Abstract
Alcohol intoxication is a potentially under-recognised precipitant of Brugada syndrome. Higher pre-cordial electrocardiogram lead placement increases sensitivity of detecting the Brugada pattern.
Keywords: Brugada Syndrome, Alcohol intoxication, Risk stratification, Syncope, Agonal breathing
Case report
A 56-year-old Caucasian male suffered a cardiac arrest while asleep. He had been teetotal for one month but had drank one bottle of wine the evening before his arrest. His wife described being woken by ‘noisy breathing’ which was similar to his usual snoring, however louder, irregular and more laboured. He was unresponsive, cardiopulmonary resuscitation was commenced and continued by the paramedics upon their arrival. Ventricular fibrillation was documented and eight rounds of direct current cardioversion were required before return of spontaneous circulation. His electrocardiogram showed infero-lateral ST-segment depression and he underwent an immediate coronary angiography. This showed minor atheroma only. Serial electrocardiograms later demonstrated an intermittent type 1 Brugada configuration (Figure 1). His electrolyte levels were normal throughout admission. A cardiac magnetic resonance imaging and echocardiogram were both normal, in keeping with a diagnosis of Brugada syndrome. He received an implantable cardioverter defibrillator.
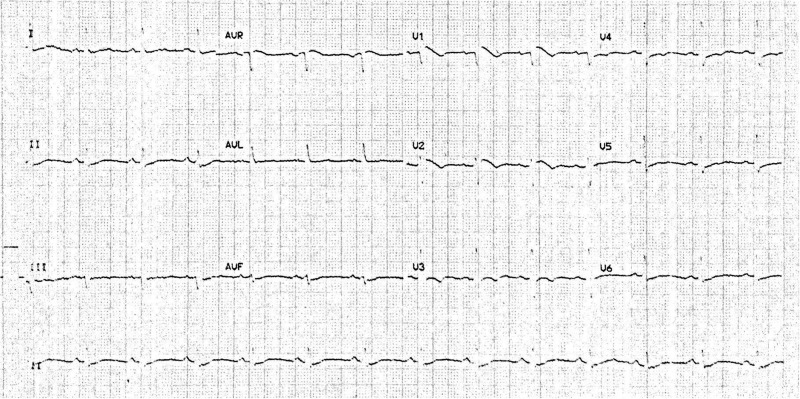
Figure 1.
Twelve lead ECG two days post cardiac arrest. ST segment elevation >2 mm in V1 and V2. T-wave inversion in V1–V3.
Five years previously he had attended a wellness clinic for a routine medical and at the time was found to have an abnormal electrocardiogram with ST-segment elevation in leads V1 and V2 (Figure 2). These electrocardiogram changes were felt not to satisfy the diagnostic criteria for a Brugada syndrome and given he was asymptomatic with no family history of sudden cardiac death, no further investigations were performed at that time.
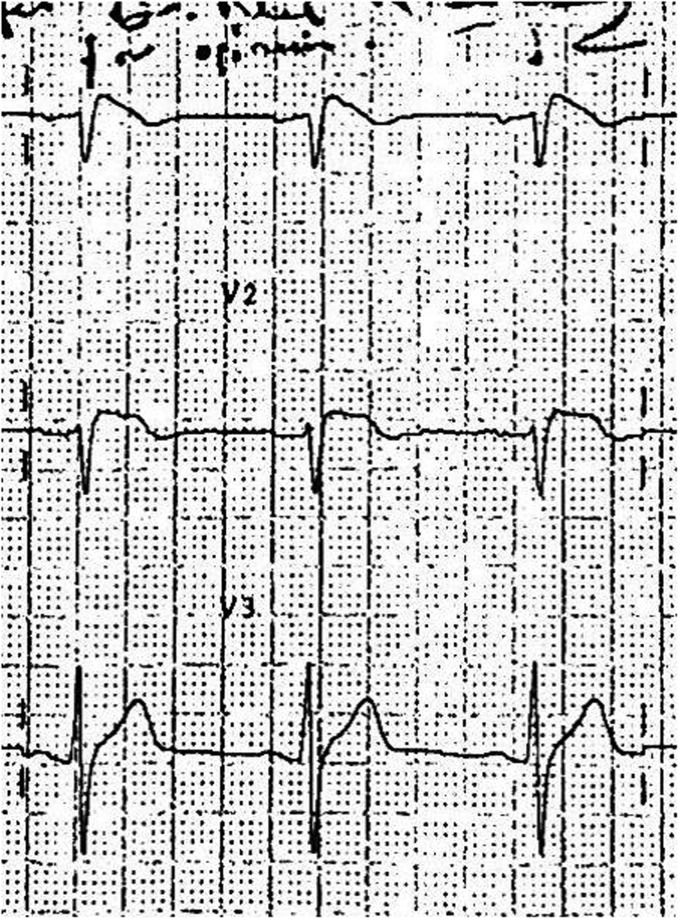
Figure 2.
ECG taken five years prior to acute presentation. Chest leads V1–V3.
Brugada syndrome
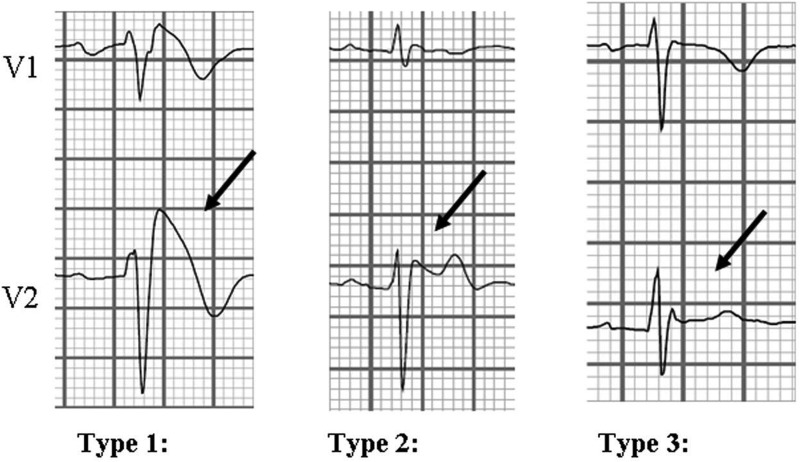
Brugada syndrome is most commonly caused by an inherited cardiac sodium-channel gene mutation. It manifests as an abnormal electrocardiogram pattern, of which three repolarisation patterns are recognised. Type 1: coved ST-segment elevation (≥2 mm) in ≥ 1 right precordial lead (V1–V3). Type 2: ST-elevation with a gradual decent followed by a biphasic T-wave resulting in a ‘saddleback’ configuration. Type 3: Right pre-cordial coved or saddleback ST-elevation <1 mm (Figure 3).1,2
Figure 3.
ECG abnormalities of suspected Brugada syndrome. Taken from Mizusawa and Wilde.3
The Brugada syndrome is currently diagnosed when a spontaneous Type 1 electrocardiogram appearance is seen in the clinical setting of ventricular fibrillation, polymorphic ventricular tachycardia, syncope, nocturnal agonal breathing or a family history of sudden cardiac death. Currently, Type 2 and 3 electrocardiogram patterns are not diagnostic of Brugada syndrome, merely suggestive.3 The electrocardiogram signature of this condition can be dynamic, can alternate between types and even disappear from the trace, further adding to the diagnostic challenge. In cases of uncertainty, pharmacological provocation with intravenous administration of class 1 sodium-channel blockers such as Ajmaline and Flecainide is recommended.2,4 Additionally, higher placement of precordial leads V1, V2 at the second intercostal space increases the sensitivity of detecting a Brugada phenotype if suspected on clinical grounds.5 The reasoning here being that the abnormal electrical activity leading to the Brugada electrocardiogram originates from the right ventricular outflow tract.1
The sodium channel dysfunction underlying the Brugada pattern is said to be variable, hence the dynamic electrocardiogram signature, and is influenced by the interaction of multiple factors.1 Most arrhythmic events tend to occur at rest or at night, suggesting an association with parasympathetic nervous system activity. Fever, autonomic factors, electrolyte imbalance and sodium-channel blocking drugs are widely acknowledged triggers for events; however, the association with alcohol intoxication is not as well-known despite a number of studies confirming its role.6 Alcohol intoxication is thought to have pro-arrhythmic effects by inhibiting sodium-channel gating, possibly mimicking the actions of sodium-channel blocking drugs.7
Risk stratification
The Brugada syndrome is associated with high risk of sudden cardiac death. Studies suggest that patients presenting with aborted sudden cardiac death have an estimated 8–13% annual risk of further events.8 It is widely accepted that affected individuals should undergo cardioverter defibrillator implantation to abate future arrhythmias and avoid sodium-channel blocking agents such as class 1 anti-arrhythmic medications and tricyclic anti-depressants. Heavy alcohol consumption and binge drinking should also be discouraged.2
Risk stratification and management of the asymptomatic Brugada electrocardiogram are somewhat more challenging and ill-defined.9 Electrophysiological studies are an option; however, its role in risk stratification is a topic of much debate.5 Recent studies estimate risk in asymptomatic patients to be much lower; 0.4–1% annual cardiac event rate and cardioverter defibrillator implantation are not recommended.8
One final caveat
Cardiac arrhythmias, such as Brugada syndrome, should always be considered in patients presenting with a first fit particularly if nocturnal. Anoxic seizures secondary to an arrhythmia can cause urinary incontinence, significant lactaemia and a slow recovery, as was witnessed in this case.10
Conclusions
We wonder if heavy alcohol consumption is easily overlooked and under-represented as a precipitant of the Brugada syndrome in at-risk individuals. To our knowledge, very few case reports exist regarding alcohol intoxication as a possible trigger of the Brugada syndrome; yet, alcohol is consumed worldwide by many including those unbeknown to have a Brugada electrocardiogram signature.
This case demonstrates the transient nature of Brugada Syndrome. The asymptomatic Brugada electrocardiogram is not necessarily benign. In the first instance, patients with suspicious electrocardiograms should undergo serial electrocardiograms with higher pre-cordial lead placement and in those with syncope or a relevant family history, provocation testing to expose the type 1 Brugada electrocardiogram is recommended. In syncopal or cardiac arrest patients with suspicion of Brugada, a history of binge alcohol consumption, drug history, atypical snoring and recent pyrexial illness may be relevant.
Awareness of the Brugada electrocardiogram appearances in asymptomatic patients is likely greater than it was five years ago following a recent update of the diagnostic criteria. The optimal way to assess the asymptomatic Brugada patient remains, however, subject to ongoing debate, particularly given the difficulties of risk stratifying asymptomatic patients. Given our patients’ electrocardiogram five years previously that was at least highly suspicious of Brugada, this case highlights the potential benefits of thorough assessment and counselling even in asymptomatic cases without a family history. Whether such cases should undergo provocative testing remains controversial as this identifies a sub-group of Brugada patients with the lowest risk.
Acknowledgements
None.
Declarations
Competing interests
None declared.
Funding
None declared.
Ethical approval
Written informed consent for publication was obtained from the patient.
Guarantor
AA
Contributorship
AA researched and wrote the article. NA oversaw this and frequently contributed to the article, and edited the final draft.
Provenance
Not commissioned; peer-reviewed by Stephen Leslie.
References
- 1.Bayés de Luna A, Brugada J, Baranchuk A, Borggrefe M, Breithardt G, Goldwasser D, et al. Current electrocardiographic criteria for diagnosis of Brugada pattern: a consensus report. J Electrocardiol 2012; 45: 433–442. [DOI] [PubMed] [Google Scholar]
- 2.Priori SG, Wilde AA, Horie M, Cho Y, Behr ER, Berul C, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm 2013; 10: 1932–1963. [DOI] [PubMed] [Google Scholar]
- 3.Mizusawa Y, Wilde AA. Brugada syndrome. Circ Arrhythm Electrophysiol 2012; 5: 606–616. [DOI] [PubMed] [Google Scholar]
- 4.Modi S, Krahn AD. Sudden cardiac arrest without overt heart disease. Circulation 2011; 123: 2994–3008. [DOI] [PubMed] [Google Scholar]
- 5.Antzelevitch C, Nof E. Brugada syndrome: recent advances and controversies. Curr Cardiol Rep 2008; 10: 376–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matsuo K, Kurita T, Inagaki M, Kakishita M, Aihara N, Shimizu W, et al. The circadian pattern of the development of ventricular fibrillation in patients with Brugada syndrome. Eur Heart J 1999; 20: 465–470. [DOI] [PubMed] [Google Scholar]
- 7.Klein G, Gardiwal A, Schaefer A, Panning B, Breitmeier D. Effect of ethanol on cardiac single sodium channel gating. Forensic Sci Int 2007; 171: 131–135. [DOI] [PubMed] [Google Scholar]
- 8.Postema PG. About Brugada syndrome and its prevalence. Europace 2012; 14: 925–928. [DOI] [PubMed] [Google Scholar]
- 9.Veltmann C, Schimpf R, Echternach C, Eckardt L, Kuschyk J, Streitner F, et al. A prospective study on spontaneous fluctuations between diagnostic and non-diagnostic ECGs in Brugada syndrome: implications for correct phenotyping and risk stratification. Eur Heart J 2006; 27: 2544–2552. [DOI] [PubMed] [Google Scholar]
- 10.Angus-Leppan H. First seizures in adults. BMJ 2014; 348: g2470–g2470. [DOI] [PubMed] [Google Scholar]