Abstract
Background
Variation in hospitalization rates have been described for decades, yet little is known about variation in emergency department (ED) admission rates across clinical conditions. We sought to describe variation in ED risk-standardized admission rates (RSAR) and the consistency between condition-specific ED admission rates within hospitals.
Methods
Cross-sectional analysis of the 2009 National Emergency Department Sample, an all-payer administrative claims dataset. We identify the 15 most frequently admitted conditions using Clinical Classification Software. To identify conditions with the highest ED RSAR variation we compared both the ratio of the 75th percentile to the 25th percentile hospital and coefficient of variation between conditions. We calculate Spearman correlation coefficients to assess within-hospital correlation of condition-specific ED RSARs.
Results
Of 21,885,845 adult ED visits, 4,470,105 (20%) resulted in admission. Among the 15 most frequently admitted conditions, the five with the highest magnitude of variation were: mood disorders (ratio of 75th:25th percentile, 6.97; coefficient of variation, 0.81), nonspecific chest pain (2.68; 0.66), skin and soft tissue infections (1.82; 0.51), urinary tract infections (1.58; 0.43) and COPD (1.57; 0.33). For these five conditions, the within-hospital RSAR correlations between each pair of conditions were greater than 0.4, except for mood disorders, which was poorly correlated with all other conditions (r<0.3).
Conclusions
There is significant condition-specific variation in ED admission rates across US hospitals. This variation appears to be consistent between conditions with high variation within hospitals.
Keywords: Emergency Department, Hospital Admission, Efficiency Measurement
Background
The decision to admit a patient to the hospital requires judgment about the marginal benefit of inpatient care. While some patients clearly require treatment and monitoring only available in the hospital setting, for many patients the decision is not clear and made on an individual basis to select those who can be reasonably treated as outpatients.(1) Moreover, clinical practice guidelines offer few explicit criteria regarding hospital admission. Clinical ambiguity as well as factors beyond a patient’s health status often impact hospitalization decisions.(2) In emergency departments (EDs) across the US, the primary portal for hospital admission, the impact of this ambiguity is revealed every day.(3–5) Better understanding of this variation is essential to provide targets for interventions and benchmarks for performance for providers and policymakers seeking to improve the efficiency of acute care delivery.
Recent work has shown nearly threefold variation in overall rates of hospital admission from hospital EDs, but we know little about whether this variation is consistent across conditions within EDs or varies based on condition.(6, 7) Prior work studying variations in hospitalization rates have designated many hospitalizations as “discretionary” because of substantial variation in patterns of care. (8–10) However, previous studies have not compared variation between conditions, which would focus provider and policymaker efforts on the conditions for which admissions are most discretionary. Nor has prior work assessed the consistency of hospital-level variation across conditions evaluated in the ED to assess whether each hospital’s practices optimize admissions decisions. In an era of Accountable Care Organizations and various incentives to improve hospital efficiency, hospitals and policymakers are seeking tools to measure and manage hospital admissions and better align the intensity of medical resource expenditures with the needs of individual patients.(11)
We hypothesized that select conditions would demonstrate substantial variation in ED admission rates despite adjustment for both patient factors that contribute to differences in hospital case mix as well as traditional hospital factors such as teaching status, ED volume, or geographic location. Our objective was to describe condition-specific, risk-standardized variation in ED admission rates in order to identify conditions with the highest degree of variation, or potentially discretionary conditions. To further understand the unique ED admission patterns within each hospital, we also explored the degree to which within-hospital condition-specific, risk-standardized admission rates are correlated. We sought to explore these objectives using a large, national sample of ED visits. In order to permit national use of these findings, we built upon the hospital profiling methodology used for the publicly reported federal government outcome measures.
Methods
Design and Dataset
We performed a cross-sectional analysis of the 2009 National Emergency Department Sample (NEDS). The NEDS is assembled by the Agency for Healthcare Research and Quality (AHRQ) and is the largest all–payer ED database in the US and includes over 25 million records from 964 hospitals, which represent an approximately 20% stratified sample of US hospital-based EDs. Hospital survey weights available in the dataset were not utilized for this study, as national estimates are not described. Patient data in the NEDS are de-identified, and therefore all analyses are conducted at the visit-level and cannot account for patients potentially being included in the analysis more than once. This study was deemed exempt from IRB review by the Yale University Human Research Protection Program.
Study Sample and Data Definitions
We included all adult ED visits in 2009 in the study sample. We excluded all visits with ED disposition of “died in ED,” “left against medical advice,” or whose ED disposition was “unknown” when disposition decisions could not be reliably evaluated. Patient level information available in the NEDS included age, sex, payer/insurance status, median income of patient’s zip code and ICD-9 principal and secondary discharge diagnoses. The AHRQ Clinical Classification Software (CCS) was used to group each visit’s principal ED or hospital discharge diagnosis into meaningful clinical conditions. The CCS schema is a mutually exclusive set of 275 clinical condition categories that includes over 14,000 ICD-9 diagnoses and 3,900 ICD-9 procedure codes. (12) Because the NEDS does not include a patient’s chief complaint or reason for ED visitation, all visits are grouped based on the discharge diagnosis which is most likely to represent the final diagnosis upon ED or hospital discharge. We also applied the Charlson Comorbidity Index to all secondary diagnoses to enable patient comorbidity adjustment. (13) In addition, hospital-level information available in the NEDS included: teaching status, hospital region, trauma center designation, ownership status and urban/rural designation from the American Hospital Association Annual Survey. We additionally created a hospital level variable based on annual ED visit volume for stratification purposes that classified EDs as Small (<10,000 annual ED visits), Medium (10,000–50,000 visits) or Large (>50,000 visits).
Outcomes
The primary outcome was the ED risk-standardized admission ratio (RSAR) for each clinical condition. We defined admission as patients with disposition from ED of “admitted as an inpatient to this hospital” or “transfer to short-term hospital” due to the large proportion of patients transferred from smaller EDs for acute care hospital and specialty services. We included transfers as part of the outcome because all require additional acute services beyond a usual ED visit, most result in hospital admission at the receiving hospital, and finally to enable more comparisons between smaller EDs and larger referral EDs. Patients admitted to observation status are not considered inpatient hospitalizations due to limitations of the NEDS.
Risk Standardized Admission Ratio
We identified the 15 clinical conditions (based on CCS) most frequently admitted to the hospital based on the annual number of admissions from the ED. We analyzed the top 15 conditions in order to ensure that each hospital had a sufficient number of visits to permit statistical comparisons and to ensure that our work identified conditions with the potential to impact hospital care. We utilized hierarchical generalized linear models (HGLM) to calculate the independent, condition-specific RSAR for each hospital. The RSAR was created to enable hospital-level profiling of ED disposition decisions using the same methodology as used by the Centers for Medicare and Medicaid Services for publicly reported hospital readmission and mortality measures.(14–16) Only hospitals with a minimum of 25 ED visits specific to each clinical condition were included to ensure stability of estimates in accordance with current publicly reported measures.(17) To account for differences in patient characteristics the RSAR is adjusted for patient age, sex, income and insurance status. Income was determined using the patient’s zip code-based median household income quartile: $1 to $38,999, $39,000 to $47,999, $48,000 to $62,999 and $63,000 or more. Insurance status was categorized into five payer categories: private, Medicare, Medicaid, self-pay plus no charge, and other. Clinical comorbidities were accounted for using the Charlson Comorbidity Index, which has been previously validated in both inpatient and ED administrative claims datasets.(18, 19) The use of HGLM allows for adjustment of patient characteristics and a random hospital intercept to account for clustering of observations. (16)
The RSAR was calculated as the ratio of the number of predicted admissions to the number of expected admissions at a given hospital for each condition. The predicted number of admissions is based on the hospital’s observed case-mix, while the expected number of admissions is based on the average hospital’s performance with similar case-mix. In short, the RSAR allows for comparison of a given hospital’s case-mix specific admission rate to an average hospital’s admission rate with that same case-mix. Thus, a lower ratio (RSAR<1) indicates a lower-than-expected admission rate, and a higher ratio (RSAR>1) indicates a higher-than-expected admission rate.
Statistical Analysis
All analyses were conducted using SAS software version 9.3 (SAS Institute, Inc., Cary, North Carolina) and hierarchical logistic models were estimated using the GLIMMIX macro in SAS. Statistical significance was considered P<0.05.
Analysis of variation in emergency department admission rates
We constructed summary statistics using frequencies and proportions for categorical variables and means and medians with interquartile ranges (IQR) for continuous variables. We reported the sample unadjusted admission rate and hospital variance in the unadjusted admission rate for all 15 conditions. We reported hospital-level variation in the condition specific RSAR as medians and percentiles. To compare the magnitude of variation between conditions, we reported the ratio of the 75th percentile hospital to the 25th percentile hospital and the coefficient of variation for each condition-specific RSAR. The coefficient of variation, defined as the ratio of the standard deviation to the mean, was analyzed in addition to the ratio between the 75th and 25th percentile hospitals because it represents a normalized measure of dispersion that allows for the meaningful comparison of variation between conditions that have different mean admission rates. We also displayed condition-specific RSAR variation with the use of Turnip plots. We assessed model performance by calculating the area under the receiver operating characteristic curve to report C-statistics. The C-statistic is an indicator of the model’s discriminant ability to correctly classify those who have and have not been admitted to the hospital. We calculate C-statistics based on the observed admissions and the predicted probability.
Analysis of hospital predictors of variation
We sought to describe the association between hospital characteristics and condition-specific, ED RSAR to identify exogenous variables at the hospital-level that impact the measurement of admission rates. To evaluate this association, we selected the five conditions with the highest degree of variability, defined as the highest ratio between the 75th and 25th percentile hospitals and highest coefficient of variation, for further analysis. The five conditions with the highest ratio in RSAR between the 75th and 25th percentile hospitals also had the highest coefficient of variation. We included each hospital factor including: teaching status, urban/rural location, ownership, trauma center designation and regional location into the HGLM. We report the 80% Interval Odds Ratio (IOR-80) as a measure of association between hospital-level characteristics and condition-specific RSAR. The IOR-80 takes into account hospital-level residual variations and is considered a superior measure of hospital level effects versus the traditionally reported mean Odds Ratio in HGLM. (20) The IOR-80 is reported as an interval similar to the traditional mean OR; an IOR-80 of 1 indicates that the effect of the hospital characteristic is weak in comparison to the remaining residual heterogeneity between hospitals.
Within hospital RSAR Correlation
To examine the degree of association between hospitals’ condition specific RSAR, we report Spearman correlation coefficients comparing within hospital, condition-specific RSARs.
Sensitivity Analysis
To test the effect of including ED transfers on our outcome definition we performed the condition-specific analyses of RSAR variation including only same hospital admission as the outcome.
Results
Sample characteristics
In the 2009 NEDS 21,885,845 ED visits from 964 hospitals met our inclusion criteria. Of all hospitals, 42% were metropolitan non-teaching, 17% were metropolitan teaching, and 41% were located in non-metropolitan areas. The majority of hospitals were non-profit (60%), and non-trauma centers (82%). The median annual ED volume per hospital was 23,265 visits (IQR: 9,484, 42,509).
The median sample age was 44 years (IQR: 19, 61), and predominantly female (58%). Sample distributions of median zip code income and insurance status are described in Supplementary Table 1.
Unadjusted ED admission rate
Of all ED visits, 4,470,105 (20%) resulted in admission. Among all hospitals, the unadjusted median admission rate was 17.6%, ranging from 7.8% at the 5th percentile to 33% at the 95th percentile (IQR: 13% to 23%) (Table 1). The most frequently admitted condition was pneumonia (185,922 admissions per year); the 15 conditions most frequently admitted from the ED are shown in Table 2. Of these 15, septicemia, acute myocardial infarction and acute cerebrovascular disease had the highest hospital-level median admission rates and the lowest variation: septicemia (median 99.1%, IQR: 97.6% to 99.9%), acute myocardial infarction (median 98.5%, IQR: 94.7% to 99.8%), and cerebrovascular disease (median: 93.4%, IQR: 87.2% to 96.7%). The five conditions with the highest hospital-level variation in unadjusted admission rate were mood disorders (median: 21.1%, IQR: 5.8% to 51.8%), nonspecific chest pain (median: 17.7%, IQR: 10.7% to 30.1%), skin and subcutaneous tissue infections (median: 13.9%, IQR: 8.6% to 20.8%), urinary tract infections (median: 16.6%, IQR: 11.8% to 23.6%) and chronic obstructive pulmonary disease (COPD) (median: 32.9%, IQR: 22.4% to 46.0%).
Table 1.
Variation in Unadjusted Admission Rate of the 15 Most Frequently Admitted Conditions
| Clinical Condition1 | # of ED visits | # of Admissions | Median Admission Rate (IQR) (%) |
|---|---|---|---|
| All conditions | 21,885,845 | 4,470,105 | 17.59 (12.95, 23.38) |
| Pneumonia | 292,417 | 185,922 | 64.03(54.27, 73.68) |
| Congestive heart failure | 215,027 | 182,935 | 83.78(73.75,92.22) |
| Nonspecific chest pain | 832,426 | 157,928 | 17.64(10.72,30.05) |
| Septicemia | 159,902 | 155,957 | 99.11(97.61,99.86) |
| COPD and bronchiectasis | 387,784 | 135,128 | 32.85(22.38,46.01) |
| Cardiac dysrhythmias | 292,824 | 130,691 | 42.08(33.33,51.94) |
| Acute cerebrovascular disease | 124,116 | 114,593 | 93.44(87.23,96.67) |
| Acute myocardial infarction | 113,939 | 109,636 | 98.46(94.74,99.79) |
| Mood disorders | 243,106 | 109,458 | 21.11(5.81,51.76) |
| Urinary tract infections | 572,479 | 107,255 | 16.64(11.83,23.58) |
| Skin and subcutaneous tissue infections | 587,009 | 95,125 | 13.90(8.63,20.75) |
| Diabetes mellitus with complications | 160,320 | 89,789 | 53.23(41.25,63.15) |
| Coronary atherosclerosis and other heart disease | 112,119 | 88,382 | 79.59(67.93,90.32) |
| Fluid and electrolyte disorders | 170,276 | 78,029 | 45.00(32.95,57.01) |
| Biliary tract disease | 139,274 | 77,668 | 54.13(41.98,65.08) |
Clinical Conditions defined using AHRQ Clinical Classification Software
Table 2.
Variation in condition-specific, risk standardized admission ratio (RSAR) of 15 most frequently admitted conditions
| Condition | Interquartile Range | Ratio of 75th percentile to 25th percentile hospital | Coefficient of Variation | Hospitals included* | C statistic |
|---|---|---|---|---|---|
| Pneumonia | 0.88,1.09 | 1.24 | 0.17 | 902 | 0.87 |
| Congestive heart failure | 0.91,1.06 | 1.17 | 0.14 | 846 | 0.88 |
| Nonspecific chest pain | 0.59,1.58 | 2.68 | 0.66 | 942 | 0.82 |
| Septicemia | 0.99,1.01 | 1.02 | 0.06 | 672 | 0.90 |
| COPD and bronchiectasis | 0.77,1.21 | 1.56 | 0.33 | 899 | 0.87 |
| Cardiac dysrhythmias | 0.84,1.16 | 1.37 | 0.25 | 880 | 0.86 |
| Acute cerebrovascular disease | 0.95,1.03 | 1.08 | 0.09 | 735 | 0.81 |
| Acute myocardial infarction | 0.97,1.01 | 1.04 | 0.10 | 726 | 0.89 |
| Mood disorders | 0.32,2.24 | 6.95 | 0.81 | 713 | 0.83 |
| Urinary tract infections | 0.77,1.22 | 1.60 | 0.43 | 916 | 0.89 |
| Skin and subcutaneoustissue infections | 0.71,1.29 | 1.80 | 0.51 | 896 | 0.84 |
| Diabetes mellitus with complications | 0.83,1.14 | 1.38 | 0.24 | 809 | 0.80 |
| Coronary atherosclerosis and other heart disease | 0.85,1.10 | 1.30 | 0.18 | 728 | 0.77 |
| Fluid and electrolyte disorders | 0.80,1.19 | 1.49 | 0.28 | 865 | 0.82 |
| Biliary tract disease | 0.81,1.15 | 1.42 | 0.24 | 759 | 0.78 |
Exclusion of hospitals with fewer than 25 visits for each condition resulted in the most hospital (n=902) being included in the Pneumonia performance model and the lowest number of hospitals (n=672) being included in the Septicemia performance model.
Hospital level variation in Risk Standardized Admission Ratio
Figure 1 shows Turnip plots for each condition-specific RSAR. All 15 condition specific models had good discrimination with c-statistics above 0.77 (range: 0.77–0.90). (Table 2) Of the 15 most frequently admitted conditions, the five conditions with the highest variation, as defined by both the interquartile ratio and the coefficient of variation, were: mood disorders (ratio of 75th:25th percentile, 6.97; coefficient of variation, 0.81), nonspecific chest pain (2.68; 0.66), skin and soft tissue infections (1.82; 0.51), urinary tract infections (1.58; 0.43) and COPD (1.57; 0.33). In comparison, the conditions with the least amount of variation were septicemia (1.02; 0.06), acute myocardial infarction (1.04; 0.10), acute cerebrovascular disease (1.08, 0.09), and CHF (1.17, 0.14). Sensitivity analyses that did not include transfers in hospital admissions identified the same five conditions as having the highest degree of variation.
Figure 1. Variation in condition-specific, risk-standardized emergency department admission ratios (RSAR).
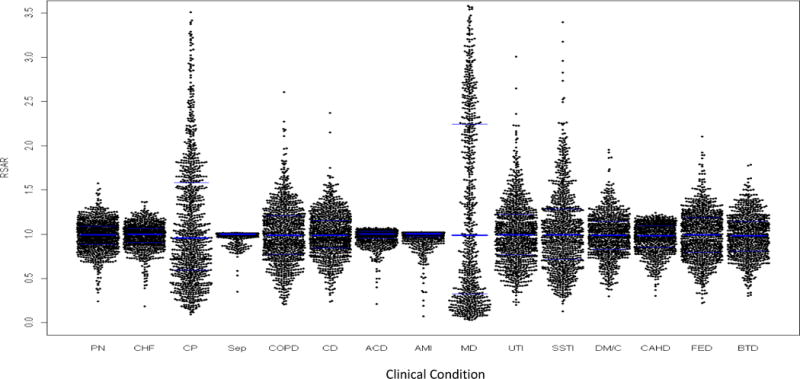
Abbreviations: PN: pneumonia; CHF: congestive heart failure; CP: nonspecific chest pain; Sep: septicemia; COPD: Chronic obstructive pulmonary disease and bronchiectasis; CD: cardiac dysrhythmias; ACD: acute cerebrovascular disease; AMI: acute myocardial infarction; MD: mood disorder; UTI: urinary tract infections; SSTI: skin and subcutaneous tissue infections; DM/C: diabetes mellitus with complications; CAHD: Coronary atherosclerotic heart disease; FED: fluids and electrolyte disturbances; BTD: biliary tract disease.
Footnote: RSAR (Condition-specific emergency department Risk Standardized Admission Ratio)
Hospital characteristics associated with the RSAR
In Table 3, we evaluated the association between each hospital characteristic and condition-specific variation for the five conditions with the most variability in RSAR. Across these five conditions, there was no hospital characteristic with a significant interval odds ratio, indicating that traditional hospital characteristics do not explain between-hospital variations in comparison to the residual hospital-level variation due to unmeasured factors. The large Interval Odds Ratios indicate that for each hospital-level factor the association for each condition-specific RSAR is minimal when accounting for residual hospital-level variation.
Table 3.
Association between hospital characteristics and RSAR for five conditions with high admission variation
| Hospital characteristic | Hospitals (%) | Mood disorder IOR-80 |
Non-specific chest pain IOR-80 |
Skin and subcutaneous tissue infections IOR-80 |
Urinary tract infections IOR-80 |
COPD and bronchiectasis IOR-80 |
|---|---|---|---|---|---|---|
| Teaching Status | ||||||
| Non metropolitan | 40.77 | (REF) | (REF) | (REF) | (REF) | (REF) |
| Metropolitan non-teaching | 42.01 | 0.06 – 27.15 | 0.17 – 7.52 | 0.33 – 5.54 | 0.30 – 4.73 | 0.34 – 6.43 |
| Metropolitan-teaching | 17.22 | 0.10 – 45.24 | 0.14 – 6.02 | 0.44 – 7.43 | 0.39 – 6.18 | 0.35 – 6.66 |
| Ownership Status | ||||||
| Private | 23.55 | (REF) | (REF) | (REF) | (REF) | (REF) |
| Government | 16.08 | 0.04 – 18.35 | 0.11 – 4.63 | 0.19 – 3.33 | 0.21 – 3.42 | 0.16 – 3.07 |
| Non profit | 60.37 | 0.08 – 35.93 | 0.10 – 4.37 | 0.26 – 4.67 | 0.24 – 4.02 | 0.21 – 4.22 |
| Urban/Rural Location | ||||||
| Metropolitan | 59.24 | (REF) | (REF) | (REF) | (REF) | (REF) |
| Micropolitan | 40.76 | 0.03 – 14.52 | 0.14 – 6.18 | 0.16 – 2.80 | 0.19 – 3.10 | 0.15 – 2.90 |
| Trauma Status | ||||||
| Trauma | 17.53 | (REF) | (REF) | (REF) | (REF) | (REF) |
| Non-trauma | 82.47 | 0.03 – 12.16 | 0.19 – 8.15 | 0.18 – 3.19 | 0.19 – 3.13 | 0.18 – 3.60 |
| Region | ||||||
| West | 17.63 | (REF) | (REF) | (REF) | (REF) | (REF) |
| Northeast | 13.59 | 0.14 – 55.14 | 0.19 – 8.36 | 0.32 – 5.81 | 0.34 – 5.51 | 0.40 – 7.57 |
| Midwest | 30.50 | 0.18 – 70.82 | 0.17 – 7.39 | 0.31 – 5.61 | 0.33 – 5.33 | 0.30 – 5.81 |
| South | 38.28 | 0.10 – 41.22 | 0.20 – 8.60 | 0.28 – 4.98 | 0.32 – 5.13 | 0.36 – 6.85 |
| ED volume | ||||||
| <10,000 | 26.24 | (REF) | (REF) | (REF) | (REF) | (REF) |
| 10,000–50,000 | 55.19 | 0.05 – 21.59 | 0.15 – 6.37 | 0.29 – 5.09 | 0.26 – 4.22 | 0.33 – 6.43 |
| >50,000 | 18.57 | 0.08 – 37.53 | 0.13 – 5.62 | 0.38 – 6.71 | 0.32 – 5.15 | 0.38 – 7.26 |
Degree of association within hospitals for the condition-specific RSAR
The within-hospital correlation between condition-specific RSARs for the five conditions with the highest variability is shown in Table 4. All correlations were statistically significant (p< 0.001). Skin and subcutaneous tissue infections and urinary tract infections had the highest within-hospital correlation (r=0.74). The within-hospital correlation between the Mood Disorders RSAR and other highly variable conditions was the weakest, with all correlations <0.3.
Table 4.
Within-hospital correlations in RSAR for five conditions with high admission variation
| Correlation coefficient (95% CI)
| |||||
|---|---|---|---|---|---|
| Condition | Mood disorder | Non-specific chest pain | Skin and subcutaneous tissue infections | Urinary tract infections | COPD and bronchiectasis |
| Mood disorder | 1 | ||||
| Non-specific chest pain | 0.2086 (0.1373,0.2778) | 1 | |||
| Skin and subcutaneous tissue infections | 0.2552 (0.1852,0.3226) | 0.3894 (0.3323,0.4436) |
1 | ||
| Urinary tract infections | 0.2731 (0.2037,0.3397) |
0.4128 (0.3570,.4652) |
0.7425 (0.7116,0.7706) |
1 | |
| COPD and bronchiectasis | 0.2096 (0.1381,0.2789) |
0.3938 (0.3371,0.4477) |
0.6191 (0.5767,0.6582) |
0.6907 (0.6547,0.7235) |
1 |
Note: All p values<0.0001
Discussion
We found wide variation in ED admission patterns across a national sample of US hospitals. Among the 15 conditions that most frequently resulted in a hospital admission, we identified mood disorders, chest pain, skin and soft tissue infections, urinary tract infections and COPD as five conditions with markedly higher hospital-level variation in ED admission rates even after adjustment for numerous patient-level characteristics and hospital case-mix. Condition-specific variation in ED admission rates for these select conditions were three to fivefold higher than for conditions such as pneumonia or congestive heart failure, which are the focus of most condition-specific quality assessment programs used by CMS. This magnitude of condition-specific variation carries numerous implications for clinicians making hospital admissions decisions, hospitals seeking to understand acute care delivery patterns, and policymakers attempting to identify targets for hospital efficiency accountability measures.
The wide variation in hospital admission from the ED for these conditions, based on the ED to which a patient arrives irrespective of the patient or hospital characteristics, suggests that physicians and hospitals are applying different criteria in the decision to admit these patients. Not surprisingly, conditions such as sepsis, acute myocardial infarctions and stroke had virtually no risk-standardized admission rate variation between EDs as these time-sensitive illnesses that necessitate hospital admission. In contrast, none of the five conditions we identified as having high variation in risk-standardized admission rates necessarily require admission. All five conditions lack either clinical practice guidelines or established clinical pathways to incorporate patient preferences and outpatient access into hospitalization decisions. This lack of clear guidance reflects the diagnostic uncertainty associated with conditions such as chest pain and COPD, which could evolve into an acute myocardial infarction or respiratory failure, as well as the paucity of tools to risk-stratify infectious processes such as urinary tract infections and cellulitis, for which the decision to admit patients for IV antibiotics may reflect provider-level clinical practice variation, as has been demonstrated for pneumonia.(21) The clinical categories with higher variation are also more diagnostically ambiguous, which may reflect the need for more accessible diagnostic and prognostic capabilities for conditions such as chest pain in comparison to well defined clinical conditions such as an acute myocardial infarction for which little variation exists.
The substantial variation identified in ED admission rates for several conditions does not suggest a “correct” hospital-level rate for ED admission, but rather demonstrates the variability in practice between EDs across the country that cannot be accounted for by differences in the patient case-mix or structural differences between hospitals. We found that a hospital’s teaching status, location, ED volume and several other factors did not explain these differences between hospitals, suggesting that other factors may be a primarily responsible for this variation. This finding is in contrast to Pines et al who found that larger hospitals had higher all-cause admission rates(6). This difference may be due to our analysis of hospital characteristics on condition-specific rates and our statistical approach that utilized a hierarchical structure as well as the interval odds ratio as optimal for hospital-level profiling.
The consistent variation evidenced by high within-hospital correlations between condition-specific risk-standardized admission rates for urinary tract infections, skin infections and COPD suggests that unmeasured hospital practices common to all of these potentially discretionary conditions may drive variation. Previous work has demonstrated within-geography correlation in condition-specific hospitalization rates; more recent data has demonstrated within-hospital correlation for readmission rates. (10, 22) Our work extends these findings to the ED setting and suggests that this correlation may be explained by unmeasured hospital-level factors that cross all potentially discretionary conditions. These factors could include hospital bed availability, as has been suggested by Wennberg et al’s work regarding supply-sensitive utilization, or less studied factors such as local practice culture, admission processes and capacity of general medical services, and the availability of alternative care settings such as observation units. Hospital admission patterns may also be driven by a hospital’s location and associated community resources. As many US communities only have access to a single ED and hospital, admission rates may reflect the local community’s lack of social services or ambulatory clinics. Taken in conjunction with the lack of association found between any hospital factor and RSAR variation—these correlations demonstrate the need for hospitals seeking to provide population-level acute care to consider broad hospital processes in addition to condition-specific factors when designing interventions to improve the efficiency of hospital care. These interventions to reduce variation could include better chronic disease management programs or facilitating community support resources to reduce acute exacerbations or the use of alternatives to hospitalization such as observation care of rapid follow-up clinics.
Policymakers seeking to improve the quality and reduce the cost of hospital care delivery should interpret this condition-specific variation in ED RSAR as a potential target for future hospital efficiency. The National Quality Forum recently published a report that sought to identify twenty high-impact conditions for quality measurement in the Medicare program based on dimensions of cost, prevalence, improvability, variability and disparities.(23) Two conditions identified in this work–chest pain and COPD—closely mirror or fall within the top ten of this list and may represent ideal initial targets for the measurement of acute care efficiency. The development of future condition-specific measures of ED admission rates will also create common targets for providers and policymakers seeking to prioritize investments in outpatient and social services and reduce variation in hospitalization rates and healthcare costs.
Over two decades ago, Wennberg and colleagues reported condition-specific variation in hospitalization rates between two cities for pneumonia, heart failure, gastroenteritis, diabetes, cardiac arrhythmias and COPD.(9) Our work extends upon these observations by utilizing contemporary hospital profiling methods and evaluating modern acute care where gastroenteritis is largely managed in the outpatient setting, and where pneumonia shows considerably less variation in ED admission rates than other acute, medical conditions after risk-standardization. Translating this work into national measures of hospital efficiency, however, requires the ability to better distinguish underuse from the overuse of hospital admission. High variation may not imply healthcare overuse; previous work by Restuccia et al. showed no relationship between geographic hospitalization rates and inappropriate hospitalizations.(24) In addition, higher admission rates for higher-risk but diagnostically ambiguous conditions such as chest pain, which may represent an early acute myocardial infarction, may reflect lower risk tolerance due to local medicolegal climates or the need to compensate for limited access to outpatient specialty care. Before national policies can be implemented, future work is necessary to understand both whether this variation reflects the use of alternatives to hospitalization by some EDs or unexplained care patterns, and if this variation impacts downstream outcomes such as ED revisitation, hospital re-admission and patient-reported outcomes such as speed of recovery from acute illness.
In contrast to the consistent patterns of variation found for potentially discretionary medical conditions, patients with mood disorders demonstrated considerably greater variation in admission patterns that likely carry different policy implications. This may represent variable access to mental health resources between hospitals including both inpatient psychiatric facilities and intensive outpatient programs. EDs that are frequently burdened by overcrowding, particularly for patients with mental health needs, may be more likely to admit these patients to the hospital in order to create necessary ED capacity. It is also possible that our use of administrative claims data cannot capture the clinical information that may be the primary driver of hospitalization. Similarly, the within-hospital RSAR correlation between mood disorders and the other four potentially discretionary conditions was quite low, suggesting that factors driving ED admissions decisions for mood disorders are less likely be driven by unmeasured hospital-level factors, and more likely to reflect a combination of ED practice variability and local mental health care access. Measuring ED admission rates for mood disorders may in fact reflect community behavioral health performance, while measuring ED admission rates for medical conditions may be more suitable for hospital profiling.
These findings must be interpreted within the limitations of our study design. While the methods used to develop the condition-specific models for this analysis was built upon prior work endorsed by the National Quality Forum and implemented for national use by CMS, our use of an administrative claims dataset for the measurement of ED admissions and risk-standardization have not been validated in comparison to clinical review of medical records. As such, while we use well established methods for case-mix adjustment based on clinical comorbidities, these methods may not effectively account for all differences in clinical severity that impact hospitalization decisions. Employing the NEDS precluded analysis of observation services, the use of which has been rising in recent years for the conditions identified in our work. However, it is unlikely that the use of observation services can explain this wide variation as only 1–6% of patients are admitted to observation status following ED evaluation for these potentially discretionary conditions.(25) In addition, our work utilized de-identified administrative claims data that lack clinical granularity as well as information about hospital environments. Future work could leverage newer electronic health record data to develop even more robust risk-adjustment models as well as primary data collection methods to understand the impact of patient and provider attitudes, local medico-legal environments, hospital care processes and community resources on variation in ED admission rates.
Conclusions
We demonstrate wide variation in ED admission rates for select conditions that represent meaningful targets for improvement at the hospital-level. Providers seeking to improve the efficiency of care delivery should develop clinical evidence and guidelines as well as hospital-level processes to safely reduce variation in admission rates for potentially discretionary conditions while policymakers should develop quality measures to ensure that we achieve improvement. As inpatient hospital care comprises over one-third of healthcare spending in the US, the success of efforts to improve the quality of healthcare in the US demand a better understanding of ED admissions decisions to ensure the optimal use of scarce hospital resources for the right patients at the right time.
Supplementary Material
Acknowledgments
Disclosures of Fudning: This work has been supported by funding from the National Institute for General Medical Sciences Loan Repayment Program, the Robert Wood Johnson Foundation Clinical Scholars Program, and grant U01 HL105270-04 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute in Bethesda, Maryland
References
- 1.Fine MJ, Hough LJ, Medsger AR, et al. The hospital admission decision for patients with community-acquired pneumonia: Results from the pneumonia patient outcomes research team cohort study. Arch Intern Med. 1997;157(1):36–44. [PubMed] [Google Scholar]
- 2.Rosenblatt RA, Moscovice IS. The physician as gatekeeper: determinants of physicians’ hospitalization rates. Med Care. 1984 Feb;22(2):150–9. doi: 10.1097/00005650-198402000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Kocher KE, Dimick JB, Nallamothu BK. Changes in the source of unscheduled hospitalizations in the united states. Med Care. 2013 Aug;51(8):689–98. doi: 10.1097/MLR.0b013e3182992c7b. [DOI] [PubMed] [Google Scholar]
- 4.Schuur JD, Venkatesh AK. The growing role of emergency departments in hospital admissions. N Engl J Med. 2012 Aug 2;367(5):391–3. doi: 10.1056/NEJMp1204431. [DOI] [PubMed] [Google Scholar]
- 5.Gonzalez Morganti K, Bauhoff S, Blanchard JC, Abir M, Iyer N, Smith A, et al. The evolving role of emergency departments in the united states. RAND Corporation; Santa Monica, CA: 2013. http://www.rand.org/pubs/research_reports/RR280. [PMC free article] [PubMed] [Google Scholar]
- 6.Pines JM, Mutter RL, Zocchi MS. Variation in emergency department admission rates across the United States. Med Care Res Rev. 2013 Jan 6; doi: 10.1177/1077558712470565. [DOI] [PubMed] [Google Scholar]
- 7.Studnicki J, Platonova EA, Fisher JW. Hospital-level variation in the percentage of admissions originating in the emergency department. Am J Emerg Med. 2011 Dec 26; doi: 10.1016/j.ajem.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 8.Roos NP. Hospitalization style of physicians in Manitoba: The disturbing lack of logic in medical practice. Health Serv Res. 1992 Aug;27(3):361–84. [PMC free article] [PubMed] [Google Scholar]
- 9.Wennberg JE, Freeman JL, Shelton RM, Bubolz TA. Hospital use and mortality among Medicare beneficiaries in boston and new haven. N Engl J Med. 1989 Oct 26;321(17):1168–73. doi: 10.1056/NEJM198910263211706. [DOI] [PubMed] [Google Scholar]
- 10.Roos NP, Wennberg JE, McPherson K. Using diagnosis-related groups for studying variations in hospital admissions. Health Care Financ Rev. 1988 Summer;9(4):53–62. [PMC free article] [PubMed] [Google Scholar]
- 11.Luft HS. From small area variations to accountable care organizations: How health services research can inform policy. Annu Rev Public Health. 2012 Apr;33:377–92. doi: 10.1146/annurev-publhealth-031811-124701. [DOI] [PubMed] [Google Scholar]
- 12.Elixhauser A, Steiner C, Palmer L. Clinical classification software (CCS) 2008 Available at http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
- 13.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005 Nov;43(11):1130–9. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 14.Krumholz HM, Lin Z, Drye EE, Desai MM, Han LF, Rapp MT, et al. An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2011 Mar;4(2):243–52. doi: 10.1161/CIRCOUTCOMES.110.957498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krumholz HM, Brindis RG, Brush JE, Cohen DJ, Epstein AJ, Furie K, et al. Standards for statistical models used for public reporting of health outcomes: An American Heart Association scientific statement from the quality of care and outcomes research interdisciplinary writing group: Cosponsored by the council on epidemiology and prevention and the stroke council. endorsed by the American College of Cardiology Foundation. Circulation. 2006 Jan 24;113(3):456–62. doi: 10.1161/CIRCULATIONAHA.105.170769. [DOI] [PubMed] [Google Scholar]
- 16.Ash AS, Fienberg SE, Louis TA, Normand SL, Stukel TA, Utts J. Statistical issues in assessing hospital performance. commissioned by the committee of presidents of statistical societies. 2012 Jan 27; Available at: http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
- 17.QualityNet: MeasureMethodology reports, readmission measures [Internet] 2014 Available at: https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier4&cid=1219069855841.
- 18.Susser SR, McCusker J, Belzile E. Comorbidity information in older patients at an emergency visit: Self-report vs. administrative data had poor agreement but similar predictive validity. J Clin Epidemiol. 2008 May;61(5):511–5. doi: 10.1016/j.jclinepi.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 19.Wang HY, Chew G, Kung CT, Chung KJ, Lee WH. The use of Charlson Comorbidity Index for patients revisiting the emergency department within 72 hours. Chang Gung Med J. 2007 Sep—Oct;30(5):437–44. [PubMed] [Google Scholar]
- 20.Merlo J, Chaix B, Ohlsson H, Beckman A, Johnell K, Hjerpe P, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: Using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006 Apr;60(4):290–7. doi: 10.1136/jech.2004.029454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dean NC, Jones JP, Aronsky D, Brown S, Vines CG, Jones BE, et al. Hospital admission decision for patients with community-acquired pneumonia: Variability among physicians in an emergency department. Ann Emerg Med. 2012 Jan;59(1):35–41. doi: 10.1016/j.annemergmed.2011.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Horwitz LI, Wang Y, Desai MM, Curry LA, Bradley EH, Drye EE, et al. Correlations among risk-standardized mortality rates and among risk-standardized readmission rates within hospitals. J Hosp Med. 2012 Nov-Dec;7(9):690–6. doi: 10.1002/jhm.1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Quality Forum. Prioritization of high-impact Medicare conditions and measure gaps. 2010 May; Available at: http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
- 24.Restuccia J, Shwartz M, Ash A, Payne S. High hospital admission rates and inappropriate care. Health Aff (Millwood) 1996 Winter;15(4):156–63. doi: 10.1377/hlthaff.15.4.156. [DOI] [PubMed] [Google Scholar]
- 25.Venkatesh AK, Geisler BP, Gibson Chambers JJ, Baugh CW, Bohan JS, Schuur JD. Use of observation care in US emergency departments, 2001 to 2008. PLoS One. 2011;6(9):e24326. doi: 10.1371/journal.pone.0024326. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


