Abstract
To change a particular quality of care outcome within a system, quality improvement initiatives must first understand the causes contributing to the outcome. After the causes of a particular outcome are known, changes can be made to address these causes and change the outcome. Using the example of home dialysis (home hemodialysis and peritoneal dialysis), this article within this Moving Points feature on quality improvement will provide health care professionals with the tools necessary to analyze the steps contributing to certain outcomes in health care quality and develop ideas that will ultimately lead to their resolution. The tools used to identify the main contributors to a quality of care outcome will be described, including cause and effect diagrams, Pareto analysis, and process mapping. We will also review common change concepts and brainstorming activities to identify effective change ideas. These methods will be applied to our home dialysis quality improvement project, providing a practical example that other kidney health care professionals can replicate at their local centers.
Keywords: Change ideas, Root cause analysis, Home dialysis, Quality improvement, Health Personnel, Humans, kidney, peritoneal dialysis, Quality of Health Care, renal dialysis
Introduction
In the previous article in this Moving Points feature (1), an interdisciplinary team consisting of (1) a lead nurse or physician from the home dialysis unit; (2) technical experts from the predialysis clinic and in–center dialysis program (nursing staff, physician, social worker, etc.); (3) a clinical leader (i.e., manager) from the dialysis program; (4) an improvement advisor; and (5) an executive sponsor was formed with the aim of promoting home dialysis (home hemodialysis and peritoneal dialysis) uptake from its current level of 15% to a target of 30%. The team is now tasked with identifying opportunities for improvement and testing their effects on the system of care for home dialysis. The team is aware that the most effective changes target the primary or root causes of the quality of care problem. However, they are unsure how to identify the main causes for their low use of home dialysis and how to use the results of such an analysis to promote change within their dialysis unit.
Using the Institute for Healthcare Improvement Model for Improvement (2) as the framework to guide improvement work, the objectives of this article are to (1) describe the tools used to identify the main contributors to a quality of care outcome, including cause and effect diagrams, Pareto analysis, and process mapping, and (2) review common change concepts and brainstorming activities to identify effective change ideas.
Root Cause Analyses
Root cause analysis was originally developed in systems engineering to identify “the basic and causal factor(s) that underlie variation in performance.” It is now a familiar tool used by hospitals and health care organizations to identify problems and their solutions. Whereas root cause analysis has historically been used in the health care setting to investigate the cause of medical errors, it has more recently been used to address lapses in the quality of care and improve quality outcomes. Hence, it is an essential tool for quality improvement. Although other approaches to understanding problems within a system exist, including Six Sigma and Lean (1), root cause analysis is the most simplistic and easy to understand, and it is the most frequently used approach in identifying quality problems.
In any given system, most outcomes stem from a complex series of behaviors and events that occur within that system. As such, investigation into why a particular outcome occurs requires a structured approach that can identify active events (events occurring at the point of interface between humans and a complex system) and latent events (the hidden problems within a system) that contribute to the outcome. Root cause analysis provides such an approach. It is a technique that uses a structured investigational approach to understand the true causes of a particular outcome. The practice of root cause analysis, as it pertains to quality improvement efforts, is on the basis of the premise that the solution to a particular outcome is found by examining the fundamental factors that may be contributing to that outcome.
The goals of a root cause analysis as they pertain to quality improvement include (1) determining what is happening, (2) determining why the outcome is happening, and (3) determining what can be done to prevent the outcome from happening again (3). Specific to our case, root cause analysis will help the quality improvement team determine why the dialysis program is not attaining the target of 30% of patients initiating home dialysis and help facilitate potential strategies for effective change.
Tools for Root Cause Analyses
Multiple tools exist that can identify the source of problems in quality and help focus improvement efforts (4,5). Although each tool has its own purpose and therefore, yields different insights about a quality of care problem, they are complementary to one another and usually used in combination. This coapplication is especially the case for fishbone and process maps, which are almost always performed in tandem. It is important to realize that performance of the tools used in root cause analysis is dependent on the perspectives and experiences of the individuals who use them. Accordingly, it is important to include key stakeholders and frontline staff to prevent inaccuracies and omissions. Table 1 lists the tools used in the identification of quality of care problems, when to use them, and their benefits and limitations.
Table 1.
Tools used in root cause analysis and when to use them
| Tool | When to Use | Benefits | Limitations |
| Fishbone/Ishikawa/cause and effect diagrams | To brainstorm about the main causes of a quality of care outcomes/problem and the subcauses leading to each main cause | Visually displays potential root causes and allows for easy analysis; helps engage team members in an in-depth discussion of the problem, which educates the whole team; prioritizes additional analysis and helps you take corrective action | It does not single out the root cause of the problem, because all causes look equally important; it may identify causes that have little effect on the problem; it is on the basis of opinion rather than evidence |
| Process mapping | To understand all of the different steps and improvement opportunities that take place in a complicated system | Provides the opportunity to bring together multidisciplinary teams and create a culture of ownership, responsibility, and accountability; provides an overview of the complete process, helping staff to understand, often for the first time, how complicated the system is; acts as an aid to help plan effectively where to test ideas for improvements that are likely to have the most effect on the improvement aims; provides an end product, a process map that is easy to understand and highly visual | Inefficient if selecting a process that is not a priority to most of the team; need all stakeholders to be present when creating the process map; therefore, it is labor intensive and requires many resources |
| Pareto charts | To visualize which causes represent the two or three most common causes of the quality of care problem/outcome; a Pareto chart uses actual data to identify root causes, which can then be addressed with change ideas | Breaks big problem into smaller pieces; identifies most significant factors contributing to a problem/outcome; shows where to focus improvement efforts; allows better use of limited resources by focusing on the main contributors of a problem | The most common causes of problems/outcomes identified by Pareto charts may not be amenable to fixing; requires accurate identification of causes of problems/outcomes via Ishikawa diagrams |
Ishikawa or Fishbone Diagram (Cause and Effect Diagram)
The Ishikawa or fishbone diagram is used when a team seeks to understand the many potential causes contributing to the quality of care problem and focus improvement efforts on these causes (6). It can be used at many different stages of the quality improvement framework but is most often used as part of root cause analysis.
The fishbone diagram resembles the skeleton of a fish. To construct this diagram for a quality of care problem, the problem (effect) is written in a box on the far right of the diagram. A central line (spine) is next drawn to the left of the box in which the problem is recorded. Diagonal lines (fish bones) are then drawn coming off the central line (spine). These diagonal lines represent different groupings of causes of the problem. Additional lines can also be drawn off the main fish bones to represent causes of causes. The groupings are usually organized into categories such as the five Ps (patients/clients, providers, policies, processes and procedures, and place/equipment), the six Ms (machine, method, materials, measurement, man, and Mother Nature), and the four Ss (surroundings, suppliers, systems, and skills); however, the groupings should be specific to the organization and problem under study, and the quality improvement team is responsible for ensuring this specificity. After the groupings have been specified, the quality improvement team engages in a brainstorming session to determine causes specific to each grouping. This process continues until the team cannot identify any additional causes.
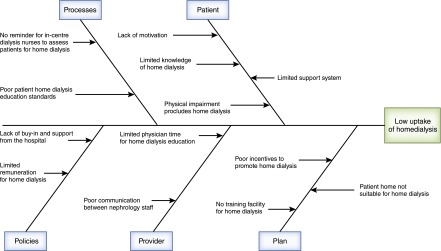
Figure 1 represents the fishbone diagram for the home dialysis quality improvement project. Using the diagram, it is clearly evident that there is a number of causes that may be contributing to the low number of patients who initiate dialysis on a home dialysis modality. It is important to remember that each potential cause is equally weighted in the fish bone diagram, and determining the root cause of the quality outcome requires the use of additional tools (described below) as well as additional discussion among the team members.
Figure 1.
The fishbone diagram for the home dialysis quality improvement project.
Pareto Analyses (Pareto Principle; 80/20 Rule)
Pareto analysis is used to categorize data so that a team can quickly identify which processes have the most effect on a quality of care outcome (6). This analysis is on the basis of the theory that a small number of processes will have the largest contribution to poor quality. As such, it follows the 80/20 rule or Pareto principle, which states that 80% of the effects/outcomes in a system are related to 20% of the causes (7). Pareto analysis is most beneficial in instances where there seems to be many processes contributing to an outcome, because it is crucial to be able to invest efforts in those processes that will have the greatest positive effect (2).
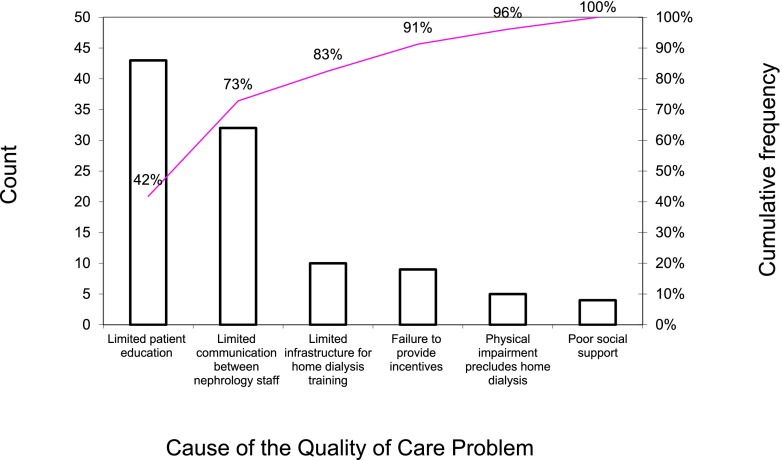
Steps to perform a Pareto analysis start with development of an Ishikawa diagram to determine the potential causes/processes contributing to a specific quality outcome. Next, a check sheet is developed. A check sheet is a structured, prepared form for collecting and analyzing data. It is used when data can be observed and collected repeatedly through various means, including clinic audits, interviews of patients and staff, and chart audits. The main applications of a check sheet include registering how often different outcomes occur and registering the frequency of the processes or potential causes that are believed to contribute to these outcomes. Creating a check sheet involves collating the list of the potential processes contributing to a quality outcome. This is done by using the results from an Ishikawa diagram to populate a column containing the potential processes/causes leading to a given outcome. Next, using a variety of methods, including clinic audits, chart audits, and interviews of patients and staff, the data collector checks off each time one of the possible causes/processes contributing to the outcome occurs. For example, if an interview is being conducted with clinic staff asking about why they think home dialysis uptake is low, then the interviewer would check off each different cause they provide, ensuring that each cause is only counted once per interviewee. It has been suggested that at least 50 causes (similar or different) are documented in this process (6). After data have been collected, their possible causes should be ranked in order of the most frequent to the least frequent, and the frequency and cumulative frequency of each presumed cause is calculated. A histogram is then created, depicting the most prevalent causes on the left and the least prevalent causes on the right (Figure 2). This exercise helps the improvement team to identify the short list of causes that contribute the most to a quality of care problem from a long list of potential causes. Change ideas can then be developed to address these common causes.
Figure 2.
A histogram depicting the most prevalent causes on the left and the least prevalent causes on the right.
For example, using the Ishikawa diagram as a reference (Figure 1), our team has hypothesized that the following six causes are the most important contributors to the low number of patients started on home dialysis: limited patient education by the nephrology staff, limited infrastructure for home dialysis training, limited communication between nephrology staff on patient modality choices, failure to provide incentives for home dialysis, limited social supports for patients, and patient physical impairments that preclude the use of home dialysis. It is important to note that, although we have chosen only six causes for illustrative purposes, all causes found within the fishbone diagram could be included in Pareto analysis to prevent the unintentional removal of an important cause. Through chart review, the improvement team has determined that the two most prevalent causes of why patients are not initially started on home dialysis are limited patient education on home dialysis modalities and limited communication between nephrology staff on patient modality choices. Hence, one change strategy that can be discussed as a next step would be for the creation of a nurse educator whose role would be to educate clinic patients about home dialysis and act as a liaison between nephrology staff. Additional discussion of change ideas will occur in subsequent sections of this paper.
Process Mapping (Flowcharts)
Process mapping (flowcharting) is a method that outlines all of the different steps in a process (2). It helps quality improvement teams to identify problems that can be fixed by breaking down a complex process into its fundamental parts. This exercise gives the improvement team clear insight into the process that it is trying to change in a number of ways, including (1) identifying the actual flow or sequence of steps in a process, (2) understanding the inner workings of and relationships between processes, (3) enabling the identification of differences between how a process actually works and how it is thought to work, (4) clarifying responsibility for work performed in a process, and (5) uncovering potential problems, bottlenecks/waits, unnecessary/nonvalue-added steps, duplication, or unnecessary complexity (2).
It is imperative that individuals who are directly involved or affected by the process create the process map, because these individuals have the greatest understanding of how the process works and how the process actually happens rather than how it should happen.
Process mapping involves a number of important steps. One of the most crucial is for the quality improvement team to determine the scope and assumptions of the mapping exercise. This involves clearly delineating the boundaries of the process (start and end points) and determining the type of process map to build (see below). The team should then begin to map the process by identifying the steps in the process. It is important that the actual—not the ideal—process be mapped. After the process map is created, it should be validated, such that individuals familiar with the process review it for clarity and content. The validation group should be comprised of individuals who were not involved in the development of the original process map. Their mandate is to analyze the process map to ensure that it accurately describes the process at hand and is clear. The input of the validation team should be shared with the original team, and modifications to the process map can be made accordingly after discussion.
Several types of process maps exist including (6) detailed, high level, and swim lane.
Detailed: Detailed process maps provide a close-up view of a process, typically showing dozens of steps. These maps make it easy to identify rework loops and complexity in a process and are most useful after teams have pinpointed issues or when they are testing changes. An example of a detailed process map can be found at http://www.hqontario.ca/portals/0/documents/qi/qi-quality-improve-guide-2012-en.pdf (6).
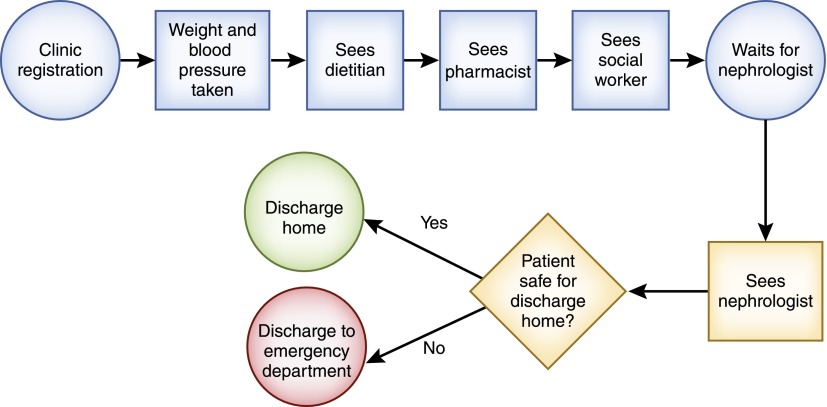
High level: This type of process map details 6–12 steps; hence, it gives a panoramic view of that process. It shows the major blocks of activity or system components in a process. It is especially useful in the early phases of a project (Figure 3).
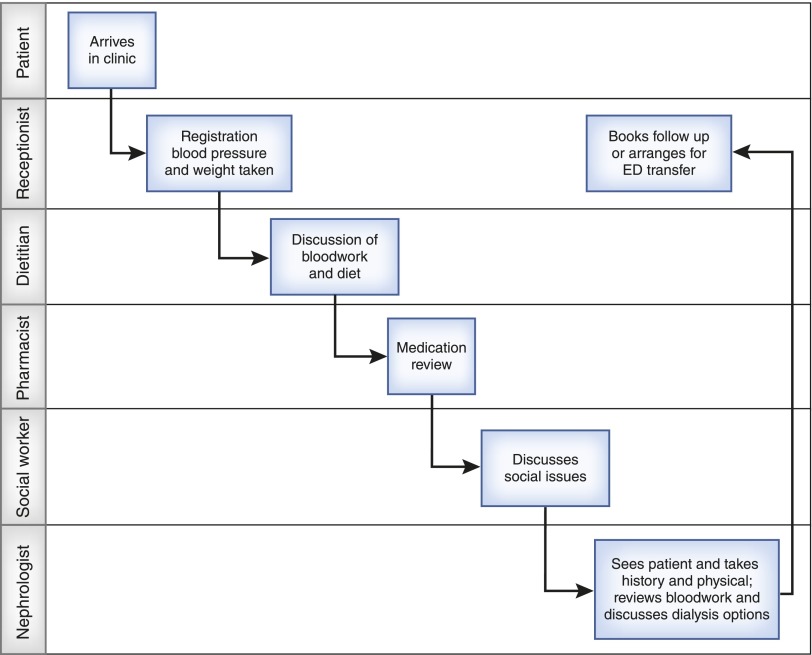
Swim lane: A swim lane process map is used to map work across different disciplines or departments. The improvement team discusses high–level process steps first, and then, each team member is asked to document his or her own individual work steps. The process map is then drawn so that each unit’s steps in the process occupy a single row or column (swim lane). This type of process map is useful for identifying handoffs where a problem might occur and keeping track of who is responsible for which steps in a complicated process. Figure 4 shows the process of a patient with CKD in a predialysis clinic. Six handoffs occur during the process: (1) the patient sees the receptionist to register and have BP and weight measured, (2) the patient sees the dietician for a discussion of diet, (3) the patient sees the pharmacist for a medication review, (4) the patient sees the social worker to discuss social issues, (5) the patient sees the nephrologist for the examination and discussion of CKD-related issues, and (6) the patient sees the receptionist again to book follow-up or facilitate transfer to the emergency department.
Figure 3.
Flow of a patient in a CKD clinic using a high–level process map.
Figure 4.
The process of a patient with CKD in a predialysis clinic. ED, emergency department.
Analysis of the process map is an important task, because it helps the team to understand the opportunities for improvement. The team should be encouraged to ask questions about the process and share their insights. Some important issues for the team to consider include (1) what drives the process, (2) whether there are inconsistencies in how the process is performed, (3) whether the process can be performed in a different way or by a different person more efficiently, (4) whether each step in the process adds value or if certain steps can be eliminated, and (5) whether the correct resources are used in the process.
It is customary to begin most quality improvement initiatives with a high–level process map, because this provides the team with a general overview of the process and prevents confusion that can arise from overly detailed mapping. Thereafter, more detailed mapping can be done as determined by the team. Our improvement team has noticed that the majority of patients who are predialysis are seen in a CKD clinic, where the majority of modality choices are made. Accordingly, the team has decided to map this process to better understand the reasons why patients are not started on home dialysis. The flow of a patient in a CKD clinic using a high–level process map is illustrated in Figure 3. Analyzing the process map shows that the nephrologist is very busy, therefore leading to a waiting period for the patient just before seeing them. The wait also pressures the nephrologist to see the patient quickly; hence, there is little time for modality education. However, if a staff member was free, he/she would be available to educate the patient just before seeing the nephrologist (hence, the idea of a nurse educator).
Tools for Identifying Change Ideas
After the main contributing or root causes of a quality problem have been identified, changes to the system/process can be made to improve it. Although all changes do not lead to improvement, all improvement requires change (8). The ability to develop, test, and implement changes is essential for any individual, group, or organization that wants to improve; however, developing effective changes can be quite challenging.
Change ideas, which are specific changes that focus on improving specific steps of a process, can be derived from a number of sources (9). These include (1) using existing changes that have been described in the literature (best practices) or from other organizations that have dealt with similar quality of care problems/outcomes, (2) using change concepts, and (3) brainstorming new innovations. Of these three sources, using existing best practices developed and tested in other organizations may be the most challenging, because these organizations may be inherently different in terms of their culture, environment, and composition. Hence, extrapolation of best practices from one setting to another may not lead to the desired effect.
Although many change ideas may be generated, it is important for the quality team to select those ideas that they feel most likely address the root cause of the quality outcome/problem. No formal process exists for prioritizing the selection of change ideas. Accordingly, through discussion, the team chooses the change ideas that they believe best target the root cause of the problem/outcome, are supported by their local stakeholders, and are easy to test.
The remainder of this article will show how to use change concepts and brainstorming to develop change ideas.
Change Concepts and Change Ideas
Although there are many kinds of changes that can lead to improvement, all changes are developed from a limited number of change concepts. A change concept is defined as a general notion or approach to change (9).
Despite being developed primarily by the manufacturing industry, change concepts are readily applicable to health care. Several resources for change concepts used in health care exist for interested readers (2,10). Some broad examples of change concepts that can help motivate change ideas include (10) the following three change concepts.
(1) Eliminating waste: This can be accomplished by recycling/reusing a product (e.g., resterilizing medical equipment), eliminating steps or resources that are not used in a process, or matching supply of a resource to its demand (e.g., decreasing dialysis staff when the dialysis unit is not busy).
(2) Designing systems to avoid mistakes: One example of this change concept is the use of reminders (e.g., computerized order entry to minimize dosing errors for patients with CKD).
(3) Changing the work environment: This change concept includes improving staff education (e.g., continuing medical education and in services) and training staff appropriately (e.g., formal training for placing personal protective equipment).
Change concepts are usually used as a starting point to generate change ideas. For example, our improvement team is tasked with increasing the number of patients new to dialysis started on home dialysis. From the previous root cause analysis exercises, important causes of this quality of care problem that the change ideas should address include improving patient education on home dialysis and improving communication between nephrology staff on patient modality choices. The change concept work environment or education could help the team to consider the change idea of adding a CKD nurse educator to the clinic team. Similarly, the change concept of work flow could lead to the change idea of weekly CKD clinic huddles to discuss patient modality choices at the same time instead of the current inconsistent system. These change ideas are actionable and can be tested by running Plan-Do-Study-Act (PDSA) cycles (1).
Brainstorming
Effective solutions to problems sometimes require creativity and innovation to facilitate change. Some of these solutions will require improvement teams to challenge the status quo (or current system) and reframe and rearrange existing information and processes. Several brainstorming tools exist to stimulate these solutions. We will describe two brainstorming tools: mental benchmarking and theory of inventive problem solving (TRIZ) exercises.
Mental benchmarking generates change ideas by identifying solutions from other industries to solve parallel problems (11). This method works by describing your quality of care problem/outcome and then asking how another industry would solve that problem. For example, to address the issue of low home dialysis knowledge by patients and caregivers, the improvement team proposes the creation of a short 2-minute video describing the different home dialysis modalities, similar to the preflight safety videos popularized in the airline industry.
TRIZ is a Russian acronym that translates to the theory of inventive problem solving. (12). TRIZ involves developing creative activities that help to challenge current thinking and practices (13). A common example of a TRIZ exercise involves taking a quality improvement objective and asking the frontline staff or improvement team how to ensure that this problem continues. A list of maladaptive activities is collated, and the activities are categorized as those that are currently taking place and those that can be changed to improve care. Specific to our case, if the goal of our team is to increase the uptake of home dialysis, the team is asked to list what can be done to ensure that no patients are started on home dialysis. This exercise could produce ideas, such as not educating patients about home dialysis, not having staff meetings about home dialysis assessments, and not discussing home dialysis with patients. The team is next asked how many of the aforementioned ideas are currently being practiced to some degree, which leads to the identification of new change ideas to be tested.
Scenario Resolution
The quality improvement team has determined the main causes of failure to increase the number of patients started on home dialysis. These causes include limited patient education by the nephrology staff, limited communication between nephrology staff on patient modality choices, and lack of a reminder for staff to assess for home dialysis suitability after a patient is on in-center hemodialysis. In consultation with the providers, patients, and management of the dialysis program, the quality improvement team has used change concepts and brainstorming exercises to generate change ideas to address the root causes. Two change ideas chosen by the improvement team include (1) adding a CKD nurse educator to the CKD clinic to improve education and potentially, communication between staff on modality choices and (2) starting weekly CKD clinic team huddles to discuss patient modality choices as a means of improving staff communication on patient modality choices.
What Are the Next Steps?
Now that change ideas have been identified to address the root causes of the dialysis unit’s low uptake of home dialysis, the next step in the model of improvement is for the team to test these change ideas using PDSA cycles. PDSA will allow the team to further refine their change ideas and determine if these changes are leading to improvement. PDSA, measurement, and improvement data interpretation will be the focus of the next article in this Moving Points feature (14).
Disclosures
None.
Acknowledgments
S.A.S. is supported by a Kidney Research Scientist Core Education and National Training Program postdoctoral fellowship (cofunded by the Kidney Foundation of Canada, the Canadian Society of Nephrology, and the Canadian Institutes of Health Research). G.M.C. is supported by a K24 midcareer mentoring award from the National Institute of Diabetes and Digestive and Kidney Diseases.
Published online ahead of print. Publication date available at www.cjasn.org.
This article is part of a Moving Points Series on quality improvement tools.
References
- 1.Silver SA, Harel Z, McQuillan R, Weizman AV, Thomas A, Chertow GM, Nesrallah G, Bell CM, Chan CT: How to begin a quality improvement project. Clin J Am Soc Nephrol 11: 893–900, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Langley GL, Moen RD, Nolan KM, Nolan TW, Norman CL, Provost LP: The Improvement Guide: A Practical Approach to Enhancing Organizational Performance, 2nd Ed., San Francisco, CA, Jossey Bass, 2009 [Google Scholar]
- 3.Wu AW, Lipshutz AK, Pronovost PJ: Effectiveness and efficiency of root cause analysis in medicine. JAMA 299: 685–687, 2008 [DOI] [PubMed] [Google Scholar]
- 4.Ziegenfuss JT Jr., McKenna CK: Ten tools of continuous quality improvement: A review and case example of hospital discharge. Am J Med Qual 10: 213–220, 1995 [DOI] [PubMed] [Google Scholar]
- 5.Ogrinc GS, Headrick LA, Moore SM, Barton AJ, Dolansky MA, Madigosky WS: Fundamentals of Health Care Improvement: A Guide to Improving Your Patient's Care, 2nd Ed., Oakbrook Terrace, IL, Joint Commission Resources, 2012 [Google Scholar]
- 6.Health Quality Ontario: Quality Improvement Guide, Toronto, Queen's Printer for Ontario, 2012
- 7.Wright A, Bates DW: Distribution of problems, medications and lab results in electronic health records: The Pareto principle at work. Appl Clin Inform 1: 32–37, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berwick DM: A primer on leading the improvement of systems. BMJ 312: 619–622, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Health Quality Ontario: Change Concepts and Ideas, Toronto, Queen's Printer for Ontario 2013
- 10.Institute for Healthcare Improvement: Using Change Concepts for Improvement, 2015. Available at: http://www.ihi.org/resources/Pages/Changes/UsingChangeConceptsforImprovement.asp. Accessed October 10, 2015
- 11.Porter-O’Grady T: M. K. Innovation Leadership: Creating the Landscape of Health Care, Sudbury, MA, Jones & Bartlett Learning, 2010 [Google Scholar]
- 12.Gao C, Guo L, Gao F, Yang B: Innovation design of medical equipment based on TRIZ. Technol Health Care 23[Suppl 2]: S269–S276, 2015 [DOI] [PubMed] [Google Scholar]
- 13.Blackstien-Hirsch P: Change Concepts, Creative Thinking, Change Ideas, Health Literacy, Institute of Health Management, Toronto, 2013 [Google Scholar]
- 14.McQuillan RF, Silver SA, Harel Z, Weizman A, Thomas A, Bell C, Chertow GM, Chan CT, Nesrallah G: How to measure and interpret quaility improvement data. Clin J Am Soc Nephrol 11: 908–914, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]