Abstract
The transfer of autologous fat has been performed since the 1890s; however, its popularity has increased owing to better understanding of fat harvesting and processing techniques. In this article, fat grafting procedure has been used to correct posttraumatic facial deformities in 25 cases. As healing of grafted fat is unpredictable, we have used longer follow-up of 2 years. Evaluation was performed using facial photographs and MRI scans. Scientific literature describes an absorption rate ranging from 20 to 90%. High fat graft resorption rates have been attributed to traumatic handling of the graft during harvest, processing, and injection. Various processing techniques have been suggested. The goal of these techniques is to obtain greater adipocyte cell survival and, consequently, more reliable clinical results. In our study, we have used syringe aspiration and low-speed centrifuge for processing of fat which has resulted in good clinical outcomes.
Keywords: fat grafting, maxillofacial deformities, posttraumatic facial deformities
The transfer of autologous fat has been performed as whole grafts since the 1890s1 and as injectable grafts since the 1920s2; however, popularity of fat grafting procedures has increased owing to better understanding of fat harvesting and processing techniques. History of free fat grafts dates back to the early 1890s when Neuber first performed an autologous fat transfer for scarred tissue.1 However, it was soon noticed that majority of grafted fat undergoes resorption. Unpredictable and inconsistent results of fat grafting procedure had resulted in declining interest among surgeons. In 1950, Peer proposed adipocyte survival theory in which he stated that quantity of viable adipocytes is inversely proportional to graft resorption.3 In 1990s, Coleman published concept of structural fat grafting.4 He emphasized on atraumatic surgical technique in harvesting and processing of fat.
Unpredictable results with fat grafting procedure are often encountered because of variable fat resorption. Various studies have reported variable percentage of fat resorption ranging from 20 to 90%.5 6 7 8 Despite higher percentage of graft resorption, surgeons have continued to use fat grafting procedures because of inexpensive and less morbid nature of the procedure. Moreover, risk of host rejection and prolong hospital stay can be obviated. Fat grafting is commonly used for facial scars, facial deformities, lip augmentation, chin augmentation, breast augmentation, and so on.
In this article, we have used autologous fat for correction of posttraumatic nonfunctional facial deformities. We have evaluated our results both clinically and by comparing preoperative and postoperative magnetic resonance imaging (MRI) scans. Our protocol for fat harvesting and processing involves use of syringe aspiration and low-speed manual centrifuge. We believe that use of slow-speed, hand-driven manual centrifuge is superior to high-speed mechanical centrifuge which results in greater adipocyte survival and subsequently better long-term esthetic results.
Materials and Methods
Patients with posttraumatic facial deformities resulting from either inadequate or no primary treatment were chosen for this study. This study was performed on a total of 25 patients out of which 16 were males and 9 females. All cases were performed by one surgeon to rule out any interoperator bias. Fat grafting was done under general anesthesia and fat was harvested from medial aspect of thigh in all patients. Patients with gross facial asymmetry requiring bony correction or implants were excluded from the study. Also, patients with poor general health, psychological disorders, and not willing to enroll in the study were excluded. MRI was done preoperatively, and at 1st and 12th months postoperatively to do comparative analysis of fat resorption.
Surgical Procedure
Under general anesthesia, patients were prepared with all aseptic precautions. For infiltration of donor site (medial aspect of thigh), we prepare a mixture of 500 mL of Ringer's lactate and 0.5 mL of 1:1,000 adrenaline. This solution was infiltrated as required.
After a waiting period of a minimum 20 minutes, fat harvesting was done by manual aspiration using Sydney Coleman aspiration system which consists of a 3-mm bore cannula attached to a 10-mL Luer lock syringe (Fig. 1).
Same 10-mL syringe is used for its placement in manual centrifuge apparatus (Fig. 2). Speed of manual centrifuge, as measured by digital tachometer, does not exceed 500 RPM (revolutions per minute). Centrifugation was thus performed at 500 RPM for 2 minutes.
-
The aspirate after centrifuge form three layers (Fig. 3):
The upper oily layer of fatty acids.
The intermediate layer consists of adipocytes cell mass.
The lower one is the dark red mass of packed red blood cells.
Fig. 1.

Fat harvesting from medial thigh.
Fig. 2.

Manual centrifuge apparatus.
Fig. 3.

Fat layers after centrifuge.
In most of our cases, we have noticed negligible thickness or more often absence of upper oily layer indicative of minimal trauma to adipocytes. Upper oily layer as well as lower RBC layer was discarded to yield intermediate layer of fat which is rich in viable adipocytes (Fig. 4).
Fig. 4.
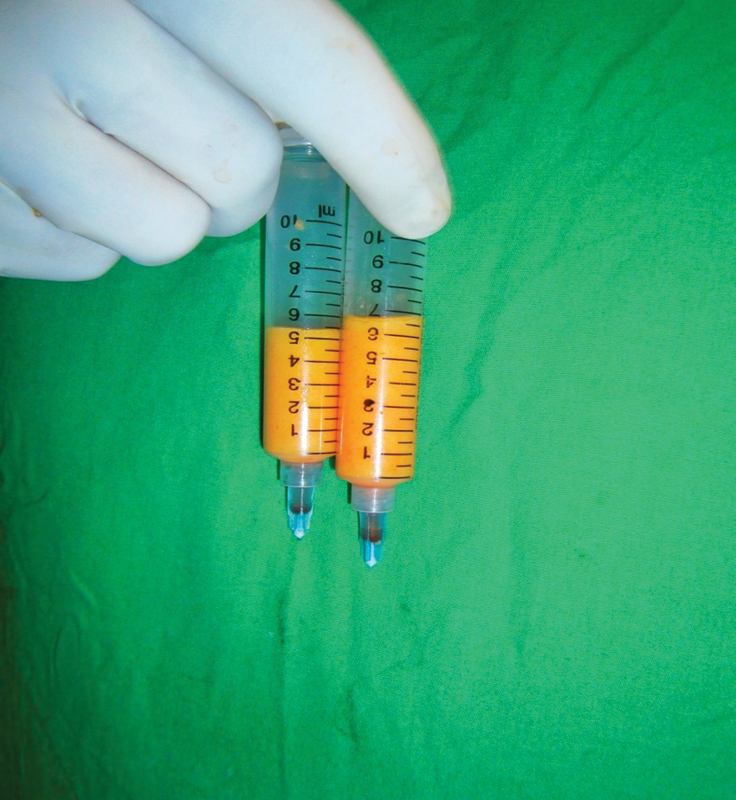
After discarding lower RBC and upper oily layer.
Placement of the fat: A 3- or 2-mL Luer lock syringe with blunt tipped cannula of 3-mm bore attached to its nozzle is used. Through small stab incision, the cannula is used to create subcutaneous tunnels in a fan-shaped manner into which the fat cells are deposited as the cannula is withdrawn. In cases of fat grafting in scarred tissue, subcision was done using 16-gauge needle. Over correction of ∼25% was done considering postoperative resorption.
-
Postoperative care:
Broad-spectrum antibiotic and anti-inflammatory drugs for 1 week.
The patient should be in semi sitting position to decrease the amount of edema.
Routine cold fermentation was advised to enhance resolution of ecchymosis and postoperative edema.
Application of antibiotic cream over the incision site twice daily.
Patient was asked to avoid pressure or massage over grafted site.
Follow-up: Every case was subjected to postoperative photography biweekly for 3 months and subsequently at 6th month, 1 year, and 2 years postoperatively. Postoperative MRI was taken at 1st and 12th months.
Clinically, results were evaluated by subjective and objective assessment.
Subjective evaluation of patients was done at 1 year in which patients were given a questionnaire as follows:
The presence of notable asymmetries in terms of volume of the treated areas (Yes/No)
The presence of nodules, infection, thickened areas, ecchymosis, or pain on either side or any other postoperative complications (Yes/No)
Their level of satisfaction scoring from 0 (very bad) to 10 (very good)
In objective assessment, preoperative and series of postoperative photographs were given to a jury consisting of another surgeon and a nurse and they were asked to evaluate outcomes by recording score from 0 (very bad) to 10 (very good).
Radiographic evaluations consist of use of MRI done using a 1.5-Tesla Siemens Sonata system (Siemens Medical Solutions, Erlangen, Germany). All patients underwent MRI scans preoperatively and 1st and 12th months postoperatively. Scans were analyzed using RadiAnt DICOM Viewer 1.0.4.4439 (Medixant Ltd, Poznan, Poland). Area of fat grafting was measured in maximum dimensions in coronal, axial, and sagittal images and subsequently compared with postoperative scans (Fig. 5).
Fig. 5.
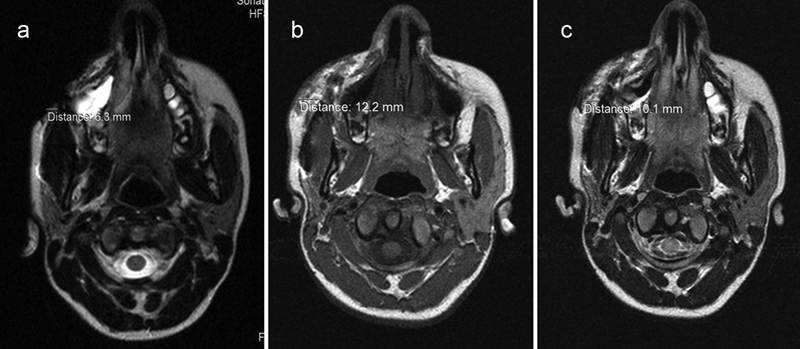
Example showing comparison of MRI scans in axial view. Preoperative MRI (a) depicting linear measurement of 6.3 mm. One month postoperative scan (b) shows grafted fat measuring 12.2 mm. One year postoperative scan (c) measuring 10.1 mm.
Results
In our study, we evaluate the efficacy of our technique of fat grafting by clinical and radiographic assessment.
Clinical Evaluation
The posttraumatic maxillofacial defects were treated in a total of 25 patients (16 males and 9 females) with mean age of 29.76 years. Subjective evaluation comprises a questionnaire given to each patient to assess notable asymmetries, postoperative complications, and overall satisfaction (Table 1). Asymmetry was recorded in 4 out of 25 patients at the end of 1 year. Three of these patients underwent second surgery of autologous fat grafting. Postoperative complications commonly encountered were pain at donor site and hematoma over the grafted site, none of which persisted beyond 4 weeks.
Table 1. Subjective and objective evaluation.
| Sr. No. | Questions | Options | Answers | Remarks | |
|---|---|---|---|---|---|
| I. Subjective Evaluation | 1 | The presence of notable asymmetries in terms of volume of the treated areas after 1st surgery | Yes | 4/25 | 16% |
| No | 21/25 | 84% | |||
| 2 | Postoperative complications | Yes | 1/25 | 4% | |
| No | 24/25 | 96% | |||
| 3 | Level of satisfaction | 0 (very bad) to 10 (very good) |
Mean score | Very good | |
| 9.1 | |||||
| II. | Objective assessment | 0 (very bad) to 10 (very good) |
Mean score | Good | |
| 8.8 | |||||
In objective evaluation, jury was asked to rate the results of each patients by seeing preoperative and series of postoperative photographs (Figs. 6 7 8 9 10 11 12). Mean of all recorded scores was 8.8 out of 10 (Table 1).
Fig. 6.

A 19-year-old boy with history of road traffic accident 3 years ago presented with depressed nasofrontal region and deviated nasal dorsum. Preoperative (Left), 1 month postoperative (Middle), and 1 year postoperative (Right) comparison after fat grafting and rhinoplasty.
Fig. 7.

A 22-year-old girl presented with old malunited zygomatico-maxillary complex fracture treated for esthetic deformity by fat grafting alone. Preoperative (Left), 1 month postoperative (Middle), and 1 year postoperative (Right) comparison post fat grafting.
Fig. 8.

Oblique view showing preoperative (Left) and 1 year postoperative (Right) comparison.
Fig. 9.

A 38-year-old patient with depressed frontonasal region following trauma, underwent fat grafting, rhinoplasty, and scar revision. Preoperative (Left), 1 year postoperative (Middle), and 2 years postoperative (Right).
Fig. 10.

A 26-year-old man with history of old trauma presented with frontonasal depression. Preoperative (Left) and 1 year after fat grafting procedure (Right).
Fig. 11.

Oblique view showing preoperative (Left) and 1 year postoperative (Right) result.
Fig. 12.

A 21-year-old patient with scarred frontal depression. Subcision was done followed by fat grafting. Preoperative (Left) and 1 year postoperative (Right) comparison.
Radiographic Evaluation
Radiographic evaluation shows consistent decrease in 1st and 12th months scan indicating resorption of fat. Difference between 1st and 12th month dimensions was calculated and expressed in percentage. Table 2 indicates average percentage of resorption from 1 month to 1 year as 21.85%.
Table 2. Evaluation by MRI scans.
| Sr. No. | Measurement in preoperative scan (mm) (A) | Measurement in 1 mo postoperative scan (mm) (B) | Measurement in 1 y postoperative scan (mm) (C) | Difference between B and C (expressed in %) |
|---|---|---|---|---|
| 1 | 0.5 | 6.7 | 5.2 | 22.39 |
| 2 | 3.4 | 10.0 | 7.8 | 22 |
| 3 | 1.8 | 4.5 | 2.8 | 37.77 |
| 4 | 2.9 | 6.3 | 3.9 | 38.09 |
| 5 | 6.3 | 12.2 | 10.1 | 17.21 |
| 6 | 2.4 | 6.0 | 3.9 | 35 |
| 7 | 1.3 | 7.4 | 5.8 | 21.62 |
| 8 | 2.5 | 7.5 | 4.8 | 36 |
| 9 | 3.9 | 8.0 | 6.8 | 15 |
| 10 | 6.1 | 13.0 | 11.2 | 13.84 |
| 11 | 7.2 | 13.1 | 10.6 | 19.08 |
| 12 | 2.4 | 7.2 | 6.0 | 16.67 |
| 13 | 3.1 | 7.0 | 6.7 | 18.57 |
| 14 | 6.0 | 12.0 | 10.3 | 14.16 |
| 15 | 1.3 | 8.3 | 6.3 | 24.09 |
| 16 | 2.0 | 5.1 | 5.0 | 1.96 |
| 17 | 3.0 | 7.1 | 6.0 | 15.49 |
| 18 | 2.2 | 8.1 | 5.9 | 27.16 |
| 19 | 5.2 | 12.2 | 10.1 | 17.21 |
| 20 | 1.8 | 11.2 | 9.0 | 19.64 |
| 21 | 5.0 | 12.0 | 9.3 | 22.50 |
| 22 | 4.7 | 9.4 | 7.3 | 22.34 |
| 23 | 3.9 | 6.8 | 4.9 | 27.94 |
| 24 | 7.1 | 12.6 | 11.1 | 11.90 |
| 25 | 4.2 | 11.2 | 8.0 | 28.57 |
| Mean | 21.85 | |||
Discussion
Posttraumatic facial deformities can be esthetically unpleasing and detrimental to social well-being of an individual. Such deformities may arise as a result of inadequate or no treatment received following trauma. Even in patients receiving prompt and appropriate treatment, unpredictable healing may result in posttraumatic facial deformities. Such defects can be very challenging to correct secondarily. Fat grafting can be considered a very powerful tool to correct posttraumatic maxillofacial deformities and it permits a long-term clinical follow-up.
Autologous fat is the closest thing to ideal filler.9 It is readily available, inexpensive, and simple to obtain. There is no risk of host rejection or other immunologic responses. The procedure may be easily performed with minimal morbidity and less recovery time. Moreover, it can avoid other conventional reconstructive procedures, with less morbidity for the patients and less costs for the society.
Major disadvantage in fat grafting procedure is its unpredictable resorption pattern. Various authors have reported variable amount of fat resorption. Based on histologic observations of free fat grafts, in 1956, Peer3 hypothesized the “cell survival theory.” The theory states that after grafting, mechanical injury and ischemia induce the death of some cells in the periphery, whereas other more centrally located cells may survive initially by plasmatic imbibition and early revascularization. Scientific literature describes an absorption rate ranging from 20 to 90%.10 11 12 13 14 15 High fat graft resorption rates have been attributed to traumatic handling of the graft during harvest, processing, and injection.
Various harvesting and preparation techniques have been suggested. The goal of these techniques is to obtain greater adipocyte cell survival and, consequently, more reliable clinical results. Commonly used aspiration techniques are lipoaspiration and syringe aspiration. It is evident in literature so far that lipoaspiration using suction apparatus is more traumatic to adipocytes than syringe aspiration.16 Therefore, in our study, we have preferred to use syringe aspiration using a 10-mL syringe. We prefer not to pull the plunger maximally, as this negative pressure can be equivalent to liposuction pressures.17
The techniques for processing the lipoaspirate are substantially more controversial than the harvest techniques. Various preparation methods have been used and compared for adipocyte viability such as sedimentation, filtration, washing, centrifugation, treatment with growth factors, or a combination of these. Smith et al17 have compared various preparatory methods such as washing with normal saline (NS), washing with ringer's lactate (RL), centrifugation, and washing plus centrifugation. They have recommended minimum manipulation of fat to yield maximum number of viable adipocytes. In our study, we have used a maximum of 500 RPM centrifugation speed. We believe that high-speed centrifugation of 2,000 to 3,000 RPM can be detrimental to adipocyte viability and thus result in higher fat resorption.
Placement of fat in posttraumatic facial defects is performed through small stab incisions preferably from two directions. Tiny parcels of fat are deposited using 3-mm blunt cannula. Such placement of tiny parcels increases surface area of fat droplets exposing it to surrounding environment, thus facilitating its nutrition through growing blood vessels.18 Fat deposition should be performed from deeper to more superficial tissues.
MRI offers a measurement tool with which to assess soft-tissue volume and density. Various authors have used MRI for objective evaluation of fat grafting.19 20 21 22 When combined with clinical evaluation, it permits precise evaluation of results with minimal error.22 Because there is no radiation risk to the patient, these scans may be used ethically in volunteers, provided that the individuals are not claustrophobic and do not have other contraindications. In this study, MRI allowed us precise quantitative comparison of preoperative and postoperative values to calculate amount of fat resorption.
In this study, fat grafting procedure has been used to correct posttraumatic facial deformities. Since healing of fat grafted region is unpredictable, we have used long-term follow-up of our operated case. Comparison was performed using facial photographs and MRI scans. Coleman's technique of fat transplantation is characterized by the placement of parcels of purified fat by multiple passes with blunt cannulas; in the beginning, it was introduced to improve facial aesthetics, and recently it was converted to perform reconstructive procedures.
Conclusion
Fat grafting can be considered a very powerful tool to correct posttraumatic maxillofacial deformities. Moreover, it can avoid other conventional reconstructive procedures with less morbidity for the patients and less costs for the society. To the best of our knowledge, fat grafting is well discussed by the scientific literature in the fields of craniofacial anomalies and facial rejuvenation, but little has been elaborated on its use in posttraumatic deformities. Although myriad varieties of harvesting and processing techniques and their combination have been studied, no single technique can be considered as gold standard. Nevertheless, in our study, gentle syringe aspiration and use of low-speed centrifuge have resulted in fairly predictable result with average resorption rate of nearly 22%. However, authors perceive that more complex case–control studies, enriched by sophisticated radiological controls, are needed to fully understand the biological behavior of the transplanted fat in the posttraumatic face and predict its long-term results.
References
- 1.Neuber G. Fett transplantation. Chir Kongr Verhandt Deutsche Gesellsch Chir. 1893;22:66. [Google Scholar]
- 2.Miller C G. Chicago, IL: Oak Press; 1926. Cannula Implants and Review of Implantation Techniques in Esthetic Surgery. [Google Scholar]
- 3.Peer L A. Loss of weight and volume in human fat grafts. Plast Reconstr Surg. 1950;5(3):217–230. [Google Scholar]
- 4.Coleman S R Structural fat grafting Aesthet Surg J 1998185386–388., 388 [DOI] [PubMed] [Google Scholar]
- 5.Niechajev I, Sevćuk O. Long-term results of fat transplantation: clinical and histologic studies. Plast Reconstr Surg. 1994;94(3):496–506. doi: 10.1097/00006534-199409000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Pinski K S, Roenigk H H Jr. Autologous fat transplantation. Long-term follow-up. J Dermatol Surg Oncol. 1992;18(3):179–184. doi: 10.1111/j.1524-4725.1992.tb02795.x. [DOI] [PubMed] [Google Scholar]
- 7.Chajchir A Benzaquen I Fat-grafting injection for soft-tissue augmentation Plast Reconstr Surg 1989846921–934., discussion 935 [PubMed] [Google Scholar]
- 8.Illouz Y G. The fat cell “graft”: a new technique to fill depressions. Plast Reconstr Surg. 1986;78(1):122–123. [PubMed] [Google Scholar]
- 9.Coleman S R. Structural fat grafts: the ideal filler? Clin Plast Surg. 2001;28(1):111–119. [PubMed] [Google Scholar]
- 10.Nguyen A Pasyk K A Bouvier T N Hassett C A Argenta L C Comparative study of survival of autologous adipose tissue taken and transplanted by different techniques Plast Reconstr Surg 1990853378–386., discussion 387–389 [PubMed] [Google Scholar]
- 11.Boyce R G, Nuss D W, Kluka E A. The use of autogenous fat, fascia, and nonvascularized muscle grafts in the head and neck. Otolaryngol Clin North Am. 1994;27(1):39–68. [PubMed] [Google Scholar]
- 12.Matsudo P K, Toledo L S. Experience of injected fat grafting. Aesthetic Plast Surg. 1988;12(1):35–38. doi: 10.1007/BF01570383. [DOI] [PubMed] [Google Scholar]
- 13.Ersek R A Transplantation of purified autologous fat: a 3-year follow-up is disappointing Plast Reconstr Surg 1991872219–227., discussion 228 [PubMed] [Google Scholar]
- 14.Fournier P F. Fat grafting: my technique. Dermatol Surg. 2000;26(12):1117–1128. [PubMed] [Google Scholar]
- 15.Coleman S R. Long-term survival of fat transplants: controlled demonstrations. Aesthetic Plast Surg. 1995;19(5):421–425. doi: 10.1007/BF00453875. [DOI] [PubMed] [Google Scholar]
- 16.Pu L L Cui X Fink B F Cibull M L Gao D The viability of fatty tissues within adipose aspirates after conventional liposuction: a comprehensive study Ann Plast Surg 2005543288–292., discussion 292 [PubMed] [Google Scholar]
- 17.Smith P, Adams W P Jr, Lipschitz A H. et al. Autologous human fat grafting: effect of harvesting and preparation techniques on adipocyte graft survival. Plast Reconstr Surg. 2006;117(6):1836–1844. doi: 10.1097/01.prs.0000218825.77014.78. [DOI] [PubMed] [Google Scholar]
- 18.Coleman S R. Facial augmentation with structural fat grafting. Clin Plast Surg. 2006;33(4):567–577. doi: 10.1016/j.cps.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 19.Wolf G A, Gallego S, Patrón A S. et al. Magnetic resonance imaging assessment of gluteal fat grafts. Aesthetic Plast Surg. 2006;30(4):460–468. doi: 10.1007/s00266-005-0202-1. [DOI] [PubMed] [Google Scholar]
- 20.Swanson E. Malar augmentation assessed by magnetic resonance imaging in patients after face lift and fat injection. Plast Reconstr Surg. 2011;127(5):2057–2065. doi: 10.1097/PRS.0b013e31820e9286. [DOI] [PubMed] [Google Scholar]
- 21.Saleh Y, Mostafa H. Clinical and radiological assessment of fat transplantation using centrifuge technique. Egypt J Plast Reconstr Surg. 2005;29(2):129–133. [Google Scholar]
- 22.Hörl H W, Feller A M, Biemer E. Technique for liposuction fat reimplantation and long-term volume evaluation by magnetic resonance imaging. Ann Plast Surg. 1991;26(3):248–258. doi: 10.1097/00000637-199103000-00007. [DOI] [PubMed] [Google Scholar]


