Abstract
Health care workers (HCW’s) are always at an increased risk of contracting tuberculosis (TB) infection. In Saudi Arabia, Interferon Gamma Release Assay (IGRA) has not been evaluated as a screening tool for latent TB infection (LTBI) among HCW’s considering their high demographic diversity. During February 2012 to January 2015 a cross sectional study has been conducted in a tertiary care center with maximum demographically diverse staff population in the capital city-Riyadh. After a short interview and consenting, all the candidates were subjected to tuberculin skin test (TST) and QuantiFERON TB gold In-tube test (QFT). A logistic regression analysis was carried out for establishing the associations between putative risk factors and the diagnostic tests. The candidates were classified according to geographical origin and a detailed analysis was conducted on the impact of their origin towards the results of TST and QFT. Of the 1595 candidates enrolled, 90.6% were BCG vaccinated, female (67.9%) and mainly nurses (53.2%). Candidates with high risk of suspected or confirmed TB patient exposure were 56.1% and 76.5% of them had <10 year’s work experience. TST positivity was observed in 503 (31.5%) candidates, while QFT was positive among 399 (25%). Majority of the candidates were non-Saudi (83%) and predominantly (52.4%) from Western Pacific region. Concordant results were obtained in 14.2% of positive cases and 57.7% negative cases. The disagreements between the two tests were relatively high (kappa co-efficient-0.312±0.026, p value- <0.00001) as TST positive/QFT negative discordance was 54.8% while TST negative/QFT positive discordance was 15.7%. Age of the candidates, BCG vaccination, and South East Asian origin were associated with TST positivity while Occupational TB exposure and geographical origin of the candidates were associated with QFT positivity. A regular follow up on recently TST converted candidates showed no progression to active TB. The putative factors associated with the discordance were origin of the candidate (p value <0.001), profession (p value-0.001), BCG vaccination (p value-0.001) and occupational TB exposure level (P value-0.001). The study demonstrated high level prevalence of LTBI among the demographically diverse study candidates. The agreement between QFT and TST was poor, thus QFT alone cannot be recommended in our setting for a routine LTBI screening. Origin of the candidates has strong association with the results of TST and QFT. The discordant results particularly TST negative and QFT positive needs more detailed analysis.
Introduction
Tuberculosis (TB) continues to be a major global health problem including in Saudi Arabia [1]. High proportion of immigrants living in the country and annual massive influx of pilgrims mostly from TB endemic areas constitute favorable conditions for TB transmission [2–4]. One of the most important challenges in global TB control is the early detection and treatment of latent tuberculosis infection (LTBI). About 10% of individuals infected with M. tuberculosis develop pulmonary TB, and the remaining 90% suppress the bacterial invasion through their immune systems and persist with LTBI [5]. Unfortunately there is very limited data on the prevalence of LTBI among health care workers in Saudi Arabia, except reports from few institutions [6].
Health care workers (HCW’s) in general are considered as a high-risk group of LTBI because of the increased risk of exposure [7–9]. A recent systematic review showed, among HCW’s of low and middle income countries, the LTBI prevalence is ranged between 33–79% with a median of 5.8% annual LTBI incidence [10]. Usually, HCW’s may come into contact with patients with undiagnosed cases or unknown/unsuspected cases of active TB, which elevates the acquisition of LTBI. HCW’s employed in sections like emergency, intensive care, internal medicine, radiology, are at greater risk of acquiring M. tuberculosis. Due to the epidemiological evidence of TB as a consequential occupational disease, HCW’s with negative TST results must undergo annual LTBI screening.
Surveillance study on LTBI among HCW’s vaccinated with BCG has been hampered by the non- specificity of TST. False-positive results secondary to cross-reactions caused by BCG vaccination and/or exposure to non tuberculous mycobacteria, booster phenomenon and technical issues, like interpretation of the result may all lead to unnecessary treatment of presumed LTBI thereby, rendering TST unsuitable as a surveillance tool in TB risk groups [11,12]. The advent of Interferon Gamma Release Assays (IGRA) and their increasing availability show promise for more accurate LTBI detection in HCW’s. The higher specificity of QuantiFERON TB gold assay (QFT) compared with TST can reduce unnecessary treatment, follow-ups and thereby, treatment cost of LTBI [13,14].
Most IGRA studies have been done in low TB-endemic regions whereas; data from low to middle-income settings, with high background of TB infection rates have been fairly scarce. We are not aware of any report describing the use of IGRA’s among HCWs in Saudi Arabia or in Gulf Cooperation Council (GCC) countries.
In Saudi Arabia, TB screening is recommended for all HCW’s. Annual LTBI screening is mandatory for all employees at King Faisal Specialist Hospital and Research Centre (KFSHRC) as part of their job contract renewals. The TST is the currently following LTBI diagnostic method at KFSHRC. However due to the limitations of the TST and to promote a more sensitive technique, IGRA was considered. The cosmopolitan nature of the employee population (citizens of more than 60 countries) has not been considered for optimizing the LTBI diagnosis. Moreover, the majority of the employee populations are from countries where BCG vaccination is mandatory. In addition, there was an increasing prevalence of NTM diseases also reported in the country recently [15]. Thus a new LTBI diagnostic test was badly needed for the institution.
Therefore, a cross sectional study has been designed with two major set objectives. The key objectives were to analyze the prevalence of LTBI among HCW’s of highly diverse origin at KFSHRC and to compare the feasibility of using TST and QFT to screen the LTBI among this diverse population.
Materials and Methods
This study was carried out for a period of 36 month (February 2012 to January 2015) in KFSHRC, Riyadh. The protocol has been reviewed and approved by the Research Advisory Council (RAC) of KFSHRC. All the candidates enrolled were subjected to a short interview and completed the consent form before withdrawing the blood samples.
Study population
The inclusion criteria for study subjects was any new (undergoing pre-employment checkup) or existing employee (annual re-contracting checkup), who can consent for the study. The exclusion criteria included candidates with previous history of active TB or undergoing TB medication. The study subjects were recruited from both clinical and non-clinical health care workers designated in various departments at KFSHRC. Clinical health-care workers (those included in any direct patient contact or giving direct care) are doctors, nurses and allied health professionals. Non-clinical health-care workers included those who did not involve in direct patient care, such as administrative staffs, researchers, housekeepers, and hospital technical maintenance staffs.
According to the job profile of the candidate, the degree of TB exposure level was defined into low, medium and high. Doctors, nurses and allied health professionals were classified into high risk group. The medium risk group consisted of candidates who are not directly giving patient care but in contact with patient samples (ex; medical lab technicians) or technicians managing respiratory units or equipments. The low risk group included researchers, maintenance staffs and administrative staffs respectively.
A standard questionnaire was used to collect the information on key variables, such as age, gender, nationality, previous exposure or treatment details of TB, previous chest x-ray details, BCG vaccination and BCG scar, prior TST (date and result), job category, service and years in the health profession. The questionnaire has been completed by face to face interview and reference to medical records.
All the TST positive converted staffs were offered with a follow up of Chest X-ray and a 9 months isoniazid treatment according to the standard guidelines. The decision of treatment was kept optional to the employee after the discussion with the physician. However a continuous follow-up was mandatory.
Performing TST and QFT
All new HCW’s, who did not have a documented TST result, were subjected to TST during the routine examination at the time of employment in the family medicine department of KFSHRC. TST was performed by administrating 2-TU of PPD RT23 (Staten’s Serum Institute, Copenhagen, Denmark). Induration was measured 48–72 h after the application. Well trained nurses performed and interpreted the results in 48–72 hours according to the American Thoracic Society (ATS) and Centers for Disease Control and Prevention guidelines [16]. The positive interpretation followed was a TST with an area of induration ≥10 mm. If HCW’s had a previous positive TST, we took note of the place and the year. If HCW’s had negative TST, it is repeated annually or after an exposure as part of KFSHRC’s infection control practice.
The QFT was carried out by using the commercially available QuantiFERON TB gold In-Tube Assay (Cellestis, Australia) according to the manufacturer’s protocol. The raw optical density was measured and interpreted with the software QuantiFERON TB Gold analysis Software v1.51 (Cellestis, Australia).
Statistical analysis
The candidates were classified according to the WHO’s geographical classification into 6 major groups; American, African, European, Eastern Mediterranean, South East Asian, and Western Pacific [17]. The statistical analysis has been carried out by using the SPSS v-20 software package. A chi squared test was utilized for categorical data. All the putative predictive variables were subjected to calculate the odds ratio and 95% confidence interval.
Results
Overall 1603 candidates were enrolled during the study period. Of the total, 8 HCWs (1.2%) were excluded from the analysis due to indeterminate QFT results and 1595 were included for final analysis. The study population included candidates from 33 countries. The native Saudi population was only 17%. The geographical classification on enrolled candidates showed, 52.4% were from Western-Pacific followed by 22.9% Eastern Mediterranean and 11.3% South East Asians. The median of age in the study was 35.5 years with a predominance of female candidates (67.9%). Clinical staffs represented the major study group by71.5% and among them nurses were predominant (53.2%). Overall, 185(11.6%) candidates reported with a previous exposure to known pulmonary TB cases. Majority of the candidates (90.6%) received at least one shot of BCG vaccination before enrollment (S1 Table). Candidates holding a healthcare experience of 2–5 years were comparatively more (37.6%), though the mean duration of experience in the study was 8.4 years (Table 1).
Table 1. General Characteristics of the study population.
| Parameters | No/% |
|---|---|
| Gender | |
| Male | 512(32.1) |
| Female | 1083(67.9) |
| Age Group | |
| 19–29 | 543 (34) |
| 29–39 | 596(37.4) |
| 39–49 | 292(18.3) |
| 49–59 | 129(8.1) |
| >60 | 35(2.2) |
| Profession | |
| Physician | 44(2.8) |
| Nurses | 849(53.2) |
| Allied Health | 248(15.5) |
| Support Services | 348(21.8) |
| Administration | 62(3.9) |
| Researchers | 44(2.8) |
| Occupational degree of TB exposure | |
| Low | 398(25) |
| Medium | 302(18.9) |
| High | 895(56.1) |
| Known Pulmonary TB exposure | |
| Yes | 185(11.6) |
| No | 556(34.9) |
| Unknown | 854(83.5) |
| TST Converters | |
| Yes | 170 |
| No | 1425 |
| Prophylaxis among converted candidates | |
| Yes | 46(2.9) |
| No | 1545(96.9) |
| TST Result | |
| Positive | 502(31.5) |
| Negative | 1093(68.5) |
| QFT Results | |
| Positive | 399(25) |
| Negative | 1196(75) |
| BCG Vaccination | |
| Yes | 1444(90.6) |
| No | 92(5.8) |
| Unknown | 58(3.6) |
| TST Induration | |
| <10mm | 1093(68.5) |
| 10-15mm | 328(20.6) |
| 16-20mm | 116(7.3) |
| >20mm | 58(3.6) |
| Years of work | |
| <2 years | 108(6.8) |
| 2–5 years | 600(37.6) |
| 5–10 years | 511(32.1) |
| 10–20 years | 289(18.1) |
| >20 years | 87(5.4) |
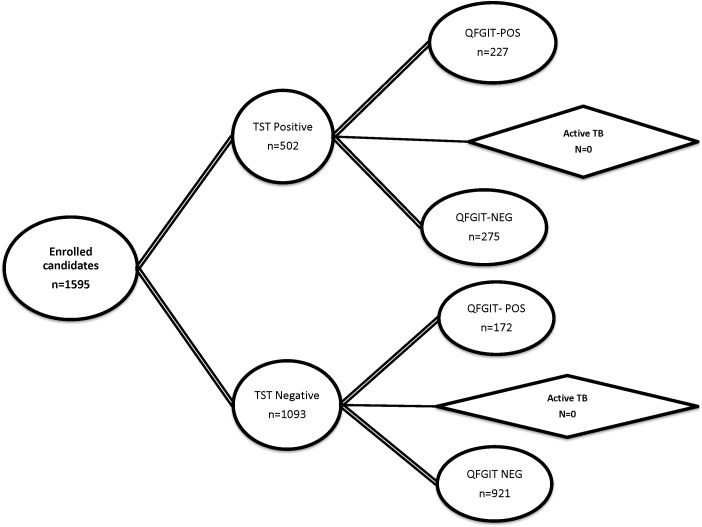
Positive TST was noticed in 31.5% of the enrolled candidates. Among the TST positive cases 45.2% were QFT positive while 54.8% were negative. On the other hand, among TST negative cases, 15.7% were QFT positive. The disagreements between the two tests were relatively high (kappa co-efficient-0.312±0.026, p value- <0.00001). Among 170 TST converted participants only 46 opted for INH prophylaxis and none of these cases progressed to active TB during the study period (Fig 1). The regression analysis of the putative predictable factors showed a significant association of younger age groups (p -0.030, 0.049), BCG vaccination (p- 0.028), European (p -<0.001) and south East Asian (p-0.009) origin with TST positivity. QFT positivity was associated with profession of candidates and occupational TB exposure risk. In addition, the origin of the candidates (p-<0.001) was highly significant in QFT positivity (Table 2).
Fig 1. Study summary diagram with results.
The figure shows the total number of samples tested (omitted 8 isolates because of Indeterminate QFT results) and the varying results of IGRA and TST. Progression of the candidates to active TB was also followed up with the concordance of test results.
Table 2. Risk factors associated with positive TST and QFT.
| Parameters | TST >10mm | QFT-Positive | ||||||
|---|---|---|---|---|---|---|---|---|
| N | OR | 95%CI | P value | N | OR | 95%CI | P value | |
| Gender | 1.021 | 0.814–1.279 | 0.859 | 0.952 | 0.747–1.212 | 0.688 | ||
| Male | 349 | 132 | ||||||
| Female | 743 | 267 | ||||||
| Age group | ||||||||
| 19–29 | 176 | 2.902 | 1.107–7.606 | 0.030 | 141 | 1.172 | 0.521–2.641 | 0.701 |
| 29–39 | 196 | 2.940 | 1.123–7.694 | 0.028 | 149 | 1.125 | 0.500–2.530 | 0.776 |
| 39–49 | 90 | 2.673 | 1.005–7.114 | 0.049 | 69 | 1.044 | 0.454–2.404 | 0.919 |
| 49–59 | 35 | 2.234 | 0.803–6.215 | 0.124 | 32 | 1.113 | 0.460–2.696 | 0.812 |
| >60 | 6 | REF | 8 | REF | ||||
| Profession | ||||||||
| Physician | 11 | 0.583 | 0.233–1.461 | 0.250 | 9 | 0.613 | 0.231–1.630 | 0.327 |
| Nurses | 260 | 0.772 | 0.411–1.452 | 0.423 | 204 | 0.754 | 0.387–1.469 | 0.754 |
| Allied Health | 79 | 0.818 | 0.419–1.598 | 0.557 | 42 | 0.486 | 0.235–1.007 | 0.052 |
| Support Services | 107 | 0.777 | 0.404–1.496 | 0.450 | 111 | 1.117 | 0.563–2.217 | 0.752 |
| Administration | 30 | 1.641 | 0.744–3.618 | 0.220 | 20 | 1.054 | 0.453–2.448 | 0.903 |
| Researchers | 16 | REF | 13 | REF | ||||
| Occupational Risk | ||||||||
| Low | 136 | REF | 127 | REF | ||||
| Medium | 96 | 0.898 | 0.653–1.235 | 0.507 | 58 | 0.507 | 0.355–0.724 | <0.001 |
| High | 271 | 0.837 | 0.651–1.076 | 0.165 | 214 | 0.666 | 0.513–0.865 | 0.002 |
| Years of work | ||||||||
| <2 Years | 33 | 1.306 | 0.655–2.602 | 0.448 | 26 | 1.306 | 0.655–2.602 | 0.448 |
| 2–5 years | 194 | 1.536 | 0.878–2.688 | 0.133 | 163 | 1.536 | 0.878–2.688 | 0.133 |
| 6–10 years | 164 | 1.264 | 0.716–2.230 | 0.419 | 120 | 1.264 | 0.716–2.230 | 0.419 |
| 10–20 years | 95 | 1.366 | 0.755–2.473 | 0.303 | 72 | 1.366 | 0.755–2.473 | 0.303 |
| >20 years | 17 | REF | 17 | REF | ||||
| BCG Vaccination | 449 | 1.039 | 0.664–1.625 | 0.028 | 356 | 1.364 | 0.866–2.146 | 0.179 |
| Geographical Origin | ||||||||
| American | 28 | 1.236 | 0.760–2.011 | 0.394 | 13 | 0.481 | 0.260–0.889 | 0.019 |
| African | 18 | 0.671 | 0.388–1.162 | 0.154 | 12 | 0.444 | 0.235–0.837 | 0.012 |
| European | 37 | 3.201 | 1.888–5.427 | <0.001 | 32 | 2.525 | 1.501–4.246 | <0.001 |
| Eastern Mediterranean | 117 | 1.020 | 0.784–1.328 | 0.881 | 60 | 0.466 | 0.340–0.637 | <0.001 |
| South East Asian | 39 | 0.598 | 0.408–0.878 | 0.009 | 33 | 0.531 | 0.354–0.797 | 0.002 |
| Western Pacific | 264 | REF | 249 | REF | ||||
Analysis of agreement of results of TST and QFT showed 14.23% concordant positive results while 57.7% is concordant negative. However, 10.8% cases were TST negative and QFT positive. On the other hand 275(17.2%) cases were TST positive and QFT negative. Analyzing the association of various putative factors showed the origin of the patient (p <0.001), occupational TB exposure level (p-<0.001), profession (p- 0.001) and BCG vaccination history (p- 0.001) have a statistical significance on the agreement of both the tests (Table 3). Among the discordant results, candidates with Western Pacific origin showed a predominant QFT positivity (65.7%) and negativity (46.9%). Interestingly, among the different professions, nurses have the highly discordant results (Table 3).
Table 3. Relationship between risk factors and pattern of concordant and discordant test results.
| Parameters | N | Concordant Positives | Concordant Negatives | Discordant; TST-/QFT+ | Discordant; QFT-/TST+ | P value |
|---|---|---|---|---|---|---|
| N = 227 | N = 921 | N = 172 | N = 275 | |||
| Gender | 0.980 | |||||
| Male | 512 | 74(32.6) | 292(31.7) | 57(33.1) | 89(32.4) | |
| Female | 1083 | 153(67.4) | 629(68.3) | 115(66.9) | 186(67.6) | |
| Age groups | ||||||
| 19–29 | 543 | 85(37.5) | 311(33.8) | 56(32.6) | 91(33.1) | 0.463 |
| 29–39 | 596 | 80(35.2) | 331(35.9) | 69(40.1) | 116(42.2) | |
| 39–49 | 292 | 42(18.5) | 175(19) | 27(15.7) | 48(17.4) | |
| 49–59 | 129 | 18(7.9) | 80(8.7) | 14(8.1) | 17(6.2) | |
| >60 | 35 | 2(0.9) | 24(2.6) | 6(3.5) | 3(1.1) | |
| Origin | <0.001 | |||||
| American | 77 | 7(3.1) | 43(4.7) | 6(3.5) | 21(7.6) | |
| African | 76 | 7(3.1) | 53(5.7) | 5(2.9) | 11(4.0) | |
| European | 62 | 25(11.0) | 18(1.9) | 7(4.1) | 12(4.4) | |
| Eastern Mediterranean | 365 | 31(13.7) | 219(23.8) | 30(17.4) | 85(30.9) | |
| South East Asian | 180 | 22(9.6) | 130(14.1) | 11(6.4) | 17(6.2) | |
| Western Pacific | 835 | 135(59.5) | 458(49.7) | 113(65.7) | 129(46.9) | |
| Profession | 0.001 | |||||
| Physician | 44 | 4(1.8) | 28(3.0) | 5(2.9) | 7(2.5) | |
| Nurses | 849 | 126(55.5) | 511(55.5) | 78(45.3) | 134(48.7) | |
| Allied Health | 248 | 25(11) | 152(16.6) | 18(10.6) | 53(19.3) | |
| Support Services | 348 | 54(23.8) | 184(19.9) | 57(33.1) | 53(19.3) | |
| Administration | 62 | 11(4.8) | 24(2.6) | 8(4.6) | 19(6.9) | |
| Researchers | 44 | 7(3.1) | 22(2.4) | 6(3.5) | 9(3.3) | |
| Occupational Risk | <0.001 | |||||
| Low | 398 | 64(28.2) | 199(21.6) | 64(37.2) | 71(25.8) | |
| Medium | 302 | 33(14.5) | 181(19.6) | 25(14.5) | 63(22.9) | |
| High | 895 | 130(57.3) | 541(58.8) | 83(48.3) | 141(51.3) | |
| Years of work | 0.153 | |||||
| <2 Years | 108 | 12(5.3) | 61(6.6) | 15(8.7) | 20(7.3) | |
| 2–5 years | 600 | 99(43.6) | 342(37.2) | 64(37.2) | 95(34.6) | |
| 6–10 years | 511 | 62(27.3) | 289(31.4) | 58(33.7) | 102(37.1) | |
| 10–20 years | 289 | 47(20.7) | 169(18.3) | 25(14.5) | 48(17.4) | |
| >20 years | 87 | 7(3.1) | 60(6.5) | 10(5.8) | 10(3.6) | |
| BCG Vaccination | 1444 | 206(90.7) | 845(91.7) | 151(87.8) | 206(74.9) | 0.001 |
Discussion
This is the largest Saudi Arabian study, which evaluated the performance of QFT and TST among highly diverse HCW’s population. The study has targeted onto the putative risk factors with an emphasis on the impact of geographic origin of study subjects. It is also the only cross sectional study in the country that looked at the possibilities of developing active TB in recently identified LTBI in HCW’s. This study has been carried out in a tertiary care center which has been listed among the top five medical facilities in the country employing staffs from more than 60 countries. The impact of this huge diversity in the origin of the staffs has been highly considered on the LTBI prevalence, as it influence the agreement between TST and IGRA. The overall agreement between TST and QFT was 72%, that can be considered as fair, when many previous international studies reported moderate or fair agreement only between both the tests [18–20]. Supportively, recent studies from Saudi Arabia on dialysis patients also showed 75.5% and 90.9% agreement between TST and QFT/TSPOT Assay respectively [21,22].
The prevalence of LTBI measured in this study by TST (31.5%) and QFT (25.0%) was relatively high. This elevated rate may be typical for a moderate TB burden country like Saudi Arabia. Furthermore, the previous estimates showed that, Saudi Arabia has only an intermediate prevalence of LTBI (2–14%) [23]. In Saudi Arabia, only limited information is available on prevalence of LTBI among HCW’s particularly screened with IGRA testing. A multicenter study utilizing TST alone in HCW’s showed 11% LTBI prevalence, while the current study showed 31.5% [6]. However, the elevated prevalence level of LTBI in the current study may largely depend on the origin of the candidates, that particularly from TB endemic regions.
The current study population consisted only 17% Saudi nationals. The results of TST and QFT stratified by the Saudi and non-Saudi origin showed a prevalence of 18.1% and 17.3% among Saudis. This finding highlights the massive role of immigrant HCW’s in the institution and mostly their origin from TB endemic countries. After applying the geographical region classification of WHO into the study, showed the Western Pacific origin candidates (mainly Philippines) as the largest group in the study followed by the Eastern Mediterranean and south East Asians. Interestingly, there are 970(60.8%) candidates truly from high TB burden countries namely, Philippines, India, Bangladesh, Pakistan, Sudan, South Africa, Eritrea, Ethiopia and Kenya. Analysis of the TST results against the nationality of the candidates, showed 305(60.6%) of the total 503 TST positive and 234 (58.6%) of the total 399 QFT positive candidates are from this group. The agreement between two results was really narrow (only 2%). Among the candidates from high TB burden countries only 94(9.7%) had TST conversion during their employment in the study center. This speculates the scope of a remote infection among those remaining 876(90.3%) candidates from their previous destination that is mostly their mother country. This finding has a support from molecular studies by Varghese et al., which showed remote TB infection among immigrants is very common Saudi Arabia [24,25].
In the current study the maximum discordance was observed in TST positive and QFT negative results. Among the TST positive cases 54.7% were negative for QFT. This finding corroborates with published studies which reported positive TST and negative IGRA is the most common discordance [26]. Majority of the study candidates were from a country where BCG vaccination is mandatory, thus 90.6% of the enrolled candidates were BCG vaccinated. This could probably affect the higher level prevalence of TST positivity. Supportively, a statistically significant association (OR 1.039, 95% CI-0.664–1.625, P value 0.028) was noticed between BCG vaccination and TST positivity while no significant association with QFT. This finding is in concordance with previous studies, which showed BCG vaccination significantly elevates the likelihood of TST positivity [27]. When compared with age >60 years, the younger age has significant association with TST positivity in concordance with various previous studies [28,29]. The rate of TST positivity among different professionals showed no significant association. In contrast, the TB exposure level based on profession showed a high significance towards QFT positivity, when low risk group was kept as a reference as seen in previous studies [30,31]. The origin of the candidates also has significant association with both TST and QFT positivity.
The maximum discordant results were noticed among candidates from Western Pacific region. Overall 65.7% of the TST negative QFT positive candidates and 46.9% of TST positive and QFT negative candidates were from mainly Philippines and Malaysia, while candidates from Eastern Mediterranean region showed the rates of 17.4% and 30.9% respectively. The massive enrollment of Filipino candidates (45.2%) has an impact on the overall findings. The two main reasons are the mandatory BCG vaccine administration and high TB burden of Philippines. Perhaps, the higher discordant results of TST negative and QFT positive could not be explained in detail. No significant association could be established between the discordant results against age of the candidates, gender, and years of work in the medical field. However, strong associations could be noticed on origin of the candidates (p <0.001), profession (p 0.001), TB exposure level (p <0.001) and BCG vaccination (p 0.001). Nurses and support service staffs showed majority of the discordant results. This finding was supported by the rate of TB exposure level as the high TB exposure group has highest discordance between results. This study has certain limitations; candidates reported as TST negative and QFT positive were not retested for confirmation and quantitative analysis of QFT testing was not considered.
Conclusion
In conclusion, the prevalence of LTBI estimated by QFT is high among Saudi Arabian HCW’s. The disagreements between TST and IGRA results were relatively high and thus QFT alone cannot be recommended to screen LTBI. The origin of the candidates has significant role in both TST and IGRA positivity. However due to the high level of LTBI prevalence, the screening and management of LTBI in HCW’s in the country must be immediately streamlined.
Supporting Information
(XLSX)
Acknowledgments
We deeply acknowledge, Maribel Carbonel, Diana Oliveira, Florence Saguid, Lenora Reyes, Tracy Lynn Alsarhani, Rania Omar Albadawi and Maria Minette Valesteros for their immense support for recruiting the candidates.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors have no support or funding to report.
References
- 1.World Health Organization. Global Tuberculosis Report- 2013. Geneva, Switzerland: 2013,W.H.O. [Google Scholar]
- 2.Alzahrani AG, Choudhry AJ, Al Mazroa MA, Turkistani AH, Nouman GS,Memish ZA. Pattern of diseases among visitors to Mina health centers during the Hajj season, 1429 H (2008 G). J Infect Public Health 2012; 5: 22–34. 10.1016/j.jiph.2011.10.003 [DOI] [PubMed] [Google Scholar]
- 3.Alzeer AH. Respiratory tract infection during Hajj. Ann Thorac Med 2009; 4: 50–53. 10.4103/1817-1737.49412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Hajoj S, Varghese B, Al-Habobe F, Shoukri MM, Mulder A, van Soolingen D. Current trends of Mycobacterium tuberculosis molecular epidemiology in Saudi Arabia and associated demographical factors. Infect Genet Evol 2013; 16: 362–368. 10.1016/j.meegid.2013.03.019 [DOI] [PubMed] [Google Scholar]
- 5.Harada N.Characteristics of a diagnostic method for tuberculosis infection based on whole blood interferon-gamma assay. Kekkaku 2006; 81: 681–686. [PubMed] [Google Scholar]
- 6.Abbas MA, AlHamdan NA, Fiala LA, AlEnezy AK, AlQahtani MS. Prevalence of latent TB among health care workers in four major tertiary care hospitals in Riyadh, Saudi Arabia. J Egypt Public Health Assoc 2010; 85: 61–71. [PubMed] [Google Scholar]
- 7.He GX, van denHof S, van der Werf MJ, Wang GJ, Ma SW, Zhao DY, et al. Infection control and the burden of tuberculosis infection and disease in health care workers in china: a cross-sectional study. BMC Infect Dis 2010; 10: 313 10.1186/1471-2334-10-313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rubbo PA, Nagot N, Le Moing V, Brabet M, Bourdin A, Nogue E, et al. Multicytokine detection improves latent tuberculosis diagnosis in health care workers. J Clin Microbiol 2012; 50: 1711–1717. 10.1128/JCM.00117-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baussano I, Nunn P, Williams B, Pivetta E, Bugiani M, Scano F,. Tuberculosis among health care workers. Emerg Infect Dis 2011; 17: 488–494. 10.3201/eid1703.100947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joshi R, Reingold AL, Menzies D, Pai M. Tuberculosis among health-care workers in low- and middle-income countries: a systematic review. PLoS Med 2006; 3: e494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chawla H, Lobato MN, Sosa LE, ZuWallack R. Predictors for a positive QuantiFERON-TB-Gold test in BCG-vaccinated adults with a positive tuberculin skin test. J Infect Public Health 2012; 5: 369–373. 10.1016/j.jiph.2012.06.003 [DOI] [PubMed] [Google Scholar]
- 12.Farhat M, Greenaway C, Pai M, Menzies D. False-positive tuberculin skin tests: what is the absolute effect of BCG and non-tuberculous mycobacteria? Int J Tuberc Lung Dis 2006; 10: 1192–1204. [PubMed] [Google Scholar]
- 13.Hung WT, Lee SS, Sy CL, Wu KS, Chen JK, Tsai HC, et al. Prevalence of latent tuberculosis infection in BCG-vaccinated healthcare workers by using an interferon-gamma release assay and the tuberculin skin test in an intermediate tuberculosis burden country. J Microbiol Immunol Infect. 2015; 48: 147–152 10.1016/j.jmii.2013.07.008 [DOI] [PubMed] [Google Scholar]
- 14.Dosanjh DP, Bakir M, Millington KA, Soysal A, Aslan Y, Efee S, et al. (2011) Novel M tuberculosis antigen-specific T-cells are early markers of infection and disease progression. PLoS One 6: e28754 10.1371/journal.pone.0028754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Varghese B, Memish Z, Abuljadayel N, Al-Hakeem R, Alrabiah F, AlHajoj SA. (2013) Emergence of clinically relevant Non-Tuberculous Mycobacterial infections in Saudi Arabia. PLoS Negl Trop Dis 7: e2234 10.1371/journal.pntd.0002234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diagnostic Standards and Classification of Tuberculosis in Adults and Children. This official statement of the American Thoracic Society and the Centers for Disease Control and Prevention was adopted by the ATS Board of Directors, July 1999. This statement was endorsed by the Council of the Infectious Disease Society of America, September 1999. Am J Respir Crit Care Med 161: 1376–1395. [DOI] [PubMed] [Google Scholar]
- 17.Organization WH (2014) Global Tuberculosis Report. Geneva: WHO. [Google Scholar]
- 18.Caglayan V, Ak O, Dabak G, Damadoglu E, Ketenci B, Ozdemir M, et al. (2011) Comparison of tuberculin skin testing and QuantiFERON-TB Gold-In Tube test in health care workers. Tuberk Toraks 59: 43–47. [PubMed] [Google Scholar]
- 19.El-Helaly M, Khan W, El-Saed A, Balkhy HH (2014) Pre-employment screening of latent tuberculosis infection among healthcare workers using tuberculin skin test and QuantiFERON-TB Gold test at a tertiary care hospital in Saudi Arabia. J Infect Public Health 7: 481–488. 10.1016/j.jiph.2014.07.012 [DOI] [PubMed] [Google Scholar]
- 20.Jong Lee K, Ae Kang Y, Mi Kim Y, Cho SN, Wook Moon J, Suk Park, M, et al. (2010) Screening for latent tuberculosis infection in South Korean healthcare workers using a tuberculin skin test and whole blood interferon-gamma assay. Scand J Infect Dis 42: 672–678. 10.3109/00365548.2010.485575 [DOI] [PubMed] [Google Scholar]
- 21.Al Jahdali H, Ahmed AE, Balkhy HH, Baharoon S, Al Hejaili FF, Hajeer A, et al. (2013) Comparison of the tuberculin skin test and Quanti-FERON-TB Gold In-Tube (QFT-G) test for the diagnosis of latent tuberculosis infection in dialysis patients. J Infect Public Health 6: 166–172. 10.1016/j.jiph.2013.02.002 [DOI] [PubMed] [Google Scholar]
- 22.Hassan HA SM, Housawi AR, Elsammak MY. Detecting latent utberculosis infection prior to kidney transplantation in a tertiary hospital in Saudi Arabia; comparison of TSPOT TB test and tuberculin test. Br Microbiol Res J.2013; 3: 116–127. [Google Scholar]
- 23.Al-Jahdali H, Memish ZA, Menzies D. The utility and interpretation of tuberculin skin tests in the Middle East. Am J Infect Control.2005; 33: 151–156. [DOI] [PubMed] [Google Scholar]
- 24.Varghese B, Supply P, Shoukri M, Allix-Beguec C, Memish Z, Abuljadayel N, et al. Tuberculosis transmission among immigrants and autochthonous populations of the eastern province of Saudi Arabia. PLoS One.2013; 8: e77635 10.1371/journal.pone.0077635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Varghese B, al-Omari R, Grimshaw C, Al-Hajoj S. Endogenous reactivation followed by exogenous re-infection with drug resistant strains, a new challenge for tuberculosis control in Saudi Arabia. Tuberculosis (Edinb). 2013; 93: 246–249. [DOI] [PubMed] [Google Scholar]
- 26.Zwerling A, van den Hof S, Scholten J, Cobelens F, Menzies D, Pai M. Interferon-gamma release assays for tuberculosis screening of healthcare workers: a systematic review. Thorax. 2012; 67: 62–70. 10.1136/thx.2010.143180 [DOI] [PubMed] [Google Scholar]
- 27.Wang L, Turner MO, Elwood RK, Schulzer M, FitzGerald JM. A meta-analysis of the effect of Bacille Calmette Guerin vaccination on tuberculin skin test measurements. Thorax.2002; 57: 804–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Casas I, Latorre I, Esteve M, Ruiz-Manzano J, Rodriguez D, Pat C, et al. Evaluation of interferon-gamma release assays in the diagnosis of recent tuberculosis infection in health care workers. PLoS One.2009; 4: e6686 10.1371/journal.pone.0006686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Costa JT, Silva R, Sa R, Cardoso MJ, Ribeiro C, Nienhaus A. Comparison of interferon-gamma release assay and tuberculin test for screening in healthcare workers. Rev Port Pneumol.2010; 16: 211–221. [PubMed] [Google Scholar]
- 30.Zwerling A, Cojocariu M, McIntosh F, Pietrangelo F, Behr MA, Schwartzman K, et al. TB screening in Canadian health care workers using interferon-gamma release assays. PLoS One.2012; 7: e43014 10.1371/journal.pone.0043014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Torres Costa J, Sa R, Cardoso MJ, Silva R, Ferreira J, Ribeiro C, et al. Tuberculosis screening in Portuguese healthcare workers using the tuberculin skin test and the interferon-gamma release assay. Eur Respir J.2009; 34: 1423–1428. 10.1183/09031936.00053809 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.