Abstract
Muscle MRI has become a very useful tool in the diagnosis and follow-up of patients with muscle dystrophies. Muscle MRI provides us about many aspects of the structure and function of skeletal muscles, such as the presence of oedema or fatty infiltration. In the last years many reports have described the particular muscles that are involved in these muscle disease. This knowledge can facilitate the diagnosis in many cases. In the present paper we review the main changes observed in muscle MRI of patients with muscle dystrophies
Key words: Limb-girdle muscular dystrophies, muscle MRI
Introduction
Muscle MRI has become a useful tool for diagnosis and follow-up of patients with limb girdle muscle dystrophies (LGMD). Muscle MRI provides information on different aspects of muscle structure and function of muscles of the body. The sequences available allow to identify fatty infiltration (T1 or 3-point Dixon sequences) or oedema (STIR or T2) in the muscles (1). Therefore, muscle MRI is useful to select a muscle for the biopsy in patients without clear muscle weakness or in patients with a severe degree of muscle atrophy, in which muscle tissue can be completely substituted by fat. Moreover, because MRI does not use radiation, it is a good technique to follow-up the progression of the disease in patients (2). There is a growing number of evidences demonstrating that the degree of muscle fatty infiltration observed in muscle MRI correlates with the muscle strength and functional status of patients with LGMD (2-4). For this reason, muscle MRI is being progressively included as a primary endpoint in clinical trials of patients with muscle dystrophy (5, 6).
It is well known that every single muscle dystrophy induces fatty infiltration of a particular group of muscles. This fact allows investigators to design diagnosis algorithms based on the MRI findings (7). However the number of reports describing the changes observed in every muscle disease has grown in the last years and a review of the main findings observed in every disease is needed. Our aim is to describe our protocol to perform muscle MRI in patients with muscle dystrophy and to summarize the main findings of MRI studies in LGMD.
Methods
Muscle MRI protocol
Good quality Muscle MRI studies can be conducted in a 1.5 Tesla MRI scanner. In our center, we are equipped with a Phillips Achieva XR Magnetic Resonance System (Philips, Eindhoven, Netherlands). Our MRI system has a moveable tabletop that allows performing whole body studies in a short period of time (less than 30 minutes) without relocating the patient. Our standard protocol includes T1 and STIR sequences. T1 weighted spin-echo sequence obtains axial and coronal images from the head to the toes using the following parameters: repetition time: 300 ms, echo-time: 10 ms and thickness 10 mm. Short-time inversion recovery (STIR) sequences obtains coronal images using the following parameters: repetition time 2,500-3,500 ms, echo time 60 ms, inversion time 150 ms in 10 mm slices.
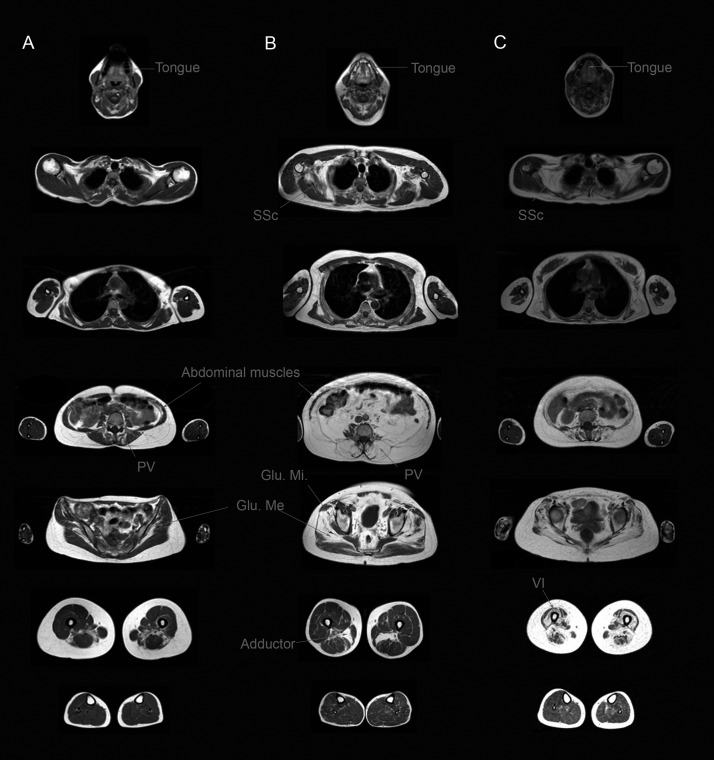
We quantify the degree of muscle fatty infiltration using the Mercuri scale modified by Fischer et al in 2008 that has been used to analyse both muscle MRI and CT scans (8) (Fig. 1):
Figure 1.
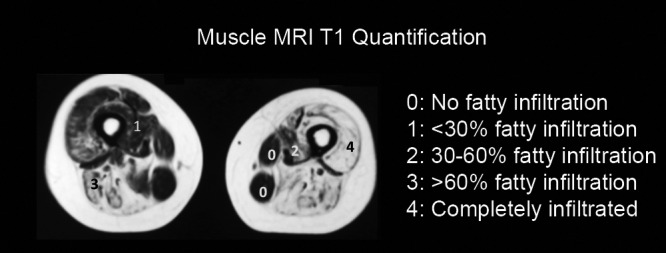
Diagram showing our quantification method of the fatty infiltration present in T1 sequences. In the image, a thigh slice is quantified using the Mercuri scale modified by Fischer.
Normal muscle appearance: 0 points.
Mild involvement: traces of increased signal intensity on the T1-weighted MR sequences: 1 point.
Moderate involvement: increased T1-weighted signal intensity with beginning confluence in less than 50% of the muscle: 2 points.
Severe involvement: increased T1-weighted signal intensity with beginning confluence in more than 50% of the muscle: 3 points.
End-stage appearance: entire muscle replaced by increased density of connective tissue and fat: 4 points.
Our protocol to analyze a whole body muscle MRI is the following: first we quantify the degree of fatty infiltration of the muscles of all body. Then, we fill out a table containing the name of the muscles with the value of the quantification. In this way, we are able to easily identify which are the most and the less involved muscles. Finally, we compare the results with the patterns already published in the literature to identify a probable diagnostic.
We use 3-point Dixon sequences for investigation purposes only, for example in natural history studies or in clinical trials. 3-point Dixon studies require a specific software to quantify the amount of fat and water per pixel in every muscle (9). Although the process of analysis of the image is longer than with T1 sequence, the results are more reliable and can be compared from one center to the other.
We use CT scan to study patients in which muscle MRI is contraindicated, for example in patients with a metallic prosthesis, a pacemaker or with claustrophobia. In these cases, whole body CT scan is performed using the following parameters: 140 kV and 120-350 mA. Section thickness is of 1.25 mm, with a section interval of 0.6 mm. The axial images are 5 mm thick, with an increment of 5 mm.
Muscle MRI in dystrophinopathies
Mutations in the dystrophin gene produce different phenotypes such as Duchenne muscle dystrophy and Becker muscle dystrophy. The MRI pattern of muscle atrophy has been well investigated both in patients with Duchenne and Becker muscle disease (4, 10, 11). In both cases the pattern is very similar. Studies have been focused on pelvic, thigh and leg muscles (Fig. 2). In general muscle atrophy is symmetric. The muscles more commonly involved are:
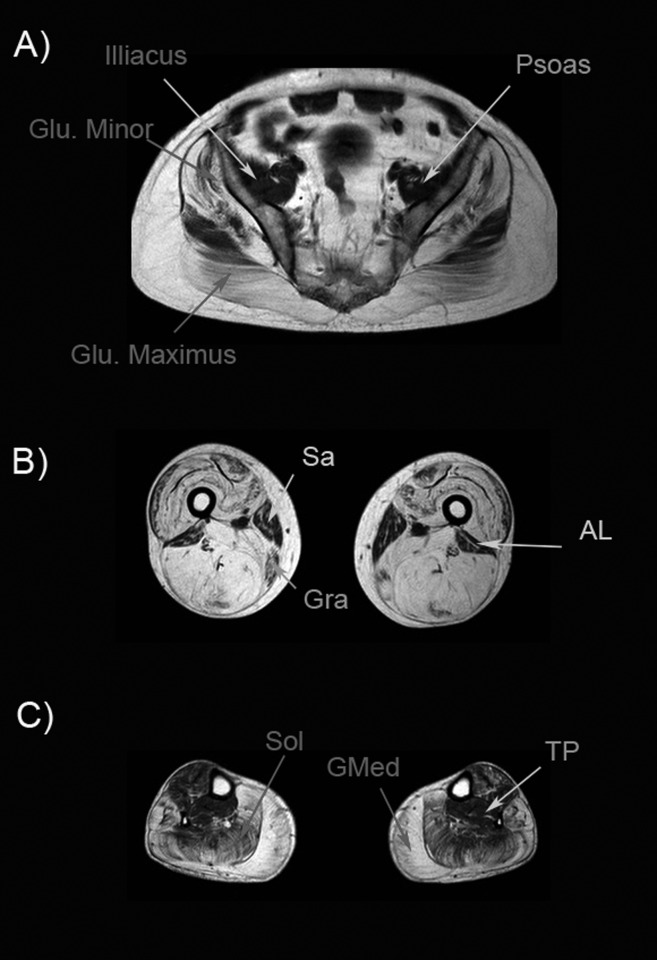
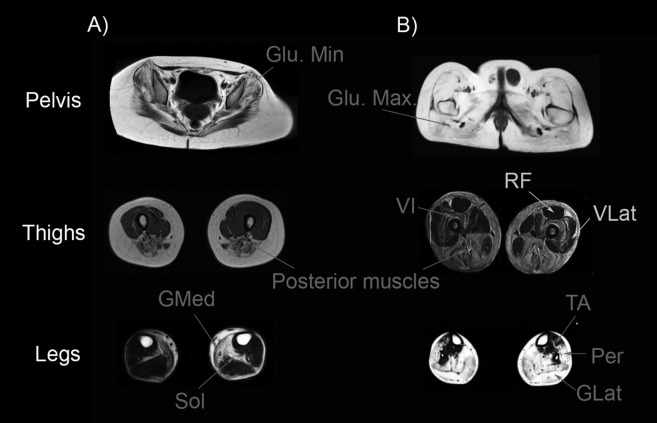
Figure 2.
Muscle MRI of a Becker muscle dystrophy patient. A) Pelvic image shows atrophy of glutei muscles (Gluteus minimus and maximus are shown in the image). Psoas and illiacus muscle are usually spared until late stages of the disease. B) Image of the thigh shows a complete atrophy of all muscles, except for sartorius (Sar), gracillis (Gra) and adductor longus (AL). C) Image of the legs showing a severe atrophy of gastrocnemius medialis (GMed) and soleus (Sol). In this patient, tibialis posterior (TP) was not involved.
Pelvis: Gluteus maximus and medius are involved from the onset of the disease and become progressively atrophied until late stages of the disease when all the glutei muscles are atrophic. In this later stage psoas and iliacus muscles could also become atrophic. Obturator internus and externus are rarely involved.
Thighs: Muscles from the anterior and posterior compartment of the thigh are involved in most of the patients, including adductor major, biceps, semi-membranosus, semitendinosus and the vasti. In contrast sartorius, gracilis and adductor longus are not involved until later stages of the disease.
Legs: There is a common involvement of both gastrocnemius, soleus and peroneus muscles. In contrast tibialis posterior is not commonly involved trough all the progression of the disease.
Keys for the diagnosis
In more than 90% of the patients there is a moderate to severe atrophy of gluteus maximus, medius, semimembranosus and the vasti (4).
Mild involvement or not involvement of psoas, iliacus, sartorius, gracilis and adductor longus. To find a normal adductor longus among completely atrophic thigh muscles is a good clue for the diagnosis.
There is only one study that has analysed muscles of upper limbs in patients with Duchenne muscle dystrophy (12), showing a preferential involvement of triceps, biceps, teres major and periscapular muscles including supraspinatus, infraspinatus and subscapularis. In contrast, deltoid is usually not involved.
The pattern of muscle atrophy of symptomatic carriers of a mutation in the dystrophin gene is very similar to the one found in Becker muscle dystrophy (13). As we have just mentioned, a normal adductor longus is a clue for the diagnosis. Moreover, many of the symptomatic carriers have clear asymmetric changes that, when present, can easily guide the diagnosis.
Muscle MRI in autosomal dominant limb girdle muscle dystrophies (AD-LGMDS)
1. LGMD1A or Myotilinopathy
Patients with mutations in the MYOT gene share a common pattern of muscle fatty infiltration on MRI studies with other myofibrillar myopathies, such as the ones produced by mutation in the ZASP and the FLNC gene [8, 14, 15] (Figure 3). The muscles involved are:
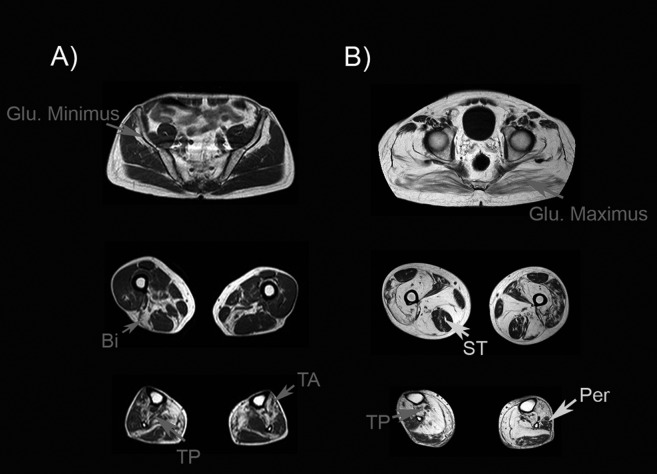
Figure 3.
Muscle MRI of two patients with mutations in the MYOT gene. A). Patient with mild weakness: muscle MRI shows mild involvement of gluteus minimus, biceps (Bi), tibialis anterior (TA) and tibialis posterior (TP). B) Patient with severe weakness: muscle MRI shows involvement of all glutei muscles, although gluteus maximus is less involved than gluteus minimus or medius. In the thighs, semitendinosus (ST) is not involved. In contrast, there is a clear involvement of the posterior muscles of the thighs. Tibialis posterior (TP) is more atrophic than peroneus muscle (Per).
Pelvis:Although there are not enough data to establish a common pattern, in our experience gluteus maximus is less involved than gluteus medius and minimus.
Thighs:In general, adductor major, biceps and semimebranosus are involved in all patients. Vasti muscles and sartorius can be also atrophic in many cases. In contrast semitendinosus is not involved until late stages of the disease.
Legs:There is a common involvement of gastrocnemius medialis, soleus, tibialis anterior and posterior. Peroneus muscles is not involved until late stages of the disease.
Keys for the diagnosis
To find a spared semitendinosus muscle associated to a severe atrophy of biceps and semimembranosus is a clue for the diagnosis.
Atrophy of tibialis posterior in a higher degree than peroneus muscle is also useful to identify this disease.
2. LGMD1B or Laminopathy
There are many publications describing the pattern of muscle involvement in patients with mutations in the LMNA gene (16-18]). The studies already published in adult patients have been focused on muscles of the lower limbs. The pattern seems to be homogeneous among patients and is characterized by a symmetric involvement of posterior muscles of the thighs and legs associated to a severe involvement of the paravertebral muscles (Figure 4). We have observed that this pattern is not different of the muscle involvement observed in patients with mutations in the STA gene (19). The muscles preferentially involved are:
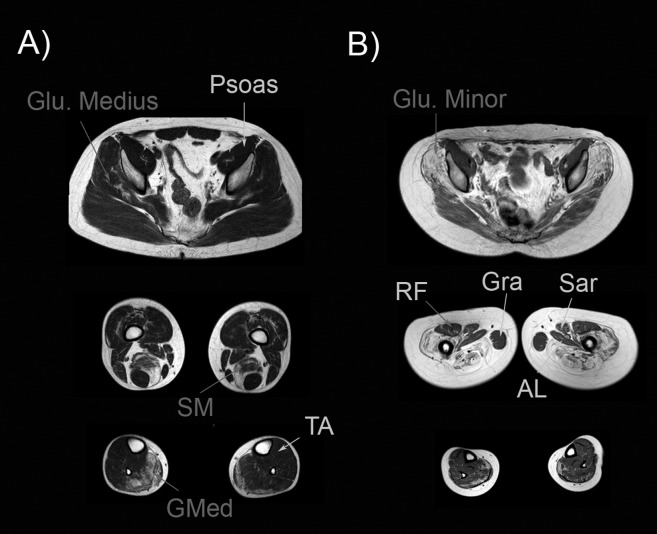
Figure 4.
Muscle MRI of two patients with mutations in the LMNA gene. A) Patient with mild weakness. In this patient we observed fatty infiltration in the gluteus medius, semimembranosus (SM) and gastrocnemius medialis (GMed) muscles. B) Patient with severe weakness: fatty infiltration was observed in gluteus minimus and medius. All the muscles of the thighs were involved, except rectus femoris (RF), adductor longus (AL), sartorius (Sar) and gracillis (Gra) that were not atrophic.
Trunk muscles:Paraspinal muscles become involved from the onset of the disease, especially multifidus and longissimus. Different to other muscle diseases, such as Pompe disease, abdominal muscles are not commonly involved during the progression of the disease.
Pelvis: Gluteus minimus and medius are involved in most of the patients, and in all the cases analysed by us these two muscles have a more severe degree of muscle atrophy than Gluteus maximus. Psoas muscle is rarely involved in these patients.
Thighs:The posterior muscles of the thighs, especially semimembranosus, the long head of biceps and the adductor major muscles are involved from the onset of the disease. In later stages semitendinosus and the short head of the biceps become also atrophic. Vasti muscles are involved in most of the patients: vastus intermedius is usually the first vasti muscle involved, followed by vastus lateralis and medialis. We have observed that the lateral part of the vastus lateralis is not involved until very late stages of the disease. Rectus femoris is normally not involved and becomes hypertrophic in many patients, as well as sartorius and gracillis muscles.
Legs:The posterior compartment of the legs is involved in all patients. Medial gastrocnemius is severely involved in most of the patients, associated in many cases to atrophy of soleus and gastrocnemius lateralis. The muscles of the anterolateral compartment are rarely involved during the progression of the disease.
Keys for the diagnosis
The combination of atrophy involving the anterior and posterior compartment of the thighs, associated to a severe atrophy of the posterior muscles of the legs and hypertrophy of rectus femoris is a very suggestive pattern of involvement in patients with mutations in the LMNA gene.
3. LGMD1C or Caveolinopathy
There is not enough information published of patients with caveolinopathy to establish a pattern of muscle involvement. We have studied patients with rippling muscle disease or isolated hyperckemia and the muscle MRI is normal in these cases.
5. LGMD1D
LGMD-1D is produced by mutations in the DNABJB6 gene. There is only one paper published reviewing the radiological features of 23 patients with this disease (20). In the initial stage of the disease, the muscles more commonly involved were the adductor major, the semimembranosus, the biceps and the soleus. In a second stage, gastrocnemius medialis and adductor longus were also involved. In advanced stages, atrophy also involved vastus medialis, laterallis and intermedius. Sartorius, rectus femoris, gracillis, gastrocnemius lateralis and the antero-lateral compartment of the legs were not involved until late stages of the disease. The most characteristic feature in this disease is a preservation of semitendinosus until latter stages, as it happens in patients with mutations in the MYOT gene.
6. LGMD-1E or Desminopathy
Patients with mutation in the DES gene develop a myofibrillar myopathy. The radiological features are very similar to those found in patients with mutation in the CRYAB gene [8]. There are many reports describing the common features in these patients, although the studies have focused mainly on thighs and legs area (Fig. 5) (14).
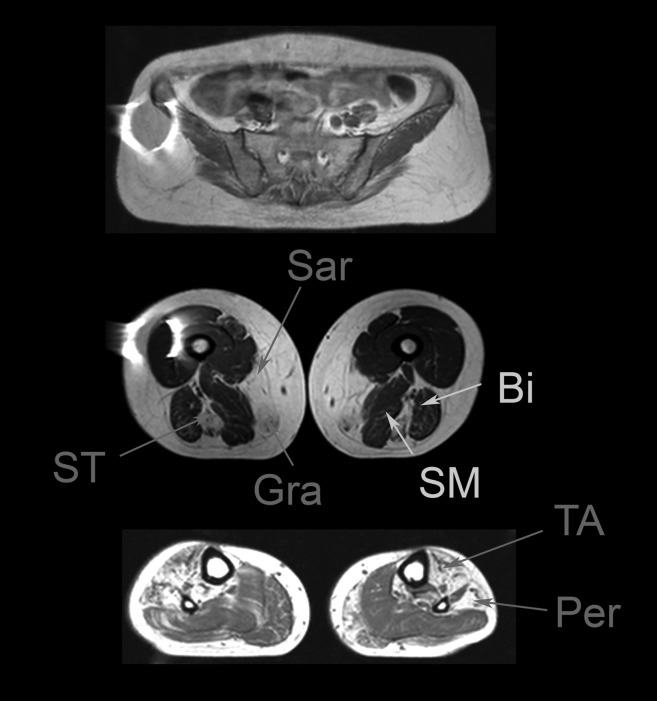
Figure 5.
Muscle MRI of a patient with mutation is the DES gene. Muscle MRI shows a preferential involvement of semitendinosus (ST), sartorius (Sar) and gracillis (Gra) muscles, while in contrast semimembranosus (SM) and biceps (Bi) are not involved. In the legs, there is an involvement of tibialis anterior (TA) and peroneus muscles (Per). Courtesy of Dr. Giorgio Tasca.
Thighs:Fatty infiltration involving the semitendinosus, the gracillis and the sartorius muscles occurs from the onset of the disease. This pattern is very suggestive of desminopathy and is not commonly observed in other diseases. Latter on, the vasti can also be involved.
Legs: Peroneus is the most commonly involved muscle in these patients, associated commonly to atrophy of the posterior muscles of the legs.
Muscle MRI in autosomal recessive limb girdle muscle dystrophies (AR-LGMDS)
1. LGMD2A or calpainopathy
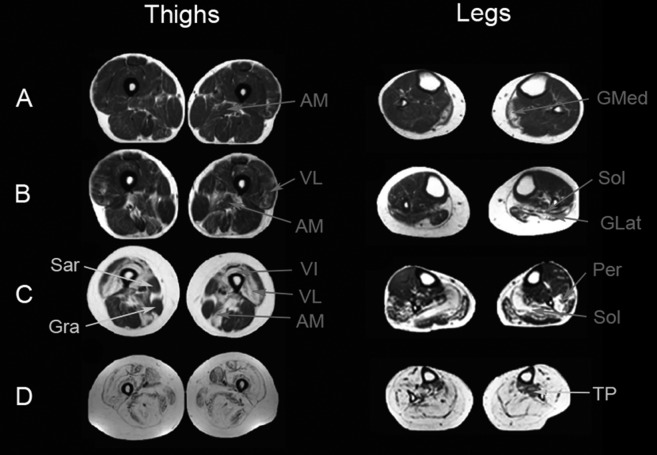
There is an important variability in the patterns described in patients with mutations in the CAPN3 gene (21-23). However there are some common traits that can be found in most of the patients (Figure 6). The common muscles involved in this disease are:
Figure 6.
Muscle MRI in patients with mutations in the CAPN3 gene. Gluteus minimus and medius tend to be more involved than gluteus maximus (A) in most of the patients, although in advanced stages, all glutei muscles can be completely atrophic. In general, posterior muscles of the thigh are more severely involved than anterior muscles (A), but is not uncommon to find involvement of vasti muscles, especially vastus intermedius (VI). Atrophy of gastrocnemius medialis (GMed) and soleus (Sol) is frequently found (A), but in advanced cases (B) is not uncommon to find atrophy of gastrocnemius lateralis (GLat), peroneus (Per) and tibialis anterior (TA) muscles.
Trunk and pelvis area: Paravertebral muscles are involved in most of the patients from the onset of the disease. In contrast, abdominal muscles are rarely involved and they are not affected until late stages. The glutei muscles are also involved from the onset, especially glutei medius and minimus, while glutei maximus tend to be involved in more advanced patients (24). Psoas muscles is not commonly involved until late stages.
Thighs: Adductor major and longus and semimembranosus are the first muscles involved. Later on the progression of the disease, the rest of the muscles of the posterior compartment of the thigh become involved. In many patients there is a clear difference between the anterior muscles (normally spared) and posterior muscles (atrophic) of the thighs. However, involvement of the anterior compartment is not uncommon, and is frequently observed in medium and advanced patients. The vasti muscles are involved: in a first step the vastus intermedius and then the vastus medialis and laterallis. Rectus femoris can also be involved in many patients. In general, sartorius and gracillis are not involved until very late stages of the disease.
Legs: One of the clues for the diagnosis is the common involvement of gastrocnemius medialis and soleus from the onset of the disease. However, as the disease advances, atrophy involves the gastrocnemius lateralis, the peroneus and the tibialis anterior.
Tibialis posterior is not commonly involved until very late stages of the disease.
Keys for the diagnosis
Predominant involvement of posterior muscles of the thighs associated to atrophy of gastrocnemius medialis and soleus.
The lateral part of the vastus laterallis is not involved until late stages of the disease. Different to other diseases, rectus femoris is also involved in many patients.
2. LGMD2B or disferlinopathy
The reports published on the radiological features of patients with mutation in the DYSF gene have mainly been focused in the study of the lower limbs (Fig. 7). The two most common phenotypes associated to mutations in the DYSF gene, the limb girdle muscle dystrophy and the distal posterior myopathy (Miyoshi myopathy) are not differentiable using MRI (2, 25). Common muscles involved are:
Figure 7.
Progression of muscle atrophy in patients with mutations in the DYSF gene. There is a mild involvement of the adductor major (AM) and gastrocnemius medialis (GMed) in the first stages of the disease (A). In a second stage (B), atrophy involves also the vastus lateralis (VL) and the soleus (Sol). Then (C), fatty infiltration progresses and involves the rest of the vasti muscles and the posterior muscles of the thighs, but sartorius (sar) and gracillis (gra) are commonly not involved. In the legs, the vastus lateralis and peroneus become atrophic. In the most advanced stages (D), all the muscles are infiltrated by fat, but in some patients tibialis posterior (TP) may be not involved.
Pelvis: Glutei minimus is commonly inlvoved in dysferlin patients. However, the glutei medius and maximus are also involved later on the progression of the disease. Psoas muscles may be not involved until late stages of the disease.
Thighs: Adductor muscles are involved from the onset of the disease. The first change is an hyperintense signal in STIR sequences, reflecting the presence of oedema before fatty muscle infiltration is observed in T1 sequences (2). Vastus lateralis, medialis and intermedius are involved early in the progression of the disease. Later on, posterior muscles of the thighs, especially the semitendinosus and the semimembranosus become atrophic. Biceps short head is less affected in many patients, until late stages of the disease when all muscles of the thighs, except sartorius and gracillis become atrophic.
Legs: An hyperintense signal in STIR sequences involving the gastrocnemius mediallis is commonly observed at the onset of the diseases. Atrophy involves this muscle first and then progress affecting gastrocnemius lateralis and soleus. In a more advanced stage antero-lateral muscles are also atrophied. Tibialis posterior is not involved until late stages.
Clues for the diagnosis
STIR hyperintensities in adductor and gastrocnemius medialis muscles at the onset of the disease (26, 27).
Involvement of the vasti muscles early in the progression of the disease associated to atrophy of adductor muscles and gastrocnemius medialis.
3. Sarcoglycanopathies (LGMD 2C-F)
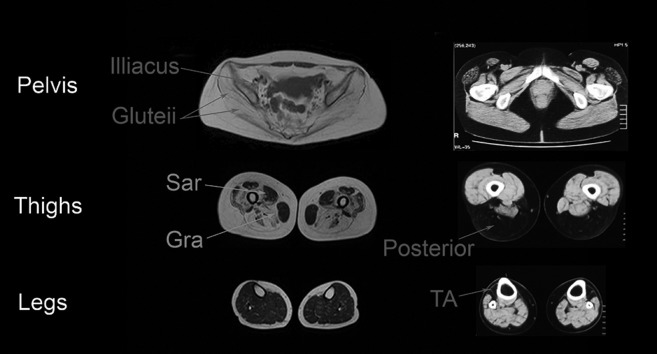
The radiologic characteristics of the patients with mutations in the sarcoglycan genes are not fully established. There are only some case reports published (24). In our experience, the pattern seems to be homogeneous among patients (Tasca et al, in preparation). There is a severe involvement of all glutei muscles and the psoas in most of the patients reported. In the legs, muscles of the anterior and posterior compartment are also severely affected from the onset without involvement of sartorius and gracillis. Different to other muscle dystrophies, muscles of the legs are not involved until late stages of the disease (Figure 8).
Figure 8.
Muscle MRI of patients with sarcoglycanopathy and titinopathy. A: 35 years old patient with LGMD-2D: there is a severe involvement of pelvic muscles (including glutei and psoas muscles) and thigh muscles. Sartorius (sar) and gracillis (gra) are not involved until advanced stages of the diseases. In contrast leg muscles are not involved. B: Muscle CT of a 62 years old patient with distal titinopathy: preferential involvement of the tibialis anterior (TA) and the posterior muscles of the thighs is observed. In contrast, the pelvis muscles are not involved.
4. LGMD-2I
LGMD-2I is produced by mutations in the FKRP gene. Muscle MRI features have been widely reported (24, 28), and the pattern seems to be very similar to patients with mutation in the CAPN3 gene.
Pelvis: Glutei muscles are involved from the onset of the disease, being severely involved in patients in a intermediate stage of the disease. Psoas and illiacus muscles are not involved until late stages of the disease.
Thighs: The posterior compartment of the legs is involved from the onset of the disease. Biceps, semitendinosus and semimembranosus are the most severely involved muscles in these patients. Vasti muscles are progressively involved in LGMD-2I patients. Vastus intermedius is the most common vasti muscle involved, associated to a variable degree of involvement of vastus lateralis and medialis. Rectus femoris can be involved in many cases, associate to atrophy of the adductor muscle. In later stages all muscles can be involved, being sartorius and gracillis the less atrophic muscles.
Legs: Both gastrocnemius and soleus are involved from the onset of the disease. In later stages, peroneus and tibialis anterior become also involved, although they are commonly less atrophic than the posterior muscles of the legs.
Clues for the diagnosis
Severe involvement of glutei muscles associated to atrophy of the posterior muscles of the thighs and legs.
Vastus intermedius is more involved than lateralis and medialis in many cases. In general atrophy affects first vastus medialis than lateralis.
5. LGMD2J or Titinopathy
Patients with the classical titin phenotype in which there is a preferential involvement of the tibialis anterior, have a very characteristic muscle MRI (7). It is very common to find an isolated atrophy of the tibialis anterior muscle, that can be the only muscle affected during many years. Later on the progression of the disease, atrophy can also affect soleus muscles, the posterior compartment of the thighs and the rectus femoris (Fig. 8).
In recent years, many different phenotypes of muscle disease have been associated to mutations in the TTN gene, including congenital myopathies or patients with proximal weakness of the lower and upper extremities. There is not a clear muscle MRI pattern in these cases.
However, patients with the hereditary myopathy and early respiratory failure phenotype (HMERF), have a common pattern of muscle MRI involvement. It has been reported that illiacus, psoas, obturator, semitendinosus, sartorius and gracillis are commonly involved in these patients.
6. LGMD2L
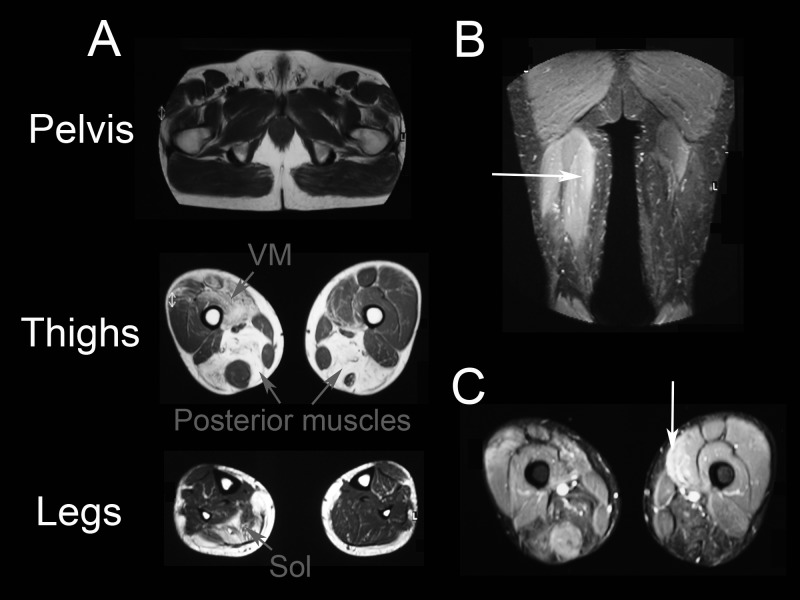
LGMD 2L is produced by mutations in the ANO5 gene. Although this disease has been recently described, the muscle MRI pattern is very well known and seems to be homogenous among patients (29, 30) (Fig. 9). In these cases, muscle MRI features are very similar to those described in patients with mutations in the DYSF gene (31). The common muscles involved are:
Figure 9.
Muscle MRI of a patient with mutations in the ANO5 gene. A: Muscle MRI of a 53 years old patient with mild involvement of the lower limbs. Axial images showed no involvement of pelvic muscles, but in contrast there was a clear asymmetric involvement of vastus lateralis (VL) and posterior muscles of the thighs. In the legs, muscles of the posterior compartment were also involved, including soleus (Sol) and gastrocnemius medialis. B and C: hypenintensities in STIR sequences were observed in the posterior muscles of the thighs and in the vastus medialis muscle (arrows).
Pelvis: Glutei, psoas and illiacus muscles are commonly not involved until late stages of the disease.
Thighs: Adductor muscles and posterior muscles of the thighs, especially the semitendinosus (32), are involved from the onset of the disease. As the weakness progresses there is an involvement of the vastus lateralis, medialis and intermedius. As in dysferlinopathy patients, sartorius, gracilllis and rectus femoris are not involved until late stages. STIR hyperintensisities are commonly observed in many muscles before atrophy is clearly detected in T1 sequences. The presence of asymmetries in the degree of muscle atrophy is very common among patients.
Legs: Soleus and gastrocnemius medialis are commonly involved from the onset of the disease, followed by atrophy of the gastrocnemius lateralis, peroneus and tibialis anterior muscles.
Clues for the diagnosis
Asymmetric involvement of the thighs muscles, especially in the degree of involvement of the vasti muscles.
Glutei muscles are less involved than muscles of the thighs and legs until very late in the disease.
Increase in the STIR signal is observed in many cases from the onset of the disease.
Muscle MRI in other hereditary myopathies
1. Adult onset Pompe disease
Pompe disease, also known as glycogenosis type II, can manifest as slowly progressive weakness involving axial and proximal muscles of the limbs. Pompe patients are in many cases misdiagnosed as patients with muscle dystrophies. Muscle MRI is very useful to identify these patients, as the pattern has been widely described and seems to be very characteristic (Fig. 10). There is a preferential involvement of tongue from the onset of the disease, also in patients without clear clinical involvement of this muscle. Periscapular muscles are commonly involved, especially the subscapularis muscle that is atrophic in many cases (33). Paravertebral muscles are affected early in the progression of the disease, especially the multifidus and longissimus muscle (34). Atrophy of the abdominal muscles runs parallel to progression of the disease. Patients may develop a severe atrophy of rectus abdominalis, obliquus internus and externus and trasversus abdominalis. Glutei muscles are also involved in all patients. In general these muscles are more involved than psoas-illiacus muscles. The involvement of the adductor muscles occurs early in the progression of the disease followed by involvement of posterior muscles of the thighs, vastus intermedius and finally vastus lateralis and medialis (35). In most of the cases, there is not involvement of the muscles of the legs, than can be normal also in wheel-chair bound patients.
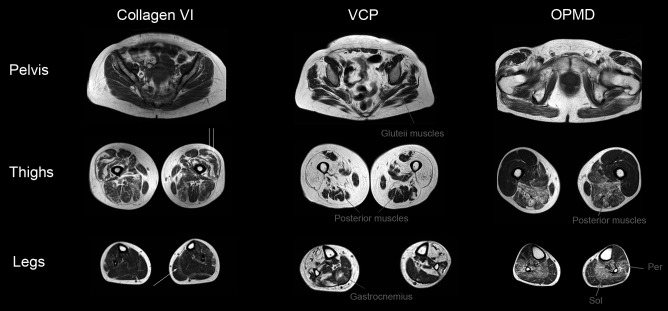
Figure 10.
Muscle MRI of patients with Pompe disease. A: Whole body muscle MRI of a 35 years olf patient with mild muscle involvement showing atrophy of tongue, paravertebral and abdominal muscles, gluteus medius (Glu.Me) and posterior muscles of the thighs. B: Muscle MRI of a 43 years old patients with moderate weakness showing involvement of tongue, subscapularis (SSc), paravertebral and abdominal muscles, gluteus medius (Glu.Me) and gluteus minimus and adductor major (AM). C: Muscle MRI of a 44 years old patients with severe weakness showing involvement of tongue, subscapularis (SSc), paravertebral, abdominal, all glutei muscles and anterior and posterior muscles of the thighs.
2. Myopathies associated to mutations in the VCP gene
Mutations in the VCP gene have been associated to a characteristic triad of diseases: myopathy with proximal and/ or distal involvement in the upper and lower limbs, Paget disease and fronto-temporal dementia (36). Although the muscle MRI pattern has not been published, in our experience atrophy involves muscles of the pelvis, thighs and legs. The most characteristic finding in this disease is that fatty infiltration is not homogeneous and in many cases shows a patchy distribution among the muscles (Fig. 11).
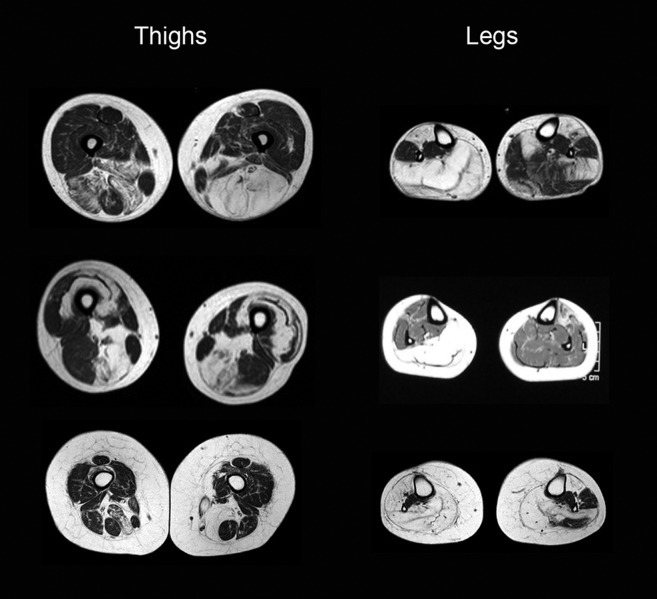
Figure 11.
Muscle MRI of patients with collagen VI related myopathy, HIBMPD and OPMD muscle dystrophies. A: Muscle MRI of a 20 years old patient with mutations in the COL6A3 gene showing concentric atrophy of the vastus lateralis (double arrow) and a band of atrophy between gastrocnemius medialis and soleus (single arrow). B: Muscle MRI of a 56 years old woman with a mutation in the VCP gene producing patchy atrophy of the glutei, posterior muscles of the thighs and both gastrocnemius. C: Muscle MRI of a 72 years old patient with OPMD showing preferential involvement of posterior muscles of the thighs and the soleus muscle.
3. Oculo-pharingeal muscle dystrophy
OPMD disease is characterized by the triad of ptosis, dysphagia and proximal weakness of the lower and upper limbs. Although the symptoms are very suggestive, sometimes it can be difficult to differentiate these patients from patients with mitochondrial myopathy. In our experience, muscle MRI is useful in this case. Muscle MRI of the pelvis shows a progressive involvement of glutei muscles, specially glutei minimus. Psoas is also involved early in the progression of the disease. In the thighs there is a preferential involvement of posterior muscles of the thighs and of the adductor muscles. In the legs, soleus and peroneus muscles are commonly involved early. In fact, soleus is commonly more atrophic than gastrocnemius muscles also in advanced patients (37) (Fig. 11).
4. Collagen VI related myopathies.
Although mutations in one of the three COLVI genes have been commonly related with congenital muscle dystrophies, this disease can also present during the adulthood. Muscle MRI is highly specific and has been described elsewhere. The main finding is a muscle atrophy involving the periphery of the vastus lateralis and medialis, while the center of the muscle is not involved (38). This pattern has been described as concentric atrophy (Fig. 11). A similar pattern can also be observed in the gastrocnemius medialis, where there is a ring of atrophy between the gastrocnemius medialis and soleus muscle. Muscle atrophy can also involve other muscles, such as the rectus femoris muscle, the posterior compartment of the thighs, the paravertebral muscles and the upper limbs muscles. In this latter case, a band of muscle atrophy is commonly observed in the triceps and in the subscapularis. It has been suggested than in those patients with unknown mutations showing this characteristic pattern, genetic tests can be performed without histologic demonstration of collagen VI deficiency.
5. Facio-scapulo-humeral muscle dystrophy (FSHD)
The clinical diagnosis of FSHD is easy to achieve based only in clinical symptoms in most of the patients. However, muscle MRI studies can be helpful in unclear cases. Although FSHD is one of the most common muscle diseases, there are not enough studies on which patterns are commonly observed in this disease. Tasca and collaborators studied MRI muscle involvement of the upper limbs and reported a preferential involvement of periscapular muscles including trapezius, serratus anterior, latissimus dorsi, pectoralis major and rhomboids (39). In contrast, supraspinatus, infraspinatus and subscapularis were not commonly involved in this disease. The frequency of asymmetric involvement was very high. The studies focused on lower limbs have shown a predominant involvement of Tibialis anterior in most of the cases (40). Other muscles can also be atrophic such as the vastii, the posterior compartment of the thighs and both gastrocnemius. Asymmetric changes were also very common in the lower limbs, and this is probably the most important clue for the radiologic diagnosis of the disease (Fig. 12).
Figure 12.
Muscle MRI of patients with Facio-Scapulo-Humeral muscle dystrophy. Muscle MRI of different patients with FSH muscle dystrophy showing asymmetries in the thighs and legs studies.
Conclusions
Muscle MRI has become a useful tool in the diagnosis of patients with muscle dystrophies. The standardization of the study protocols has allowed obtaining information from many patients with different muscle diseases. But still, most of the studies published are performed in relatively small cohorts of patients and are in general transversal. More information regarding progression of the atrophy during the natural history of the disease is needed. Collaboration between different study groups is necessary to increase the number of patients analyzed and to include patients in different clinical stages (from presymptomatic to advanced patients). In this sense the effort performed by the European Comission creating an ECOST action centered in the application of muscle MRI to the study of muscle diseases is remarkable (http://myomri.eu). Patients associations have also shown interest in radiological studies. This is the case of the Jain Foundation that sponsors a clinical-radiological study to describe the natural history of patients with LGMD-2B that has already recruited 196 patients all over the world (http://www.jain-foundation.org). Although the diagnosis of muscle dystrophies still continues to be based on a careful clinical history, a detailed physical examination and a complete study of the muscle biopsy, information on the muscle MRI pattern could be helpful for the genetic diagnosis of these diseases. Along the same lines, a high level of expertise is needed to identify muscle MRI patterns, that in many cases are not patognomonic of a single disease (41). In this sense, the creation of training schools will improve the level of knowledge among radiologists and neurologists all over the world, making muscle MRI studies more useful for clinical practice.
Acknowledgements
We would like to thank Giorgio Tasca for his contribution to the manuscript and all the staff of our radiology department for their patience with us and with the patients. We would like to thanks the patients for their continuous support in clinical research. this work has been supported by grants from the Instituto de Salud Carlos III to EG (PI 12/02291) and to JDM (PI 15/01822)
References
- 1.Carlier PG, Mercuri E, Straub V. Applications of MRI in muscle diseases. Neuromuscul Disord. 2012;22(Suppl 2):S41–S41. doi: 10.1016/j.nmd.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 2.Paradas C, Llauger J, Diaz-Manera J, et al. Redefining dysferlinopathy phenotypes based on clinical findings and muscle imaging studies. Neurology. 2010;75:316–323. doi: 10.1212/WNL.0b013e3181ea1564. [DOI] [PubMed] [Google Scholar]
- 3.Dahlqvist JR, Vissing CR, Thomsen C, Vissing J. Severe paraspinal muscle involvement in facioscapulohumeral muscular dystrophy. Neurology. 2014;83:1178–1183. doi: 10.1212/WNL.0000000000000828. [DOI] [PubMed] [Google Scholar]
- 4.Tasca G, Iannaccone E, Monforte M, et al. Muscle MRI in Becker muscular dystrophy. Neuromuscul Disord. 2012;22(Suppl 2):S100–S106. doi: 10.1016/j.nmd.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 5.Arpan I, Willcocks RJ, Forbes SC, et al. Examination of effects of corticosteroids on skeletal muscles of boys with DMD using MRI and MRS. Neurology. 2014;83:974–980. doi: 10.1212/WNL.0000000000000775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hollingsworth KG. Quantitative MRI in muscular dystrophy: An indispensable trial endpoint? Neurology. 2014;83:956–957. doi: 10.1212/WNL.0000000000000785. [DOI] [PubMed] [Google Scholar]
- 7.Udd B. Distal myopathies - new genetic entities expand diagnostic challenge. Neuromuscul Disord. 2012;22:5–12. doi: 10.1016/j.nmd.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Fischer D, Kley RA, Strach K, et al. Distinct muscle imaging patterns in myofibrillar myopathies. Neurology. 2008;71:758–765. doi: 10.1212/01.wnl.0000324927.28817.9b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hollingsworth KG, Sousa PL, Straub V, et al. Towards harmonization of protocols for MRI outcome measures in skeletal muscle studies: consensus recommendations from two TREATNMD NMR workshops, 2 May 2010, Stockholm, Sweden, 1-2 October 2009, Paris, France. Neuromuscul Disord. 2012;22(Suppl 2):S54–S67. doi: 10.1016/j.nmd.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 10.Liu M, Chino N, Ishihara T, et al. Muscle damage progression in Duchenne muscular dystrophy evaluated by a new quantitative computed tomography method. Arch Phys Med Rehabil. 1993;74:507–514. doi: 10.1016/0003-9993(93)90115-q. [DOI] [PubMed] [Google Scholar]
- 11.Finanger EL, Russman B, Forbes SC, et al. Use of skeletal muscle MRI in diagnosis and monitoring disease progression in Duchenne muscular dystrophy. Phys Med Rehabil Clin N Am. 2012;23:1–10. doi: 10.1016/j.pmr.2011.11.004. ix. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Faridian-Aragh N, Wagner KR, Leung DG, Carrino JA. Magnetic resonance imaging phenotyping of Becker muscular dystrophy. Muscle Nerve. 2014;50:962–967. doi: 10.1002/mus.24246. [DOI] [PubMed] [Google Scholar]
- 13.Tasca G, Monforte M, Iannaccone E, et al. Muscle MRI in female carriers of dystrophinopathy. Eur J Neurol. 2012;19:1256–1260. doi: 10.1111/j.1468-1331.2012.03753.x. [DOI] [PubMed] [Google Scholar]
- 14.Olive M, Odgerel Z, Martinez A, et al. Clinical and myopathological evaluation of early- and late-onset subtypes of myofibrillar myopathy. Neuromuscul Disord. 2011;21:533–542. doi: 10.1016/j.nmd.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McNeill A, Birchall D, Straub V, et al. Lower limb radiology of distal myopathy due to the S60F myotilin mutation. Eur Neurol. 2009;62:161–166. doi: 10.1159/000227266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carboni N, Mura M, Marrosu G, et al. Muscle MRI findings in patients with an apparently exclusive cardiac phenotype due to a novel LMNA gene mutation. Neuromuscul Disord. 2008;18:291–298. doi: 10.1016/j.nmd.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 17.Carboni N, Mura M, Marrosu G, et al. Muscle imaging analogies in a cohort of patients with different clinical phenotypes caused by LMNA gene mutations. Muscle Nerve. 2009;41:458–463. doi: 10.1002/mus.21514. [DOI] [PubMed] [Google Scholar]
- 18.Mercuri E, Clements E, Offiah A, et al. Muscle magnetic resonance imaging involvement in muscular dystrophies with rigidity of the spine. Ann Neurol. 2010;67:201–208. doi: 10.1002/ana.21846. [DOI] [PubMed] [Google Scholar]
- 19.Díaz-Manera J, Alejaldre A, González L, et al. Muscle imaging in muscle dystrophies produced by mutations in the EMD and LMNA genes. Neuromuscul Disord. 2016;26:33–40. doi: 10.1016/j.nmd.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 20.Sandell SM, Mahjneh I, Palmio J, et al. 'Pathognomonic' muscle imaging findings in DNAJB6 mutated LGMD1D. Eur J Neurol. 2013;20:1553–1559. doi: 10.1111/ene.12239. [DOI] [PubMed] [Google Scholar]
- 21.Wattjes MP, Kley RA, Fischer D. Neuromuscular imaging in inherited muscle diseases. Eur Radiol. 2010;20:2447–2460. doi: 10.1007/s00330-010-1799-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mercuri E, Bushby K, Ricci E, et al. Muscle MRI findings in patients with limb girdle muscular dystrophy with calpain 3 deficiency (LGMD2A) and early contractures. Neuromuscul Disord. 2005;15:164–171. doi: 10.1016/j.nmd.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 23.Stramare R, Beltrame V, Borgo R, et al. MRI in the assessment of muscular pathology: a comparison between limb-girdle muscular dystrophies, hyaline body myopathies and myotonic dystrophies. La Radiologia Medica. 2010;115:585–599. doi: 10.1007/s11547-010-0531-2. [DOI] [PubMed] [Google Scholar]
- 24.Fischer D, Walter MC, Kesper K, et al. Diagnostic value of muscle MRI in differentiating LGMD2I from other LGMDs. J Neurol. 2005;252:538–547. doi: 10.1007/s00415-005-0684-4. [DOI] [PubMed] [Google Scholar]
- 25.Kesper K, Kornblum C, Reimann J, et al. Pattern of skeletal muscle involvement in primary dysferlinopathies: a whole-body 3.0-T magnetic resonance imaging study. Acta Neurol Scand. 2009;120:111–118. doi: 10.1111/j.1600-0404.2008.01129.x. [DOI] [PubMed] [Google Scholar]
- 26.Paradas C, Gonzalez-Quereda L, Luna N, et al. A new phenotype of dysferlinopathy with congenital onset. Neuromuscul Disord. 2009;19:21–25. doi: 10.1016/j.nmd.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 27.Jethwa H, Jacques TS, Gunny R, et al. Limb girdle muscular dystrophy type 2B masquerading as inflammatory myopathy: case report. Pediatric Rheumatology online journal. 2013:11–19. doi: 10.1186/1546-0096-11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Willis TA, Hollingsworth KG, Coombs A, et al. Quantitative magnetic resonance imaging in limb-girdle muscular dystrophy 2I: a multinational cross-sectional study. Plos One. 2014;9:e90377–e90377. doi: 10.1371/journal.pone.0090377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sarkozy A, Deschauer M, Carlier RY, et al. Muscle MRI findings in limb girdle muscular dystrophy type 2L. Neuromuscul Disord. 2012;22(Suppl 2):S122–S129. doi: 10.1016/j.nmd.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 30.Hicks D, Sarkozy A, Muelas N, et al. A founder mutation in Anoctamin 5 is a major cause of limb-girdle muscular dystrophy. Brain. 2011;134:171–182. doi: 10.1093/brain/awq294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mahjneh I, Bashir R, Kiuru-Enari S, et al. Selective pattern of muscle involvement seen in distal muscular dystrophy associated with anoctamin 5 mutations: a follow-up muscle MRI study. Neuromuscul Disord. 2012;22(Suppl 2):S130–S136. doi: 10.1016/j.nmd.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 32.Tasca G, Evila A, Pane M, et al. Isolated semitendinosus involvement in the initial stages of limb-girdle muscular dystrophy 2L. Neuromuscul Disord. 2014;24:1118–1119. doi: 10.1016/j.nmd.2014.06.442. [DOI] [PubMed] [Google Scholar]
- 33.Carlier RY, Laforet P, Wary C, et al. Whole-body muscle MRI in 20 patients suffering from late onset Pompe disease: Involvement patterns. Neuromuscul Disord. 2011;21:791–799. doi: 10.1016/j.nmd.2011.06.748. [DOI] [PubMed] [Google Scholar]
- 34.Alejaldre A, Diaz-Manera J, Ravaglia S, et al. Trunk muscle involvement in late-onset Pompe disease: study of thirty patients. Neuromuscul Disord. 2012;22(Suppl 2):S148–S154. doi: 10.1016/j.nmd.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 35.Pichiecchio A, Uggetti C, Ravaglia S, et al. Muscle MRI in adultonset acid maltase deficiency. Neuromuscul Disord. 2004;14:51–55. doi: 10.1016/j.nmd.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 36.Kimonis VE, Mehta SG, Fulchiero EC, et al. Clinical studies in familial VCP myopathy associated with Paget disease of bone and frontotemporal dementia. Am J Med Genet A. 2008;146A:745–757. doi: 10.1002/ajmg.a.31862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.King MK, Lee RR, Davis LE. Magnetic resonance imaging and computed tomography of skeletal muscles in oculopharyngeal muscular dystrophy. J Clin Neuromuscul Dis. 2005;6:103–108. doi: 10.1097/01.cnd.0000152060.57673.25. [DOI] [PubMed] [Google Scholar]
- 38.Mercuri E, Lampe A, Allsop J, et al. Muscle MRI in Ullrich congenital muscular dystrophy and Bethlem myopathy. Neuromuscul Disord. 2005;15:303–310. doi: 10.1016/j.nmd.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 39.Tasca G, Monforte M, Iannaccone E, et al. Upper girdle imaging in facioscapulohumeral muscular dystrophy. PLoS One. 2014;9:e100292–e100292. doi: 10.1371/journal.pone.0100292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Leung DG, Carrino JA, Wagner KR, Jacobs MA. Whole-body magnetic resonance imaging evaluation of facioscapulohumeral muscular dystrophy. Muscle Nerve. 2015;52:512–520. doi: 10.1002/mus.24569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dam L, Kooi AJ, Wattingen M, Haan RJ, Visser M. Reliability and accuracy of skeletal muscle imaging in limbgirdle muscular dystrophies. Neurology. 2012;79:1716–1723. doi: 10.1212/WNL.0b013e31826e9b73. [DOI] [PubMed] [Google Scholar]