Abstract
Background
Hepatitis B virus (HBV) transmission through blood transfusion is reduced by screening for hepatitis B surface antigen (HBsAg). However this method cannot detect the presence of occult hepatitis B virus infection. This study sought to determine the prevalence of occult hepatitis B virus infection among blood donors in Ile-Ife, Nigeria. For the first time in Nigeria we employed an automated real-time PCR- method to investigate the prevalence of occult HBV in blood donors.
Methods
Blood donors screened with HBsAg immunochromatographic rapid test kits at the blood transfusion units of two hospitals and found to be negative were recruited into the study. Questionnaires to elicit risk factors for HBV infection were administered and then 10 ml of blood was collected from each donor. Plasma samples obtained from these HBsAg negative blood donors were screened again for HBsAg using an enzyme-linked immunosorbent assay (ELISA) method, and those found negative were screened for the presence of total antibody to the HBV core antigen (anti-HBc) using ELISA method. Those positive to anti-HBc were then tested for HBV DNA, using an automated real-time PCR method.
Results
Five hundred and seven blood donors found HBsAg negative by immunochromatographic rapid test kits at both blood transfusion units, were tested for HBsAg using ELISA and 5 (1 %) were HBsAg positive. The 502 found negative were tested for anti-HBc and 354 (70.5 %) were found positive implying previous exposure to HBV and 19 (5.4 %) of the 354 anti-HBc positive had HBV DNA signifying occult HBV infection. No risk factors were found to be associated with the presence of HBV DNA among those who tested positive.
Conclusion
Occult HBV infection exists in blood donors in Ile-Ife, Nigeria and the use of HBsAg alone for screening prospective donors will not eliminate the risk of HBV transmission in blood transfusion or stem cell transplantation.
Keywords: Occult hepatitis B Virus, Blood donors, HBV DNA, HBsAg, Anti-HBc
Background
Hepatitis B virus (HBV) infection is a global, public health issue [1–3] of immense importance. It occurs worldwide and up to two billion people, approximately 30 % of the world’s population, have been infected globally [2]. Of this, 300–400 million people are chronically infected, approximating to about 5 % of the world’s population at risk of developing the complications of chronic HBV infection [1–5]. Deaths resulting from HBV yearly, stand at about 500,000 to 1.2 million worldwide. Most of these are due to sequelae of chronic HBV infection such as cirrhosis, liver failure and hepatocellular carcinoma (HCC) [2–5].
Blood transfusion could be an important route for the transmission of infection especially when donated blood is not screened for HBV infection [6]. Screening of donated blood for Hepatitis B surface Antigen (HBsAg) was introduced in the 1970s [7–10]. This greatly reduced HBV transmission due to blood transfusions [9, 11] as blood found to be HBsAg positive was not transfused.
In many developing countries including Nigeria, screening of blood donors or blood donated, for HBsAg alone, is still the only practice on which the prevention of HBV transmission during blood transfusion is based [12].
Numerous scientific papers have highlighted the presence of HBV infection in some individuals negative for HBsAg but having detectable HBV DNA in the liver or blood and some of these publications have documented HBV transmission resulting from transfusion of blood tested and found to be HBsAg negative [9, 13–15].
Occult HBV infection (OBI) has been the subject of numerous publications focusing on different aspects of and issues relating to OBI [10, 16–51]. It is a term that has been chosen by experts [33] to denote HBV infections in which HBsAg cannot be detected and the presence of infection is only established by amplifying and detecting HBV DNA [18–22, 28, 33, 34, 46].
One significant importance of OBI is the risk of transmission of HBV from individuals with OBI to recipients. This could occur if blood or blood components, stem cells or solid organs are transfused or transplanted following negative HBsAg results in donors with OBI.
Such infections could manifest overtly becoming HBsAg positive with possibly fatal consequences, the risk rising with immune suppressed recipients [14–16, 18, 25, 33, 46, 52, 53].
In Nigeria, which is highly endemic for HBV infection [54–57], current blood banking practices do not include procedures that would identify OBI and prevent transfusion of blood or blood products from apparently healthy donors with OBI to recipients [58].
As the prevalence of OBI tends to be higher where the prevalence of overt HBV infection is high [27] there may be a relatively high prevalence of OBI in Nigeria. All of these translating to an increasing number of patients who may be at risk of HBV infection from occult donors. Nevertheless there is limited data on the prevalence of OBI in blood donors in this country as only HBsAg screening is still relied upon [12, 58].
Against this background, we sought to investigate the prevalence of occult HBV in this region, to enable us make evidence-based recommendations for effective HBV screening to prevent HBV transmission from donors with OBI to recipients during blood transfusion.
Methods
Ethical issues
Approval was sought and obtained from the Ethics and Research Committee of Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC) Ile-Ife with reference number IRB/IEC/0004553 and the Ethics and Research Committee of Seventh Day Adventist Hospital (SDAH), Ile-Ife. Prospective subjects were informed about the study and written consent was obtained from those who agreed to participate. The study was a prospective, cross-sectional study.
Selection of study population
Apparently healthy blood donors who had been screened and found eligible by the respective blood banks for donation were recruited over a period of six and a half months, from June 2013 to January 2014. Subjects who had hepatitis B vaccination in the previous one month were excluded.
Sociodemographic information
With the aid of a structured questionnaire, relevant sociodemographic information was obtained from blood donors. This included age, sex, number of lifetime sexual partners, presence of tatoos/scarification marks, history of alcohol use, smoking, sharing of sharps and hepatitis B vaccination. The questionnaires were self-administered by subjects or any subjects who needed help in filling the questionnaires were assisted by trained volunteers who were medical doctors, medical laboratory scientists, medical laboratory science students, and laboratory technologists.
Collection of specimens
Ten milliliters (mls) of venous blood was collected from each consecutive consenting, eligible, previously screened, apparently healthy blood donor, donating to the blood banks at OAUTHC and SDAH in Ile-Ife. The blood was collected aseptically into a specimen bottle containing potassium ethylene diamine tetra acetate (K+EDTA) anticoagulant. All samples were centrifuged at room temperature at 3500 rpm for 10 min within 24 h of collection. The plasma was then separated and stored at −70 °C until analysed.
Serological analysis
The serological studies were done at the department of Medical Microbiology and Parasitology, OAUTHC. HBsAg was tested for in all specimens using commercially available Monolisa™ HBsAg ULTRA ELISA kits manufactured by BIORAD (3,bd Raymond Poincare, 92430 Marnes-la-Coquette-France) with a lower limit of detection estimated to be less than 0.13 IU/ml, according to the manufacturer’s instructions.
All HBsAg negative plasma samples were then tested for total anti-HBc using commercially available Monolisa™ Anti-HBc PLUS ELISA kits by BIORAD (3,bd Raymond Poincare, 92430 Marnes-la-Coquette-France) according to the manufacturer’s instructions.
HBV DNA studies
Detection and quantification of HBV DNA was done at the Human Virology Laboratory of the Nigerian Institute of Medical Research (NIMR) Lagos and all HBsAg negative, anti-HBc positive plasma samples were tested for HBV DNA using “COBAS AmpliPrep/COBAS TaqMan HBV Test version 2.0” kits made by Roche (Roche Molecular Systems Inc. Branchburg, NJ 08876 USA) using the “Cobas Ampliprep instrument and COBAS TaqMan 48 Analyzer” with a limit of detection of less than 20 IU/ml for HBV DNA. All procedures were performed according to manufacturer’s instructions.
Initial daily maintenance and priming were performed and specimens and controls were brought to room temperature. Reagent cassettes and disposables were then loaded onto the COBAS AmpliPrep Instrument as per manufacturer’s instructions. Sample racks were prepared, then 650 μl of High Positive control (HPC), Low Positive Control (LPC), Negative control (NC) and each specimen was transferred using a micropipette and DNase-free tips into the appropriate sample input tubes (S-tubes) The sample racks with S-tubes and K-tubes were then loaded onto the appropriate rack position on the COBAS AmpliPrep Instrument.
The COBAS AmpliPrep Instrument was then started using the AMPLILINK software and automated specimen processing was done. Each set of processed specimens in K-tubes, on K- carriers were then manually transferred to the COBAS TaqMan 48 Analyzer using the K- carrier transporter and the COBAS TaqMan 48 Analyzer run was then started for automated real-time PCR amplification and detection and quantification. At the end of each run the results were printed out. Positive (HPC and LPC) and negative controls were included in each run.
Data analysis and statistical techniques
Descriptive statistics were calculated and reported for sociodemographic characteristics. Percentages were used to describe frequency analyses of categorical variables. Chi-squared test was used to compare categorical variables. A P value < 0.05 was considered to indicate statistical significance. Data processing and statistical analyses were performed using Epi Info 7 Software by CDC.
Results
Hepatitis B surface antigen testing in donors
Five hundred and seven blood donors tested at both OAUTHC and SDAH blood banks for HBsAg using immunochromatographic rapid test kits and found negative were tested for HBsAg using ELISA and five of them were found to be HBsAg positive as presented in Table 1.
Table 1.
HBsAg Screening by ELISA
| Blood Bank | OAUTHC | SDAH | Total |
|---|---|---|---|
| Number Screened | 405a | 102a | 507 |
| Number Positive | 4 | 1 | 5 |
aPreviously screened and found HBsAg negative by the immunochromatographic rapid test kits
HBsAg Hepatitis B surface antigen, OAUTHC Obafemi Awolowo University Teaching Hospitals Complex, SDAH Seventh Day Adventist Hospital
Assessment of HBsAg negative donors for anti-HBc
The 502 donors found to be HBsAg negative using ELISA tests were tested for anti-HBc also using ELISA. Three hundred and fifty four (71 %) were positive giving an anti-HBc prevalence of 71 % among blood donors.
Real time PCR assays for HBV DNA
Out of the 354 HBsAg negative, anti-HBc positive subjects whose specimens were tested, HBV DNA was detected in 19 (5.4 %) as shown in Table 2. The viral load for those with OBI ranged from 68 to < 20 IU/ml.
Table 2.
Quantitative HBV DNA results for HBsAg negative, anti-HBc positive subjects with occult HBV
| Viral Load | Number of Subjects | HBsAg | Anti-HBc |
|---|---|---|---|
| <20 IU/ml | 16 | Negative | Positive |
| 21 IU/ml | 1 | Negative | Positive |
| 64 IU/ml | 1 | Negative | Positive |
| 68 IU/ml | 1 | Negative | Positive |
HBsAg Hepatitis B surface antigen, Anti-HBc antibody to hepatitis B core antigen, IU/ml international units per milliliter
Summary of laboratory tests and results
See Fig. 1 below.
Fig. 1.
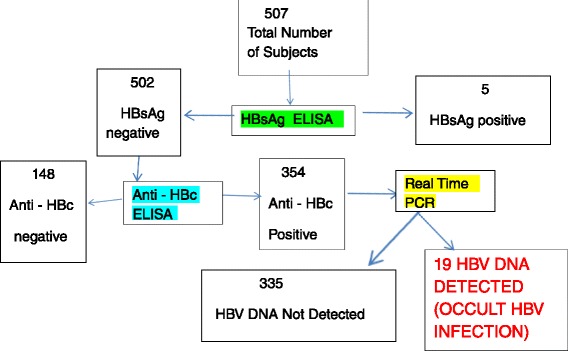
Summary of Results. Figure one summarizes the laboratory tests done and the results seen in form of a flow chart. There were 507 subjects and their plasma specimens were screened for HBsAg using ELISA and five were positive. The remaining 502 were then screened for anti-HBc also using ELISA and 354 were found to be positive. The 354 anti-HBc samples were then screened for HBV DNA using real time PCR. HBV DNA was found in 19. (HBV – Hepatitis B virus, HBsAg –Hepatitis B surface Antigen Anti-HBc – antibody to hepatitis B core antigen, ELISA – Enzyme linked immunosorbent assay, PCR – Polymerase chain reaction)
Sociodemographic characteristics of subjects with occult HBV
Nineteen subjects were found to have occult HBV infection. All (100 %) of them were males and 17 (89.5 %) of them were less than 35 years (Table 3). There was no significant association between occult HBV infection and any of the variables tested as seen in Table 3.
Table 3.
Sociodemographic characteristics of anti-HBc positive subjects with/without occult HBV infection
| Variables | HBV DNA | Tests of Statistical Significance | |||
|---|---|---|---|---|---|
| positive(%) | negative(%) | Χ2 | df | p | |
| Age (years) | 0.68 | 1 | 0.41 | ||
| ≤35 >35 |
17(89.5) 2(10.5) |
270(82.1) 59(17.9) |
|||
| Sex | 0.58 | 1 | 1.00 | ||
| Male Female |
19(100.0) 0(0.0) |
325(97.0) 10(3.0) |
|||
| Alcohol | 1.32 | 1 | 0.33 | ||
| Yes No |
10(52.6) 9(47.4) |
131(39.3) 202(60.7) |
|||
| Smoking | 1.98 | 1 | 0.25 | ||
| Yes No |
4(21.0) 15(79.0) |
35(10.6) 295(89.4) |
|||
| Share Sharps | 0.18 | 1 | 1.00 | ||
| Yes No |
2(14.3) 12(85.7) |
50(18.9) 215(81.1) |
|||
| Scarification marks/Tattoos | 0.17 | 1 | 0.78 | ||
| Yes No |
4(28.6) 10(71.4) |
90(33.8) 176(66.2) |
|||
| Number of Lifetime Sexual Partners | 0.21 | 1 | 0.78 | ||
| ≤1 >1 |
7(50.0) 7(50.0) |
116(43.8) 149(56.2) |
|||
P.S For the last three characteristics/variables no responses were available for five of those with occult HBV infection
HBV Hepatitis B virus
Anti-HBc antibody to hepatitis B core antigen, X 2 chi square, df degree of freedom, p p-value
Discussion
In this study we found in HBsAg negative blood donors an anti-HBc prevalence of 70.5 %. This means over 70 % of our adult population have been infected with HBV at some point in their lives. This has previously been reported by others [59] including Kiire who in 1996 [60] reported that 72.5 % of Nigerians show evidence of exposure to HBV infection. This means that the burden of HBV infection has not changed significantly over the last 18 years especially in adults. This is not surprising as they were born before 2004 when hepatitis B vaccine actually became widely available as part of the universal immunization schedule for infants in Nigeria [61]. Other workers such as Japhet et al. [62] found a prevalence of 5.4 % for IgM anti-HBc only positive blood donors but did not look for total anti-HBc. Salawu et al. [63] also found about 4.4 % of anti-HBc in HBsAg negative donors but in that study rapid test kits were used which may be less sensitive than the ELISA used in this study.
This study found an OBI prevalence of 5.4 % among anti-HBc positive blood donors in Ile-Ife. This means that after HBsAg screening about 1 in 20 to 1 in 25 blood donations still have HBV DNA. Therefore the risk of transfusing blood from donors with OBI is about 1 in 20 donations. Published data on OBI in blood donors in Nigeria is sparse. Nna et al. [64] found a prevalence of 8 % in Abakaliki, South-Eastern Nigeria among 100 donors, Opaleye et al. [65] found a very high prevalence of 36 % among 429 donors while Oluyinka et al. [66] found a prevalence of 17 % in Southwestern Nigeria among 429 donors. These prevalence values are all higher than that found in this study. In all three, the method of HBV DNA detection was nested PCR. Nested PCR has the significant drawback of being prone to contamination and false positives especially during the sample transfer step preceding the second round of amplification [67–69] and so that may explain the much higher values. The problem of contamination and false positives in nucleic acid amplification assays is eliminated in automated real time PCR assays [70] such as the one we used in this study. However there may be differences in the prevalence of OBI among blood donors from one part of the country to another, reflecting differences in the prevalence of overt HBV infection which exist from one part of the country to the other [54–57].
Other studies on OBI in Nigeria have been in other subject populations such as Ola et al. [71] who found OBI in 2 of 28 chronic hepatitis patients in Ibadan, Opaleye et al. [72] also in Nigeria found a prevalence of 11.2 % of OBI in HIV positive patients using archived specimens from Ikole Ekiti, however this subjects were not likely to qualify as blood donors and as such no risk of their blood being transfused.
The prevalence in this study was higher than the 1.7 % found in Ghana by Zahn et al. [73] but this may be because the HBV DNA was tested for in all blood donors and not just those that were anti- HBc positive as was done in this study. HBsAg positive individuals who are anti-HBc positive have been found to be more likely to have OBI than those without anti-HBc.
In Brazil, Silva et al. found 3.3 % but used a PCR assay with a LLOD of about 200 IU/ml [23], which is less sensitive than the real-time PCR assay used in this study. This could have resulted in a lower detection of OBI.
The prevalence found in this study is much higher than what has been found in the US and some other western countries where only 0.1–2.4 % of HBsAg negative, anti-HBc positive blood donors were found to have HBV DNA [46, 74]. This is not surprising because only about 5 % of the population have come in contact with HBV in those regions unlike in Nigeria where over 70 % of the population have at some time in their lives been exposed to or infected with HBV [59, 60].
Manzini et al. in Italy [29] found 4.86 % among HBsAg negative, anti-HBc positive blood donors which is similar to what we found.
This prevalence is much smaller than the 38 % that was reported by Yotsuyanagi et al. in Japan [13] but the sample size was just 50 blood donors which is small compared to this study. This may also be the reason why Jafarzahdeh et al. found a 28.56 % prevalence in Iran [31] as they only assayed 14 HBsAg negative, anti-HBc positive samples for HBV DNA and found in four samples.
This study did not find any significant association between occult HBV and the variables tested such as age, sex, alcohol use, smoking, sharing of sharps scarification marks/tattoos and number of lifetime sexual partners. This is most likely because of the small number (19) of individuals in which we detected HBV DNA. This number was probably too small for reliable statistical analysis. However all those with OBI in this study were found to be males, mostly less than 36 years.
Of note is that in this study HBsAg was detected by ELISA in five (1 %) blood donors who had previously been screened with rapid test kits, declared HBsAg negative and cleared for donation. In at least two of these blood donors HBV DNA was demonstrated by real-time PCR. This shows that the rapid test kits being used for HBsAg screening in the blood banks where the subjects were recruited are not adequate for screening in blood transfusion services and would allow transfusion of HBsAg positive blood in 1 out of every 100 blood donations.
The inadequacy in sensitivity and variation in performance between different locations of some rapid test kits used in resource poor settings for HBsAg screening has been shown by Bjoerkvoll et al. [75]. In their cross-sectional epidemiological study they compared the accuracy of rapid test immunochromatographic kits in the detection of HBsAg, anti-HBc and anti-HCV against ELISA, in two populations of 1200 potential blood donors in rural Cambodia and Vietnam. For HBsAg specifically, they found the rapid test kits to be high in specificity (99.8–99.9 %) but lower in sensitivity (86.5 %). They also found a difference in its sensitivity between both countries. In Cambodia the sensitivity was 93.5 % and in Vietnam 81.8 %.
Anti-HBs prevalence has been studied in Nigeria. Salawu et. al [63] in a study in Ile-Ife among 457 blood donors negative for hepatitis B surface antigen(HBsAg) found a prevalence rate of 12.7 %, Japhet et. al [62] found a rate of 15.2 % among 92 donors also studied in Ile-Ife while Oluyinka et. al [66] found 35 % of those with OBI had anti-HBs. However we did not investigate the prevalence of anti-HBs among blood donors with or without OBI in our study because we did not have enough funds to do that.
Conclusion
Hepatitis B virus infection is still endemic in Nigeria with a large percentage of the population showing evidence of prior exposure to HBV in this environment evidently from routes other than blood transfusion. There is a relatively high burden of occult HBV infection in our environment and the use of HBsAg alone for screening either in blood transfusion or transplantation services does not eliminate the risk of HBV transmission.
Recommendations
We recommend that assays including rapid test kits used for HBsAg screening should be validated before routine use locally comparing their performance with at least 3rd generation ELISA. Only ELISA assays or rapid test kits with comparable performance with regard to sensitivity or specificity should be used for HBsAg screening in blood transfusion.
Nucleic acid tests (NATs) should be introduced for routine screening of donors in blood transfusion and mandatorily for screening of donors and recipients in transplantation services. Individual donor (sample) testing using a NAT is more sensitive than testing in pools and so is preferred for this purpose [76–79].
Limitations
Other HBsAg negative and anti-HBc negative specimens could not be tested by real time PCR because of the high costs involved. We also were not able to test for anti-HBs in the specimens of subjects with OBI because our funds were limited.
Acknowledgements
This work was made possible by a generous donation of kits from Roche Products Nigeria Limited. We are grateful for the donation. We are grateful to Professor G. E. Erhabor for his generous financial donation to this work. We are grateful to the management of OAUTHC for the generous financial donation from the institution. We are grateful to the Director General of NIMR for allowing us access to the facility and equipment at a greatly reduced cost. We are indebted to our medical and dental colleagues, students, staff of OAUTHC and the staff of SDAH who all assisted us during the course of this study with logistic support.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Study concept and design: OAA, OAO, SL, AAO. Acquisition of data: OAA, ARA, OAP. Analysis and interpretation of data: OAA, OAO, SL, ARA, OAP, AAO. Statistical Analysis: OAA. Drafting of the manuscript: OAA, OAO, SL, ARA, OAP,AAO. All authors read and approved the final version.
References
- 1.Lok AS, McMahon BJ. Chronic hepatitis B. Hepatology. 2001;34(6):1225–41. doi: 10.1053/jhep.2001.29401. [DOI] [PubMed] [Google Scholar]
- 2.Kao JH, Chen DS. Global control of hepatitis B virus infection. Lancet Infect Dis. 2002;2:395–403. doi: 10.1016/S1473-3099(02)00315-8. [DOI] [PubMed] [Google Scholar]
- 3.Sorrell MF, Belongia EA, Costa J, Gareen IF, Grem JL, Inadomi JM, et al. National Institutes of Health Consensus Development Conference Statement: Management of hepatitis B. Ann Intern Med. 2009;150:104–10. doi: 10.7326/0003-4819-150-2-200901200-00100. [DOI] [PubMed] [Google Scholar]
- 4.Maddrey WC. Hepatitis B: An Important Public Health Issue. J Med Virol. 2000;61:362–6. doi: 10.1002/1096-9071(200007)61:3<362::AID-JMV14>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 5.Lavanchy D. Hepatitis B, virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat. 2004;11:97–107. doi: 10.1046/j.1365-2893.2003.00487.x. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organisation . Department of Vaccines and Biologicals. Introduction of hepatitis B vaccine into childhood Immunization services. Geneva: World Health Organisation; 2001. [Google Scholar]
- 7.Allain JP. Occult hepatitis B virus infection and transfusion. (Letters to the Editor) J Hepatol. 2006;44:616–9. doi: 10.1016/j.jhep.2005.11.041. [DOI] [PubMed] [Google Scholar]
- 8.Fang CT. Blood screening for HBV DNA. J Clin Virol. 2006;Suppl 1:S30–2. doi: 10.1016/S1386-6532(06)80006-5. [DOI] [PubMed] [Google Scholar]
- 9.Hennig H, Puchta I, Luhm J, Schlenke P, Goerg S, Kirchner H. Frequency and load of hepatitis B virus DNA in first-time blood donors with antibodies to hepatitis B core antigen. Blood. 2002;100:2637–41. doi: 10.1182/blood-2002-03-0798. [DOI] [PubMed] [Google Scholar]
- 10.Said ZNA. An overview of occult hepatitis B virus infection. World J Gastroenterol. 2011;17(15):1927–38. doi: 10.3748/wjg.v17.i15.1927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Contreras M, Taylor CPF, Barbara JA. Clinical blood transfusion. In: Hoffbrand AV, Catovsky D, Tuddenham EGD, editors. Postgraduate Heamatology. 5. Oxford: Blackwell Publishing Ltd; 2005. pp. 249–76. [Google Scholar]
- 12.Salawu L, Murainah HA. Pre-donation screening of intending blood donors for antibodies to infectious agents in a Nigerian tertiary health institution: a pilot study. Afr J Med Med Sci. 2006;35(4):453–6. [PubMed] [Google Scholar]
- 13.Yotsuyanagi H, Yasuda K, Moriya K, Shintani Y, Fujie H, Tsutsumi T, et al. Frequent presence of HBV in the sera of HBsAg-negative, anti-HBc-positive blood donors. Transfusion. 2001;41:1093–9. doi: 10.1046/j.1537-2995.2001.41091093.x. [DOI] [PubMed] [Google Scholar]
- 14.Gerlich WH, Wagner FF, Chudy M, Harrishoj LH, Lattermenn A, Wienzek S, et al. HBsAg non-reactive HBV infection in blood donors: transmission and pathogenicity. J Med Virol. 2007;79:S32–6. doi: 10.1002/jmv.20963. [DOI] [Google Scholar]
- 15.Satake M, Taira R, Yugi H, Hino S, Kanemitsu K, Ikeda H, et al. Infectivity of blood components with low hepatitis B virus DNA levels identified in a look back program. Transfusion. 2007;47:1197–205. doi: 10.1111/j.1537-2995.2007.01276.x. [DOI] [PubMed] [Google Scholar]
- 16.Conjeevaram HS, Lok AS. Occult hepatitis B virus infection: a hidden menace? Hepatology. 2001;34(1):204–6. doi: 10.1053/jhep.2001.25225. [DOI] [PubMed] [Google Scholar]
- 17.Brechot C, Thiers V, Kremsdorf D, Nalpas B, Pol S, Paterlini-Brechot P. Persistent hepatitis B virus: clinically significant or purely occult? Hepatology. 2001;34:194–203. doi: 10.1053/jhep.2001.25172. [DOI] [PubMed] [Google Scholar]
- 18.Hu KQ. Occult hepatitis B virus infection and its clinical implications. J Viral Hepat. 2002;9:243–57. doi: 10.1046/j.1365-2893.2002.00344.x. [DOI] [PubMed] [Google Scholar]
- 19.Torbenson M, Thomas DL. Occult hepatitis B. Lancet Infect Dis. 2002;2:479–86. doi: 10.1016/S1473-3099(02)00345-6. [DOI] [PubMed] [Google Scholar]
- 20.Allain JP. Occult hepatitis B virus infection. Transfus Clin Biol. 2004;11:18–25. doi: 10.1016/j.tracli.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 21.Allain JP. Occult hepatitis B virus infection: implications in transfusion. Vox Sang. 2004;86:83–91. doi: 10.1111/j.0042-9007.2004.00406.x. [DOI] [PubMed] [Google Scholar]
- 22.Allain JP. Occult hepatitis B virus infection. Hep B Annual. 2005;2(1):14-30. Available from: http://www.hepatitisbannual.org/downloadpdf.asp?issn=0972-9747;year=2005;volume=2;issue=1;spage=14;epage=30;aulast=Allain;type=2. Accessed 4 Mar 2016.
- 23.Silva CMD, Costi C, Costa C, Michelon C, Oravec R, Ramos AB, et al. Low rate of occult hepatitis B virus infection among anti-HBc positive blood donors living in a low prevalence region in Brazil. J Infect. 2005;51:24–9. doi: 10.1016/j.jinf.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 24.Minuk GY, Sun DF, Uhanova J, Zhang M, Caouette S, Nicolle LE, et al. Occult hepatitis B virus infection in a North American community-based population. J Hepatol. 2005;42:480–5. doi: 10.1016/j.jhep.2004.11.037. [DOI] [PubMed] [Google Scholar]
- 25.Hui CK, Sun J, Au WY, Lie AK, Yueng YH, Zhang HY, et al. Occult hepatitis B virus infection in hematopoietic stem cell donors in a hepatitis B virus endemic area. J Hepatol. 2005;42:813–9. doi: 10.1016/j.jhep.2005.01.018. [DOI] [PubMed] [Google Scholar]
- 26.Liu CJ, Lo SC, Kao JH, Tseng PT, Lai MY, Ni YH, et al. Transmission of occult hepatitis B virus by transfusion to adult and pediatric recipients in Taiwan. J Hepatol. 2006;44:39–46. doi: 10.1016/j.jhep.2005.06.016. [DOI] [PubMed] [Google Scholar]
- 27.Liu CJ, Chen DS, Chen PJ. Epidemiology of HBV infection in Asian blood donors: emphasis on occult HBV infection and the role of NAT. J Clin Virol. 2006;36(Suppl 1):S33–44. doi: 10.1016/S1386-6532(06)80007-7. [DOI] [PubMed] [Google Scholar]
- 28.Mulrooney-Cousins PM, Michalak TI. Persistent occult hepatitis B virus infection: Experimental findings and clinical implications. World J Gastroenterol. 2007;13(43):5682–6. doi: 10.3748/wjg.v13.i43.5682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Manzini P, Girotto M, Borsotti R, Giachino O, Guaschino R, Lanteri M, et al. Italian blood donors with anti-HBc and occult hepatitis B virus infection. Haematologica. 2007;92:1664–70. doi: 10.3324/haematol.11224. [DOI] [PubMed] [Google Scholar]
- 30.Yoshikawa A, Gotanda Y, Minegishi K, Taira R, Hino S, Tadokoro K, et al. Lengths of hepatitis B viremia and antigenemia in blood donors: preliminary evidence of occult (hepatitis B surface antigen-negative) infection in the acute stage. Transfusion. 2007;47:1162–71. doi: 10.1111/j.1537-2995.2007.01234.x. [DOI] [PubMed] [Google Scholar]
- 31.Jafarzadeh A, Arababadi MK, Mirzaee M, Pourazar A. Occult hepatitis B virus infection among blood donors with antibodies to hepatitis B core antigen. Acta Med Iran. 2007;45(5):27–32. [Google Scholar]
- 32.Yuen MF, Wong DKH, Lee CK, Tanaka Y, Allain JP, Fung J, et al. Transmissibility of hepatitis B virus (HBV) infection through blood transfusion from blood donors with occult HBV infection. Clin Infect Dis. 2011;52(5):624–32. doi: 10.1093/cid/ciq247. [DOI] [PubMed] [Google Scholar]
- 33.Raimondo G, Pollicino T, Cacciola I, Squadrito G. Occult hepatitis B virus infection. J Hepatol. 2007;46:160–70. doi: 10.1016/j.jhep.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 34.Raimondo G, Allain JP, Brunetto MR, Buendia MA, Chen DS, Colombo M, et al. Statements from the Taormina expert meeting on occult hepatitis B virus infection. J Hepatol. 2008;49:652–7. doi: 10.1016/j.jhep.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 35.Candotti D, Grabarczyk P, Ghiazza P, Roig R, Casamitjana N, Iudicone P, et al. Characterization of occult hepatitis B virus from blood donors carrying genotype A2 or genotype D strains. J Hepatol. 2008;49:537–47. doi: 10.1016/j.jhep.2008.04.017. [DOI] [PubMed] [Google Scholar]
- 36.Reesink HW, Engelfriet CP, Henn G, Mayr WR, Delage G, Bernier F, et al. Occult hepatitis B infection in blood donors. Vox Sang. 2008;94:153–66. doi: 10.1111/j.1423-0410.2008.01017.x. [DOI] [PubMed] [Google Scholar]
- 37.Hollinger FB. Hepatitis B, virus infection and transfusion medicine: science and the occult. Transfusion. 2008;48:1001–12. doi: 10.1111/j.1537-2995.2008.01701.x. [DOI] [PubMed] [Google Scholar]
- 38.Raimondo G, Navarra G, Mondello S, Costantino L, Colloredo G, Cucinotta E, et al. Occult hepatitis B virus in liver tissue of individuals without hepatic disease. J Hepatol. 2008;48:743–6. doi: 10.1016/j.jhep.2008.01.023. [DOI] [PubMed] [Google Scholar]
- 39.van Hemert FJ, Zaaijer HL, Berkhout B, Lukashov VV. Occult hepatitis B infection: an evolutionary scenario. Virol J. 2008;5:146. doi: 10.1186/1743-422X-5-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bremer CM, Saniewski M, Wend UC, Torres P, Lelie N, Gerlich WH, Glebe D. Transient occult hepatitis B virus infection in a blood donor with high viremia. Transfusion. 2009;49:1621–9. doi: 10.1111/j.1537-2995.2009.02188.x. [DOI] [PubMed] [Google Scholar]
- 41.Manzini P, Abate ML, Valpreda C, Milanesi P, Curti F, Rizzetto M, Smedile A. Evidence of acute primary occult hepatitis B virus infection in an Italian repeat blood donor. Transfusion. 2009;49:757–64. doi: 10.1111/j.1537-2995.2008.02041.x. [DOI] [PubMed] [Google Scholar]
- 42.Yuen MF, Lee CK, Wong DK, Fung J, Hung I, Hsu A, et al. Prevalence of occult hepatitis B infection in a highly endemic area for chronic hepatitis B: a study of a large blood donor population. Gut. 2010;59:1389–93. doi: 10.1136/gut.2010.209148. [DOI] [PubMed] [Google Scholar]
- 43.Urbani S, Fagnoni F, Missale G, Franchini M. The role of anti-core antibody response in the detection of occult hepatitis B virus infection. Clin Chem Lab Med. 2010;48:23–9. doi: 10.1515/CCLM.2010.002. [DOI] [PubMed] [Google Scholar]
- 44.Liu Y, Li P, Li C, Zhou J, Wu C, Zhou YH. Detection of hepatitis B virus DNA among accepted blood donors in Nanjing, China. Virol J. 2010;7:193. doi: 10.1186/1743-422X-7-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Panigrahi R, Biswas A, Datta S, Banerjee A, Chandra PK, Mahapatra PK, et al. Anti-hepatitis B core antigen testing with detection and characterization of occult hepatitis B virus by an in-house nucleic acid testing among blood donors in Behrampur, Ganjam. Orissa in southeastern India: implications for transfusion. Virol J. 2010;7:204. doi: 10.1186/1743-422X-7-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hollinger FB, Sood G. Occult hepatitis B virus infection: a covert operation. J Viral Hepat. 2010;17:1–15. doi: 10.1111/j.1365-2893.2009.01245.x. [DOI] [PubMed] [Google Scholar]
- 47.Larrubia JR. Occult hepatitis B virus infection: A complex entity with relevant clinical implications. World J Gastroenterol. 2011;17(12):1529–30. [DOI] [PMC free article] [PubMed]
- 48.Aller de la Fuente R, Gutiérrez ML, Garcia-Samaniego J, Fernández-Rodriguez C, Lledó JL, Castellano G. Pathogenesis of occult chronic hepatitis B virus infection. World J Gastroenterol. 2011;17(12):1543–8. [DOI] [PMC free article] [PubMed]
- 49.Romero M, Madejón A, Fernández-Rodríguez C, García-Samaniego J. Clinical significance of occult hepatitis B virus infection. World J Gastroenterol. 2011;17(12):1549–52. doi: 10.3748/wjg.v17.i12.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ocana S, Casas ML, Buhigas I, Lledo JL. Diagnostic strategy for occult hepatitis B virus infection. World J Gastroenterol. 2011;17(12):1553–7. doi: 10.3748/wjg.v17.i12.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lledó JL, Fernández C, Gutiérrez ML, Ocaña S. Management of occult hepatitis B virus infection: An update for the clinician. World J Gastroenterol. 2011;17(12):1563–8. doi: 10.3748/wjg.v17.i12.1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang JT, Lee CZ, Chen PJ, Wang TH, Chen DS. Transfusion-transmitted HBV infection in an endemic area: the necessity of more sensitive screening for HBV carriers. Transfusion. 2002;42:1592–7. doi: 10.1046/j.1537-2995.2002.00274.x. [DOI] [PubMed] [Google Scholar]
- 53.Levicnik-Stezinar S, Rahne-Potokar U, Candotti D, Lelie N, Allain JP. Anti-HBs positive occult hepatitis B virus carrier blood infectious in two transfusion recipients. J Hepatol. 2008;48:1022–5. doi: 10.1016/j.jhep.2008.02.016. [DOI] [PubMed] [Google Scholar]
- 54.Jombo GT, Egah DZ, Banwat EB. Hepatitis B virus infection in a rural settlement of Northern Nigeria. Niger J Med. 2005;14(4):425–8. [PubMed] [Google Scholar]
- 55.Sirisena ND, Njoku MO, Idoko JA, Isamade E, Barau C, Jelpe D, Zamani A, Otowo S. Carriage rate of hepatitis-B surface antigen (HBsAg) in an urban community in Jos, Plateau State, Nigeria. Niger Postgrad Med J. 2002;9(1):7–10. [PubMed] [Google Scholar]
- 56.Adoga MP, Gyar SD, Pechulano S, Bashayi OD, Emiasegen SE, Zungwe T, et al. Hepatitis B virus infections in apparently healthy urban Nigerians: data from pre-vaccination tests. J Infect Dev Ctries. 2010;4(6):397–400. [PubMed] [Google Scholar]
- 57.Forbi JC, Vaughan G, Purdy MA, Campo DS, Xia G-l, et al. Epidemic history and evolutionary dynamics of hepatitis B virus infection in two remote communities in rural Nigeria. PLoS One. 2010;5(7) doi: 10.1371/journal.pone.0011615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Salawu L, Bolarinwa RA, Adegunloye AB, Muraina HA. HBsAg, anti-HCV, anti-HIV and VDRL in blood donors: prevalence and trends in the last three and a half years in a tertiary health care facility in Ile-Ife, Nigeria. Int J Med Med Sci. 2010;2(11):335–41. [Google Scholar]
- 59.Uneke CJ, Ogbu O, Inyama PU, Anyanwu GI, Njoku MO. Idoko JH Prevalence of hepatitis-B surface antigen among blood donors and human immunodeficiency virus-infected patients in Jos, Nigeria. Mem Inst Oswaldo Cruz. 2005;100(1):13–6. doi: 10.1590/S0074-02762005000100002. [DOI] [PubMed] [Google Scholar]
- 60.Kiire CF. The epidemiology and prophylaxis of hepatitis B in sub-Saharan Africa: a view from tropical and subtropical Africa. Gut. 1996;38(Suppl 2):S5–12. doi: 10.1136/gut.38.Suppl_2.S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sadoh AE, Eregie CO. Age at presentation for infant immunization in Nigeria: Implications for hepatitis B immunization. Public Health. 2008;122:1318–20. doi: 10.1016/j.puhe.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 62.Japhet MO, Adesina OA, Donbraye E, Adewumi MO. Hepatitis B core IgM Antibody (anti-HBc IgM) among hepatitis B surface antigen(HBsAg) negative blood donors in Nigeria. Virol J. 2011;8:513. doi: 10.1186/1743-422X-8-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Salawu L, Adegoke AO, Aboderin AO, Huraina HA. Hepatitis B viral markers in surface antigen negative blood donors: the need to look beyond antibody negativity. West Afr J Med. 2011;30(4):292–5. [PubMed] [Google Scholar]
- 64.Nna E, Mbamalu C, Ekejindu I. Occult hepatitis B viral infection among blood donors in South-Eastern Nigeria. Pathog Glob Health.2014 Jul 4:2047773214Y0000000144. [Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 65.Opaleye OO, Fagbami AH, Bolaji OS. Occult hepatitis B virus infection in fully screened blood units in Nigeria. Int. J. Infect. Dis. (16th ICID Abstracts) 2014;21(Supplement 1):455. doi: 10.1016/j.ijid.2014.03.1360. [DOI] [Google Scholar]
- 66.Oluyinka OO, Tong HV, Bui Tien S, Fagbami AH, Adekanle O, Ojurongbe O, et al. Occult Hepatitis B Virus Infection in Nigerian Blood Donors and Hepatitis B Virus Transmission Risks. PLoS One. 2015;10(7) doi: 10.1371/journal.pone.0131912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Farma E, Boeri E, Bettini P, Repetto CM, McDermott J, Lillo FB, Varnier OE. Single-step PCR in molecular diagnosis of hepatitis C virus infection. J Clin Microbiol. 1996;34(12):3171–4. doi: 10.1128/jcm.34.12.3171-3174.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hernandez-Rodriguez P, Gomez Ramirez A. Polymerase Chain Reaction: Types, Utilities and Limitations. In: Hernandez-Rodriguez P editor Polymerase Chain Reaction, 2012, ISBN: 978-953-51-0612-8, InTech, doi: 10.5772/37450. Available at: http://cdn.intechopen.com/pdfs-wm/37264.pdf. Accessed on 4 May 2016.
- 69.Smith-Zagone MJ, Pulliam JF, Farkas DH. Molecular Pathology Methods In: Leonard DGB editor. LLC, 233 Spring Street, New York, NY 10013, USA: Molecular Pathology in Clinical Practice Springer Science + Business Media; 2007
- 70.Storch GA. Diagnostic Virology In: Knipe DM, Howle PM. Fields Virology, 5th Edition. Philadelphia, PA, USA: Lippincott Williams & Wilkins; 2007
- 71.Ola SO, Otegbayo JA, Odaibo GN, Olaleye DO, Olubuyide IO, Summerton CB, Bamgboye EA. Occult HBV infection among a cohort of Nigerian adults. J Infect Dev Ctries. 2009;3(6):442–6. doi: 10.3855/jidc.415. [DOI] [PubMed] [Google Scholar]
- 72.Opaleye OO, Oluremi AS, Atiba AB, Adewumi MO, Mabayoje OV, Donbraye E, Ojurongbe O, Olowe OA. Occult Hepatitis B virus infection among HIV positive patients in Nigeria. J Trop Med. 2014 (2014), Article ID 796121, 5pages http://dx.doi.org/10.1155/2014/796121 Available at http://www.hindawi.com/journals/jtm/2014/796121/ [DOI] [PMC free article] [PubMed]
- 73.Zahn A, Li C, Danso K, Candotti D, Owusu-Ofori S, Temple J, Allain JP. Molecular characterization of occult hepatitis B virus in genotype E-infected subjects. J Gen Virol. 2008;89:409–18. doi: 10.1099/vir.0.83347-0. [DOI] [PubMed] [Google Scholar]
- 74.Gutiérrez-García ML, Fernandez-Rodriguez CM, Lledo-Navarro JL, Buhigas-Garcia I. Prevalence of occult hepatitis B virus infection. World J Gastroenterol. 2011;17(12):1538–42. doi: 10.3748/wjg.v17.i12.1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bjoerkvoll B, Viet L, Ol HS, Lan NT, Sothy S, Hoel H, Gutteberg T, Husebekk A, Larsen S, Husum H. Screening test accuracy among potential blood donors of HBsAg, anti-HBc and anti-HCV to detect hepatitis B and C virus infection in rural Cambodia and Vietnam. Southeast Asian J Trop Med Public Health. 2010;41(5):1127–35. [PubMed] [Google Scholar]
- 76.Seo DH, Whang DH, Song EY, Han KS. Occult hepatitis B virus infection and blood transfusion. World J Hepatol. 2015;7(3):600–6. doi: 10.4254/wjh.v7.i3.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chatterjee K, Agarwal N, Coshic P, Borgohain M, Chakroborty S. Sensitivity of individual and mini-pool nucleic acid testing assessed by dilution of hepatitis B nucleic acid testing yield samples. Asian J Transfus Sci. 2014;8(1):26–8. doi: 10.4103/0973-6247.126684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Arora S, Doda V, Kirtania T. Sensitivity of individual donor nucleic acid testing (NAT) for the detection of hepatitis B infection by studying diluted NAT yield samples. Blood Transfus. 2015;13(2):227–3. doi: 10.2450/2014.0048-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Vermeulen M, van Drimmelen H, Coleman C, Mitchel J, Reddy R, Lelie N. A mathematical approach to estimate the efficacy of individual-donation and minipool nucleic acid amplification test options in preventing transmission risk by window period and occult hepatitis B virus infections. Transfusion. 2014;54(10):2496–504. doi: 10.1111/trf.12657. [DOI] [PMC free article] [PubMed] [Google Scholar]


