Sir:
In autologous breast reconstruction after mastectomy, fat induration is a rather common complication that causes deep tissue infection, pain, and contracture deformity. Follow-up for fat induration provides important clues after breast reconstruction with an autologous flap because fat induration is the clinical stage before fat necrosis that may lead to the need for corrective surgery. Our understanding of fat necrosis until now has been limited because previous studies were based exclusively on physical examination and used diverse definitions.1
Ultrasound elastography (UE) is a relatively novel technique that is being evaluated for use to measure tissue stiffness. We have previously reported that UE is useful for detection of fat induration and necrosis after breast reconstruction with an autologous flap.2 There are presently 2 UE techniques available that are very different in terms of the forces being measured and in their display methods (Fig. 1). In strain elastography (STE), stress is applied by repeated manual compression of the transducer, and the amount of lesion deformation relative to the surrounding normal tissue is measured and displayed in color. In contrast to strain elastography, shear-wave elastography (SWE) uses an acoustic radiation force impulse, which allows measurement of the propagation speed of shear waves within the tissue to locally quantify its stiffness in either kilopascals or meters per second.3,4 Previous studies have demonstrated that both STE and SWE can help characterize breast lesions as either benign or malignant on the basis of stiffness. However, to our knowledge, there have been no studies comparing the diagnostic performances of the 2 different techniques in the same region of fat induration. It is not known which one is better, STE or SWE, for follow-up for fat induration after breast reconstruction with an autologous flap.
Fig. 1.
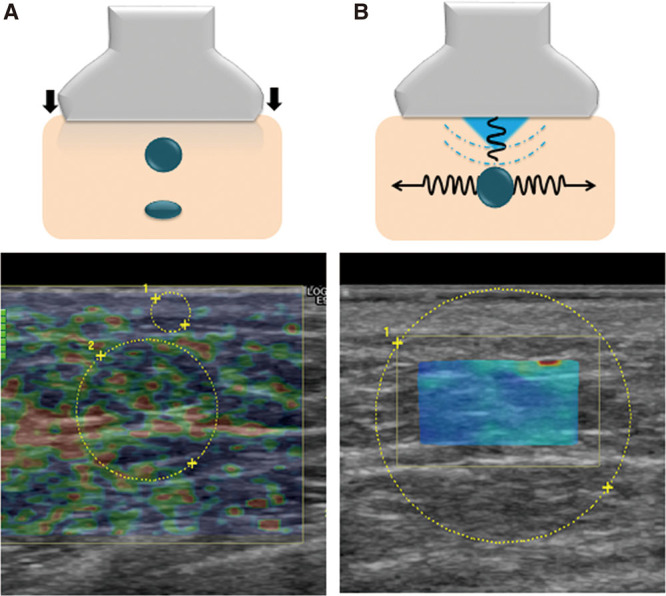
Schematic representation of 2 types of ultrasound elastography. A, Strain elastography. Stress is applied by repeated manual compression of the transducer, and the amount of lesion deformation relative to the surrounding normal tissue is measured in a 2-dimensional (2D) region under the transducer. The relative tissue stiffness of interest lesion in color is displayed as the strain ratio. B, Shear-wave elastography. High intensity focused ultrasound beams can be used to push on tissue to generate shear waves, which propagate laterally away from the region of excitation, which allows the user to visualize the tissue stiffness as a color-coded map in a 2D region of interest.
Fourteen patients, who had clinical fat induration after breast reconstruction with a deep inferior epigastric perforator flap, were included in this study. Fat tissue stiffness in the palpable hard area was measured with each technique, and the data obtained by the same device operator were recorded on the same day on the same subjects. Intraclass correlation coefficients for repeatability assessment and correlation coefficients were used to evaluate the agreement between the 2 devices.
As a result of our investigation, the intraclass correlation coefficients were 0.86 (95% confidence interval: 0.70–0.95) for strain elastography and 0.96 (90% confidence interval: 0.90–0.99) for shear-wave elastography. The correlation coefficients comparing fat tissue stiffness measured with the 2 devices were low (r = 0.6028), ranging from 0.1061 to 0.8588. Significant differences were found between the 2 methods for repeatability.
When the shear-wave and strain elastography techniques are used on the same reconstructed breast lesions, consistent or similar results are to be expected if the examination is performed by the same device operators. However, we actually found better repeatability of tissue stiffness measurements with SWE than that with STE. The strain ratio was calculated by dividing the mean strain of the reference normal tissue by the mean strain within the region of interest. However, there was no consistency in selecting the reference normal tissue. Unlike strain elastography, SWE can quantify tissue stiffness on an absolute scale and has been previously reported to be highly reproducible and repeatable for assessing tissue stiffness of breast lesions within and across observers.5 Our results suggest that SWE may be more useful in facilitating postoperative follow-up for either induration or fat necrosis of breast reconstruction with autologous tissue. In the future, we will investigate the optimal cut-off values for either significant fat induration or necrosis after autologous breast reconstruction using SWE to define the diagnostic criteria and provide further reliability.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Rao A, Saadeh PB. Defining fat necrosis in plastic surgery. Plast Reconstr Surg. 2014;134:1202–1212. doi: 10.1097/PRS.0000000000000700. [DOI] [PubMed] [Google Scholar]
- 2.Sowa Y, Numajiri T, Nishino K. Ultrasound shear-wave elastography for follow-up fat induration after breast reconstruction with an autologous flap. Plast Reconstr Surg Glob Open. 2015;3:e518. doi: 10.1097/GOX.0000000000000493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Youk JH, Son EJ, Gweon HM, et al. Comparison of strain and shear wave elastography for the differentiation of benign from malignant breast lesions, combined with B-mode ultrasonography: qualitative and quantitative assessments. Ultrasound Med Biol. 2014;40:2336–2344. doi: 10.1016/j.ultrasmedbio.2014.05.020. [DOI] [PubMed] [Google Scholar]
- 4.Barr RG, Zhang Z. Shear-wave elastography of the breast: value of a quality measure and comparison with strain elastography. Radiology. 2015;275:45–53. doi: 10.1148/radiol.14132404. [DOI] [PubMed] [Google Scholar]
- 5.Cosgrove DO, Berg WA, Doré CJ, et al. BE1 Study Group BE1 Study Group. Shear wave elastography for breast masses is highly reproducible. Eur Radiol. 2012;22:1023–1032. doi: 10.1007/s00330-011-2340-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


