Abstract
Over one billion Muslims worldwide fast during the month of Ramadan. Ramadan fasting brings about some changes in the daily lives of practicing Muslims, especially in their diet and sleep patterns, which are associated with the risk of cardiovascular diseases. Over the years, many original studies have made the effort to identify the possible impact of the Ramadan fast on cardiovascular diseases. This systematic review and meta-analysis is an attempt to present the summary of key findings from those articles and an appraisal of selected literature. A systematic search using keywords of “;Ramadan fasting” and “;cardiovascular diseases” was conducted in primary research article and gray-literature repositories, in combination with hand searching and snow balling. Fifteen studies were finally selected for data extraction on the outcomes of stroke, myocardial infarction, and congestive heart failure. The analysis revealed that the incidence of cardiovascular events during the Ramadan fast was similar to the nonfasting period. Ramadan fast is not associated with any change in incidence of acute cardiovascular disease.
Keywords: Fasting, meta-analysis, Ramadan, systematic review
INTRODUCTION
Fasting over a prescribed period of time is a common religious tradition practiced by several prominent faiths in the world. It is also currently regaining interest as a medical practice, both as preventive and as therapy and/or simple choice of lifestyle. Fasting takes different forms: Complete (total abstinence from food and water), liquid only (only water/liquid is consumed), partial (low calories of about 300 kcal/day), continuous or intermittent. For Muslims, fasting during the day in Ramadan (the 9th month of the Islamic lunar calendar) is one of the five pillars of the Islam.[1] This spiritual practice includes refraining from food, drink, sexual activities, and any form of ingestion into the body from dawn until dusk.[2]
A common tradition for people fasting during Ramadan is to eat a prefast meal called “;Suhoor” before initiating the fast, which then ends with a postsunset meal called “;Iftar.”[3,4] It is also common for many cultures around the world to take another meal during the night between the Iftar and Suhoor. Fasting is obligatory on all adult Muslims, male and female except for individuals with medical conditions that prohibit them from fasting.[5]
All these changes of schedules in dietary intake are accompanied by major changes in the sleep habits that might lead to sleep deprivation during this month. Furthermore, some patients who follow the religious rituals rigidly arrange to change their medication schedule to suit the fasting practice. Furthermore, during Ramadan, there is also a tendency to consume more fat-rich, carbohydrate-rich, sugar-rich sweet food and liquid. Hence, fasting during Ramadan is essentially a drastic change in the lifestyle of the devotees for a full lunar month (29 or 30 days). This might contribute to biochemical and physiological variations in the people who fast during Ramadan;[6] especially in those for whom there is a marked change in dietary and sleep habits from their normal daily lifestyle at other times of the year. This systematic review aims to summarize the effect of Ramadan fasting on the occurrences of cardiovascular diseases, including stroke, myocardial infarction (MI), and congestive heart failure (CHF).
METHODS
Search strategy
We systematically searched the following electronic databases: Medline Embase, EBM Reviews (including Cochrane), PubMed, PubMed Central, Scopus, Web of Science, CINAHL, Nursing Reference Center, and Academic Search Complete (health source - consumer edition, health source: Nursing/academic edition Medline) for studies that showed the effect of Ramadan on CHF, MI, and stroke. In addition, we searched OpenDOAR, health sciences online, turning research into practice, OAIster (WorldCat), Canadian Institute for Health Information, Public Health Agency of Canada, Health Canada, and National Institutes of Health (NIH) for gray literature on the same topic. Medical subject heading terms and keywords for CHF (CHF/heart failure/heart disease/cardiac disease/cardiac failure), MI (MI/heart attack), and stroke were combined with Ramadan/fasting. We did not limit our search to any time period.
Screening process
AP(population): Muslim, I (Intervention): Ramadan, C (comparison): Before and after Ramadan, O (observation) (PICO) statement was set for the screening of the extant literature: Incidences or diagnosis of CHF, MI, and stroke. Initially, the articles were screened by abstracts and titles. Conference abstracts, reviews, and research manuscripts that did not match with the PICO statement were excluded from the study. Two members of our research team (SA and NSS) screened the articles independently based on the titles and abstracts. When there was any disagreement between them, the screeners discussed the full texts of the literature to reach an agreement. To ensure a comprehensive scope of coverage, single citation search of all retrieved publications was further done in PubMed and Google Scholar search engines. In addition, reference lists of the retrieved publications were manually searched for additional relevant publications that may have been missed in the computerized database search [Figure 1].
Figure 1.
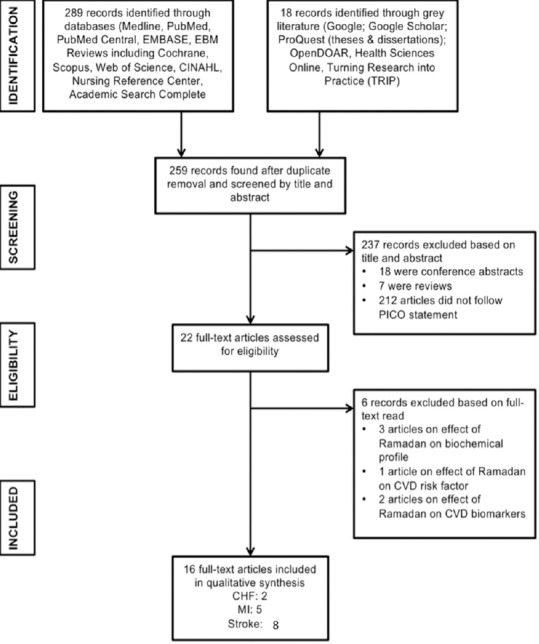
Search flow for “effect of Ramadan fasting on cardiovascular diseases”
Data abstraction
Full texts of the selected articles were read to extract information according to the PICO statement. The data for comparative incidences of CHF, MI, and stroke, and the rate of hospitalization for these diseases were extracted together with the information in the article (Author's name and publication year) and the demographic information of the studied population. The extracted information was presented in tables.
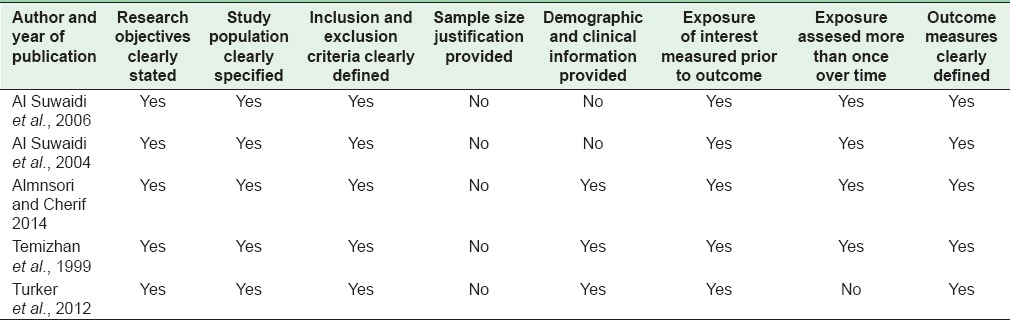
Quality assessment of selected literatures
Study quality assessment for systematic review is common practice that is well established for randomized control trials. However, quality assessment is much less established for observational studies with no standard methodology for acceptance.[7] Hence, in systematic reviews based on observational studies, researchers either ignore the quality assessment of studies or develop their own ways of appraisal.[8] In this study, the selected articles were appraised using a method previously adapted [9] from the “;Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies” from the NIH-national heart, lung and blood institute's guideline: Research objectives clearly stated, study population clearly specified, inclusion and exclusion criteria clearly defined, sample size justification provided, demographic and clinical information provided, exposure of interest measured prior to outcome, exposure assessed more than once over time, and outcome measures clearly defined.[10]
Meta-analysis of the studies on the impact of Ramadan fasting on the incidence of stroke
In this review, owing to the heterogeneous nature of the included articles regarding MI and CHF, we performed a meta-analysis only for the stroke-related publications and computed the odds ratio of ischemic or a hemorrhagic stroke in all stroke patients: (1) During Ramadan and 1 month before Ramadan; (2) during Ramadan and 1 month after Ramadan; and (3) Ramadan and other months of the year. We stratified the studies according to the hypothesis tested by the original authors. We analyzed studies separately based on the stroke sub-types; ischemic and hemorrhagic. To test the homogeneity across studies, we used the Cochrane's Q test.
RESULTS
Fifteen studies met the inclusion criteria for this study. Of these, eight focused on stroke, five on MI, and only two on CHF [Figure 1]. These studies, both prospective and retrospective, reported measures on incidence or patterns of acute cardiac illness, patients' demographical and clinical status with known cardiac illness and cardiovascular risk factors. The patient outcome measures were compared either in terms of time (during Ramadan, before and after Ramadan, or other months of the year) or between fasting and nonfasting condition of the patients.
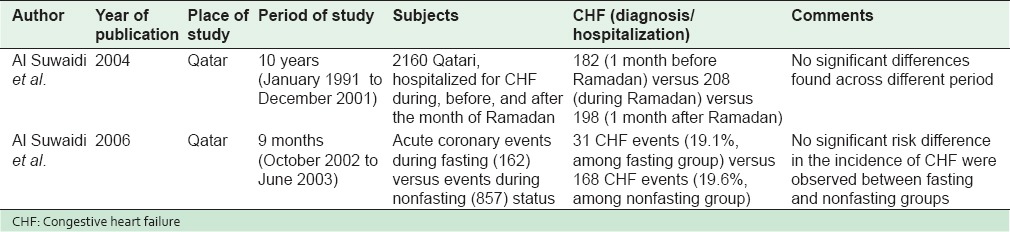
Impact of Ramadan fasting on congestive heart failure
Table 1 shows the two clinical studies, which reported the incidence of CHF and the clinical status of cardiac patients to look into the impact of Ramadan fasting. Al Suwaidi et al. collected information about the fasting status of 1019 consecutive acute coronary disease patients admitted to a general hospital in Qatar from October 2002 to June 2003. Ramadan started on the 5th of November and ended on the 4th of December.[11] Among the hospitalized cases, the authors did not find any significant difference in the occurrence of CHF between fasting and nonfasting status. In another study using retrospective review of clinical charts of 2160 hospitalized CHF patients, Al Suwaidi et al. reported that the number of hospitalizations for CHF was not statistically significantly different in Ramadan from a month before or after Ramadan (p > 0.37).[12] They also did not find any difference in CHF hospitalization between the Ramadan month and the remaining 9 months of the year.[12]
Table 1.
Congestive heart failure risk: During, before, and after the month of Ramadan/fasting status
Impact of Ramadan fasting on acute myocardial infarction
Table 2 shows the five studies, which reported the incidence of MI during Ramadan and other months, as well as the fasting status. Almansori and Cherif,[13] Turker et al.,[14] and Al Suwaidi et al.[11] studied the effect of the fasting status on the risk of MI hospitalization. Al Suwaidi et al. studying 1019 consecutive acute coronary disease patients admitted to a general hospital in the span of 9 months (including a Ramadan month) reported a higher relative risk for MI in the nonfasting group.[11] Compiling data from the charts of all patients with a diagnosis of acute myocardial infarction (AMI) who were admitted during the months of Ramadan of the year 2007–2012 to King Fahad University Hospital, Almansori, and Cherif reported a significant difference in favor of the fasting state with regard to the duration of hospital stay after AMI.[13] In their study of 151 consecutive Turkish patients with ST-elevation MI (STEMI) during the Ramadan months of 2010 and 2011, Turker et al. reported that higher proportions of the STEMI occurred during the nonfasting state.[14] Baseline hemodynamics (heart rate, systolic-diastolic blood pressure, etc.) and biomedical profiles (hemoglobin, creatinine, total cholesterol, etc.) were reported to be similar between fasting and nonfasting groups.[13,14] The use of medications such as aspirin, Beta-blockers, and angiotensin-converting enzyme inhibitors were also the same between the two groups.[13]
Table 2.
Acute myocardial infarction risk: During, before, and after the month of Ramadan/fasting status
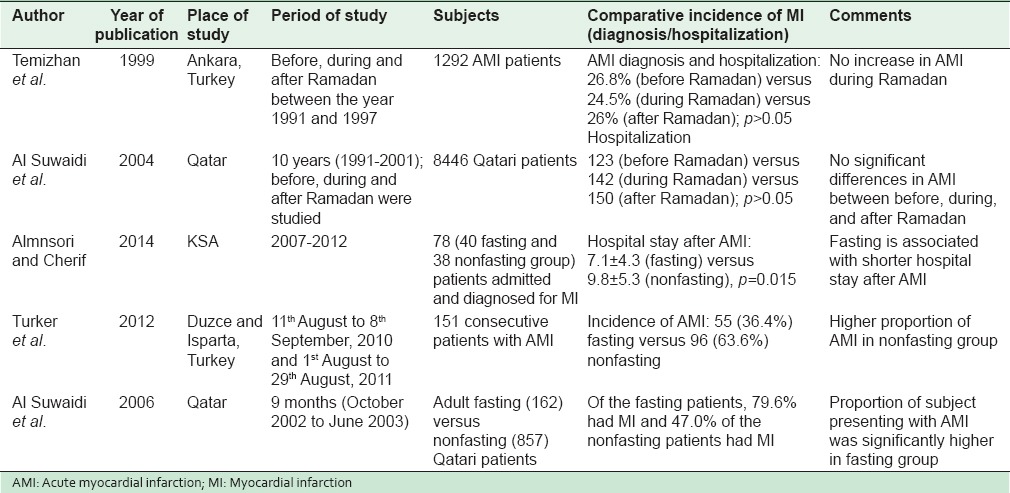
In their studies, Temizhan et al. and Al Suwaidi et al. reported that the incidence of MI was similar in the month of Ramadan to 1 month before or after Ramadan.[15,16] Temizhan et al. studied 1292 AMI patients hospitalized at their institution's emergency center in Ankara from 1991 and 1997.[16] The authors reported that there was no difference in the occurrence of AMI during the period of 1 month before Ramadan, during the Ramadan month, and 1 month after.[16] In Qatar, Al Suwaidi et al.[15] studied 8446 Qatari patients who were admitted to general hospital from 1991 to 2001 and estimated the incidence of AMI 1 month before, during, and 1 month after Ramadan. There was no difference in the incidence of AMI in these three periods.
Researchers also focused on evaluating the impact of Ramadan fasting on the circadian pattern of MI.[11,14] Al Suwaidi et al. reported that there were significant differences (p = 0.002) between the fasting and nonfasting groups with respect to the time when the symptoms of AMI began. The symptoms of fasting patients were less likely to start between 5 am and 8 am but more likely between 5 pm and 6 pm and between 3 am and 4 am, which correspond to the time of the meals for fasting patients.[11] In their study, Turker et al. reported that there were significant differences between fasting and nonfasting groups regarding circadian variation of STEMI (p< 0.001).[14] The highest incidence of STEMI among the fasting group was between 12 am and 6 pm, whereas the highest incidence of STEMI in the nonfasting group occurred between 6 am and 12 am.[14]
Impact of Ramadan fasting on stroke
Table 3 enumerates the 8 clinical studies, which reported the impact of Ramadan fasting period on the occurrence of stroke. In their study of 1579 stroke hospitalizations from 1991 to 1995, Akhan et al. found no significant difference in the incidence of stroke during Ramadan compared to other months of the year.[17] Similarly, another study from Turkey by Kutluhan et al. based on 815 stroke cases admitted to their hospital during a 5-year period reported that there was no significant difference in the frequency of strokes between the Ramadan month and other months.[18] In their study of 517 consecutive adult stroke patients admitted in a stroke unit in Egypt during 2007–2008, El-Mitwalli et al. reported that there was no difference between the stroke rates in the Ramadan fasting month and the month previous to Ramadan.[19] In a study that compared stroke hospitalizations across the month before Ramadan, Ramadan month, and the month after Ramadan, Comoglu et al. from Turkey reported no significant changes in ischemic as well as hemorrhagic strokes in those months.[20] Similar results were observed in a study in Qatar by Al Suwaidi et al.[15] in which there was no significant difference in the incidence of stroke 1 month before, during, and 1 month after Ramadan. Retrospectively reviewing a 13-year stroke database on 335 Muslim patients, Bener et al. reported that there was no difference in the incidence of stroke in the month before, during, and 1 month after Ramadan. The authors also estimated the incidence of stroke for the remaining 9 months of the year and found no difference in the occurrence of stroke in the Ramadan related months. To determine whether Ramadan fasting impacts the occurrence of cerebral venous sinus thrombosis (CVST), a rare type of stroke, Saadatnia et al. studied 162 CVST patients.[21] The authors reported a significantly increased frequency of CVST events in Ramadan compared to other months.
Table 3.
Stroke risk: During, before, and after the month of Ramadan/fasting status
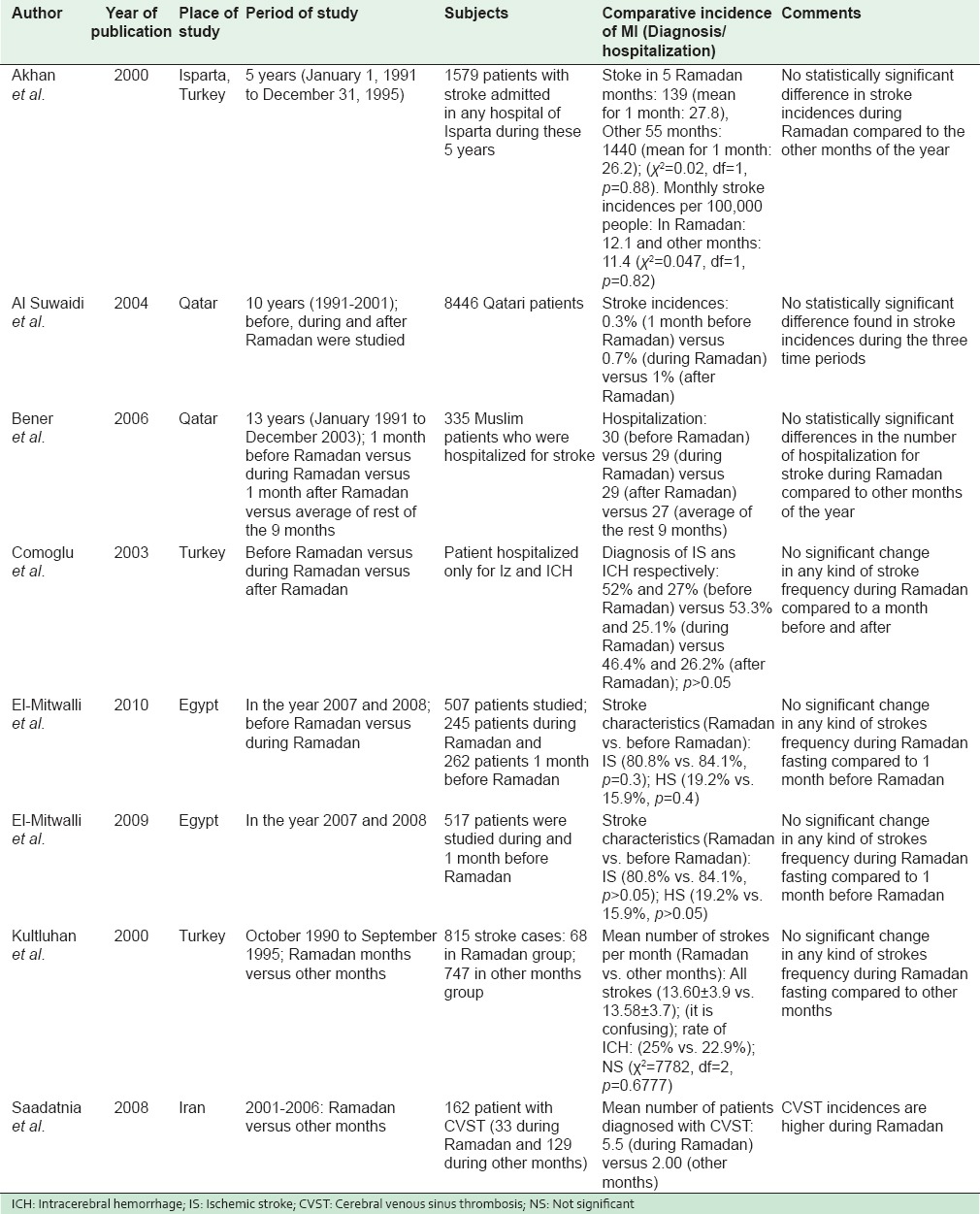
Studies have also shown that the ratios of hemorrhagic and ischemic stroke were not significantly different between Ramadan and other nonfasting months.[17,19,20,22] Some interesting observations were presented in different studies. For instance, rate of cerebral infarct is slightly lower (70.6%) during Ramadan than other nonfasting months (74.3%) whereas rate of intracerebral hemorrhage (ICH) was 25% in Ramadan compared to 22.9% in other months.[18] However, no significant relationship was found between the duration of fasting and the frequency and type of stroke that occurred during Ramadan. Among patients with cardiovascular risk factors,[20] in particular among diabetic patients, the ratio of ischemic stroke in Ramadan was significantly higher than before and after Ramadan, whereas in hypertensive patients, the ratio of ICH was lower in Ramadan than before and after Ramadan.[20]
For a number of the studies, the primary focus was to evaluate the impact of Ramadan fasting on the circadian pattern of stroke. Irrespective of the types, the frequency of onset of all strokes in both (Ramadan and other months) groups was significantly higher in the morning than in the other periods of time.[17,22] All strokes occurred less frequently in the afternoon in the first group and at night in the second group.[17,22]
The Figures 2 and 3 are the forest plots from the meta-analysis for different stroke types during Ramadan and other nonfasting months. The p- value for the Cochrane's Q test is > 0.05, indicating the studies are homogeneous and a meta-analysis can be performed. Consistent with the individual papers, our pooled odds ratios showed no significant difference on the onset of stroke during Ramadan and other nonfasting months across stroke subtype. Table 4–6 shows the quality assessment results of the studies on CHF, AMI, and stroke.
Figure 2.
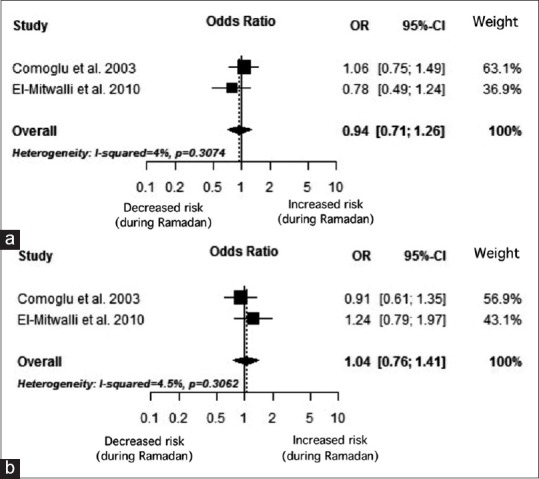
(a) Forest plot of ischemic stroke risk among stroke patients: during versus the month before Ramadan month. (b) Forest plot of hemorrhagic stroke risk among stroke patients: During versus the month before Ramadan month
Figure 3.
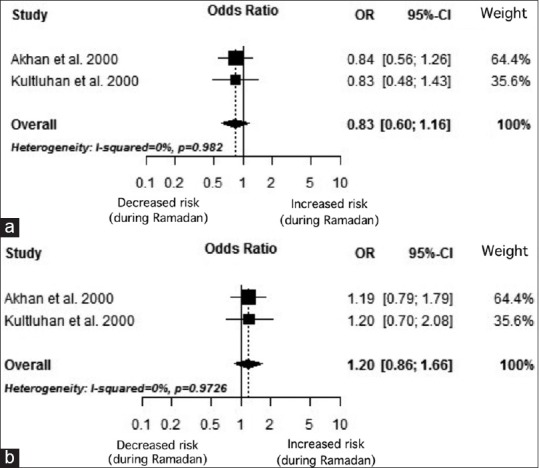
(a) Forest plot of ischemic stroke risk among stroke patients: during Ramadan month versus the other months of the year. (b) Forest plot of hemorrhagic stroke risk among stroke patients: during Ramadan month versus the other months of the year
Table 4.
Quality assessment of articles selected for congestive heart failure
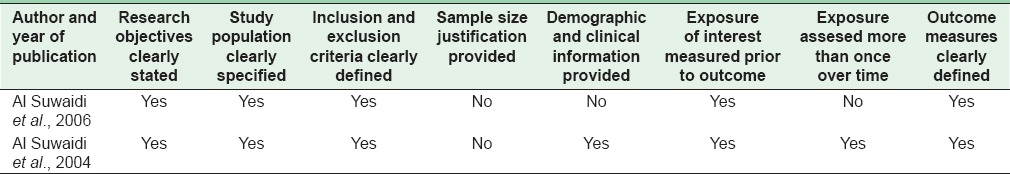
Table 6.
Quality assessment of articles selected for stroke
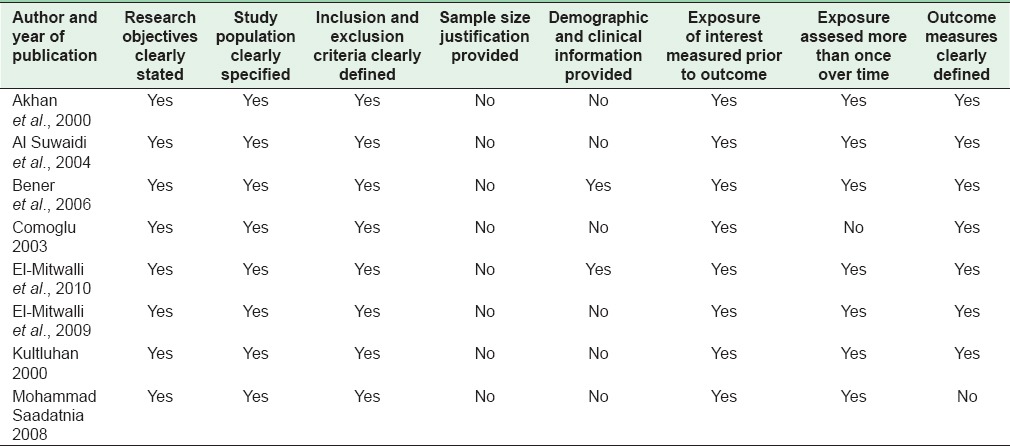
Table 5.
Quality assessment of articles selected for acute myocardial infarction
DISCUSSION
There are approximately 1.6 billion Muslims living in all countries of the world.[23] Although the importance of religion to Muslims across the world varies significantly, fasting in the month of Ramadan remains very high for most Muslims. In a multi-national study of 39 countries and over 38,000 personal interviews (in 80 different languages), it was shown that of the Muslims in Southeast Asia, South Asia, the Middle East and North Africa, and sub-Saharan Africa, medians of between 94% and 99% stated they fasted in the month of Ramadan.[24] Muslims, all over the world, are religiously obliged to fast from dawn to dusk during the month of Ramadan. This significantly alters their dietary habits for one whole month. In addition to dietary intake, other habits such as smoking, physical exercise, and sleeping patterns are also altered extensively during Ramadan. While at first glance, these changes in lifestyle may appear quite intimidating, occurrences of cardiovascular diseases have shown very few signs of escalation during the month of Ramadan. When compared to other times of the year, no significant difference has been revealed in the incidences of diagnosis and/or hospitalization due to critical cardiac conditions such as CHF, MI, and ischemic or hemorrhagic stroke during Ramadan. The only exception is the occurrence of CVST, a rare type of stroke among young adults and children, which significantly increased during the month of Ramadan. As this is not a common type of stroke, the effect of fasting on its occurrence needs to be further investigated.
Although overall stroke occurrence among patients did not change during Ramadan, the occurrence of ICH strokes in hypertensive patients was lower though diabetic patients exhibited a higher frequency of CI stroke during Ramadan.[20] Hunger is known to positively affect the health of the heart. When hungry, sympathetic tone is supressed leading to a fall in blood pressure, heart rate, and cardiac output.[25,26] Given the prolonged period of starvation during Ramadan, these protective effect on hypertensive patients could have led to reduced frequency of ICH.[20] In the case of diabetic patients, the fear of becoming hypoglycemic during Ramadan, makes them increase their carbohydrate intake [27] and reduce medication.[20] This together with reduced physical activity increases the chances of hyperglycemia,[28,29] which by aggravating lactic acidosis [30] contributes to brain injury. Increased CI stroke in diabetic patients [20] may be related to hyperglycemia during Ramadan.[20]
When compared with a nonfasting group, incidences of CHF did not show any added manifestation among the fasting adults. When the rate of MI was compared, Turker et al. reported less frequency of AMI in the fasting groups in Turkey.[14] Moreover, fasting patients in Saudi Arabia needed shorter hospital stays after AMI than nonfasting ones.[13] Suppression of sympathetic tone by starvation may contribute to this cardiac benefit.[25] Furthermore, though not clinically proven, a restriction on smoking during Ramadan may have additional advantageous effect on cardiac patients.[27] However, despite the beneficial effects of fasting in Ramadan, Al Suwaidi (2006) found higher rates of AMI in the fasting group than in nonfasting group. As this finding contradicts other findings stated above, the underlying cause requires further investigation.
A few of the selected studies investigated the effect of Ramadan fasting on the timing of acute cardiac onset. It was observed that stroke [22] or MI [14] occurred more frequently between noon and 6 pm during the Ramadan months in contrast to the period of 6am and noon during nonfasting months.[14,22] The abnormal pattern of food intake and sleep during Ramadan is most likely to contribute to some extent to this shift in circadian pattern in cardiac outcomes.[11]
It needs to be kept in mind that the studies found in the systematic search were conducted in different geographical locations with varying climates and daylight hours. Hence, the conditions under which Ramadan fast was observed were not the same in all the studies. Moreover, heterogeneity in defining and reporting outcomes make evaluation in the different studies difficult. In addition, a limited number of studies in the different subgroups of cardiac patients restricts our ability to draw firm conclusions.
Aside from the contribution to existing literature on this topic, the importance of understanding the effects of Ramadan on health are necessary for multiple reasons. First, health practitioners working with Muslim clients who observe the fast in Ramadan would be better equipped to assess changes in health that could be the result of fasting. Since a major lifestyle change is common during this month for many Muslims, practitioners can also recommend to their clients what behaviors to maintain or reduce as the fasting month ends. In addition to assessment and recommendations, practitioners should be aware of Ramadan and the fasting rituals of their clients in order to properly educate them on factors that can cause complications (i.e. changing their medication schedules, the use of other medications, change in eating habits, sleep deprivation, etc.). An understanding of the various behaviors that promote or hinder health factors of people who fast (e.g. Muslims in Ramadan and people of other faiths during their respective time periods) can be used by practitioners and other health educators to improve public education. Another area that needs more exploration is the use of fasting as therapy for certain conditions. At the societal level, policy makers on health can also utilize such information to increase awareness, develop policies that promote health in Muslim majority countries where Ramadan is practiced throughout the nation.
Although we did a comprehensive literature search, research in this particular field was scarce. Thus, we did not have enough studies for synthesis or definitive summary measure from meta-analysis. Moreover, although Muslims are present in different geographic areas, there were no studies of the different regions. We recommend multinational prospective studies with sound methodology involving Muslim populations from different regions of the world in order to examine the association between fasting during the holy month of Ramadan and cardiovascular disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Yusuf Ali Abdullah., translator. The Qur’an. Ch. 2, Ver. 183. New York: Tahrike Tarsile Qur’an Inc.; 2003. [Google Scholar]
- 2.Sakr AH. Fasting in Islam. J Am Diet Assoc. 1975;67:17–21. [PubMed] [Google Scholar]
- 3.Al-Bukhari S. In: Book 30, Hadith 27. Khan MM, translator. Riyad: Darussalam; 1996. [Google Scholar]
- 4.Al-Bukhari S. In: Book 30, Hadith 32. Khan MM, translator. Riyad: Darussalam; 1996. [Google Scholar]
- 5.Ali AY, translator. The Qur’an. Ch. 2, Ver. 185. New York: Tahrike Tarsile Qur’an Inc.; 2003. [Google Scholar]
- 6.Yegi INM, Yegi INA, Agibase A, Bakan E. Starvation and diet. J Ankara Univ Med Sch. 1981;13:57–62. [Google Scholar]
- 7.Mallen C, Peat G, Croft P. Quality assessment of observational studies is not commonplace in systematic reviews. J Clin Epidemiol. 2006;59:765–9. doi: 10.1016/j.jclinepi.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 8.Egger M, Smith GD, Altman DG. Index. In: Egger M, Smith G, Altman DG, editors. Systematic Reviews in Health Care. London, United Kingdom: BMJ Publishing Group; 2008. pp. 475–87. [Google Scholar]
- 9.Tonelli M, Wiebe N, Culleton B, House A, Rabbat C, Fok M, et al. Chronic kidney disease and mortality risk: A systematic review. J Am Soc Nephrol. 2006;17:2034–47. doi: 10.1681/ASN.2005101085. [DOI] [PubMed] [Google Scholar]
- 10.Quality Assessment Tool for Observational Cohort and Cross-sectional Studies: National Heart, Lung and Blood Institute. 2014. [Last updated on 2014 Mar 26; Last cited on 2015 May 03]. Available from: http://www.nhlbi.nih.gov/health.pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort .
- 11.Al Suwaidi J, Bener A, Gehani AA, Behair S, Al Mohanadi D, Salam A, et al. Does the circadian pattern for acute cardiac events presentation vary with fasting? J Postgrad Med. 2006;52:30–3. [PubMed] [Google Scholar]
- 12.Al Suwaidi J, Bener A, Hajar HA, Numan MT. Does hospitalization for congestive heart failure occur more frequently in Ramadan: A population-based study (1991-2001) Int J Cardiol. 2004;96:217–21. doi: 10.1016/j.ijcard.2003.06.018. [DOI] [PubMed] [Google Scholar]
- 13.Almansori M, Cherif E. Impact of fasting on the presentation and outcome of myocardial infarction during the month of Ramadan. Italian J Med. 2013;8:4. [Google Scholar]
- 14.Turker Y, Aydin M, Aslantas Y, Ozaydin M, Ali UB, Bulur S, et al. The effect of Ramadan fasting on circadian variation of Turkish patients with acute myocardial infarction. Posteẹpy Kardiol Interwencyjnej. 2012;8:193–8. [Google Scholar]
- 15.Al Suwaidi J, Bener A, Suliman A, Hajar R, Salam AM, Numan MT, et al. Apopulation based study of Ramadan fasting and acute coronary syndromes. Heart. 2004;90:695–6. doi: 10.1136/hrt.2003.012526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Temizhan A, Dönderici O, Ouz D, Demirbas B. Is there any effect of Ramadan fasting on acute coronary heart disease events? Int J Cardiol. 1999;70:149–53. doi: 10.1016/s0167-5273(99)00082-0. [DOI] [PubMed] [Google Scholar]
- 17.Akhan G, Kutluhan S, Koyuncuoglu HR. Is there any change of stroke incidence during Ramadan? Acta Neurol Scand. 2000;101:259–61. doi: 10.1034/j.1600-0404.2000.101004259.x. [DOI] [PubMed] [Google Scholar]
- 18.Kutluhan S, Galip A, Koyuncuoglu HR, Gultekin F, Kumral E. Diurnal variation of stroke in Ramadan. Biomed Res. 2000;11:303–7. [Google Scholar]
- 19.el-Mitwalli A, Zaher AA, Mohamed MA, Elmenshawi E. The effect of Ramadan fasting on cerebral stroke: A prospective hospital-based study. Eur J Neurol. 2009;16:e80. doi: 10.1111/j.1468-1331.2009.02566.x. [DOI] [PubMed] [Google Scholar]
- 20.Comoglu S, Temizhan A, Pesinci E, Tandogan I, Ozbakir S. Effects of Ramadan fasting on stroke. Turk J Med Sci. 2003;33:237–41. [Google Scholar]
- 21.Saadatnia M, Zare M, Fatehi F, Ahmadi A. The effect of fasting on cerebral venous and dural sinus thrombosis. Neurol Res. 2009;31:794–8. doi: 10.1179/016164109X12445505689481. [DOI] [PubMed] [Google Scholar]
- 22.El-Mitwalli A, Zaher AA, El Menshawi E. Circadian rhythm of stroke onset during the month of Ramadan. Acta Neurol Scand. 2010;122:97–101. doi: 10.1111/j.1600-0404.2009.01265.x. [DOI] [PubMed] [Google Scholar]
- 23.The Future of the Global Muslim Population Projections for 2010-2030. Pew Research 2011. [Last retrieved on 2015 May 07]. Available from: http://www.pewforum.org/uploadedFiles/Topics/Religious_Affiliation/Muslim/FutureGlobalMuslimPopulation-WebPDF-Feb10.pdf .
- 24.The World's Muslims: Unity and Diversity. Pew Research. 2012. [Last retrieved on 2015 May 07]. Available from http://www.pewforum.org/files/2012/08/the-worlds-muslims-full-report.pdf .
- 25.Stokholm KH, Breum L, Astrup A. Cardiac contractility, central haemodynamics and blood pressure regulation during semistarvation. Clin Physiol (Oxford, England) 1991;11:513–23. doi: 10.1111/j.1475-097x.1991.tb00671.x. [DOI] [PubMed] [Google Scholar]
- 26.Landsberg L, Young JB. Fasting, feeding and regulation of the sympathetic nervous system. N Engl J Med. 1978;298:1295–301. doi: 10.1056/NEJM197806082982306. [DOI] [PubMed] [Google Scholar]
- 27.Salim I, Al Suwaidi J, Ghadban W, Alkilani H, Salam AM. Impact of religious Ramadan fasting on cardiovascular disease: A systematic review of the literature. Curr Med Res Opin. 2013;29:343–54. doi: 10.1185/03007995.2013.774270. [DOI] [PubMed] [Google Scholar]
- 28.Laajam MA. Ramadan fasting and non-insulin-dependent diabetes: Effect on metabolic control. East Afr Med J. 1990;67:732–6. [PubMed] [Google Scholar]
- 29.Al-Fayez SK, Khogheer YA, Sulaiman MI. Plasma glucose changes in diabetes during Ramadan fasting. J Islam Med Assoc. 1988;20:47–9. [Google Scholar]
- 30.Yip PK, He YY, Hsu CY, Garg N, Marangos P, Hogan EL. Effect of plasma glucose on infarct size in focal cerebral ischemia-reperfusion. Neurology. 1991;41:899–905. doi: 10.1212/wnl.41.6.899. [DOI] [PubMed] [Google Scholar]


