIV risk behavior of MSM.
The objective of these analyses is to describe the association between screening positive for depression and the stigma, discrimination, and social capital of MSM in Lesotho, a small lower middle income nation that is wholly surrounded by South Africa and has a high adult HIV prevalence (23% in 2012) (37). In Lesotho, male homosexual acts were only recently legalized in 2012 and sodomy is still prohibited as a common-law offense (14). In addition, the analyses described here aim to characterize the association between receiving a positive depression screen and condom use, as well as prevalent infections for HIV or other STIs. Given the limited study of HIV among MSM in Lesotho and in particular the relationship of HIV with depression and mental health, findings may inform comprehensive HIV prevention services.
Methods
Study Population and Design
Cross-sectional data were analyzed from 530 MSM recruited at two study sites in Maseru (n=318) and Maputsoe (n=212), Lesotho. MSM at both sites were eligible to participate if they were aged 18 years or older, assigned male sex at birth, and reported having receptive or insertive anal intercourse with another man in the past 12 months. In addition, participants were required to have lived in Lesotho for the past 3 months, to be capable of providing informed consent, and to understand English, Sesotho, or both languages. All eligible participants provided informed oral consent prior to completing the questionnaire and serological testing. This study was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board and the Lesotho National Health Research Ethics Committee.
Participants were recruited using respondent-driven sampling (RDS) (38, 39), which is a peer-driven chain-referral sampling method useful for reaching hidden populations such as MSM. Out of 10 initial seeds in Maseru, 9 recruited participants, and out of 12 initial seeds in Maputsoe 7 recruited participants. Thirteen waves of recruitment were reached in Maseru and 17 in Maputsoe. Participants were reimbursed the equivalent of approximately 5 USD for their time and travel to the study site. In addition, recruiters were compensated the equivalent of 2 USD for each eligible participant they recruited into the study.
Data Collection and Key Measures
Data were collected from February – September, 2014. During the study visit, trained interviewers administered a structured questionnaire including modules on demographics, stigma and discrimination, depression, social capital (e.g., social cohesion), HIV-related knowledge and behaviors, and STI/HIV diagnoses. To assess recent STI diagnoses, participants were asked if they had been told by a doctor or healthcare provider that they have an STI in the last 12 months, including genital ulcerative diseases such as syphilis, gonorrhea, chlamydia and blood borne viruses such as herpes simplex virus and hepatitis B and C virus. To assess condom use, participants were asked how often in the past 30 days condoms were used when having anal sex with a male partner. Response options were dichotomized to “any” vs “no” unprotected sex.
After completing the questionnaire, participants were tested for HIV [Determine Rapid Test, Alere, USA] and syphilis [Unigold Rapid Test, Trinity, Ireland] via whole blood samples collected by trained nurse counselors. National testing guidelines were followed for both HIV and syphilis testing and free treatment was offered for participants who were found to be positive for active syphilis. Participants who tested positive for HIV were referred to treatment and care services during post-test counseling, which were available at the same location as the study site.
Depression
A positive depression screen was defined as a Patient Health Questionnaire (PHQ-9) (40) score of 10 or greater. The PHQ-9 measures the frequency of depression symptoms within the past two weeks. This scale has been used previously in Sub-Saharan African populations (41, 42) and had good internal consistency in our study sample (Cronbach's alpha = 0.83) (43).
Social and healthcare stigma
Social stigma experienced or perceived as a result of being MSM was measured by asking participants a series of questions regarding how they have been treated by family, friends, and other members of society (Table 1). Stigma experiences with healthcare were measured in a similar manner. These measures have been used in previous studies conducted in Sub-Saharan Africa (15-18). Items were assessed for their association with depression both individually and cumulatively by using the sum of the total number of “yes” responses.
Table 1. Measurement of stigma and social cohesion.
| Items | Properties | |||
|---|---|---|---|---|
|
|
||||
| Mean (SD) | Median | Range | Alpha | |
|
|
||||
| Social stigma | -- | -- | -- | -- |
| Have you ever felt excluded from family gatherings because you have sex with men or because of your gender identity? | ||||
| Have you ever felt that family members have made discriminatory remarks or gossiped about you because you have sex with men or because of your gender identity? | ||||
| Have you ever felt rejected by your friends because you have sex with men or because of your gender identity? | ||||
| Have you ever felt that the police refused to protect you because you have sex with men? | ||||
| Have you ever felt scared to walk around in public places because you have sex with men or because of your gender identity? | ||||
| Has someone ever verbally harassed you and you felt it was because you have sex with men or because of your gender identity? | ||||
| Has someone ever blackmailed you because you have sex with men or because of your gender identity? | ||||
| Has someone ever physically hurt you (pushed, shoved, slapped, hit, kicked, choked or otherwise physically hurt you) [AND] Do you believe any of these experiences of physical violence was/were related to the fact that you have sex with men and/or your gender identity? | ||||
| Has anyone ever said discriminatory things about homosexuality in your presence without knowing you have sex with other men? | ||||
| Healthcare stigma | -- | -- | -- | -- |
| Have you ever felt afraid to go to healthcare services because you worry someone may learn you have sex with men? | ||||
| Have you ever avoided going to healthcare services because you worry someone may learn you have sex with men? | ||||
| Have you ever felt that you were not treated well in a health center because someone knew that you have sex with men? | ||||
| Have you ever heard healthcare providers gossiping about you (talking about you) because you have sex with men or because of your gender identity? | ||||
| Social cohesion (scale) | 23 (7) | 24 | 0 - 32 | 0.85 |
| You can count on other men who have sex with men if you need to borrow money. | ||||
| You can count on other men who have sex with men to accompany you to the doctor or hospital. | ||||
| You can count on other men who have sex with men if you need to talk about your problems. | ||||
| You can count on other men who have sex with men if you need somewhere to stay. | ||||
| You can count on other men who have sex with men to help you find other partners. | ||||
| You can count on other men who have sex with men to support the use of condoms. | ||||
| The group of men who have sex with men with whom you work is a group that is integrated into the larger community. | ||||
| You can trust the majority of other men who have sex with men living in your area. | ||||
| (Response options: 0 - Strongly disagree, 1- disagree, 2 - neutral, 3 - agree, or 4 - strongly agree) | ||||
Social capital
Social capital was measured using a social cohesion scale, which was modified from the World Bank's Social Capital Tool (34). Social cohesion focused on cognitive social capital within the MSM community, with items in Table 1 being summed to create a scale with scores ranging from 0 – 32.
Statistical Analyses
For the purpose of these analyses, three people did not answer questions pertaining to the PHQ-9 and were excluded. Because we combined data from two separate study sites in order to maximize the number of positive depression screens, no adjustments for RDS sampling methods were made (44). Chi-square tests were used to compare the prevalence of depression among different socio-demographic groups, and logistic regression models were used to assess the bivariate associations between depression and positive and negative social constructs. In addition, a single generalized structural equation model (GSEM) conducted using Stata 13.1 (College Station, Texas) was used to identify associations of social constructs with screening positive for depression, as well as associations of social constructs and depression with condom use, self-reported past 12-month STI diagnoses, and testing positive for syphilis. A separate GSEM was used to characterize the associations of social constructs and depression with testing positive for HIV, among those who had no previous knowledge of living with HIV (note that no participants reported previous knowledge of having syphilis). All modeled relationships (or “paths”) adjusted for age, gender identity, income, education, marital status, and study site. These potential confounders were identified a priori based on previous literature (12, 45, 46).
In both GSEMs, we started with a saturated model and obtained the final model by deleting all paths with p-value >0.10. However, in order to describe the associations of interest (i.e., associations with depression or potentially mediated by depression), the following paths were kept regardless of their p-values: Stigma and depression, social cohesion and depression, history of HIV and depression, depression and condom use, and depression and STI/HIV diagnosis. The final model is depicted in Figure 1.
Figure 1.
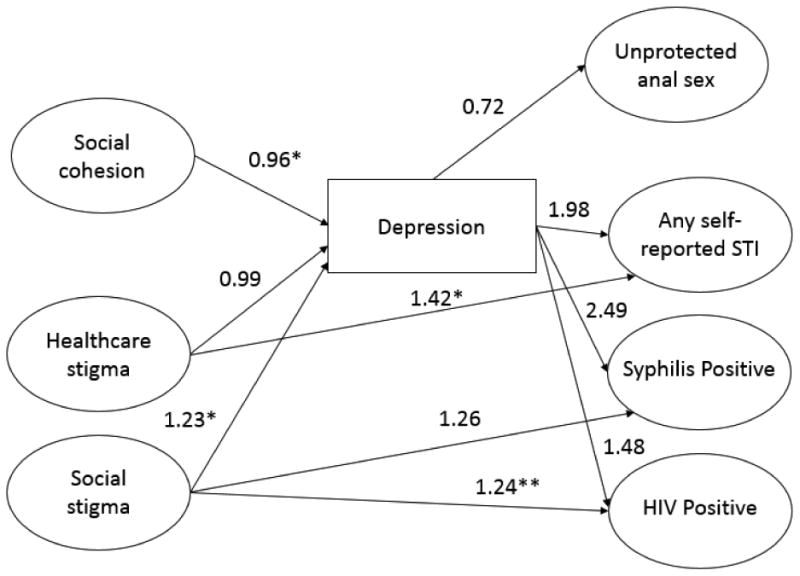
Final GSEM indicating adjusted odds ratios for associations between social capital, stigma, depression, and STIs/HIV among MSM in Lesotho (n=527). *p<0.05; **p<0.01
Results
Study Sample
Of the 527 participants who completed the PHQ-9, 84 (16%) screened positive for depression (Table 2). Overall, participants were young with more than one-third aged 18-21 years. All participants reported being assigned male sex at birth; however, 8% identified as a woman or “other” gender (includes intersex). A little more than half had at least a high school education and the majority (79%) were single/never married. About 13% had prior knowledge of living with HIV and 33% tested positive for HIV at the study visit. In addition, almost 10% self-reported an STI within the past 12 months and 5% tested positive for syphilis.
Table 2. Prevalence of depression screen result by socio-demographic characteristics and STI/HIV diagnosis.
| Characteristics | Total | Depressed | Not depressed | χ2 | p-value | |||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| n | % | n | % | n | % | |||
| Total | 527 | 100.0 | 84 | 15.9 | 443 | 84.1 | -- | -- |
| Age, in years | ||||||||
| 18-21 | 193 | 36.6 | 24 | 12.4 | 169 | 87.6 | 3.03 | 0.22 |
| 22-27 | 214 | 40.6 | 40 | 18.7 | 174 | 81.3 | ||
| 28+ | 120 | 22.8 | 20 | 16.7 | 100 | 83.3 | ||
| Gender identity | ||||||||
| Man | 484 | 91.8 | 71 | 14.7 | 413 | 85.3 | 7.14 | 0.008** |
| Woman/Other | 43 | 8.2 | 13 | 30.2 | 30 | 69.8 | ||
| Monthly income, in maloti | ||||||||
| 0-400 | 218 | 41.5 | 28 | 12.8 | 190 | 87.2 | 2.90 | 0.23 |
| 401-1000 | 116 | 22.1 | 20 | 17.2 | 96 | 82.8 | ||
| 1001+ | 191 | 36.4 | 36 | 18.9 | 155 | 81.2 | ||
| Education completed | ||||||||
| Primary school or less | 98 | 18.6 | 16 | 16.3 | 82 | 83.7 | 0.73 | 0.69 |
| Secondary school | 132 | 25.1 | 18 | 13.6 | 114 | 86.4 | ||
| High school or higher | 296 | 56.3 | 50 | 16.9 | 246 | 83.1 | ||
| Marital status | ||||||||
| Single/never married | 415 | 79.0 | 68 | 16.4 | 347 | 83.6 | 0.25 | 0.61 |
| Ever married or cohabited | 111 | 21.0 | 16 | 14.4 | 95 | 85.6 | ||
| Study site | ||||||||
| Maputsoe | 211 | 40.0 | 17 | 8.1 | 194 | 91.9 | 16.32 | <0.001*** |
| Maseru | 316 | 60.0 | 67 | 21.2 | 249 | 78.8 | ||
| Prior knowledge of living with HIV | ||||||||
| No | 458 | 86.9 | 69 | 15.1 | 389 | 84.9 | 1.99 | 0.16 |
| Yes | 69 | 13.1 | 15 | 21.7 | 54 | 78.3 | ||
| Self-reported STI, past 12 months | ||||||||
| No | 474 | 90.5 | 67 | 14.4 | 407 | 85.9 | 8.62 | 0.003** |
| Yes | 50 | 9.5 | 15 | 30.0 | 35 | 70.0 | ||
| Tested positive for HIV | ||||||||
| No | 352 | 67.2 | 47 | 13.4 | 305 | 86.7 | 5.71 | 0.02* |
| Yes | 172 | 32.8 | 37 | 21.5 | 135 | 78.5 | ||
| Tested positive for syphilis | ||||||||
| No | 497 | 94.9 | 76 | 15.3 | 421 | 84.7 | 3.91 | 0.048* |
| Yes | 27 | 5.2 | 8 | 29.6 | 19 | 70.4 | ||
p<0.05;
p<0.01;
p<0.001
P-values derived by Pearson Chi-Square Test
Percentages may not sum to 100 due to rounding
Associations with Screening Positive for Depression
Those who screened positive for depression were similar in terms of demographic characteristics to those who screened negative. However, more individuals screened positive in the capital city of Maseru as compared with Maputsoe (21% vs. 8%, p<0.01) and depression prevalence was higher among those who identified as a woman or “other” as opposed to identifying as a man (30% vs. 15%, p<0.01). Depression prevalence was also higher among those who self-reported an STI (30% vs. 14%, p<0.01), tested positive for HIV (22% vs. 13%, p<0.05), and tested positive for syphilis (30% vs. 15%, p<0.05). However, depression was not found to be more prevalent among those with prior knowledge of living with HIV (22% vs. 15%, p=0.16).
In the bivariate analyses, depression was positively associated with feeling rejected by friends as a result of one's sexual orientation (Odds Ratio [OR]=2.98, 95% Confidence Interval [CI]=1.78, 5.00) (Table 3). In addition, depression was positively associated with hearing discriminatory remarks made about homosexuality (OR=2.36, 95% CI=1.18, 4.72), feeling scared to walk around in public places (OR=2.35, 95% CI=1.33, 4.15), being blackmailed (OR=1.96, 95% CI=1.15, 3.35), as well as with increasing report of social stigma items (OR=1.32, 95% CI=1.16, 1.52). For healthcare-related stigma, depression was associated with report of hearing a healthcare worker gossip about one's sexual orientation (OR=2.79, 95% CI=1.09, 7.13) and increasing number of healthcare-related stigma items (OR=1.36, 95% CI=1.03, 1.81). However, individuals with increasing social cohesion scores were less likely to screen positive for depression (OR=0.96, 95% CI=0.93, 0.99).
Table 3. Bivariate associations with screening positive for depression, among MSM in Lesotho.
| Characteristics | Proportion Participants with Depression (n/N) | Odds Ratio | p-value | |
|---|---|---|---|---|
|
|
||||
| OR | 95% CI | |||
| Social stigma due to being an MSM | ||||
| Excluded by family | 7/38 | 1.22 | 0.52, 2.87 | 0.65 |
| Gossiped about by family | 15/71 | 1.52 | 0.81, 2.84 | 0.19 |
| Felt rejected by friends | 30/100 | 2.98*** | 1.78, 5.00 | <0.001*** |
| Did not feel protected by police | 5/18 | 2.09 | 0.72, 6.02 | 0.17 |
| Felt scared in public | 21/76 | 2.35** | 1.33, 4.15 | 0.003** |
| Verbally harassed | 40/212 | 1.43 | 0.90, 2.29 | 0.13 |
| Blackmailed | 24/99 | 1.96* | 1.15, 3.35 | 0.013* |
| Physically hurt | 12/49 | 1.88 | 0.93, 3.77 | 0.08 |
| Heard discriminatory remarks about MSM | 74/410 | 2.36* | 1.18, 4.72 | 0.02* |
| Total social stigma items | -- | 1.32*** | 1.16, 1.52 | <0.001*** |
| Healthcare stigma as a result of being an MSM | ||||
| Afraid to seek services | 14/63 | 1.61 | 0.84, 3.07 | 0.15 |
| Avoided services | 10/42 | 1.74 | 0.82, 3.68 | 0.15 |
| Not treated well | 5/19 | 1.94 | 0.68, 5.54 | 0.22 |
| Healthcare worker gossiped | 7/21 | 2.79* | 1.09, 7.13 | 0.03* |
| Total healthcare stigma items | -- | 1.36* | 1.03, 1.81 | 0.03* |
| Social cohesion score | -- | 0.96** | 0.93, 0.99 | 0.009** |
p<0.05;
p<0.01;
p<0.001
After adjusting for potential confounders in the GSEM, total number of experienced or perceived social stigma items was positively associated with screening positive for depression (Adjusted Odds Ratio [aOR]=1.23, 95% CI=1.04, 1.45) (Table 4). In addition, increasing social cohesion score was negatively associated with screening positive for depression (aOR=0.96, 95% CI 0.92, 0.99).
Table 4. Adjusted associations with depression from GSEM, among MSM in Lesotho.
| Outcome variable | n | Explanatory variable | Adjusted Odds Ratio | ||
|---|---|---|---|---|---|
|
| |||||
| AOR | 95% CI | p-value | |||
| Depression | 84 | Total social stigma items | 1.23 | 1.04, 1.45 | 0.02* |
| Total healthcare stigma items | 0.99 | 0.71, 1.38 | 0.97 | ||
| Social cohesion score | 0.96 | 0.92, 0.99 | 0.01* | ||
| Self-reported living with HIV | 1.31 | 0.63, 2.72 | 0.47 | ||
| Tested positive for syphilis | 27 | Depressed | 2.49 | 0.95, 6.53 | 0.06 |
| Total social stigma items | 1.26 | 0.99, 1.61 | 0.06 | ||
| Unprotected anal sex with male partner, past 30 days | 136 | Depressed | 0.72 | 0.38, 1.39 | 0.33 |
| Self-reported diagnosis with any STI, past 12 months | 50 | Depressed | 1.98 | 0.99, 3.97 | 0.054 |
| Total healthcare stigma items | 1.42 | 1.01, 1.99 | 0.04* | ||
| Positive for HIV, among those never told they had HIVa | 103 | Depressed | 1.48 | 0.79, 2.75 | 0.22 |
| Total social stigma items | 1.24 | 1.06, 1.44 | 0.007** | ||
p<0.05;
p<0.01
A separate GSEM was run in order to limit the sample to those who were never told that they have HIV.
Note: Each modeled relationship adjusts for age, gender identity, income, marital status, education, and study site
Associations with STI/HIV Outcomes
In the GSEM, depression was marginally associated with testing positive for syphilis among those who had never been told they had syphilis (aOR=2.49, 95% CI=0.95, 6.53). In addition, depression was marginally associated with any self-reported STIs in the past 12 months (aOR=1.98, 95% CI=0.99, 3.97). However, there was no association found between depression and unprotected anal sex in the past 30 days (aOR=0.72, 95% CI=0.38, 1.39).
Although depression was not significantly associated with testing positive for HIV (aOR=1.48, 95% CI=0.79, 2.75), there was an association between social stigma and testing positive for HIV (aOR=1.24, 95% CI=1.06, 1.44) among those who were not previously told that they have HIV. Social stigma was also marginally associated with testing positive for syphilis (aOR=1.26, 95% CI=0.99, 1.61). Finally, healthcare stigma was positively associated with self-reporting an STI (aOR=1.42 95% CI=1.01, 1.99).
Discussion
In this sample of MSM, depression was associated with the report of several individual and cumulative experiences of perceived or enacted stigma. Previous literature has indicated that systemic stigma among MSM within a cultural context and its resulting associations with depression can negatively influence quality of life and ability to make healthy decisions, including decisions regarding HIV preventive behaviors or initiation and adherence to HIV treatment (47-50). Of the social stigma indicators in our data, the strongest associations with depression were observed with ever experiencing friend rejection, hearing discriminatory remarks about MSM, feeling scared to walk around in public, and being blackmailed. All of these experiences were perceived as being due to one's sexual orientation or gender identity. These findings highlight the need to address systemic and cultural discrimination towards MSM, which could also help to reduce the psychological impediments to HIV/STI prevention and care.
The results of the bivariate analysis suggest that depression is elevated among individuals in Lesotho who were assigned male sex at birth but do not identify with the male gender. Perhaps the experience of stigma, abuse, and discrimination is more extreme among these individuals because they may represent clearer examples of violation of the traditional male gender role (30, 51). For example, recent studies in the U.S. indicate that experience of stigma and adverse mental health conditions, as well as HIV prevalence, are higher among transgender populations (52-55). However, additional research including qualitative studies are necessary to better explore the mental health and HIV/STI prevention needs of transgender and intersex populations in Lesotho and other Sub-Saharan African countries.
In addition to addressing stigma, another potential way to improve psychological factors is to facilitate or allow for the growth of social capital among MSM. In particular, we found that social cohesion, which included several measures of cognitive social capital particular to the MSM community, was negatively associated with depression. These findings are consistent with a study of older adults in Sweden and Finland, which suggested an inverse association between interpersonal trust in friends and neighbors with depression (56). Other studies have similarly linked cognitive social capital with more positive health outcomes, including better self-rated health, more life satisfaction, and lower risk for HIV infection among non-MSM (57-59).
There are several methods by which social capital can improve mental health among MSM in Sub-Saharan Africa, although research regarding social capital interventions to promote health is still growing. First, peer-based social capital interventions can be used to build or strengthen ties within or between groups. For example, social ties can be built or strengthened within MSM networks or between MSM and different community groups of varying power and authority, such as police or healthcare workers (60). Although we only measured cognitive social capital within MSM networks, bonds outside of MSM networks may be especially important for marginalized groups of MSM because they could facilitate access to HIV/STI prevention and care as well as a safer, more comfortable living environment. In particular, the Internet may serve as a promising social capital intervention delivery mechanism given its anonymity and increasing popularity and use among MSM for the purpose of finding sexual partners (61, 62). Finally, support group interventions could be used to improve psychological functioning outcomes and improvements in depressive symptoms (63-65), social support and integration (60), and HIV- or sexual-orientation-related stigma (66, 67).
Previous research assessing the relationship between depression and risk for HIV/STIs has indicated mixed findings (68, 69). However, several studies conducted among MSM in the U.S. have suggested that depression is associated with increased sexual risk behaviors and risk for HIV acquisition (29, 47, 70, 71). Studies conducted among MSM in Sub-Saharan Africa are limited but provide additional evidence for the association between depression and risk for HIV/STIs (11, 28, 42). Our findings are somewhat consistent with the concept that depression is linked to higher risk for syphilis and self-reported STIs, although these associations were not statistically significant (p=0.06 and p=0.05, respectively). In addition, a primary proposed mechanism by which depression might influence risk for HIV/STIs is through increased sexual risk behaviors such as inconsistent condom use. However, we did not detect an association between past 30-day condom use for anal sex and depression. This could be partially due to the varying time frame of the measurements, because depression was assessed within a very recent time period (past 2 weeks). Alternatively, perhaps depression influences other STI risk behaviors for which we did not have study data, such as increasing acts of unprotected oral sex with multiple sexual partners.
Further, we did not find evidence for an indirect association of social stigma with testing positive for HIV or syphilis through depression. Instead, increasing social stigma was directly associated with testing positive for HIV. This suggests that there could be other mechanisms besides depression through which social stigma influences HIV risk, which should be explored in future studies. In addition, healthcare stigma was directly associated with self-reporting an STI but was not associated with depression. One potential explanation is that healthcare stigma dissuades MSM from getting the STI-related prevention services they need (72-74). Alternatively, it is possible that participants experience greater healthcare stigma as a result of having an STI. Despite mixed results, depression remains an important consideration for comprehensive HIV/STI-related care given that the prevalence of depression was higher among those who tested positive for HIV or syphilis as compared with those who did not test positive.
The findings of this study should be interpreted in light of several limitations. Measures were self-reported and may be subject to recall bias or social desirability bias. For example, participants may be more likely to underreport HIV or depressive symptoms due to the sensitive nature of these topics. In addition, data were cross-sectional and therefore we cannot provide evidence for temporality or causality in the associations between depression and social constructs or depression and HIV/STI risk. However, we measured the associations between depression and laboratory-diagnosed syphilis/HIV among participants who had never been told that they have had that particular disease. Laboratory tests were conducted at the end of the study visit after completion of the questionnaire. This suggests that among these individuals, depression was not linked to previous knowledge of either syphilis or HIV. In addition, the PHQ-9 measured symptoms of depression within the past two weeks whereas social stigma was assessed over the participant's lifetime, further suggesting that experience of stigma may have preceded depression. An additional limitation is that this study does not provide any evidence for a mechanism by which depression might increase risk for HIV/STIs because depression was not found to be associated with condom use. Finally, in order to maximize the number of depression cases, data were pooled from two study sites within Lesotho. Because of this, we were unable to adjust for RDS methods. However, there is a lack of consensus regarding how to handle RDS data in multivariable regressions or when primary objectives are to test associations between variables (44). Further, we examined the study sites individually (as well as with and without RDS-adjustment) to check for heterogeneity of effect estimates and found no significant differences that would have challenged the interpretation of our results.
These findings regarding the associations between social stigma and depression among MSM in this southern African country are consistent with studies of MSM from other parts of the world (42, 75, 76). Experiences of stigma and discrimination among MSM in Lesotho are highly prevalent and associated with screening positive for depression. In addition, social and healthcare related stigma may facilitate risk for HIV/STIs through other mechanisms besides depression. This calls to attention the need for integrated HIV care that addresses social stigma and facilitates positive social support for MSM in these communities.
Acknowledgments
We would like to acknowledge and thank the Lesotho LGBT community for their participation and effective mobilization to disseminate messages about this study. We also wish to thank the study staff and interviewers who worked on this project at personal risk, including disclosure of sexual orientation to their families or communities. The Lesotho Ministry of Health was instrumental in the oversight, direction, and supervision of the study, and we are grateful for the incredible government engagement and ownership of this work. We would especially like to thank Dr. Limpho Maile, Dr. Mosilinyane Letsie, Tsietso Mot'soane, David Mothabeng, Puleng Ramphalla-Phatela, and Dr. Kyaw Thin for their invaluable support and input. This study was funded by the U.S. Agency for International Development (USAID, AID-674-A-00-00001), and implemented by Population Services International/Lesotho (PSI). From PSI, we would like to thank Dwan Dixon, Pierre Loup-Lesage, and Brian Pedersen who provided invaluable support and guidance. Finally, from USAID, we thank David Brown, Todd Koppenhaver, and Diana Acosta who provided oversight and technical assistance for the project. Additional support was provided by Johns Hopkins University Center for AIDS Research (P30AI094189) and the American Foundation for AIDS Research.
References
- 1.Stoloff K, Joska JA, Feast D, et al. A description of common mental disorders in men who have sex with men (MSM) referred for assessment and intervention at an MSM clinic in Cape Town, South Africa. AIDS and behavior. 2013;17(Suppl 1):S77–81. doi: 10.1007/s10461-013-0430-3. Epub 2013/03/28. [DOI] [PubMed] [Google Scholar]
- 2.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological bulletin. 2003;129(5):674–97. doi: 10.1037/0033-2909.129.5.674. Epub 2003/09/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cochran SD, Mays VM, Sullivan JG. Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. Journal of consulting and clinical psychology. 2003;71(1):53–61. doi: 10.1037//0022-006x.71.1.53. Epub 2003/02/27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gilman SE, Cochran SD, Mays VM, Hughes M, Ostrow D, Kessler RC. Risk of psychiatric disorders among individuals reporting same-sex sexual partners in the National Comorbidity Survey. American journal of public health. 2001;91(6):933–9. doi: 10.2105/ajph.91.6.933. Epub 2001/06/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mays VM, Cochran SD. Mental health correlates of perceived discrimination among lesbian, gay, and bisexual adults in the United States. American journal of public health. 2001;91(11):1869–76. doi: 10.2105/ajph.91.11.1869. Epub 2001/10/31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meyer IH. Minority stress and mental health in gay men. Journal of health and social behavior. 1995;36(1):38–56. Epub 1995/03/01. [PubMed] [Google Scholar]
- 7.Herek GM, Garnets LD. Sexual orientation and mental health. Annual review of clinical psychology. 2007;3:353–75. doi: 10.1146/annurev.clinpsy.3.022806.091510. Epub 2007/08/25. [DOI] [PubMed] [Google Scholar]
- 8.Yan H, Wong FY, Zheng T, et al. Social support and depressive symptoms among ‘money’ boys and general men who have sex with men in Shanghai, China. Sexual health. 2014;11(3):285–7. doi: 10.1071/SH14017. Epub 2014/06/13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lackner JB, Joseph JG, Ostrow DG, et al. A longitudinal study of psychological distress in a cohort of gay men. Effects of social support and coping strategies. The Journal of nervous and mental disease. 1993;181(1):4–12. doi: 10.1097/00005053-199301000-00002. Epub 1993/01/01. [DOI] [PubMed] [Google Scholar]
- 10.Ross MW. The relationship between life events and mental health in homosexual men. Journal of clinical psychology. 1990;46(4):402–11. doi: 10.1002/1097-4679(199007)46:4<402::aid-jclp2270460405>3.0.co;2-q. Epub 1990/07/01. [DOI] [PubMed] [Google Scholar]
- 11.Tucker A, Liht J, de Swardt G, et al. Homophobic stigma, depression, self-efficacy and unprotected anal intercourse for peri-urban township men who have sex with men in Cape Town, South Africa: a cross-sectional association model. AIDS care. 2014;26(7):882–9. doi: 10.1080/09540121.2013.859652. Epub 2013/12/04. [DOI] [PubMed] [Google Scholar]
- 12.Risher K, Adams D, Sithole B, et al. Sexual stigma and discrimination as barriers to seeking appropriate healthcare among men who have sex with men in Swaziland. Journal of the International AIDS Society. 2013;16(3 Suppl 2):18715. doi: 10.7448/IAS.16.3.18715. Epub 2013/11/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith AD, Tapsoba P, Peshu N, Sanders EJ, Jaffe HW. Men who have sex with men and HIV/AIDS in sub-Saharan Africa. Lancet. 2009;374(9687):416–22. doi: 10.1016/S0140-6736(09)61118-1. Epub 2009/07/21. [DOI] [PubMed] [Google Scholar]
- 14.Itaborahy LP, Zhu J. State-sponsored homophobia. A world survey of laws: Criminalisation, protection and recognition of same-sex love. International Lesbian Gay Bisexual Trans and Intersex Association. 2014 May; [Google Scholar]
- 15.Wirtz AL, Jumbe V, Trapence G, et al. HIV among men who have sex with men in Malawi: elucidating HIV prevalence and correlates of infection to inform HIV prevention. Journal of the International AIDS Society. 2013;16(Suppl 3):18742. doi: 10.7448/IAS.16.4.18742. Epub 2014/01/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baral S, Adams D, Lebona J, et al. A cross-sectional assessment of population demographics, HIV risks and human rights contexts among men who have sex with men in Lesotho. Journal of the International AIDS Society. 2011;14:36. doi: 10.1186/1758-2652-14-36. Epub 2011/07/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fay H, Baral SD, Trapence G, et al. Stigma, health care access, and HIV knowledge among men who have sex with men in Malawi, Namibia, and Botswana. AIDS and behavior. 2011;15(6):1088–97. doi: 10.1007/s10461-010-9861-2. Epub 2010/12/15. [DOI] [PubMed] [Google Scholar]
- 18.Baral S, Trapence G, Motimedi F, et al. HIV prevalence, risks for HIV infection, and human rights among men who have sex with men (MSM) in Malawi, Namibia, and Botswana. PloS one. 2009;4(3):e4997. doi: 10.1371/journal.pone.0004997. Epub 2009/03/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000-2006: a systematic review. PLoS medicine. 2007;4(12):e339. doi: 10.1371/journal.pmed.0040339. Epub 2007/12/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.26th Meeting of the UNAIDS Programme Coordinating Board. Reducing HIV transmission among men who have sex with men and transgender people. Geneva, Switzerland: Jun, 2010. [Google Scholar]
- 21.Ross MW, Nyoni J, Ahaneku HO, Mbwambo J, McClelland RS, McCurdy SA. High HIV seroprevalence, rectal STIs and risky sexual behaviour in men who have sex with men in Dar es Salaam and Tanga, Tanzania. BMJ open. 2014;4(8):e006175. doi: 10.1136/bmjopen-2014-006175. Epub 2014/08/30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park JN, Papworth E, Kassegne S, et al. HIV prevalence and factors associated with HIV infection among men who have sex with men in Cameroon. Journal of the International AIDS Society. 2013;16(Suppl 3):18752. doi: 10.7448/IAS.16.4.18752. Epub 2014/01/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wade AS, Kane CT, Diallo PA, et al. HIV infection and sexually transmitted infections among men who have sex with men in Senegal. AIDS (London, England) 2005;19(18):2133–40. doi: 10.1097/01.aids.0000194128.97640.07. Epub 2005/11/15. [DOI] [PubMed] [Google Scholar]
- 24.Johnston LG, Holman A, Dahoma M, et al. HIV risk and the overlap of injecting drug use and high-risk sexual behaviours among men who have sex with men in Zanzibar (Unguja), Tanzania. The International journal on drug policy. 2010;21(6):485–92. doi: 10.1016/j.drugpo.2010.06.001. Epub 2010/07/20. [DOI] [PubMed] [Google Scholar]
- 25.Muraguri N, Temmerman M, Geibel S. A decade of research involving men who have sex with men in sub-Saharan Africa: current knowledge and future directions. SAHARA J : journal of Social Aspects of HIV/AIDS Research Alliance / SAHARA, Human Sciences Research Council. 2012;9(3):137–47. doi: 10.1080/17290376.2012.744176. Epub 2012/12/15. [DOI] [PubMed] [Google Scholar]
- 26.Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC public health. 2013;13:482. doi: 10.1186/1471-2458-13-482. Epub 2013/05/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beyrer C, Sullivan PS, Sanchez J, et al. A call to action for comprehensive HIV services for men who have sex with men. Lancet. 2012;380(9839):424–38. doi: 10.1016/S0140-6736(12)61022-8. Epub 2012/07/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tucker A, Liht J, de Swardt G, et al. An exploration into the role of depression and self-efficacy on township men who have sex with men's ability to engage in safer sexual practices. AIDS care. 2013;25(10):1227–35. doi: 10.1080/09540121.2013.764383. Epub 2013/02/08. [DOI] [PubMed] [Google Scholar]
- 29.Alvy LM, McKirnan DJ, Mansergh G, et al. Depression is associated with sexual risk among men who have sex with men, but is mediated by cognitive escape and self-efficacy. AIDS and behavior. 2011;15(6):1171–9. doi: 10.1007/s10461-010-9678-z. Epub 2010/03/11. [DOI] [PubMed] [Google Scholar]
- 30.Mayer KH, Wheeler DP, Bekker LG, et al. Overcoming biological, behavioral, and structural vulnerabilities: new directions in research to decrease HIV transmission in men who have sex with men. Journal of acquired immune deficiency syndromes (1999) 2013;63(Suppl 2):S161–7. doi: 10.1097/QAI.0b013e318298700e. Epub 2013/08/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pronyk PM, Harpham T, Morison LA, et al. Is social capital associated with HIV risk in rural South Africa? Social science & medicine (1982) 2008;66(9):1999–2010. doi: 10.1016/j.socscimed.2008.01.023. Epub 2008/02/27. [DOI] [PubMed] [Google Scholar]
- 32.Vogel DL, Wade NG, Wester SR, Larson L, Hackler AH. Seeking help from a mental health professional: the influence of one's social network. Journal of clinical psychology. 2007;63(3):233–45. doi: 10.1002/jclp.20345. Epub 2007/01/11. [DOI] [PubMed] [Google Scholar]
- 33.Woolcock M, Narayan D. Social Capital: Implications for Development Theory, Research, and Policy. World Bank Research Observer. 2000;15(2):225–49. [Google Scholar]
- 34.Grootaert C, Narayan D, Jones V, Woolcock M. Integrated questionnaire for the measurement of social capital (SC-IQ) Washington, DC: World Bank Social Capital Thematic Group; 2003. [Google Scholar]
- 35.Krishna A, Uphoff N. Mapping and Measuring Social Capital: A Conceptual and Empirical Study of Collective Action for Conserving and Developing Watersheds in Rajasthan, India. Social Capital Initiative Working Paper Series. 1999;13 [Google Scholar]
- 36.Putnam R. Bowling alone: The collapse and revival of American community. New York: Simon & Schuster; 2000. [Google Scholar]
- 37.UNICEF. [December 18, 2014];Lesotho: Statistics. 2013 Available from: http://www.unicef.org/infobycountry/lesotho_statistics.html.
- 38.Heckathorn DD. Respondent-Driven Sampling: A New Approach to the Study of Hidden Populations. Social Problems. 1997;44(2):174–99. [Google Scholar]
- 39.Heckathorn DD. Respondent-driven sampling II: Deriving valid population estimates from chain-referral samples of hidden populations. Social Problems. 2002;49(1):11–34. [Google Scholar]
- 40.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of general internal medicine. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. Epub 2001/09/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Adewuya AO, Ola BA, Afolabi OO. Validity of the patient health questionnaire (PHQ-9) as a screening tool for depression amongst Nigerian university students. Journal of affective disorders. 2006;96(1-2):89–93. doi: 10.1016/j.jad.2006.05.021. Epub 2006/07/22. [DOI] [PubMed] [Google Scholar]
- 42.Anderson AM, Ross MW, Nyoni JE, McCurdy SA. High prevalence of stigma-related abuse among a sample of men who have sex with men in Tanzania: implications for HIV prevention. AIDS care. 2014:1–8. doi: 10.1080/09540121.2014.951597. Epub 2014/08/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cronbach L. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. [Google Scholar]
- 44.Johnston LG, Malekinejad M, Kendall C, Iuppa IM, Rutherford GW. Implementation challenges to using respondent-driven sampling methodology for HIV biological and behavioral surveillance: field experiences in international settings. AIDS and behavior. 2008;12(4 Suppl):S131–41. doi: 10.1007/s10461-008-9413-1. Epub 2008/06/07. [DOI] [PubMed] [Google Scholar]
- 45.Fonner VA, Kerrigan D, Mnisi Z, Ketende S, Kennedy CE, Baral S. Social cohesion, social participation, and HIV related risk among female sex workers in Swaziland. PloS one. 2014;9(1):e87527. doi: 10.1371/journal.pone.0087527. Epub 2014/02/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ha H, Risser JM, Ross MW, Huynh NT, Nguyen HT. Homosexuality-related stigma and sexual risk behaviors among men who have sex with men in hanoi, Vietnam. Archives of sexual behavior. 2015;44(2):349–56. doi: 10.1007/s10508-014-0450-8. Epub 2015/01/27. [DOI] [PubMed] [Google Scholar]
- 47.Fendrich M, Avci O, Johnson TP, Mackesy-Amiti ME. Depression, substance use and HIV risk in a probability sample of men who have sex with men. Addictive behaviors. 2013;38(3):1715–8. doi: 10.1016/j.addbeh.2012.09.005. Epub 2012/12/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hatzenbuehler ML, O'Cleirigh C, Mayer KH, Mimiaga MJ, Safren SA. Prospective associations between HIV-related stigma, transmission risk behaviors, and adverse mental health outcomes in men who have sex with men. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 2011;42(2):227–34. doi: 10.1007/s12160-011-9275-z. Epub 2011/05/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hou WL, Chen CE, Liu HY, et al. Mediating effects of social support on depression and quality of life among patients with HIV infection in Taiwan. AIDS care. 2014;26(8):996–1003. doi: 10.1080/09540121.2013.873764. Epub 2014/01/16. [DOI] [PubMed] [Google Scholar]
- 50.Ammassari A, Trotta MP, Murri R, et al. Correlates and predictors of adherence to highly active antiretroviral therapy: overview of published literature. Journal of acquired immune deficiency syndromes (1999) 2002;31(Suppl 3):S123–7. doi: 10.1097/00126334-200212153-00007. Epub 2003/02/04. [DOI] [PubMed] [Google Scholar]
- 51.Beyrer C. LGBT Africa: a social justice movement emerges in the era of HIV. SAHARA J : journal of Social Aspects of HIV/AIDS Research Alliance / SAHARA, Human Sciences Research Council. 2012;9(3):177–9. doi: 10.1080/17290376.2012.743813. Epub 2012/12/15. [DOI] [PubMed] [Google Scholar]
- 52.Grant JM, Mottet LA, Tanis J. Injustice at every turn: A report of the national transgender survey. Washington, D.C: National Center for Transgender Equality; 2011. [Google Scholar]
- 53.Flentje A, Heck NC, Sorensen JL. Characteristics of transgender individuals entering substance abuse treatment. Addictive behaviors. 2014;39(5):969–75. doi: 10.1016/j.addbeh.2014.01.011. Epub 2014/02/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS and behavior. 2008;12(1):1–17. doi: 10.1007/s10461-007-9299-3. Epub 2007/08/19. [DOI] [PubMed] [Google Scholar]
- 55.Baral SD, Poteat T, Stromdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. The Lancet Infectious diseases. 2013;13(3):214–22. doi: 10.1016/S1473-3099(12)70315-8. Epub 2012/12/25. [DOI] [PubMed] [Google Scholar]
- 56.Forsman AK, Nyqvist F, Schierenbeck I, Gustafson Y, Wahlbeck K. Structural and cognitive social capital and depression among older adults in two Nordic regions. Aging & mental health. 2012;16(6):771–9. doi: 10.1080/13607863.2012.667784. Epub 2012/04/11. [DOI] [PubMed] [Google Scholar]
- 57.Barefoot JC, Maynard KE, Beckham JC, Brummett BH, Hooker K, Siegler IC. Trust, health, and longevity. Journal of behavioral medicine. 1998;21(6):517–26. doi: 10.1023/a:1018792528008. Epub 1999/01/19. [DOI] [PubMed] [Google Scholar]
- 58.Frumence G, Emmelin M, Eriksson M, et al. Access to social capital and risk of HIV infection in Bukoba urban district, Kagera region, Tanzania. Archives of public health = Archives belges de sante publique. 2014;72(1):38. doi: 10.1186/2049-3258-72-38. Epub 2015/02/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rose R. How much does social capital add to individual health? A survey study of Russians. Social science & medicine (1982) 2000;51(9):1421–35. doi: 10.1016/s0277-9536(00)00106-4. Epub 2000/10/19. [DOI] [PubMed] [Google Scholar]
- 60.Pronyk PM, Harpham T, Busza J, et al. Can social capital be intentionally generated? a randomized trial from rural South Africa. Social science & medicine (1982) 2008;67(10):1559–70. doi: 10.1016/j.socscimed.2008.07.022. Epub 2008/09/06. [DOI] [PubMed] [Google Scholar]
- 61.Benotsch EG, Kalichman S, Cage M. Men who have met sex partners via the Internet: prevalence, predictors, and implications for HIV prevention. Archives of sexual behavior. 2002;31(2):177–83. doi: 10.1023/a:1014739203657. Epub 2002/04/27. [DOI] [PubMed] [Google Scholar]
- 62.Garofalo R, Herrick A, Mustanski BS, Donenberg GR. Tip of the Iceberg: young men who have sex with men, the Internet, and HIV risk. American journal of public health. 2007;97(6):1113–7. doi: 10.2105/AJPH.2005.075630. Epub 2007/04/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Verduin F, Smid GE, Wind TR, Scholte WF. In search of links between social capital, mental health and sociotherapy: A longitudinal study in Rwanda. Social science & medicine (1982) 2014;121C:1–9. doi: 10.1016/j.socscimed.2014.09.054. Epub 2014/10/12. [DOI] [PubMed] [Google Scholar]
- 64.Petersen I, Hanass Hancock J, Bhana A, Govender K. A group-based counselling intervention for depression comorbid with HIV/AIDS using a task shifting approach in South Africa: a randomized controlled pilot study. Journal of affective disorders. 2014;158:78–84. doi: 10.1016/j.jad.2014.02.013. Epub 2014/03/25. [DOI] [PubMed] [Google Scholar]
- 65.Cao W, Li L, Zhou X, Zhou C. Social capital and depression: evidence from urban elderly in China. Aging & mental health. 2014:1–12. doi: 10.1080/13607863.2014.948805. Epub 2014/08/27. [DOI] [PubMed] [Google Scholar]
- 66.Sivaram S, Zelaya C, Srikrishnan AK, et al. Associations between social capital and HIV stigma in Chennai, India: considerations for prevention intervention design. AIDS education and prevention : official publication of the International Society for AIDS Education. 2009;21(3):233–50. doi: 10.1521/aeap.2009.21.3.233. Epub 2009/06/13. [DOI] [PubMed] [Google Scholar]
- 67.Kertzner RM, Meyer IH, Frost DM, Stirratt MJ. Social and psychological well-being in lesbians, gay men, and bisexuals: the effects of race, gender, age, and sexual identity. The American journal of orthopsychiatry. 2009;79(4):500–10. doi: 10.1037/a0016848. Epub 2010/01/27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Crepaz N, Marks G. Are negative affective states associated with HIV sexual risk behaviors? A meta-analytic review. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2001;20(4):291–9. doi: 10.1037//0278-6133.20.4.291. Epub 2001/08/23. [DOI] [PubMed] [Google Scholar]
- 69.Mustanski BS, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. Journal of sex research. 2011;48(2-3):218–53. doi: 10.1080/00224499.2011.558645. Epub 2011/03/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Houston E, Sandfort T, Dolezal C, Carballo-Dieguez A. Depressive symptoms among MSM who engage in bareback sex: does mood matter? AIDS and behavior. 2012;16(8):2209–15. doi: 10.1007/s10461-012-0156-7. Epub 2012/02/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.O'Cleirigh C, Newcomb ME, Mayer KH, Skeer M, Traeger L, Safren SA. Moderate levels of depression predict sexual transmission risk in HIV-infected MSM: a longitudinal analysis of data from six sites involved in a “prevention for positives” study. AIDS and behavior. 2013;17(5):1764–9. doi: 10.1007/s10461-013-0462-8. Epub 2013/04/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Eaton LA, Driffin DD, Kegler C, et al. The role of stigma and medical mistrust in the routine health care engagement of black men who have sex with men. American journal of public health. 2015;105(2):e75–82. doi: 10.2105/AJPH.2014.302322. Epub 2014/12/19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kennedy CE, Baral SD, Fielding-Miller R, et al. “They are human beings, they are Swazi”: intersecting stigmas and the positive health, dignity and prevention needs of HIV-positive men who have sex with men in Swaziland. Journal of the International AIDS Society. 2013;16(Suppl 3):18749. doi: 10.7448/IAS.16.4.18749. Epub 2014/01/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pyun T, Santos GM, Arreola S, et al. Internalized homophobia and reduced HIV testing among men who have sex with men in China. Asia-Pacific journal of public health / Asia-Pacific Academic Consortium for Public Health. 2014;26(2):118–25. doi: 10.1177/1010539514524434. Epub 2014/02/21. [DOI] [PubMed] [Google Scholar]
- 75.Wohl AR, Galvan FH, Carlos JA, et al. A comparison of MSM stigma, HIV stigma and depression in HIV-positive Latino and African American men who have sex with men (MSM) AIDS and behavior. 2013;17(4):1454–64. doi: 10.1007/s10461-012-0385-9. Epub 2012/12/19. [DOI] [PubMed] [Google Scholar]
- 76.Adebajo SB, Eluwa GI, Allman D, Myers T, Ahonsi BA. Prevalence of internalized homophobia and HIV associated risks among men who have sex with men in Nigeria. African journal of reproductive health. 2012;16(4):21–8. Epub 2013/03/01. [PubMed] [Google Scholar]


