Abstract
Background
New avenues of data collection such as eHealth and mobile technology have the potential to revolutionize the way large populations can be assessed and managed outside of standard research and clinical settings.
Methods and Results
A digital connectedness survey was administered within the Framingham Heart Study from 2014 to 2015. The exposure was usage of the Internet, email, cell phones, and smartphones in relation to demographic and cardiovascular disease risk factors; all results were adjusted for age and sex. Among 8096 living study participants, 6503 (80.3%) completed the digital survey. Among survey responders, 5678 (87.4%) reported regular Internet use. Participants reporting regular Internet use were younger (aged 59.1 versus 76.5 years, P<0.0001), were more likely to be employed (70.3% versus 23.7%, P=0.002), and had more favorable cardiovascular disease risk factors than those who did not use the Internet (all P≤0.05). Overall, 5946 (92.1%) responders reported using cell phones. Among cell phone users, 3907 (67.8%) had smartphones. Smartphone users were younger (aged 55.4 versus 68.5 years, P<0.0001), more likely to be employed (81.1% versus 43.9%, P<0.0001) and to have a college education, and less likely to have hypertension (27.9% versus 55.7%, P=0.0002) than those who did not use smartphones.
Conclusions
Digital connectedness varies substantially by age; connected persons tend to be younger and better educated and to have more favorable cardiovascular disease risk factor profiles. Less than two‐thirds of study participants who completed the survey had a smartphone. The generalizability of studies focused on digitally connected persons may have limitations.
Keywords: cardiovascular risk, eHealth, epidemiology, mHealth, smartphones, technology
Subject Categories: Lifestyle, Risk Factors, Primary Prevention
Introduction
Traditional cohort epidemiology has been the mainstay of population‐based science for several decades; however, classical cohort epidemiology is costly and time consuming1, 2, 3 and has been criticized for incremental findings, lack of validation, and lack of flexibility.4 New models of scalable population‐based data collection are necessary.5 The digital health revolution may have the potential to transform health care by offering larger scale phenotyping performed outside of standard research clinic settings.6, 7, 8, 9 New avenues for collecting population‐level data, such as eHealth and mobile (mHealth) technology, are potentially exciting and may improve clinicians’ and researchers’ abilities to assess risk factors and health behaviors in vivo (ie, data are collected in participants’ true environments).10 Use of these new modalities requires access to technology including the Internet, email, cell phones, and smartphones. The overall penetrance of digital technology within an existing cohort study and associations with cardiovascular disease (CVD) risk burden remain largely unknown.
The purpose of our study was to assess the digital connectedness, which we defined as usage of digital technologies, of Framingham Heart Study (FHS) participants, using a recently administered digital connectedness survey. In addition to overall connectivity, we examined the CVD risk factor profiles associated with technology usage. We hypothesized that those who used digital technologies would be younger and would have less adverse CVD risk factor profiles than their counterparts who did not use such technologies.
Methods
Study Sample
In 1948, 5209 women and men aged 28 to 62 years enrolled in the FHS Original cohort. Because <100 participants from the Original cohort are living, that cohort was not included in the present report. The offspring and spouses of the offspring of the Original cohort were enrolled in the Offspring study.11, 12 In 2002, 4095 Third Generation participants with at least 1 parent in the Offspring cohort were enrolled. From 1994 to 1998, Omni Group 1 (n=506) was recruited to reflect the contemporary diversity of the town of Framingham, Massachusetts. From 2002 to 2005, the Omni Group 2 cohort (n=410) was recruited to parallel recruitment of the Third Generation cohort. The standard research clinical examination typically included physician‐administered medical history interviews, physical examinations, and laboratory tests. The study was approved by the institutional review board of Boston University Medical Center, and participants provided written informed consent.
Digital Connectedness Survey
We created a digital connectedness survey to administer to all living FHS participants without significant cognitive impairment (n=8096). The full survey appears in Data S1. Briefly, we asked participants about their usage of the Internet, email, cell phones, smartphones, social networks, computer games, and health applications (“apps”). The survey was estimated to take about 3 minutes to complete. The survey was first administered in REDCap (http://project-redcap.org) to all participants with a unique email address on file. The link was re‐sent twice, weekly, and if the participant still did not respond, a telephone call was placed. Up to 3 attempts were made to reach the participant by telephone. During the telephone call, the participant was given the opportunity to complete the survey over the telephone, to receive the REDCap link again, or to complete the survey using a mailed paper version. For participants who did not have an email address on file or who shared email accounts (n=2922), attempts were made to call participants to retrieve their email addresses. Finally, paper surveys were mailed to all participants who did not complete the survey either by REDCap or by telephone. Overall, 2649 Offspring, 3321 Third Generation, and 533 Omni participants completed the survey. The survey was administered between study examinations. Compared with survey responders, survey nonresponders (n=1593) were younger (aged 57.4 versus 61.3 years), were less likely to have attended a recent examination (54.8% versus 85.3%), had a higher body mass index (in kg/m2; 28.6 versus 28.2), were more likely to smoke cigarettes (13.1% versus 8.7%), were less likely to have completed college (38.3% versus 49.5%), and had higher rates of hypertension (42.6% versus 39.8%) and diabetes (20.4% versus 16.7%; all P<0.02).
Cardiovascular Risk Assessment
CVD risk factors were measured at the most recently attended examination. Overall, 81% of participants attended Offspring examination 9 (2011–2014), and 88% of participants attended the second examination of the Third Generation (2008–2011). Body mass index was defined as weight (in kilograms) indexed to height squared (in meters). Plasma glucose and total cholesterol were measured in fasting samples. Hyperlipidemia was defined as total cholesterol ≥200 mg/dL or lipid treatment. Diabetes was defined as fasting glucose ≥126 mg/dL or treatment with a hypoglycemic agent or insulin. Participants were classified as current smokers if they smoked at least 1 cigarette per day in the prior year. Hypertension was defined as systolic blood pressure ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg or being on treatment. CVD events were adjudicated by 3 investigators and included myocardial infarction, coronary insufficiency, atherothrombotic infarct, transient ischemic attack, intermittent claudication, and congestive heart failure. Atrial fibrillation was confirmed, as described previously.13
Statistical Analysis
Data were tabulated by frequency across different survey components. CVD risk factor profiles were examined by survey response (yes versus no). Chi‐square P values for dichotomous CVD risk factors or F test P values for continuous risk factors were calculated using logistic or general linear models that were adjusted for age and sex. All statistics were performed using SAS v9.3 (SAS Institute). A 2‐sided P<0.05 was considered statistically significant.
Results
Among 8096 living FHS participants, 6503 (80.3%) completed the survey: Overall, 3902 completed the survey by REDCap (60.0%), 883 completed the survey by mail (13.5%), and 1718 completed it by telephone (26.5%). Participants who completed the survey by telephone were older (69.1 years) on average compared with those who completed the survey by REDCap (58.2 years) or by mail (59.4 years, P<0.0001).
Among survey responders, 5678 (87.4%) reported Internet usage, 5121 (91.1%) reported home Wi‐Fi, 5509 (85.0%) reported regular email use, 5946 (92.1%) reported using a cell phone, and 3907 (67.8%) of cell phone users reported having a smartphone. When queried regarding the use of apps and social networks, 1426 (24.4%) reported using health apps, 2746 (42.4%) reported using computer games, and 3163 (48.8%) reported using social networks. Social network users predominantly accessed Facebook (n=2944), LinkedIn (n=1244), Google+ (n=347), and Twitter (n=478).
Participants reporting Internet usage were younger (aged 59.1 versus 76.5 years), were more likely to be employed, and had more favorable CVD risk factors compared with those who did not use the Internet (Table 1). Tables 2, 3 through 4 stratify the sample by FHS cohort (Offspring, Third Generation, Omni). The figure presents CVD risk factor data by Internet use and cell phone status (Figure).
Table 1.
Study Sample Characteristics Among Framingham Heart Study Participants by Internet, Cell Phone, or Smartphone Usage
| Internet (n=5678) | No Internet (n=806) | P Value | Cell Phone (n=5946) | No Cell Phone (n=517) | P Value | Smartphone (n=3907) | No Smartphone (n=1857) | P Valuea | |
|---|---|---|---|---|---|---|---|---|---|
| Age, y | 59.1 (13.0) | 76.5 (10.2) | <0.0001 | 60.0 (13.4) | 75.5 (11.0) | <0.0001 | 55.4 (11.8) | 68.5 (11.9) | <0.0001 |
| Age groups, y | <0.0001 | <0.0001 | <0.0001 | ||||||
| 25 to 34 | 178 (3.1) | — | 178 (3.0) | — | 165 (4.2) | 13 (0.7) | |||
| 35 to 44 | 663 (11.7) | 2 (0.3) | 659 (11.1) | 3 (0.6) | 615 (15.7) | 43 (2.3) | |||
| 45 to 54 | 1378 (24.3) | 31 (3.9) | 1383 (23.3) | 22 (4.3) | 1153 (29.5) | 214 (11.5) | |||
| 55 to 64 | 1495 (26.3) | 80 (9.9) | 1515 (25.5) | 60 (11.6) | 1105 (28.3) | 378 (20.4) | |||
| 65 to 74 | 1321 (23.3) | 199 (24.7) | 1362 (22.9) | 151 (29.2) | 676 (17.3) | 626 (33.7) | |||
| 75 to 84 | 537 (9.5) | 318 (39.5) | 687 (11.6) | 165 (31.9) | 179 (4.6) | 449 (24.2) | |||
| ≥85 | 106 (1.9) | 176 (21.8) | 162 (2.7) | 116 (22.4) | 14 (0.36) | 134 (7.2) | |||
| Women (%) | 3166 (55.8) | 464 (57.6) | 0.44 | 3319 (55.8) | 293 (56.7) | 0.78 | 2156 (55.2) | 1060 (57.1) | 0.12 |
| Race/ethnicity | 0.09 | 0.99 | 0.02 | ||||||
| White | 5168 (91.1) | 730 (90.6) | 5401 (90.9) | 479 (92.7) | 3505 (89.8) | 1734 (93.4) | |||
| Black | 142 (2.5) | 19 (2.4) | 148 (2.5) | 12 (2.3) | 105 (2.7) | 35 (1.9) | |||
| Hispanic | 142 (2.5) | 45 (5.6) | 170 (2.9) | 17 (3.3) | 123 (3.2) | 39 (2.1) | |||
| Asian | 128 (2.3) | 8 (1.0) | 132 (2.2) | 4 (0.8) | 96 (2.5) | 33 (1.8) | |||
| Other | 95 (1.7) | 4 (0.5) | 92 (1.6) | 5 (1.0) | 75 (1.9) | 16 (0.9) | |||
| BMI, kg/m2 | 28.1 (5.6) | 28.6 (5.6) | 0.88 | 28.1 (5.6) | 28.8 (6.1) | 0.64 | 27.9 (5.5) | 28.5 (5.7) | 0.59 |
| Smoking (%) | 404 (8.2) | 80 (13.0) | <0.0001 | 442 (8.7) | 41 (10.0) | 0.004 | 281 (8.3) | 147 (9.4) | <0.0001 |
| Currently employed (%) | 3320 (70.3) | 132 (23.7) | 0.002 | 3351 (68.5) | 99 (26.7) | 0.0005 | 2630 (81.1) | 657 (43.9) | <0.0001 |
| Education | <0.0001 | <0.0001 | <0.0001 | ||||||
| Less than high school (%) | 31 (0.6) | 54 (7.9) | 57 (1.1) | 28 (6.3) | 16 (0.45) | 36 (2.2) | |||
| High school (%) | 779 (15.2) | 318 (46.7) | 939 (17.6) | 153 (34.4) | 399 (11.3) | 492 (29.8) | |||
| Some college (%) | 1552 (30.3) | 202 (29.7) | 1606 (30.0) | 137 (30.8) | 1031 (29.1) | 522 (31.6) | |||
| College and higher (%) | 2767 (54.0) | 107 (15.7) | 2746 (51.4) | 127 (28.5) | 2093 (59.1) | 601 (36.4) | |||
| Hypertension (%) | 1746 (35.5) | 451 (73.2) | 0.0009 | 1907 (37.4) | 276 (67.3) | 0.35 | 946 (27.9) | 869 (55.7) | 0.0002 |
| Hyperlipidemia (%) | 2743 (55.9) | 442 (72.9) | 0.002 | 2884 (56.7) | 289 (71.2) | 0.01 | 1726 (51.0) | 1044 (67.3) | 0.15 |
| Diabetes (%) | 726 (15.0) | 181 (30.6) | 0.05 | 784 (15.6) | 121 (30.7) | 0.07 | 421 (12.6) | 326 (21.3) | 0.61 |
| CVD (%) | 443 (7.8) | 213 (26.4) | 0.0002 | 531 (8.9) | 122 (23.6) | 0.26 | 215 (5.5) | 277 (14.9) | 0.16 |
| Atrial fibrillation (%) | 249 (4.4) | 101 (12.6) | 0.79 | 282 (4.8) | 66 (12.8) | 0.79 | 104 (2.7) | 157 (8.5) | 0.07 |
BMI indicates body mass index; CVD, cardiovascular disease.
P value is adjusted for age and sex.
Table 2.
Study Sample Characteristics Among Framingham Heart Study Offspring Participants by Internet, Cell Phone, or Smartphone Usage
| Internet (n=1947) | No Internet (n=620) | P Value | Cell Phone (n=2164) | No Cell Phone (n=392) | P Value | Smartphone (n=909) | No Smartphone (n=1128) | P Valuea | |
|---|---|---|---|---|---|---|---|---|---|
| Age, y | 71.5 (7.7) | 79.6 (7.8) | <0.0001 | 72.4 (8.0) | 78.9 (8.3) | <0.0001 | 69.1 (7.0) | 74.7 (7.9) | <0.0001 |
| Age groups, y | <0.0001 | <0.0001 | <0.0001 | ||||||
| 45 to 54 | 24 (1.2) | 4 (0.6) | 25 (1.2) | 3 (0.8) | 18 (2.0) | 7 (0.6) | |||
| 55 to 64 | 330 (16.9) | 17 (2.7) | 334 (15.4) | 14 (3.6) | 224 (24.6) | 97 (8.6) | |||
| 65 to 74 | 1013 (52.0) | 150 (24.2.) | 1041 (48.1) | 117 (29.8) | 498 (54.7) | 495 (43.9) | |||
| 75 to 84 | 489 (25.1) | 282 (45.5) | 617 (28.5) | 150 (38.3) | 158 (17.4) | 405 (35.9) | |||
| ≥85 | 91 (4.7) | 167 (26.9) | 148 (6.8) | 108 (27.6) | 12 (1.3) | 124 (11.0) | |||
| Women (%) | 858 (44.1) | 251 (40.5) | 0.09 | 944 (43.6) | 165 (42.1) | 0.95 | 419 (46.0) | 471 (41.8) | 0.03 |
| Race/ethnicity | |||||||||
| White | 1946 (100) | 620 (100) | NA | 2165 (100) | 392 (100) | 909 (100) | 1128 (100) | NA | |
| BMI, kg/m2 | 28.4 (5.3) | 28.6 (5.5) | 0.03 | 28.4 (5.3) | 28.9 (5.9) | 0.01 | 28.5 (5.1) | 28.3 (5.4) | 0.98 |
| Smoking (%) | 112 (6.9) | 46 (9.7) | <0.0001 | 131 (7.4) | 27 (8.8) | 0.005 | 43 (5.8) | 79 (8.6) | <0.0001 |
| Currently employed (%) | 574 (35.6) | 66 (13.9) | 0.01 | 602 (34.0) | 39 (12.7) | 0.34 | 362 (48.5) | 213 (23.1) | <0.0001 |
| Education | |||||||||
| Less than high school (%) | 18 (1.0) | 50 (8.7) | <0.0001 | 40 (2.0) | 28 (7.8) | <0.0001 | 5 (0.6) | 30 (2.9) | <0.0001 |
| High school (%) | 369 (20.6) | 260 (45.1) | 495 (24.8) | 131 (36.4) | 120 (14.3) | 335 (32.2) | |||
| Some college (%) | 540 (30.1) | 169 (29.3) | 594 (29.7) | 108 (30.0) | 237 (28.1) | 317 (30.5) | |||
| College and higher (%) | 867 (48.5) | 97 (16.8) | 871 (43.6) | 93 (25.8) | 480 (57.0) | 357 (34.4) | |||
| Hypertension (%) | 958 (59.4) | 371 (78.4) | 0.001 | 1093 (61.8) | 228 (74.5) | 0.43 | 399 (53.4) | 627 (68.2) | 0.01 |
| Hyperlipidemia (%) | 1224 (76.3) | 349 (75.2) | 0.11 | 1341 (76.4) | 227 (74.7) | 0.32 | 557 (75.1) | 704 (77.52) | 0.95 |
| Diabetes (%) | 354 (22.2) | 140 (30.6) | 0.004 | 400 (23.0) | 93 (31.1) | 0.02 | 159 (21.5) | 214 (23.8) | 0.67 |
| CVD (%) | 289 (14.8) | 178 (28.7) | 0.001 | 362 (16.7) | 105 (26.8) | 0.12 | 111 (12.2) | 218 (19.3) | 0.23 |
| Atrial fibrillation (%) | 192 (9.9) | 91 (14.7) | 0.86 | 221 (10.2) | 60 (15.3) | 0.8 | 70 (7.7) | 132 (11.7) | 0.41 |
BMI indicates body mass index; CVD, cardiovascular disease.
P value is adjusted by age and sex.
Table 3.
Study Sample Characteristics Among Framingham Heart Study Third Generation Participants by Internet, Cell Phone, or Smartphone Usage
| Internet (n=3216) | No Internet (n=96) | P Value | Cell Phone (n=3225) | No Cell Phone (n=80) | P Value | Smartphone (n=2606) | No Smartphone (n=585) | P Valuea | |
|---|---|---|---|---|---|---|---|---|---|
| Age, y | 51.4 (8.9) | 59.6 (7.7) | <0.0001 | 51.4 (8.9) | 59.0 (7.6) | <0.0001 | 50.3 (8.6) | 56.2 (8.7) | <0.0001 |
| Age groups, y | <0.0001 | <0.0001 | <0.0001 | ||||||
| 20 to 34 | 148 (4.5) | — | 148 (4.6) | — | 136 (5.2) | 12 (2.1) | |||
| 35 to 44 | 609 (18.9) | 2 (2.1) | 606 (18.8) | 3 (3.8) | 564 (21.6) | 41 (7.0) | |||
| 45 to 54 | 1275 (39.6) | 25 (26.0) | 1278 (39.6) | 18 (22.5) | 1067 (40.9) | 197 (33.7) | |||
| 55 to 64 | 1007 (31.3) | 52 (54.2) | 1018 (31.6) | 40 (50.0) | 754 (28.69) | 250 (42.7) | |||
| 65 to 74 | 174 (5.4) | 14 (14.6) | 169 (5.2) | 19 (23.8) | 82 (3.1) | 82 (14.0) | |||
| 75 to 84 | 3 (0.1) | 3 (3.1) | 6 (0.2) | — | 3 (0.1) | 3 (0.5) | |||
| Women (%) | 1439 (44.7) | 56 (58.3) | 0.02 | 1447 (44.9) | 45 (56.3) | 0.06 | 1157 (44.4) | 276 (47.2) | 0.25 |
| Race/ethnicity | |||||||||
| White | 3162 (98.4) | 93 (96.9) | 0.18 | 3172 (98.4) | 76 (95.0) | 0.01 | 2565 (98.5) | 573 (97.9) | 0.26 |
| Black | 3 (0.1) | — | 3 (0.1) | — | 2 (0.1) | 1 (0.2) | |||
| Asian | 1 (0.01) | — | 1 (0.009) | — | 1 (0.005) | — | |||
| Others | 48 (1.5) | 3 (3.1) | 47 (1.5) | 4 (5.0) | 36 (1.4) | 11 (1.9) | |||
| BMI, kg/m2 | 27.8 (5.8) | 28.6 (5.5) | 0.03 | 27.8 (5.7) | 28.7 (7.3) | 0.48 | 27.6 (5.6) | 28.7 (6.4) | 0.02 |
| Smoking (%) | 274 (9.6) | 46 (9.7) | <0.0001 | 289 (10.1) | 13 (13.8) | 0.02 | 220 (9.6) | 64 (12.3) | 0.015 |
| Currently employed (%) | 2456 (86.2) | 56 (69.1) | 0.0009 | 2461 (86.3) | 49 (69.0) | 0.019 | 2027 (88.2) | 404 (77.4) | <0.0001 |
| Education | |||||||||
| Less than high school (%) | 13 (0.4) | 4 (4.2) | <0.0001 | 17 (0.5) | — | 0.06 | 11 (0.4) | 6 (1.0) | <0.0001 |
| High school (%) | 389 (12.1) | 52 (54.7) | 420 (13.1) | 19 (24.4) | 269 (10.4) | 143 (24.5) | |||
| Some college (%) | 1002 (31.3) | 32 (33.7) | 1001 (31.1) | 29 (37.2) | 787 (30.3) | 203 (34.8) | |||
| College and higher (%) | 1802 (56.2) | 7 (7.4) | 1778 (55.3) | 30 (38.5) | 1532 (58.9) | 231 (39.6) | |||
| Hypertension (%) | 605 (21.3) | 35 (43.2) | 0.32 | 609 (21.4) | 28 (39.4) | 0.83 | 425 (18.5) | 169 (32.4) | 0.02 |
| Hyperlipidemia (%) | 1262 (44.3) | 48 (59.3) | 0.9 | 1268 (44.5) | 38 (54.3) | 0.22 | 990 (43.1) | 257 (49.2) | 0.17 |
| Diabetes (%) | 272 (9.7) | 18 (23.1) | 0.39 | 272 (9.7) | 18 (26.5) | 0.09 | 194 (8.6) | 75 (14.6) | 0.32 |
| CVD (%) | 109 (3.4) | 9 (9.4) | 0.19 | 109 (3.4) | 6 (7.5) | 0.76 | 73 (2.8) | 33 (5.6) | 0.34 |
| Atrial fibrillation (%) | 48 (1.5) | 2 (2.1) | 0.32 | 47 (1.5) | 3 (3.8) | 0.92 | 28 (1.1) | 17 (2.9) | 0.06 |
BMI indicates body mass index; CVD, cardiovascular disease.
P value is adjusted for age and sex.
Table 4.
Study Sample Characteristics Among Framingham Heart Study Omni Participants by Internet, Cell Phone, or Smartphone Usagea
| Internet (n=459) | No Internet (n=73) | P Value | Cell Phone (n=496) | No Cell Phone (n=33) | P Value | Smartphone (n=364) | No Smartphone (n=112) | P Valueb | |
|---|---|---|---|---|---|---|---|---|---|
| Age, y | 58.6 (13.2) | 71.7 (8.6) | <0.0001 | 59.6 (13.3) | 71.9 (9.4) | <0.0001 | 56.4 (12.8) | 67.9 (10.5) | <0.0001 |
| Age groups, y | <0.0001 | <0.0001 | <0.0001 | ||||||
| 20 to 34 | 30 (6.5) | — | 30 (6.0) | — | 29 (8.0) | 1 (0.9) | |||
| 35 to 44 | 54 (11.8) | — | 53 (10.7) | — | 51 (14.0) | 2 (1.8) | |||
| 45 to 54 | 79 (17.2) | 2 (2.7) | 80 (16.1) | 1 (3.0) | 68 (18.7) | 10 (8.9) | |||
| 55 to 64 | 139 (30.3) | 11 (15.1) | 144 (29.0) | 6 (18.2) | 115 (31.6) | 24 (21.4) | |||
| 65 to 74 | 116 (25.3) | 35 (47.9) | 135 (27.2) | 14 (42.4) | 85 (23.4) | 43 (38.4) | |||
| 75 to 84 | 33 (7.2) | 18 (24.7) | 44 (8.9) | 8 (24.2) | 15 (4.1) | 25 (22.3) | |||
| ≥85 | 8 (1.7) | 7 (9.6) | 10 (2.0) | 4 (12.1) | 1 (0.3) | 7 (6.3) | |||
| Women (%) | 190 (41.4) | 27 (37.0) | 0.48 | 206 (41.5) | 11 (33.3) | 0.06 | 160 (44.0) | 36 (32.1) | 0.02 |
| Race/ethnicity | |||||||||
| White | 6 (1.2) | — | 0.98 | 6 (1.2) | — | 0.01 | 5 (1.4) | 1 (0.9) | 0.23 |
| Black | 139 (30.3) | 19 (26.0) | 145 (29.2) | 12 (36.4) | 103 (28.3) | 34 (30.4) | |||
| Hispanic | 142 (30.9) | 45 (61.6) | 170 (34.3) | 17 (51.5) | 123 (33.8) | 39 (34.8) | |||
| Asian | 127 (27.7) | 8 (11.0) | 131 (26.4) | 4 (12.1) | 95 (26.1) | 33 (29.5) | |||
| Others | 45 (9.8) | 1 (1.4) | 44 (8.9) | — | 38 (10.4) | 5 (4.5) | |||
| BMI, kg/m2 | 28.1 (5.7) | 28.9 (6.6) | 0.41 | 28.2 (5.8) | 27.6 (6.1) | 0.48 | 28.4 (5.8) | 27.7 (5.5) | 0.17 |
| Smoking (%) | 18 (4.4) | 5 (10.0) | 0.056 | 22 (5.1) | 1 (4.0) | 0.02 | 18 (5.6) | 4 (4.3) | 0.72 |
| Currently employed (%) | 266 (65.0) | 9 (18.0) | 0.03 | 264 (61.3) | 10 (40.0) | 0.019 | 228 (70.8) | 30 (32.3) | 0.72 |
| Hypertension (%) | 169 (41.3) | 38 (76.0) | 0.07 | 189 (43.9) | 15 (60.0) | 0.83 | 115 (35.7) | 64 (68.8) | 0.02 |
| Hyperlipidemia (%) | 225 (55.1) | 37 (75.5) | 0.84 | 242 (56.3) | 17 (70.8) | 0.22 | 164 (51.1) | 66 (71.0) | 0.92 |
| Diabetes (%) | 93 (23.3) | 21 (45.7) | 0.26 | 103 (24.5) | 10 (45.5) | 0.09 | 64 (20.2) | 32 (36.0) | 0.56 |
| CVD (%) | 36 (7.8) | 18 (24.7) | 0.04 | 49 (9.9) | 5 (15.2) | 0.76 | 28 (7.7) | 18 (16.1) | 0.73 |
| Atrial fibrillation (%) | 5 (1.1) | 3 (4.4) | 0.31 | 7 (1.5) | 1 (3.3) | 0.92 | 4 (1.2) | 3 (2.9) | 0.65 |
BMI indicates body mass index; CVD, cardiovascular.
Education information incompletely ascertained and therefore not included in this table.
P value is adjusted for age and sex.
Figure 1.
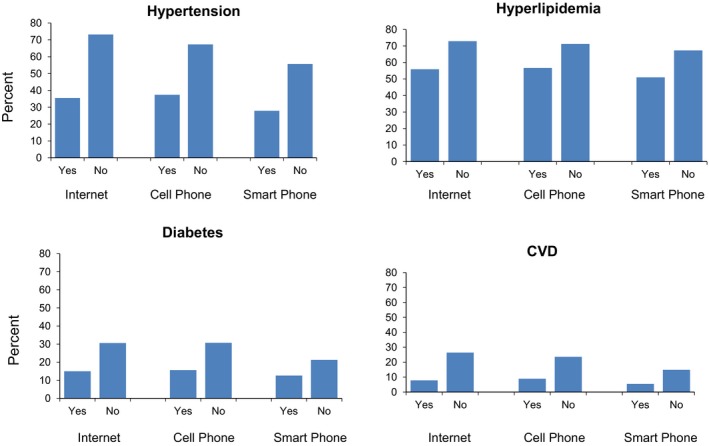
Prevalence of hypertension, hyperlipidemia, diabetes, and cardiovascular disease (CVD) among those with Internet, cell phone, and smartphone access compared with those without access. CVD was defined as myocardial infarction, angina pectoris, coronary insufficiency, cerebrovascular accident, transient ischemic attack, intermittent claudication, and heart failure. All cell counts can be found in Table 1.
Cell phone users tended to be younger (aged 60.0 versus 75.5 years), were more likely to be currently employed (68.5% versus 26.7%, P=0.0005), were less likely to smoke (8.7% versus 6.1%, P=0.004), and were less likely to have hyperlipidemia (56.7% versus 71.2%, P=0.01, Table 1). We did not observe differences in hypertension, diabetes, CVD, or atrial fibrillation by cell phone use.
Slightly less than two‐thirds (60.1%) of survey responders had a smartphone. Among smartphone users, 2689 had an iPhone (Apple Inc) and 1548 had an Android‐based (Google Inc) smartphone. Smartphone users were younger (aged 55.4 versus 68.5 years, P<0.0001), less likely to smoke (8.3% versus 9.4%, P<0.0001), more likely to be currently employed (81.1% versus 43.9%, P<0.0001), more likely to have a college education, and less likely to have hypertension (27.9% versus 55.7%, P=0.0002). We did not observe differences in hyperlipidemia, diabetes, CVD, or atrial fibrillation by smartphone use. Additional details can be found in Table 1.
In the Offspring cohort (Table 2), Internet users tended to be 8 years younger on average than those who did not use the Internet (P<0.0001). Internet users were less likely to smoke and had lower rates of hypertension, diabetes, and CVD. Similar but less striking trends were observed for cell and smartphone usage in this cohort as well as in the Third Generation (Table 3) and Omni (Table 4) cohorts.
Discussion
Digital connectedness, when assessed on the basis of access to the Internet, email, Wi‐Fi, cell phones, or smartphones, was fairly high among FHS participants. Despite this, important differences existed among those who use technology and those who do not, with marked differences in age, educational attainment, and CVD risk factor profiles. Finally, those with smartphones represented less than two‐thirds of survey respondents.
With the increasing ubiquity of home Internet, Wi‐Fi, and smartphones, paired with the rapid development of wearable devices, there is increased focus on collecting biomedical data from participants in their home environments. The digital health trend has been hailed as potentially revolutionary in transforming health care.6, 7, 8, 9 The eHealth and mHealth technologies have been advanced as convenient, resource‐effective, and efficient ways to collect health data from individual persons in their everyday lives to inform both clinical care and research. A key component of the success and ultimate transformative power of this new technology is whether people have access to the technology and are willing to use it. Mobile digital health data collection is fairly new and remains largely untested in established population‐based cohorts and in clinical research.14
Our findings highlight potential opportunities and challenges of reaching study participants through technology. Within an existing cohort, there might be limited reach (≈60% of eligible participants) with smartphones. An alternative approach is to recruit a de novo cohort based on access to technology. Whereas de novo targeted recruitment would increase the number of participants within any given study, generalizability is an important consideration, given the demographics of those who use technology. In addition, participants who report technology usage tend to be younger and to have more favorable CVD risk factor profiles, potentially biasing cohorts that ascertain participants using these modalities. Our findings also have implications for users of clinical technology applications, suggesting that similar biases may exist. Leveraging social networks to reach potential participants through technology is an important future opportunity. The social network of the Offspring cohort of the FHS has been mapped,15 and it may be possible to leverage this network in the future to promote the uptake and use of technology.
Strengths of our work include the use of the well‐characterized FHS cohort. Some limitations warrant mention. The generalizability of the FHS may be limited; however, our findings mirrored those in a recent report from the Pew Research Center that noted 64% of US respondents have a smartphone16 and 84% of US respondents use the Internet.17 The FHS consists predominantly of white participants; generalizability to other ethnicities and races is uncertain. Finally, even though our connectedness survey was administered recently (2014–2015), continued penetrance of digital connectedness and smartphone technology will occur over time. Nonetheless, our findings remain applicable to studies wishing to recruit technology‐enabled cohorts in the present, such as cohorts being considered through the Precision Medicine Initiative (http://www.nih.gov/precisionmedicine/09172015-pmi-working-group-report.pdf).
Digital connectedness varies substantially by age; those who are connected tend to be younger and to have more favorable CVD risk factor profiles. Less than two‐thirds of FHS participants responding to the survey had a smartphone. The generalizability of studies focused on digitally connected persons may have limitations.
Sources of Funding
The National Heart, Lung, and Blood Institute's Framingham Heart Study is supported by contract N01‐HC‐25195 and HHSN268201500001I; 2R01HL092577; 1R01HL128914; 1P50HL120163.
Disclosures
Dr Caroline S. Fox became an employee of Merck Research Labs as of December 14, 2015. None of the additional authors report any relevant conflicts of interest.
Supporting information
Data S1. Framingham Heart Study Participant Tracking Update.
(J Am Heart Assoc. 2016;5:e003193 doi: 10.1161/JAHA.116.003193)
References
- 1. Rosbash M. A threat to medical innovation. Science. 2011;333:136. [DOI] [PubMed] [Google Scholar]
- 2. Lauer MS. Time for a creative transformation of epidemiology in the United States. JAMA. 2012;308:1804–1805. [DOI] [PubMed] [Google Scholar]
- 3. Khoury MJ, Lam TK, Ioannidis JP, Hartge P, Spitz MR, Buring JE, Chanock SJ, Croyle RT, Goddard KA, Ginsburg GS, Herceg Z, Hiatt RA, Hoover RN, Hunter DJ, Kramer BS, Lauer MS, Meyerhardt JA, Olopade OI, Palmer JR, Sellers TA, Seminara D, Ransohoff DF, Rebbeck TR, Tourassi G, Winn DM, Zauber A, Schully SD. Transforming epidemiology for 21st century medicine and public health. Cancer Epidemiol Biomarkers Prev. 2013;22:508–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sorlie PD, Bild DE, Lauer MS. Cardiovascular epidemiology in a changing world–challenges to investigators and the National Heart, Lung, and Blood Institute. Am J Epidemiol. 2012;175:597–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Manolio TA, Weis BK, Cowie CC, Hoover RN, Hudson K, Kramer BS, Berg C, Collins R, Ewart W, Gaziano JM, Hirschfeld S, Marcus PM, Masys D, McCarty CA, McLaughlin J, Patel AV, Peakman T, Pedersen NL, Schaefer C, Scott JA, Sprosen T, Walport M, Collins FS. New models for large prospective studies: is there a better way? Am J Epidemiol. 2012;175:859–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Patel MS, Asch DA, Volpp KG. Wearable devices as facilitators, not drivers, of health behavior change. JAMA. 2015;313:459–460. [DOI] [PubMed] [Google Scholar]
- 7. Powell AC, Landman AB, Bates DW. In search of a few good apps. JAMA. 2014;311:1851–1852. [DOI] [PubMed] [Google Scholar]
- 8. Steinhubl SR, Muse ED, Topol EJ. Can mobile health technologies transform health care? JAMA. 2013;310:2395–2396. [DOI] [PubMed] [Google Scholar]
- 9. Topol EJ, Steinhubl SR, Torkamani A. Digital medical tools and sensors. JAMA. 2015;313:353–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. The coming era of human phenotyping. Nat Biotechnol. 2015;33:567. [DOI] [PubMed] [Google Scholar]
- 11. Dawber TR, Kannel WB, Lyell LP. An approach to longitudinal studies in a community: the Framingham Heart Study. Ann N Y Acad Sci. 1963;107:539–556. [DOI] [PubMed] [Google Scholar]
- 12. Shurtleff D. Some characteristics related to the incidence of cardiovascular disease and death: Framingham Study, 18‐year follow‐up. Section 30 In: Kannel WB, Fordon T, eds. The Framingham Study: An Epidemiological Investigation of Cardiovascular Disease. Washington, DC: Department of Health, Education, and Welfare; 1973. (DHEW publication no. (NIH) 74‐599.). [Google Scholar]
- 13. Schnabel RB, Sullivan LM, Levy D, Pencina MJ, Massaro JM, D'Agostino RB Sr, Newton‐Cheh C, Yamamoto JF, Magnani JW, Tadros TM, Kannel WB, Wang TJ, Ellinor PT, Wolf PA, Vasan RS, Benjamin EJ. Development of a risk score for atrial fibrillation (Framingham Heart Study): a community‐based cohort study. Lancet. 2009;373:739–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Burke LE, Ma J, Azar KM, Bennett GG, Peterson ED, Zheng Y, Riley W, Stephens J, Shah SH, Suffoletto B, Turan TN, Spring B, Steinberger J, Quinn CC. Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2015;132:1157–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357:370–379. [DOI] [PubMed] [Google Scholar]
- 16. Pew Research Center, April, 2015, “The Smartphone Difference”. Available at: http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/. Accessed April 5, 2016.
- 17. Perrin A, Duggan M. “Americans’ Internet Access: 2000–2015.” Pew Research Center, June 2015.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Framingham Heart Study Participant Tracking Update.


