Abstract
Background
Attention deficit hyperactivity disorder (ADHD) is a common psychiatric disorder in children that can extend into adulthood and that is often associated with a variety of comorbid psychiatric disorders.
Aim
Assess the comorbidity of ADHD with anxiety disorders and depressive disorders in school-aged children, and the relationship of the severity of ADHD, anxiety, and depressive symptoms in children who have ADHD with the severity of the corresponding symptoms in their parents.
Methods
A two-stage screening process identified children 7-10 years of age with and without ADHD treated at the Xin Hua Hospital in Shanghai. ADHD and other DSM-IV diagnoses were determined by a senior clinician using the Schedule for Affective Disorder and Schizophrenia for School-Aged Children (K-SADS-PL). One parent for each enrolled child completed three self-report scales: the ADHD Adult Self Report Scale (ASRS), the State-Trait Anxiety Inventory (STAI), and the Beck Depression Inventory (BDI). In total 135 children with ADHD and 65 control group children without ADHD were enrolled; parents for 94 of the children with ADHD and 63 of the children without ADHD completed the parental assessment scales.
Results
Among the 135 children with ADHD, 27% had a comorbid anxiety disorder, 18% had a comorbid depressive disorder, and another 15% had both comorbid anxiety and depressive disorders. Parents of children with ADHD self-reported more severe ADHD inattention symptoms than parents of children without ADHD and were more likely to meet criteria for adult ADHD. Mothers (but not fathers) of children with ADHD had significantly more severe trait anxiety and depressive symptoms than mothers of children without ADHD. Among children with ADHD, the severity of ADHD symptoms was not significantly correlated with the severity of ADHD symptoms in parents, but depressive symptoms and anxiety symptoms in the children were significantly correlated with the corresponding symptoms in the parents.
Conclusion
School-aged children with ADHD commonly suffer from comorbid anxiety and depressive disorders, and the severity of these symptoms parallels the level of anxiety and depressive symptoms in their parents. Self-reported symptoms of ADHD are significantly more common in parents of children with ADHD than in parents of children without ADHD. Longitudinal studies are needed to disentangle the genetic, biological, and social factors responsible for these complex inter-relationships.
Keywords: attention deficit hyperactivity disorder, anxiety, depression, comorbidity, heritability, correlation analyses, China
Abstract
背景
在儿童中,注意缺陷与多动障碍 (attention deficit hyperactivity disorder, ADHD) 是一种常见的精神障碍,可能会持续到成人期,并且往往与多种精神疾病的共病相关。
目标
评估患有ADHD 的学龄儿童焦虑、抑郁的共病情况,以及ADHD 儿童的ADHD 症状、焦虑症状和抑郁症状的严重程度与其父母相应症状严重程度的相关性。
方法
本研究在上海新华医院进行,经过两阶段的筛选入组患有ADHD 和未患有ADHD 的7-10 岁儿童。高年资的临床医师采用学龄期儿童情感障碍与精神分裂症检查表 (Schedule for Affective Disorder and Schizophrenia for School-Aged Children, K-SADS-PL) 诊断 ADHD 与其它符合DSM-IV 诊断标准的疾病。每一个入组儿童的父亲或母亲完成三个自评量表:成人ADHD 自评量表 (ADHD Adult Self Report Scale, ASRS)、状态- 特质焦虑问卷(State-Trait Anxiety Inventory, STAI) 和 Beck 抑郁自评问卷 (Beck Depression Inventory, BDI)。 本研究共入组135 名患有ADHD 的儿童和65 名未患有 ADHD 的儿童作对照组;94 名患有ADHD 的儿童的父母和63 名未患ADHD 的儿童的父母完成了针对家长的评估量表。
结果
在135 名ADHD 儿童中,27% 的儿童共病焦虑障碍,18% 共病抑郁障碍,另外15% 同时共病焦虑和抑郁障碍。ADHD 儿童的母亲(不是父亲)与未患有的ADHD 儿童母亲相比,有更严重的注意力缺陷症状、更严重的特质性焦虑症状以及更严重的抑郁症状。 在ADHD 儿童中,ADHD 症状的严重程度与其父母的 ADHD 症状的严重程度之间无显著的相关性,但儿童的抑郁症状和焦虑症状与其父母的相应症状显著相关。
结论
学龄期ADHD 儿童常伴发焦虑、抑郁障碍。相较于未患有ADHD 的儿童的父母,ADHD 儿童的父母的自评ADHD 症状更为常见。在患有ADHD 的儿童父母中, 母亲们自我报告的焦虑症状较父亲们更为严重。我们还需要开展随访研究来理清导致这一复杂的相互关系的遗传性、生物性和社会因素。
中文全文
本文全文中文版从2016年4月25日起在http://dx.doi.org/10.11919/j.issn.1002-0829.215115可供免费阅览下载
1. Introduction
Attention deficit hyperactivity disorder (ADHD) is a common psychiatric disorder in children with the core symptoms of attention deficit, hyperactivity, and impulsiveness. It no longer appears that these children ‘outgrow’ the condition. Although some ADHD symptoms ameliorate with age,[1] many children with ADHD do not subsequently achieve the same level of functioning in adulthood as their healthy peers.[2, 3] Children with ADHD often have comorbid psychiatric disorders[4] - particularly anxiety and depressive disorders[5, 6] - that magnify their impairment and are usually associated with a poorer prognosis.
Both genetic and social factors influence the occurrence, duration, and severity of ADHD and the co-occurrence of anxiety and depressive symptoms in children with ADHD. Some studies report that the degree of heritability for ADHD is as high as 0.7 to 0.8.[7, 8] Other studies suggest a negative feedback loop by which critical feedback from parents about a child’s ADHD behaviors strains family relationships and, thus, worsens ADHD symptoms and increases the risk that the child develops comorbid mental disorders.[9, 10] Alternatively, poor adaptive skills and cognitive biases of parents can be learned by their children and, thus, increase the risk of anxiety, depression, and other mental disorders in the children.[11] Taken together, the relatively high prevalence, the often life-long impairment, and the frequent occurrence of comorbid psychiatric and behavioral disorders make ADHD an important clinical and public health problem.[12]
This case-control study aims to unravel part of this complex web of relationships by (a) comparing self-reported anxiety and depressive symptoms in school-aged children with and without ADHD; (b) comparing self-reported symptoms of ADHD, anxiety, and depression in parents of children with and without ADHD; and (c) correlating the severity of ADHD, anxiety, and depressive symptoms in children with ADHD with the severity of the corresponding symptoms in their parents.
2. Methods
We identified children with and without ADHD who were being treated at the Xin Hua Hospital (a general hospital with a large pediatric department) using a two-stage diagnostic process and assessed their level of depressive and anxiety symptoms using self-completion instruments. We also recruited one parent of each of the children and assessed their level of ADHD symptoms, depressive symptoms, and anxiety symptoms using self-completion instruments. The study recruitment process is shown in Figure 1.
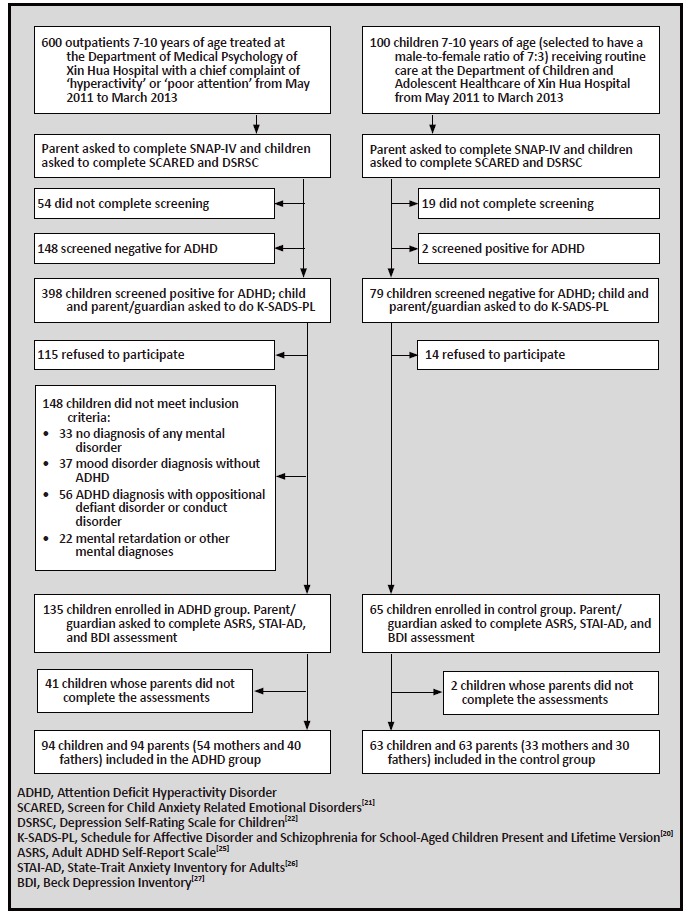
Figure 1. Recruitment of children and parents for the study
2.1. Two-stage diagnostic process
Parents or guardians of all outpatients 7 to 10 years of age at the Department of Medical Psychology of the Xin Hua Hospital with a chief complaint of ‘hyperactive’ or ‘inattentive’ are routinely asked to complete a general status questionnaire about the patient and also the parent form of the Swanson, Nolan, and Pelham Teacher and Parent Rating Scale (SNAP-IV), a self-rated screening instrument for ADHD.[13] From May 2011 to March 2013 parents or guardians of children who screened positive for ADHD on the SNAP-IV and the children themselves were invited to participate in the study. Those who provided written informed consent (283/398, 71%) were subsequently assessed by senior psychiatrists using the Schedule for Affective Disorder and Schizophrenia for School-Aged Children Present and Lifetime Version (K-SADS-PL)[14] to confirm the ADHD diagnosis and to identify any comorbid psychiatric conditions. Children were enrolled in the ADHD group for the study if they (a) met the diagnosis criteria of current ADHD; (b) had no neurological disorders; (c) had no concurrent mental disorders other than depression or anxiety disorders; and (d) the child’s parent or guardian provided written informed consent.
Over the same period, co-resident parents or guardians of 100 children 7 to 10 years of age receiving routine care (primarily for advice about nutrition or normal development) at the Department of Children and Adolescent Healthcare in Xin Hua Hospital and the children themselves were invited to participate in the study. We set the male-to-female ratio for this control group as 7:3 because previous studies[15] found this to be the gender ratio of ADHD. The parents or guardians of these children completed the general status questionnaire and the SNAP-IV; those who screened negative for ADHD on the SNAP-IV were subsequently evaluated by a senior clinician using K-SADS-PL. Children were enrolled in the control group if they (a) did not meet ADHD criteria; (b) had no neurological disorder; (c) had no mental disorders other than depression or anxiety disorders; and (d) the parent or guardian provided written informed consent.
2.2. Measures
The demographic and general status questionnaire administered to all children recorded (a) the child’s gender, age, physical development, and health history; (b) the age and educational level of the parents; (c) the pregnancy history of the mother; and (d) the economic status of the family.
The SNAP-IV Rating Scale[13] includes items that assess the ADHD criteria from the 4th edition of the Diagnostic and Statistical Manual of the American Psychiatric Association (DSM-IV).[16] Items are scored on a 4-point scale (0=not present, 1=mild, 2=moderate, 3=severe); symptoms with a score of 2 or 3 are considered present. This study used the Chinese translation of the 18-item Parent version of the scale which has two subscales; 9 items assess symptoms of inattention and 9 items assess symptoms of hyperactivity. This scale has previously been shown to have good reliability and validity.[17, 18] If the child has 6 or more of the 9 inattention items or 6 or more of the 9 hyperactivity symptoms coded as present, this is considered a positive screen for ADHD.
The K-SADS-PL is a semi-structured interview involving both the child and parent that is designed to diagnose the current and lifetime mental disorders of children between 2 and 18 years of age.[14] The English version of K-SADS-PL has good reliability and validity.[14, 19] The Chinese version of the scale[20] also has good reliability and validity.
Both groups of children also completed two self-report scales: the Screen for Child Anxiety Related Emotional Disorders (SCARED)[21] and the Depression Self-Rating Scale for Children (DSRSC).[22] SCARED is a 41-item self-report measure of a broad range of anxiety symptoms that has five subscale scores which parallel the five subtypes of anxiety in the DSM-IV: panic, generalized anxiety disorder, separation anxiety, social phobia, and school phobia. Each item is scored 0 to 2 with higher scores reflecting greater anxiety; for children aged 7 to 12, a total score over 23 indicates the existence of clinically relevant anxiety. The Chinese version of SCARED has been shown to have reasonable reliability and validity.[23]
The DSRSC[22] includes 18 items; each item is scored from 0 to 2, with higher scores indicating more severe depression. For children 8 to 12 years of age, total scores >16 for boys and total scores >15 for girls indicate clinically significant depressive symptoms. The reliability and validity of the Chinese version of DSRSC is acceptable.[24]
One parent or guardian for each child who met the inclusion criteria for the ADHD group or the control group was asked to complete three self-report instruments: the Adult ADHD Self-Report Scale (ASRS), [25] the State-Trait Anxiety Inventory for Adults (STAI-AD), [26] and the Beck Depression Inventory (BDI).[27] The ASRS is an 18-item checklist based on the ADHD diagnostic criteria in DSM-IV, 9 items assessing inattention and 9 items assessing hyperactivity. Items are rated on a 5-point Likert scale (1 to 5); scores of 4 or 5 indicate that the corresponding symptom is present. A previous study found that ASRS was a reliable and valid scale for evaluating ADHD for adults.[26] In most studies, respondents with six or more of the nine inattention symptoms or six or more of the nine hyperactivity symptoms are screened positive for Adult ADHD (a clinical interview is needed to make a final diagnosis), but Kooij and colleagues[28] suggest using four symptoms or more for either subscale as the cutoff. In this study, we considered both of these standards. The results for the 9-item inattention and the 9-item hyperactivity subscales of the ASRS are converted into an attention deficit (AD) factor score and a hyperactivity (HA) factor score by dividing the total score of the nine items for each subscale by 9 (so the theoretical range of the two factor scores is from 1 to 5).
The STAI-AD is a self-completion scale with 40 items rated on 4-point Likert scales (1 to 4); 20 items assess the temporary condition of current anxiety (‘state anxiety’, SAI) and 20 items assess the long-standing anxious personality characteristic (‘trait anxiety’, TAI). The cut-off score for clinically significant anxiety of the STAI-AD-SAI is 53 for males and 55 for females; the cutoff score of the STAI-AD-TAI is 56 for males and 57 for females. The adapted Chinese version of STAI-AD has good test-retest reliability and internal consistency.[29]
We use a 13-item version of the BDI to assess the level of depression in participating parents. The items are rated 0 to 3 with higher scores representing more severe depressive symptoms. Total BDI scores >14 are considered moderate to severe (i.e., ‘clinically significant’) depression. The reliability and validity of the Chinese version of BDI are satisfactory.[30]
2.3. Statistical analysis
Data were analyzed using SPSS 13.0. T-tests, Chi-square tests, and Fisher’s exact test were used to compare the demographic variables and the results of different measures. Pearson correlation coefficients were used to determine the association between ADHD symptoms, anxiety symptoms, and depressive symptoms in children and their parents. Multiple linear regression was used to identify the independent factors associated with the severity of self-reported anxiety and depressive symptoms in children with ADHD. All tests were two-tailed and a p-value of < 0.05 was considered statistically significant.
2.4. Ethics approval and informed consent
This study was approved by the Ethics Committee of the Xin Hua Hospital affiliated to Shanghai Jiao Tong University. All parents or guardians of the children who were screened in this study provided written informed consent for both the screening and the clinical assessments.
3. Results
3.1. Demographic characteristics of the children and their parents
As shown in Figure 1, 135 children (99 boys and 36 girls) met the enrollment criteria for the ADHD group and 65 children (46 boys and 19 girls) met the enrollment criteria for the control group. There were no statistically significant differences in age, gender, educational level of parents, or family economic status between two groups. The self-reported anxiety and depressive symptoms in children with ADHD were significantly higher than the self-reported symptoms in children without ADHD (Table 1).
Table 1. Comparison of the characteristics of children with attention deficit hyperactivity disorder (ADHD) and healthy controls who were evaluated using the Schedule for Affective Disorder and Schizophrenia for School-Aged Children Present and Lifetime Version (K-SADS-PL)[20]
| characteristic | children with ADHD (n=135) |
children without ADHD (n=65) |
statistic | p-value |
|
a Screen for Child Anxiety Related Emotional Disorders (SCARED)[21] b Depression Self-Rating Scale for Children (DSRSC)[22] | ||||
| mean (sd) age of child | 8.8 (1.4) | 9.2 (0.5) | t=1.23 | 0.109 |
| number (%) male children | 99 (73%) | 46 (71%) | X2=0.08 | 0.777 |
| mean (sd) years of fathers’ education | 14.9 (4.0) | 15.5 (4.1) | t=1.84 | 0.066 |
| mean (sd) years of mothers’ education | 12.4 (3.0) | 13.3 (3.1) | t=1.49 | 0.087 |
| mean (sd) age of father | 37.5 (3.8) | 36.9 (3.7) | t=1.85 | 0.066 |
| mean (sd) age of mother | 34.2 (4.3) | 33.8 (4.2) | t=1.35 | 0.099 |
| mean (sd) annual household income in 10, 000 Renminbi | 20.2 (9.3) | 22.7 (8.3) | t=0.63 | 0.527 |
| mean (sd) total score on self-report anxiety scalea | 18.3 (7.5) | 8.1 (5.9) | t=10.45 | <0.001 |
| mean (sd) total score on self-report depression scaleb | 10.8 (5.2) | 3.1 (2.5) | t=14.14 | <0.001 |
As shown in Figure 1, 94 parents of children with ADHD (54 mothers and 40 fathers) completed the three self-report scales and 63 parents of children without ADHD (33 mothers and 30 fathers) completed the scales. There were no statistically significant differences in the gender (X2=0.39, p=0.531), age (t=1.00, p=0.320), or years of education (t=0.97, p=0.334) between these two groups of participating parents.
3.2. Comorbidity of depression and anxiety disorder among ADHD children
Based on the diagnosis of the senior clinician who administered the K-SADS-PL, among the 135 children with current ADHD, 37 (27.4%) had a comorbid anxiety disorder without a depressive disorder, 24 (17.8%) had a comorbid depressive disorder without an anxiety disorder, 20 (14.8%) had both a comorbid anxiety disorder and a comorbid depressive disorder, and 54 (19.3%) did not meet the diagnostic criteria of either an anxiety disorder or a depressive disorder. Among the 57 (42.2%) children in the ADHD group with a comorbid anxiety disorder, the specific disorders were as follows: 20 (35.1%) had generalized anxiety disorder, 12 (21.1%) had separation anxiety disorder, 5 (8.8%) had obsessive compulsive disorder, 10 (17.5%) had specific phobias, and 10 (17.5%) had an anxiety disorder not otherwise specified (NOS). The 44 (32.6%) children in the ADHD group with a comorbid depressive disorder were not sub-classified into the specific disorders.
None of the 65 children in the control group met the diagnosis for a depressive disorder or an anxiety disorder.
3.3. Self-reported symptoms of ADHD in parents of children with and without ADHD
The results of the ADHD Adult Self Report Scale (ASRS) for the 94 parents of children with ADHD and the 63 parents of children without ADHD are shown in Table 2. For fathers, the total ASRS score and the attention deficit (AD) and hyperactivity (HA) factor scores of the ASRS were not significantly different between groups, but the proportion that screened positive for ADHD using the 6+ symptoms criteria (i.e., 6 or more of the 9 symptoms on either the inattention or hyperactivity subscale) was higher among fathers of children with ADHD than among fathers without ADHD (32.5% versus 10.0%, Fisher exact test, p=0.042). Among the mothers the differences between groups were greater: the total ASRS score, the AD factor score of the ASRS, and the proportion of mothers who screened positive for ADHD using both the 6+ symptoms criteria and the 4+ symptoms criteria were significantly greater among mothers of children with ADHD than among mothers of children without ADHD.
Table 2. Comparison of self-reported symptoms of attention deficit hyperactivity disorder (ADHD) among parents of children with and without ADHD based on results of the ADHD Adult Self Report Scale (ASRS)[25]
| subscale | parents of children with ADHD |
parents of children without ADHD |
statistic | p-value |
|
a comparison of fathers and mothers in the ADHD group: ASRS total score (t=1.97, p=0.050), % positive for ADHD using ≥6 symptoms
present for either the attention or hyperactivity subscale as cutoff (p=0.961), % positive for ADHD using ≥4 symptoms as cutoff
(p < 0.001), ASRS AD factor score (t=1.04, p=0.300), ASRS HA factor score (t=3.52, p=0.001). b comparison of fathers and mothers in the control group: ASRS total score (t=0.38, p=0.701), % positive for ADHD using ≥6 symptoms present for either the attention or hyperactivity subscale as cutoff (p < 0.001), % positive for ADHD using ≥4 symptoms as cutoff (p < 0.001), ASRS AD factor score (t=2.97, p=0.004), ASRS HA factor score (t=1.13, p=0.263). | ||||
| ALL PARENTS | n=94 | n=63 | ||
| Total ASRS score, mean (sd) | 41.9 (10.9) | 37.6 (10.1) | t=2.54 | 0.012 |
| ASRS attention deficit (AD) factor score, mean (sd) | 2.8 (0.6) | 2.5 (0.4) | t=3.73 | < 0.001 |
| ASRS hyperactivity (HA) factor score, mean (sd) | 2.0 (0.4) | 1.9 (0.4) | t=1.41 | 0.159 |
| Screen positive for ADHD (≥6 symptoms rated as present in either 9-item ASRS subscale), n (%) |
31 (33.0%) | 3 (4.8%) | exact test | < 0.001 |
| Screen positive for ADHD (≥4 symptoms rated as present in either 9-item ASRS subscale), n (%) |
41 (43.6%) | 14 (22.2%) | exact test | 0.006 |
| FATHERS | n=40a | n=30b | ||
| Total ASRS score, mean (sd) | 40.1 (10.0) | 37.2 (11.7) | t=1.09 | 0.282 |
| ASRS attention deficit (AD) factor score, mean (sd) | 2.8 (0.5) | 2.8 (0.4) | t=0.00 | 1.000 |
| ASRS hyperactivity (HA) factor score, mean (sd) | 1.8 (0.5) | 1.8 (0.3) | t=0.00 | 1.000 |
| Screen positive for ADHD (≥6 symptoms rated as present in either 9-item ASRS subscale), n (%) |
13 (32.5%) | 3 (10.0%) | exact test | 0.042 |
| Screen positive for ADHD (≥4 symptoms rated as present in either 9-item ASRS subscale), n (%) |
13 (32.5%) | 5 (16.7%) | exact test | 0.172 |
| MOTHERS | n=54a | n=33b | ||
| Total ASRS score, mean (sd) | 43.2 (11.5) | 37.9 (8.5) | t=2.48 | 0.021 |
| ASRS attention deficit (AD) factor score, mean (sd) | 2.7 (0.4) | 2.5 (0.4) | t=2.28 | 0.034 |
| ASRS hyperactivity (HA) factor score, mean (sd) | 2.2 (0.6) | 1.7 (0.4) | t=1.82 | 0.072 |
| Screen positive for ADHD (≥6 symptoms rated as present in either 9-item ASRS subscale), n (%) |
18 (33.0%) | 0 (0.0%) | exact test | < 0.001 |
| Screen positive for ADHD (≥4 symptoms rated as present in either 9-item ASRS subscale), n (%) |
28 (51.9%) | 9 (27.3%) | exact test | 0.028 |
For both fathers and mothers in both groups, the mean factor score for the attention deficit subscale of ASRS was significantly greater than the mean factor score for the hyperactivity subscale of the ASRS (all p-values < 0.001). As shown in the footnote to Table 2, among parents of children with ADHD, the ASRS total score and the HA factor score were significantly higher in mothers than in fathers, and the proportion of mothers screening positive for ADHD using the relaxed criteria (i.e., >4 symptoms on either of the subscales) was significantly greater than the proportion of fathers screening positive for ADHD. However, the results were different among parents with children who did not have ADHD: the total ASRS and the HA factor score of the ASRS were similar in mothers and fathers but fathers had significantly greater AD factor scores than mothers; a significantly higher proportion of fathers than mothers screened positive for ADHD using the ≥6 symptoms criteria while the reverse was the case when using the ≥4 symptoms criteria.
3.4. Self-reported anxiety and depressive symptoms in parents of children with and without ADHD
The self-reported anxiety and depressive symptoms of parents of children with and without ADHD are shown in Table 3. There were no significant differences in the self-reported severity of anxiety or depressive symptoms between fathers of children with ADHD and fathers of children without ADHD. However, mothers of children with ADHD self-reported significantly more severe trait anxiety symptoms (STAI-AD-TAI) and significantly more severe depressive symptoms than mothers of children without ADHD. As shown in the footnote to Table 3, in both groups of parents, mothers reported more severe anxiety and depressive symptoms than fathers, but these differences between mothers and fathers only reached statistical significance for state anxiety and trait anxiety among parents who had children with ADHD and for state anxiety among parents who did not have children with ADHD.
Table 3. Comparison of self-reported anxiety symptoms and depressive symptoms among parents of children with and without ADHD
| parents of children with ADHD mean (sd) |
parents of children without ADHD mean (sd) |
t-test (p-value) | |
|
STAI-AD-SAI, State-Trait Anxiety Inventory for Adult-State-Anxiety scale[26] STAI-AD-TAI score, State-Trait Anxiety Inventory for Adult-Trait-Anxiety scale[26] BDI, Beck Depression Inventory[27] a compare fathers and mothers in ADHD group: STAI-AD-SAI (t=4.14, p < 0.001), STAI-AD-TAI (t=2.37, p=0.020), and BDI (t=1.85, p=0.068) b compare fathers and mothers in control group: STAI-AD-SAI (t=2.11, p=0.039), STAI-AD-TAI (t=0.66, p=0.511), and BDI (t=0.91, p=0.366) | |||
| ALL PARENTS | n=94 | n=63 | |
| STAI-AD-SAI | 43.0 (7.6) | 41.4 (8.4) | 1.21 (0.226) |
| STAI-AD-TAI | 45.1 (8.3) | 40.7 (7.2) | 3.53 (0.001) |
| BDI | 4.8 (2.2) | 4.7 (1.3) | 0.36 (0.721) |
| FATHERS | n=40a | n=30b | |
| STAI-AD-SAI | 39.3 (8.7) | 39.4 (8.9) | 0.05 (0.963) |
| STAI-AD-TAI | 42.8 (8.0) | 40.1 (6.8) | 1.52 (0.131) |
| BDI | 4.3 (1.7) | 4.5 (1.1) | 0.60 (0.552) |
| MOTHERS | n=54a | n=33b | |
| STAI-AD-SAI | 45.7 (5.2) | 43.2 (4.5) | 1.39 (0.172) |
| STAI-AD-TAI | 46.8 (8.2) | 41.3 (7.6) | 3.20 (< 0.001) |
| BDI | 5.1 (2.5) | 4.8 (1.5) | 2.21 (< 0.001) |
Among the 34 parents who screened positive for ADHD using the criteria of >6 symptoms on one or both of the ASRS subscales, 10 (29.4%) had clinically significant anxiety symptoms (i.e., STAI-AD-SAI>53 or STAI-AD-TAI>56 for males; STAI-AD-SAI>55 or STAI-ADTAI> 57 for females) and 3 (8.8%) had clinically significant depressive symptoms (i.e., BDI>14). Among the 55 parents that screened positive for ADHD using the 4+ symptoms criteria on the ASRS, 12 (21.8%) reported clinically significant anxiety symptoms and 5 (9.1%) reported clinically significant depressive symptoms.
3.5. Correlations of severity of ADHD symptoms, anxiety symptoms, and depressive symptoms in children with ADHD and their parents
As shown in Table 4, the severity of self-reported ADHD symptoms in parents of children with ADHD (i.e., the total score on the ASRS) is not significantly correlated with the severity of ADHD symptoms in their children. However, the severity of anxiety symptoms of parents of children with ADHD is significantly associated with both the severity of anxiety symptoms and of depressive symptoms in their children, and the severity of parents’ depressive symptoms is significantly correlated with the severity of depressive symptoms in their children. Among the parents, depressive and anxiety symptoms are significantly correlated with each other, but this is not the case among the children with ADHD.
Table 4. Correlation of parental report of the severity of child’s symptoms of attention deficit hyperactivity disorder (ADHD) and child’s self-report of anxiety, and depression with severity of parent’s selfreport of ADHD symptoms, anxiety, and depression in 94 children with ADHD and their parentsa, b
| factor | ADHD symptoms of parents r(p) |
anxiety symptoms of parents r(p) |
depressive symptoms of parents r(p) |
ADHD symptoms of children r(p) |
anxiety symptoms of children r(p) |
|
a For parents, the severity of ADHD symptoms is the total score of the ADHD Adult Self Report Scale (ASRS)[25]; the severity of anxiety
symptoms is the combined total score of the State-Trait Anxiety Inventory for Adult -State-Anxiety scale(STAI-AD-SAI)[26] and the State-
Trait Anxiety Inventory for Adult-Trait-Anxiety scale (STAI-AD-TAI)[26]; and the severity of depressive symptoms is the total score of
the Beck Depression Inventory (BDI)[27]. For children, the severity of ADHD symptoms is the total score of the parent version of the
Swanson, Nolan and Pelham Teacher and Parent Rating Scale (SNAP-IV)[18]; the severity of anxiety symptoms is the total score of the
self-completion Screen for Child Anxiety Related Emotional Disorders (SCARED)[21]; and the severity of depressive symptoms is the total
score on the Depression Self-Rating Scale for Children (DSRSC)[22] b The results when using rank (Spearman) correlation coefficients are very similar to the results presented in this table based on Pearson correlation coefficients. | |||||
| anxiety symptoms of parents |
0.27 (0.325) | 1 | |||
| depressive symptoms of parents |
0.24 (0.273) | 0.70 (< 0.001) | 1 | ||
| ADHD symptoms of children |
0.35 (0.342) | 0.32 (0.325) | 0.25 (0.287) | 1 | |
| anxiety symptoms of children |
0.30 (0.322) | 0.58 (< 0.001) | 0.26 (0.293) | 0.36 (0.472) | 1 |
| depressive symptoms of children |
0.29 (0.304) | 0.45 (0.001) | 0.59 (0.030) | 0.38 (0.353) | 0.22 (0.292) |
As shown in Table 5, a multivariate regression analysis that used the self-reported severity of anxiety symptoms in children with ADHD (based on the SCARED total score) as the dependent variable and the severity of parents’ self-reported anxiety symptoms, parents’ self-reported depressive symptoms, and the child’s self-reported depressive symptoms as independent variables found that the severity of parental anxiety symptoms was the most important predictor of the severity of the child’s anxiety symptoms. A parallel analysis that used the self-reported severity of depressive symptoms in children with ADHD (i.e., the total DSCRC score) as the dependent variable and the severity of parents’ self-reported anxiety symptoms, parents’ self-reported depressive symptoms, and the child’s self-reported anxiety symptoms as independent variables found that the severity of parental depressive symptoms was the most important predictor of the severity of the child’s depressive symptoms.
Table 5. Multiple linear regression of factors associated with the self-reported severity of anxiety and depressive symptoms among 94 children with attention deficit hyperactivity disorder (ADHD)
| factors | factors associated with severity of child’s anxiety symptoms (R2=0.483) |
factors associated with severity of child’s depressive symptoms(R2=0.423) |
||
| standardized regression coefficient (Beta) |
t (p-value) | standardized regression coefficient (Beta) |
t (p-value) | |
| a For parents, the severity of anxiety symptoms is the combined total score of the State-Trait Anxiety Inventory for Adult-State-Anxiety scale (STAI-AD-SAI)[26] and the State-Trait Anxiety Inventory for Adult-Trait-Anxiety scale (STAI-AD-TAI)[26]; and the severity of depressive symptoms is the total score of the Beck Depression Inventory (BDI)[27]. For children, the severity of anxiety symptoms is the total score of the self-completion Screen for Child Anxiety Related Emotional Disorders (SCARED)[21]; and the severity of depressive symptoms is the total score on the Depression Self-Rating Scale for Children (DSRSC)[22] | ||||
| severity of parent’s anxiety symptoms |
1.071 | 8.43 (< 0.001) | -0.252 | -1.20 (0.243) |
| severity of parent’s depressive symptoms |
-0.107 | -0.70 (0.493) | 1.361 | 3.35 (< 0.001) |
| severity of child’s anxiety symptoms | ---- | ---- | 0.119 | 1.42 (0.178) |
| severity of child’s depressive symptoms |
0.159 | 1.85 (0.078) | ---- | ---- |
4. Discussion
4.1. Main findings
Our results found that children with ADHD had relatively high rates of comorbid anxiety disorders and depressive disorders. This confirms results from other studies: prior research reported rates of comorbid anxiety disorders in ADHD of 13 to 51% (our rate was 42%) and rates of comorbid depressive disorders with ADHD of 12 to 50% (our rate was 33%).[6, 31] We also found that parents who screened positive for ADHD reported relatively high rates of clinically significant anxiety or depressive symptoms, further confirming the relationship between these different conditions.
Our results found that children with ADHD had relatively high rates of comorbid anxiety disorders and depressive disorders. This confirms results from other studies: prior research reported rates of comorbid anxiety disorders in ADHD of 13 to 51% (our rate was 42%) and rates of comorbid depressive disorders with ADHD of 12 to 50% (our rate was 33%).[6, 31] We also found that parents who screened positive for ADHD reported relatively high rates of clinically significant anxiety or depressive symptoms, further confirming the relationship between these different conditions.
A previous study by Brown[32] suggested that comorbid anxiety may mute the hyperactivity symptoms of ADHD and magnify the inattention symptoms of ADHD. Another study[33] considered the possibility that comorbid depression in children with ADHD was actually a secondary depression due to the social problems that arise for children with ADHD but concluded that in most cases these were independent, co-occurring conditions. Our finding of no relationship between the severity of ADHD symptoms and the severity of anxiety or depressive symptoms in children with ADHD or in the parents of children with ADHD provides support for the hypothesis about the independence of these co-occurring conditions. Further analyses of the correlationship of anxiety and depressive symptoms with the severity of the different subtypes of ADHD (inattention and hyperactivity) are needed to refine these findings. These types of analyses of the subtypes of ADHD may help in identifying shared risk factors and prioritizing different treatment strategies.[34]
We found significantly higher trait anxiety in mothers of children with ADHD than in mothers of children without ADHD, but similar levels of state anxiety in the two groups of mothers. This appears counter-intuitive: current depressive symptoms are higher in mothers of children with ADHD, so one would expect that current, environment-related state anxiety would also be higher. However, previous research suggests that the relationship of anxiety symptoms with ADHD may be more complex, simultaneously influenced by environmental, personality, and genetic factors.[35, 36, 37]
We found strong correlations (r > 0.50) between the self-reported severity of anxiety and depressive symptoms of children with ADHD and the selfreported ratings of the corresponding symptoms in their parents, relationships that remained robust even after adjusting for potential confounding variables by including them in a multiple linear regression analysis. Several studies discuss the influence of anxiety and depressive symptoms in parents (primarily mothers) on the corresponding symptoms in their children.[38, 39, 40] Our study confirms this relationship in the special population of children with ADHD, but much more detailed genetic, diagnostic, and social history analyses will be needed to differentiate the relative importance of biological and social factors.
Applying DSM-IV criteria for ADHD - which are focused on activities of children - to diagnose adult ADHD is problematic.[1] A related problem is that the symptom pattern of ADHD changes with age: external hyperactivity and impulsiveness symptoms tend to improve with age while the inattention symptoms, which have a greater impact on cognitive functioning, are likely to persist into adolescence or adulthood.[1, 41, 42] Our finding that self-reported inattention symptoms were significantly more prominent than self-reported hyperactivity symptoms in the parents of children with ADHD provides indirect support for this finding, but parents of children without ADHD also had more prominent self-reported symptoms of inattention than hyperactivity, so this may be a population-wide phenomenon that is not specific to parents of ADHD children.
4.2. Limitations
This is a case-control study in a clinical sample of patients 7-10 years old with ADHD from one hospital in Shanghai in which a relatively high proportion of potential participants who screened positive for ADHD on a parental screening form (115 of 398, 29%) refused to participate in the study. Thus, it is uncertain how representative this sample is of all children with ADHD in China. The diagnostic assessment of the children was quite rigorous, but the classification of the severity of depression and anxiety in both the patients and their parents and the determination of possible adult ADHD in the parents were all based on self-report measures, so they were susceptible to a variety of biases (e.g., recall bias) that we were unable to control for in the analysis. Only one of the parents of each participating child completed the study instruments, so the comparisons between mothers and fathers within each group were potentially confounded by differences in the children and in the family environment of the mothers and fathers. The depressive measures for children and their parents (DSRSC and BDI) and the anxiety measure for the children (SCARED) assessed current symptoms at the time of the survey, so they did not reflect the long-term or mean level of anxiety and depressive symptoms. Rigorous clinical evaluations of the depressive and anxiety symptoms in children and their parents and, most importantly, clinical confirmation of the adult ADHD diagnosis in the parents would be needed to confirm the results suggested by analysis of the self-report measures used in this study. Moreover, long-term follow-up studies of patients and their parents are needed to clarify the interaction between the psychological symptoms of children with ADHD and their parents and to describe the different clinical trajectories of children with ADHD who do and do not have comorbid conditions.
4.3. Implications
This study of a Chinese clinical sample of children with ADHD confirms the reported high prevalence of comorbid anxiety and depression among children with ADHD that has been previously reported in other countries. The relatively high prevalence of self-reported ADHD symptoms among the parents of children with ADHD (particularly the mothers) supports reports about the heritability of ADHD, but more detailed clinical examinations and detailed histories from parents of children with ADHD will be needed to confirm this finding. The much higher level of depressive and anxiety symptoms among mothers of children with ADHD than among fathers, suggests that the burden for caring for the children is more likely to fall on the mother rather than on the father; but it was trait anxiety (not state anxiety) that was elevated, so there may be personality factors involved that are unrelated to the stress of caring for a child with ADHD. Finally, the strong correlation of the severity of anxiety and depressive symptoms between children with ADHD and their parents probably reflects both genetic and environmental influences.
Acknowledgments
The authors thank the clinicians in the Departments of Medical Psychology and Child and Adolescent Health Care at Xin Hua Hospital who helped in the recruitment and assessment of study participants.
Biography

Dr. Weiping Xia received a master’s degree from the Mental Health Institute of Central South University in 2007 and has worked in the Department of Medical Psychology at Xin Hua Hospital affiliated to Shanghai Jiao Tong University School of Medicine since July 2007. Currently an attending psychiatrist, she is starting a PhD. program at the Shanghai Mental Health Center of the Shanghai Jiao Tong University School of Medicine in 2013. Her primary clinical and research interests include the symptomatology and pathogenesis of attention deficit hyperactivity disorder (ADHD) and clinical and imaging studies of depression.
Funding Statement
This study was supported by Medical Planning Program of Papers Prize Plan for Collaborative School Education, Social Science and Medical Research (YX10004).
Footnotes
Conflict of interest statement: The authors declare no conflict of interest.
Informed consent: All parents or guardians of the children who were screened in this study provided written informed consent for both the screening and the clinical assessments.
Ethics approval: The ethics committee of the Xin Hua Hospital approved the study.
Authors' contribution: XWP performed the statistical analysis and wrote the first draft of the manuscript. SLX provided valuable advice on the protocol and revised the draft manuscript. ZJS designed the protocol and supervised the conduct of the study. All authors approved the final manuscript.
References
- 1.Faraone S V, Biederman J, MickE The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36(2):159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- 2.Biederman J, Faraone SV, Taylor A, Sienna M, Williamson S, Fine C. Diagnostic continuity between child and adolescent ADHD: findings from a longitudinal clinical sample. J Am Acad Child Adolesc Psychiatry. 1998;37(3):305–313. doi: 10.1097/00004583-199803000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Spencer TJ, Biederman J, Wilens TE, Faraone SV. Overview and neurobiology of attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2002;63(12):3–9. [PubMed] [Google Scholar]
- 4.Pliszka SR. Comorbidity of attention-deficit/hyperactivity disorder with psychiatric disorder: an overview. J Clin Psychiatry. 1998;59(7):50–58. [PubMed] [Google Scholar]
- 5.McGough JJ, Barkley RA. Diagnostic controversies in adult attention deficit hyperactivity disorder. Am J Psychiatry. 2004;161(11):1948–1956. doi: 10.1176/appi.ajp.161.11.1948. [DOI] [PubMed] [Google Scholar]
- 6.Biederman J, Newcorn J, Sprich S. Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. Am J Psychiatry. 1991;148(5):564–577. doi: 10.1176/ajp.148.5.564. [DOI] [PubMed] [Google Scholar]
- 7.Sprich S, Biederman J, Crawford MH, Mundy E, Faraone SV. Adoptive and biological families of children and adolescents with ADHD. J Am Acad Child Adolesc Psychiatry. 2000;39(11):1432–1437. doi: 10.1097/00004583-200011000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Faraone SV, Mick E. Molecular genetics of attention-deficit/hyperactivity disorder. Psychiatr Clin North Am. 2010;33(1):159–180. doi: 10.1016/j.psc.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Low SB, Stocker C. Family functioning and children’s adjustment: associations among parent’s depressed mood, marital hostility, parent-child hostility and children’s adjustment. J Fam Psychol. 2005;19(3):394–403. doi: 10.1037/a0027944. [DOI] [PubMed] [Google Scholar]
- 10.Harpin VA. The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Arch Dis Child. 2005;90(1):12–17. doi: 10.1136/adc.2004.059006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Field AP. The behavioral inhibition system and the verbal information pathway to children’s fears. J Abnorm Psychol. 2006;115(4):742–752. doi: 10.1037/0021-843X.115.4.742. [DOI] [PubMed] [Google Scholar]
- 12.Kessler RC, Lenard A, Russell B, Joseph B, Keith C, Olga D, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(4):716–723. doi: 10.1176/appi.ajp.163.4.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Swanson JM. School-Based Assessments and Interventions for ADD Students. Irvine, CA: KC publishing. 1992 [Google Scholar]
- 14.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Aged Children Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–989. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 15.Jin W, Du Y, Zhong X, David C. Prevalence and contributing factors to attention deficit hyperactivity disorder: a study of five-to fifteen-year-old children in Zhabei District, Shanghai. Asia Pac Psychiatry. 2014;6(4):397–404. doi: 10.1111/appy.12114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington: American Psychiatric Association; 1994. [Google Scholar]
- 17.Gau SS, Shang CY, Liu SK, Lin CH, Swanson JM, Liu YC, Tu CL. Psychometric properties of the Chinese version of the Swanson, Nolan, and Pelham, version IV scale -parent form. Int J Methods Psychiatr Res. 2008;17(1):35–44. doi: 10.1002/mpr.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Su LY, Geng YG, Wang H, Du YS, Sun L, Zhao FT, et al. [Norm of ADHD Diagnostic Scale-Parent Version in Chinese urban children]. Zhongguo Shi Yong Er Ke Za Zhi. 2006;21(11):833–836. doi: 10.3969/j.issn.1005-2224.2006.11.013. Chinese. [DOI] [Google Scholar]
- 19.Birmaher B, Ehmann MD, Goldstein B, Monk K, Kalas C, Kupfer D, et al. Schedule for Affective Disorders and Schizophrenia for School-age Children (K-SADS-PL) for the assessment of preschool children – a preliminary psychometric study. J Psychiatr Res. 2009;43(7):680. doi: 10.1016/j.jpsychires.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhou JB, Guo LT, Chen Y. Reliability and validity of the Chinese version of Swanson, Nolan, and Pelham Version IV Rating Scale-Parent Form for attention-deficit/hyperactivity disorder. 2013;7(6):424–428. doi: 10.3969/j.issn.1000-6729.2013.06.005. [DOI] [Google Scholar]
- 21.Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. Am Acad Child Adolesc Psychiatry. 1999;38(10):1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Birleson P. The validity of depressive disorder in childhood and the development of a self-rating scale: a research report. J Child Psychol Psychiat. 1981;22(1):73–88. doi: 10.1111/j.1469-7610.1981.tb00533.x. [DOI] [PubMed] [Google Scholar]
- 23.Wang K, Su LY, Zhi Y, Zhou J, Yang ZW, Zhang JS. [Norms of the screen for child anxiety related emotional disorders in Chinese urban children]. Zhongguo Lin Chuang Xin Li Xue Za Zhi. 2002;10(4):270–272. doi: 10.3969/j.issn.1005-3611.2002.04.009. Chinese. [DOI] [Google Scholar]
- 24.Su LY, Wang K, Zhu Y, Luo XR, Yang ZW. [Norm of The Depression Self-rating Scale for children in Chinese urban children]. Zhongguo Xin Li Wei Sheng Za Zhi. 2003;17(8):547–549. doi: 10.3321/j.issn:1000-6729.2003.08.011. Chinese. [DOI] [Google Scholar]
- 25.Adler LA, Spencer T, Faraone SV. Validity of pilot Adult ADHD Self-Report Scale (ASRS) to rate adult ADHD symptoms. Ann Clin Psychiatry. 2006;18(3):145–148. doi: 10.1080/10401230600801077. [DOI] [PubMed] [Google Scholar]
- 26.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983 [Google Scholar]
- 27.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory of measuring depression. Arch Gen Psychiatry. 1961;4:53–63. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 28.Kooij JJ, Buitelaar JK, van den Oord EJ, Furer JW, Rijnders CA, Hodiamont PP. Internal and external validity of attention-deficit hyperactivity disorder in a population-based sample of adults. Psychol Med. 2005;35(6):817–827. doi: 10.1017/s003329170400337x. [DOI] [PubMed] [Google Scholar]
- 29.Zhen XH, Shu L, Zhang AL, Huang GL, Zhao JF, Sun M. [The test report of State-Trait Anxiety Inventory in Changchun]. Zhongguo Xin Li Wei Sheng Za Zhi. 1993;7(2):60–62. Chinese. [Google Scholar]
- 30.Zhang YX, Wang Y, Qian MY. [The reliability and validity of the Beck Depression Scale]. Zhongguo Xin Li Wei Sheng Za Zhi. 1990;4(4):164–168. Chinese. Chinese. [Google Scholar]
- 31.Jensen PS. Introduction--ADHD comorbidity and treatment outcomes in the MTA. J Am Acad Child Adolesc Psychiatry. 2001;40(2):134–136. doi: 10.1097/00004583-200102000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Brown TE. Attention Deficit Disorders and Comorbidities in Children, Adolescents, and Adults. Washington DC: American Psychiatric Press; 2000:203–215. [Google Scholar]
- 33.Biederman J, Faraone S, Mick E, Lelon E. Psychiatric comorbidity among referred juveniles with major depression: fact or artifact? Am Acad Child Adlolesc Psychiatry, . 1995;34(5):579–590. doi: 10.1097/00004583-199505000-00010. [DOI] [PubMed] [Google Scholar]
- 34.Schatz DB, Rostain AL. ADHD with comorbid anxiety: a review of the current literature. J Atten Disord. 2006;10(2):141–149. doi: 10.1177/1087054706286698. [DOI] [PubMed] [Google Scholar]
- 35.Lau JY, Eley TC, Stevenson J. Examining the state-trait anxiety relationship: a behavioural genetic approach. J Abnorm Child Psychol. 2006;34(1):19–27. doi: 10.1007/s10802-005-9006-7. [DOI] [PubMed] [Google Scholar]
- 36.Simon V, Czobor P, Bitter I. Is ADHD severity in adults associated with the lifetime prevalence of comorbid depressive episodes and anxiety disorders? Eur Psychiatry. 2013;28(5):308–314. doi: 10.1016/j.eurpsy.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 37.Chang LR, Chiu YN, Wu YY, Gau SS. Father’s parenting and father-child relationship among children and adolescents with attention-deficit/hyperactivity disorder. Compr Psychiatry. 2013;54(2):128–140. doi: 10.1016/j.comppsych.2012.07.008. [DOI] [PubMed] [Google Scholar]
- 38.Whaley SE, Pinto A, sigman M. Characterizing interactions between anxious mothers and their children. J Consult Clin Psychol. 1999;67(6):836–836. doi: 10.1037/0022-006X.67.6.826. [DOI] [PubMed] [Google Scholar]
- 39.Malcarne VL, Hamilton NA, Ingram RE, Taylor L. Correlates of distress in children at risk for affective disorder: exploring predictors in the offspring of depressed and non depressed mothers. J Affect Disord. 2000;59(3):243–251. doi: 10.1016/S0165-0327(99)00155-X. [DOI] [PubMed] [Google Scholar]
- 40.Marchand JF, Horck E. The relation of problem behaviors in preschool children to depressive symptoms in mothers and fathers. J Genet Psychol. 1998;159(3):353–366. doi: 10.1080/00221329809596157. [DOI] [PubMed] [Google Scholar]
- 41.Wilens TE, Spencer TJ. Understanding attention-deficit/hyperactivity disorder from childhood to adulthood. Postgrad Med. 2010;122(5):97–109. doi: 10.3810/pgm.2010.09.2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sorensen L, Plessen KJ, Lundervold AJ. The impact of attention deficits and emotional problems on cognitive control in primary school children. J Atten Disord. 2012;16(7):589–599. doi: 10.1177/1087054711417394. [DOI] [PubMed] [Google Scholar]


