Abstract
Vitamin A (retinol) and its active metabolite, all-trans-retinoic acid (atRA), play critical roles in regulating the differentiation, growth and migration of immune cells. Similarly, as critical signaling molecules in the regulation of the cell cycle, retinoids are important in cancers. Concentrations of atRA are tightly regulated in tissues, predominantly by the availability of retinol, synthesis of atRA by ALDH1A enzymes and metabolism and clearance of atRA by CYP26 enzymes. The ALDH1A and CYP26 enzymes are expressed in several cell types in the immune system and in cancer cells. In the immune system the ALDH1A and CYP26 enzymes appear to modulate RA concentrations. Consequently, alterations in the activity of ALDH1A and CYP26 enzymes are expected to change disease outcomes in inflammation. There is increasing evidence from various disease models of intestinal and skin inflammation that treatment with atRA has a positive effect on disease markers. However, whether aberrant atRA concentrations or atRA synthesis and metabolism play a role in inflammatory disease development and progression is not well understood. In cancers, especially in acute promyelocytic leukemia and neuroblastoma, increasing intracellular concentrations of atRA appears to provide clinical benefit. Inhibition of the CYP26 enzymes to increase atRA concentrations and combat therapy resistance has been pursued as a drug target in these cancers. This chapter covers the current knowledge of how atRA and retinol regulate the immune system and inflammation, how retinol and atRA metabolism is altered in inflammation and cancer and what roles atRA metabolizing enzymes have in immune responses and cancers.
Keywords: Retinoic acid, vitamin A, CYP26, Inflammatory bowel disease, psoriasis, leukemia, neuroblastoma
I. Introduction
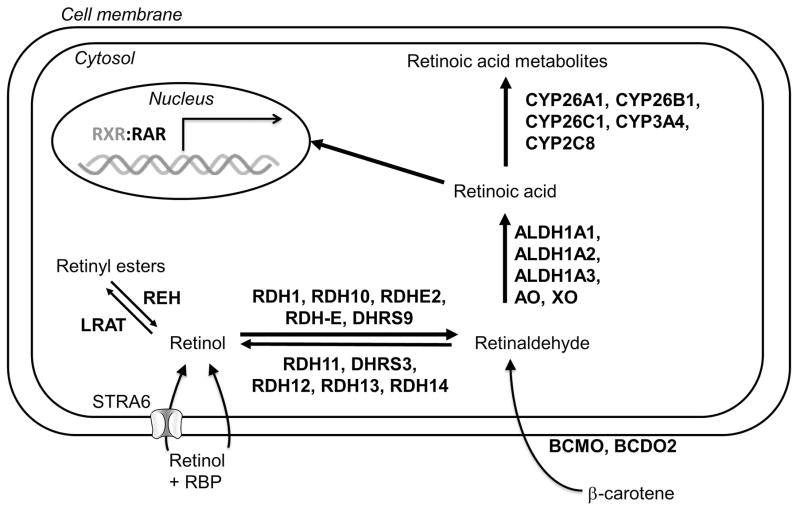
Vitamin A is one of the fat-soluble vitamins critical for health in humans and other mammals. Typically the term vitamin A is used to describe retinol and retinyl esters (Figure 1), including retinyl palmitate, that are the main dietary forms of vitamin A obtained from animal products (Schoeff, 1983; Sklan, 1987). However, retinol and retinyl esters are not biologically active but require oxidation by several enzymes to generate retinoic acid (RA), the main compound responsible for the biological activity of vitamin A. Retinyl esters serve as the reservoir of vitamin A in an organism and are stored in the body primarily in the liver stellate cells and in the lungs and adipose (Chytil, 1992; Sauvant, Cansell, & Atgié, 2011). The esterification of retinol and the hydrolysis and release of the stored esters as retinol are regulated by the activity of two enzymes, lecithin retinol acyltransferase (LRAT) and retinyl ester hydrolase (REH), respectively (Figure 2). The circulating retinol is taken up into target cells by an uptake transporter STRA6, but due to its high lipophilicity retinol may also cross membranes by passive diffusion. In target cells retinol is oxidized to retinaldehyde by several alcohol dehydrogenase enzymes including RDH10, RDH-E, RDHE2 and DHRS9 (D’Ambrosio, Clugston, & Blaner, 2011; Napoli, 2012; Ross, 2003) (Figure 2). Alternatively, retinaldehyde can be obtained via direct cleavage of β-carotene by carotenoid cleavage enzymes (Lobo, Amengual, Palczewski, Babino, & von Lintig, 2012). Two enzymes have been indicated as the primary enzymes generating retinaldehyde, mammalian β,β-carotene-15,15′-monooxygenase 1 (BCMO1) and β,β-carotene-9,10-dioxygenase 2 (BCDO2) (Lobo et al., 2012). To generate vitamin A from dietary carotenoids, retinaldehyde has to be reduced to retinol, and retinol is subsequently esterified and stored as the esters (Figure 2). The reduction of retinaldehyde to retinol in humans is catalyzed by several enzymes including RDH11, RDH12, RDH13, RDH14 and DHRS3 (Kedishvili, 2013). The relative contribution of these reductive enzymes to retinol synthesis from retinaldehyde is not well characterized, and the importance may vary between species, tissues, developmental stages and age after birth. While the conversion of retinol to retinaldehyde is reversible, oxidation of retinaldehyde to RA appears to be irreversible. Four aldehyde dehydrogenase (ALDH) enzymes and aldehyde and xanthine oxidase have been reported to catalyze the oxidation of retinaldehyde to RA (Figure 2) (Ambroziak, Izaguirre, & Pietruszko, 1999; Kumar, Sandell, Trainor, Koentgen, & Duester, 2012; Taibi & Nicotra, 2007; Terao, Kurosaki, Barzago, Fratelli, Bagnati, Bastone, et al., 2009). In addition, several cytochrome P450 enzymes in humans and rats oxidize retinaldehyde to RA (Raner, Vaz, & Coon, 1996; Tomita, Okuyama, Ohnishi, & Ichikawa, 1996; Zhang, Dunbar, & Kaminsky, 2000). It is generally believed that ALDH1A2 and ALDH1A3 are the predominant enzymes that form RA during fetal and embryonic development, as neither the Aldh1a2−/− nor the Aldh1a3−/− mice are viable. However, the importance of ALDH1A1 in RA synthesis is unclear as Aldh1a1−/− mice are viable and fertile (Kumar et al., 2012). Very little is known of the potential importance of ALDH8A1 in RA synthesis. Recent studies have shown that the relative importance of ALDH1A enzymes in RA synthesis is tissue specific. For example ALDH1A1 appears to be responsible for RA synthesis in the liver while ALDH1A2 and ALDH1A1 make the main contributions to RA synthesis in the testes (Arnold, Kent, Hogarth, Schlatt, Prasad, Haenisch, et al., 2015; Arnold, Kent, Hogarth, Griswold, Amory, & Isoherranen, 2015). This tissue specific expression is important, as locally generated RA gradients are believed to be a key factor in regulating biological processes. Yet, the overall quantitative importance of the different enzymes in retinaldehyde oxidation in different species and organs is not well characterized.
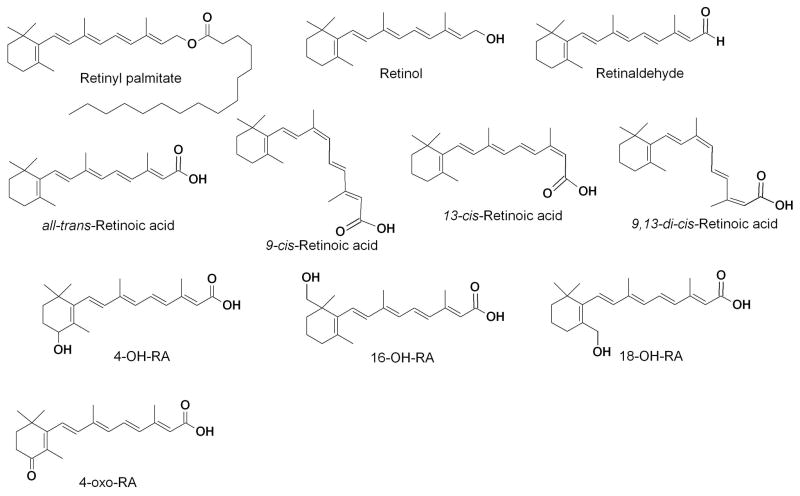
Figure 1.
Chemical Structures of retinyl palmitate, retinol, retinaldehyde and the retinoic acid isomers and metabolites
Figure 2. Enzymatic processes that regulate retinoic acid homeostasis in humans.
The enzyme retinyl ester hydrolase (REH) hydrolyzes retinyl esters, acquired as vitamin A from the diet, to retinol, and lecithin retinol acyltransferase (LRAT) esterifies retinol to the esters for storage. STRA6 transports retinol bound to the retinol binding protein (RBP) into the target cell where several enzymes control the reversible oxidation of retinol to retinaldehyde. Retinaldehyde, derived from retinyl esters or from β-carotene precursors, is irreversibly oxidized to the active metabolite retinoic acid. In the cell retinoic acid will traverse to the nucleus and bind to RXR or RAR to initiate gene transcription. Retinoic acid is cleared through oxidation to polar metabolites by several P450s, predominantly the CYP26 family.
Retinoic acid has five chemical isomers (all-trans-RA, 9-cisRA, 13-cisRA, 11-cisRA and 9,13-dicisRA) (Figure 1). Of these isomers all-trans-RA (atRA) is considered to be the biologically active isomer and the primary enzymatic product of retinaldehyde oxidation. However, in various species including humans, the 9-cisRA, 13-cisRA, and 9,13-dicisRA isomers have also been detected in different organs (Arnold, Amory, Walsh, & Isoherranen, 2012; Kane, Folias, Wang, & Napoli, 2008). The in vivo source of these isomers is not clear. Although isomerization between all-trans and cis retinols has been characterized (McBee, Kuksa, Alvarez, de Lera, Prezhdo, Haeseleer, et al., 2000), the stereochemistry of the retinaldehyde precursor in vivo has not been determined. 9-cisRA binds to retinoid X receptors (RXRs) and this isomer may be important in some tissues such as the pancreas where it has been detected (Kane, Folias, Pingitore, Perri, Obrochta, Krois, et al., 2010). Yet, 9-cisRA concentrations in vivo are typically very low or undetectable, and the biological role of this isomer has not been confirmed. In contrast, 13-cisRA is detected in all tissues and the concentrations of 13-cisRA are often higher than atRA. Yet, 13-cisRA is considered to be devoid of biological activity due to its low affinity to nuclear retinoic acid receptors (RARs) in comparison to atRA (Aström, Pettersson, Krust, Chambon, & Voorhees, 1990). In vivo, 13-cisRA isomerizes to atRA both via glutathione-S-transferase-mediated and thermodynamic processes (Chen & Juchau, 1997; Sass, Forster, Bock, & Nau, 1994). Hence the activity of 13- cisRA is believed to be a result of isomerization to atRA. In many species, including human, 9,13-dicisRA is also found at concentrations as high as atRA and 13-cisRA. However, this isomer appears to be devoid of biological activity (Chen, Sass, Seltmann, Nau, Orfanos, & Zouboulis, 2000; Nonnecke, Horst, Dubeski, & Reinhardt, 1997; Zile, Emerick, & DeLuca, 1967). Throughout this text the terms atRA and 13-cisRA are used when a specific isomer has been identified in the research, and the generic term RA is employed when the identity of the isomer has not been specified.
a) Retinoic acid signaling and biological activity
Retinoid signaling and atRA have been shown to be important in various biological processes and in treatment of several diseases. For example, endogenous atRA is critical in the maintenance of healthy skin, epithelia and immune system (Napoli, 2012), in regulation of bone growth and homeostasis, and in regulating continuous, asynchronous, spermatogenesis (Chung & Wolgemuth, 2004; Hogarth & Griswold, 2013). In addition, atRA is a classic morphogen that regulates embryonic development (Duester, 2008), organogenesis, stem cell differentiation (Gudas & Wagner, 2011) and body patterning in all chordates. Retinoid signaling also plays a central role in neuronal differentiation (Maden, 2007) and in tissue repair and regeneration (Gudas, 2012). In addition, retinoid signaling has been linked to regulation of insulin stimulated glucose secretion (Chung et al., 2004; Kane et al., 2010, 2008) and to lipid homeostasis and adiposity (Bonet, Ribot, & Palou, 2012). Recently atRA has been found to also play a role in modulating the inflammation that accompanies many human diseases. Exogenous atRA and 13-cisRA have been shown to be beneficial in the treatment of chronic hand eczema (Ruzicka, Larsen, Galewicz, Horváth, Coenraads, Thestrup-Pedersen, et al., 2004) and in a variety of cancers including acute promyelocytic leukemia (APL) (Tang & Gudas, 2011), neuroblastoma in children (Veal, Cole, Errington, Pearson, Foot, Whyman, et al., 2007), and Kaposi’s sarcoma (Altucci, Leibowitz, Ogilvie, de Lera, & Gronemeyer, 2007). Whether exogenous RA functions via similar pathways and receptors as endogenous atRA is not well defined.
The biological activity of atRA is predominantly mediated by binding to RARα, RARβ and RARγ, but atRA has also been shown to bind to peroxisome proliferator-activated receptors (PPARβ/δ) (Schug, Berry, Shaw, Travis, & Noy, 2007). Binding of retinoids to either RARs or PPARs results in increased transcription of respective target genes, and these regulatory mechanisms have been thoroughly reviewed elsewhere (Gudas, 2012; Noy, 2010). The observed effects of atRA on gene transcription are dependent on the cellular concentrations of atRA as well as the expression levels of RAR and PPAR isoforms. In addition, the expression of cellular binding proteins that bind atRA, most notably CRABPs and FABPs, has been shown to direct the activity of atRA isomers towards the different nuclear receptors (Noy, 2000; Schug et al., 2007). Overall, atRA signaling in various tissues is tightly controlled by the interplay between expression levels of the nuclear receptors and binding proteins, and the expression and activity of the atRA synthesizing and eliminating enzymes that control of atRA concentrations in target tissues.
b) Biochemistry, expression and function of CYP26 enzymes
The clearance of atRA is mediated predominantly by the cytochrome P450 family 26 enzymes (CYP26) in all chordates, although many other CYP enzymes including human CYP3A4 and CYP2C8 and rat Cyp2c22 also oxidize atRA and its 9-cisRA and 13-cisRA isomers (Marill, Cresteil, Lanotte, & Chabot, 2000; McSorley & Daly, 2000; Nadin & Murray, 1999). It is widely believed that oxidation of atRA in the 4-position of the β-ionone ring to generate 4-OH-RA (Figure 1) is the predominant route of elimination of atRA but no unequivocal mass balance studies confirm this. Determining the major route of atRA elimination in humans or animal species is challenging as 4-OH-RA is extensively metabolized both in vitro and in vivo. 4-OH-RA is glucuronidated predominantly by UGT2B7 and oxidized by CYP26s and microsomal ADHs to 4-oxo-RA and other products (Samokyszyn, Gall, Zawada, Freyaldenhoven, Chen, Mackenzie, et al., 2000; Topletz, Tripathy, Foti, Shimshoni, Nelson, & Isoherranen, 2015). The CYP26s and other CYP enzymes also generate several other hydroxylation products from atRA (Thatcher, Buttrick, Shaffer, Shimshoni, Goodlett, Nelson, et al., 2011). The best characterized of these additional hydroxylation products is the 18-OH-RA (Figure 1) which has been synthesized (Rosenberger & Neukom, 1982) and shown to be a metabolite formed by CYP26A1, CYP26B1 and other CYPs (Topletz, Thatcher, Zelter, Lutz, Tay, Nelson, et al., 2012). In addition, 16-OH-RA (Figure 1) has been proposed as a metabolite of atRA, but this metabolite has never been synthesized, and therefore the identification of the metabolite is based on interpretation of mass spectrometry fragmentation patterns (Thatcher et al., 2011).
The CYP26 family consists of three highly conserved enzymes CYP26A1, CYP26B1 and CYP26C1. Despite the fact that RA appears to be the primary substrate of all three CYP26 enzymes and all CYP26s metabolize atRA predominantly to 4-OH-RA, these three enzymes share only 40–50% sequence similarity in a given species (Thatcher & Isoherranen, 2009). Yet, the individual isoforms are highly conserved across chordates which all have three CYP26 enzymes. Overall, from genomic and phylogenetic analysis it appears that CYP26 enzymes evolved very early together with RA signaling and play critical roles in regulating developmental processes. As such it is not surprising that both Cyp26a1−/− and Cyp26b1−/− mice suffer from multiple developmental defects. The Cyp26a1−/− mice die during gestation while Cyp26b1−/− mice survive till birth but die shortly after and have severe, but specific, malformations (Abu-Abed, Dollé, Metzger, Beckett, Chambon, & Petkovich, 2001; MacLean, Abu-Abed, Dollé, Tahayato, Chambon, & Petkovich, 2001; Uehara, Yashiro, Mamiya, Nishino, Chambon, Dolle, et al., 2007; Yashiro, Zhao, Uehara, Yamashita, Nishijima, Nishino, et al., 2004). Notably the pattern of developmental defects in the two mouse models is different pointing to the unique roles the two CYP26 enzymes play during organogenesis and body axis formation. In contrast, Cyp26c1−/− mice are viable and free of malformations although the simultaneous knock-out of Cyp26c1 with Cyp26a1 aggravates the phenotype of the Cyp26a1−/− mice (Uehara et al., 2007).
Functionally, CYP26 enzymes are membrane anchored P450 proteins that require NADPH and P450 reductase for their function. While it is theoretically possible that the CYP26 enzymes reside in the mitochondria instead of the endoplasmic reticulum (ER), the fact that the CYP26 enzymes require P450 reductase from the ER membrane to function suggests that these enzymes are ER membrane bound (Lutz, Dixit, Yeung, Dickmann, Zelter, Thatcher, et al., 2009; Topletz et al., 2012). However, the localization of the CYP26 enzymes within a cell has not been unequivocally determined. Interestingly, unlike other P450 enzymes such as CYP17, cytochrome b5 does not affect the catalytic activity of the CYP26 enzymes, and P450 reductase seems to solely support the catalytic activity of these enzymes (Lutz et al., 2009). Overall the affinity of atRA to each of the CYP26 enzymes is high and the Km values for CYP26A1 and CYP26B1 are <100 nM for atRA. Interestingly, the Km value for atRA with the CYP26s approximates the concentrations of atRA in various tissues (Topletz et al., 2012). While the affinity of the substrate is high, the kcat values for atRA with CYP26 enzymes are similar to other mammalian P450 enzymes (approximately 1–10 pmol/min/pmol) (Thatcher, Zelter, & Isoherranen, 2010; Topletz et al., 2012). Since the affinity of atRA to CYP26 is approximately 1000-fold higher than that to other CYP enzymes, the overall intrinsic clearance of atRA by CYP26 enzymes is 1,000 to 10,000 fold higher than other CYP enzymes such as CYP3A4 and CYP2C8 (Thatcher et al., 2010). Therefore, even in tissues such as the human liver which have high expression levels of CYP3A4 and CYP2C8, the CYP26s are expected to be the main contributors to RA clearance even if they are expressed at low levels (Thatcher et al., 2011, 2009, 2010). Indeed, in a study of individual donors in a human liver bank, CYP26A1 was shown to be the main enzyme contributing to atRA clearance, but the expression of CYP26A1 was subject to considerable inter-individual variability (Thatcher, Zelter, & Isoherranen, 2010). Interestingly, in the human liver CYP26B1 protein was completely absent pointing to tissue and cell type specific roles of the CYP26 enzymes in adult tissues and during fetal development.
It is generally believed that RA concentrations in target tissues are regulated locally by RA synthesis and clearance, and that systemic RA concentrations do not reflect RA homeostasis in specific tissues. Therefore extrahepatic expression of CYP26 enzymes is expected and likely plays a role in tissue specific clearance and regulation of RA concentrations. Indeed CYP26A1 and CYP26B1 mRNA and protein are found in multiple extrahepatic human tissues (Topletz et al., 2012; Xi & Yang, 2008) with CYP26B1 appearing to have a higher expression in extrahepatic tissues than CYP26A1. In agreement with the human tissue data of CYP26 expression, metabolism of atRA was shown in rat testes, kidney, and lung microsomes (Fiorella & Napoli, 1994). In addition, CYP26 enzymes have been suggested to constitute a tissue barrier for RA distribution from circulation to specific organs. This hypothesis originated from the observation that uptake of administered radiolabeled RA to some tissues, such as the testes, pancreas and spleen, was limited (Ahluwalia, Gambhir, & Sekhon, 1975; Kurlandsky, Gamble, Ramakrishnan, & Blaner, 1995; McCormick, Kroll, & Napoli, 1983; J. E. Smith, Milch, Muto, & Goodman, 1973), and that CYP26 enzymes were detected in several barrier cells (Heise, Mey, Neis, Marquardt, Joussen, Ott, et al., 2006; Vernet, Dennefeld, Rochette-Egly, Oulad-Abdelghani, Chambon, Ghyselinck, et al., 2006; Xia, Ma, Sun, Yang, & Peng, 2010). The metabolic barrier provided by CYP26 enzymes in some tissues such as the testes likely ensures that RA gradients are regulated by enzyme expression and activity within the tissue and not by circulating concentrations. Therefore understanding the activity and expression of CYP26 enzymes in individual tissues and cell types is critically important for defining the relationship between atRA concentrations and biological outcomes within a tissue. Based on tissue specific expression and activity of CYP26 enzymes it can be hypothesized that tissue specific alterations in CYP26 activity will alter atRA concentrations in the given tissue and result in altered atRA signaling. For example, inhibition of CYP26s or genetic polymorphisms that decrease CYP26 activity would be expected to increase atRA concentrations within the tissue in which CYP26s are expressed. On the other hand, induction of CYP26s or increased activity of CYP26 enzymes within an organ is expected to decrease the overall exposure to atRA and possibly increase exposure to atRA metabolites that may also have pharmacological activity. Yet a direct effect of decreased or increased CYP26 activity and atRA concentrations in a tissue has never been demonstrated, even though P450 inhibitors such as talarozole and liarozole that also inhibit CYP26 do increase RA concentrations in various tissues and plasma (Nelson, Buttrick, & Isoherranen, 2013; Stoppie, Borgers, Borghgraef, Dillen, Goossens, Sanz, et al., 2000; Van Wauwe, Coene, Goossens, Cools, & Monbaliu, 1990). Likewise specific effects of CYP26A1 or CYP26B1 inhibition have never been shown to have different effects in different tissues.
In addition to metabolic enzymes, small binding proteins of the class of lipid binding proteins such as cellular retinoic acid binding proteins (CRABP-I and CRABP-II) that bind atRA with high affinity (Kd = 0.06 nM for CRABP-I and Kd = 0.13 nM for CRABP-II) (Dong, Ruuska, Levinthal, & Noy, 1999) are believed to alter atRA homeostasis and CYP26 activity. However, CRABP−/− mice are viable and devoid of any malformations or negative health effects (de Bruijn, Oerlemans, Hendriks, Baats, Ploemacher, Wieringa, et al., 1994; Lampron, Rochette-Egly, Gorry, Dollé, Mark, Lufkin, et al., 1995) putting the biological significance of the binding proteins to question. CRABP-II has been shown to deliver atRA to RAR in the nucleus whereas CRABP-I may serve a different function such as delivering atRA to the CYP26 enzymes. Whether these functions affect overall atRA homeostasis is still unknown.
II. Role of Retinoic Acid in the Immune System
For nearly 100 years vitamin A has been recognized as a critical nutritional component needed to support immunity. It is well established that vitamin A deficiency results in increased morbidity and mortality from certain pathogens, and several clinical trials have shown that vitamin A supplementation in at risk populations improves overall outcomes (Ross, 2012). In support of human studies, vitamin A deficient mice were shown to be completely deficient in CD4+ and CD8+ T-cells in the submucosal lamina propria in the intestine (Iwata, Hirakiyama, Eshima, Kagechika, Kato, & Song, 2004). This suggests that gut mucosal immunity is impaired in vitamin A deficiency, and potentially explains the specific link between poor outcomes in diarrheal disease and vitamin A deficiency. Yet, it is possible that retinol and RBP4 also contribute to regulation of gut mucosal immunity either together with RA or independent of RA as retinol and RBP concentrations are significantly decreased in vitamin A deficiency (de Pee & Dary, 2002; Gamble, Ramakrishnan, Palafox, Briand, Berglund, & Blaner, 2001) and retinol and RBP have been shown to have activity in the absence of RA via binding to STRA6 (Berry, Levi, & Noy, 2014; Marwarha, Berry, Croniger, & Noy, 2014). However, current evidence suggests that atRA itself is critical in maintaining immune homeostasis (Hall, Grainger, Spencer, & Belkaid, 2011; Raverdeau & Mills, 2014), is the required signaling molecule in the regulation of T-cell, B-cell and dendritic cell (DC) differentiation and function, and in the production of both pro- and anti-inflammatory cytokines (Hansen, Westendorf, & Buer, 2008; Raverdeau et al., 2014).
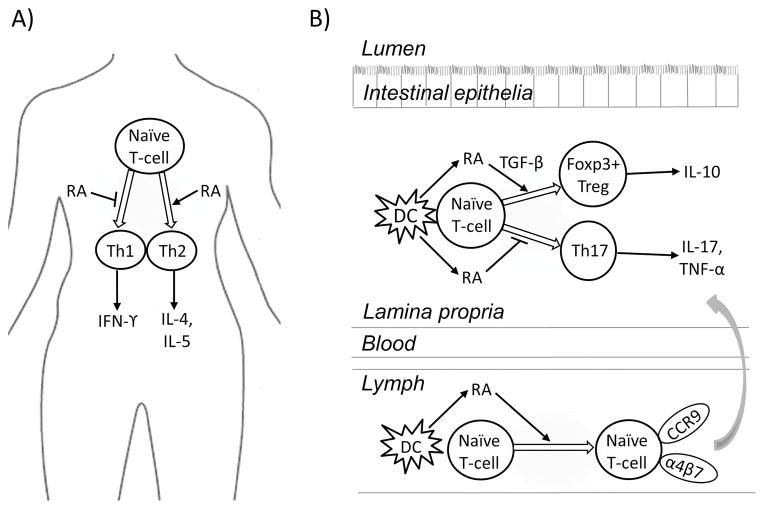
Vitamin A deficiency, which presumably results in lower concentrations of atRA, promotes naive CD4+ T-cell differentiation into Th1 cells, which secrete interferon-γ (Cantorna, Nashold, & Hayes, 1995). High concentrations of atRA on the other hand generally promote T-cell differentiation into Th2 cells producing IL-4 and IL-5 (Figure 3). Hence it appears that increasing concentrations of atRA in the precursor T-cell environment will increase the Th2 to Th1 cell ratio (Ross, 2012). In addition, of interest especially to gut mucosal immunity, atRA also regulates Th17 cell function by opposing Th17 cell commitment and inhibiting T-cell differentiation into Th17 cells (Mucida, Park, Kim, Turovskaya, Scott, Kronenberg, et al., 2007) (Figure 3). RA synthesis by the DCs in the gut-associated lymphoid tissue (GALT) is believed to initiate Treg cell differentiation. RA produced by DCs in GALT also induces the expression of α4β7 and CCR9 on T-cells upon antigen presentation (Iwata et al., 2004) inducing gut homing of the T-cells to the lamina propria over peripheral lymph nodes (Figure 3). Activation of naïve T-cells in the presence of RA induced CCR9 and the α4 integrin as well (Kang, Park, Cho, Ulrich, & Kim, 2011). In Treg cell activation RA acts synergistically with TGF-β to enhance the expression of Foxp3, a critical transcription factor for Treg cells (Hall et al., 2011; Mucida et al., 2007). The effects of atRA on differentiation and homing of Treg cells to the gut mucosa and inhibition of Th17 cell formation appears to be regulated via RARα (Mucida et al., 2007; Raverdeau et al., 2014). Hence, increasing RA concentrations is expected to prevent the induction of autoimmune T-cells and modulate inflammatory responses. Yet many of the responses observed with RA appear to be dependent on the cytokine environment. Overall, RA plays a critical role in modulating immune responses and inflammation, and regulation of RA concentrations is likely important in inflammatory and autoimmune diseases. However, how RA concentrations are controlled within the immune system is not well established, and it is possible that the roles of the individual enzymes are divergent in different inflammatory conditions and in different tissues.
Figure 3. Retinoic acid in steady state immune homoestatsis.
A) Throughout the body RA plays an important role in the ratio of Th1:Th2 cells by reducing differentiation of naïve T-cells into IFN-γ producing Th1 cells and promoting differentiation of Th2 cells which secrete IL-4 and IL-5. B) In gut associated lymphoid tissue dendritic cells (DCs) synthesize RA, which acts synergistically with TGF-β to initiate differentiation of Foxp3+ Treg cells and suppress T-cell differentiation into Th17 cells. RA produced by DCs also induces the expression of α4β7 and CCR9 on naïve T-cells to prompt gut homing to the lamina propria over peripheral lymph nodes. Cytokines shown are not a complete list but were chosen based on relevance to the text.
Based on current data, the DCs in the GALT express RDH and ALDH1A enzymes and produce RA (Iwata et al., 2004). The elimination of atRA also appears to be regulated within the immune system as CYP26 enzymes are expressed and inducible by atRA in T- and B-cells (Takeuchi, Yokota, Ohoka, & Iwata, 2011; Wen, Lopes, Soares, Farrell, Nelson, Qiao, et al., 2013). Interestingly, in naïve T-cells in vitro TGF-β inhibits and TNF-α enhances CYP26B1 induction by atRA (Takeuchi et al., 2011). CYP26B1 mRNA was found in T-cells from mouse GALT, including mesenteric lymph nodes and Payer’s patches, but not from peripheral lymph nodes (Takeuchi et al., 2011). CYP26A1 and CYP26B1 mRNA expression and RA-dependent induction has also been demonstrated in B-cells of healthy humans (Wen et al., 2013). In vitro, when T-cells from mice were stimulated under conditions promoting T-cell differentiation, CYP26B1 expression was significantly increased in differentiated Th17 cells but was significantly lower in differentiated Treg cells and lowest in undifferentiated T-cells suggesting that depletion of RA by CYP26B1 regulates RA concentrations within the T-cells (Chenery, Burrows, Antignano, Underhill, Petkovich, & Zaph, 2013). A higher expression of CYP26B1 should result in lower RA concentrations within the cells removing the RA signaling. However, somewhat surprisingly when CYP26B1 was knocked out in the T-cells, the frequency of both IL-17 producing T-cells (Th17 cells) and FoxP3+ Treg cells was increased (Chenery et al., 2013). Based on these data, it is likely that alterations in the activity of ALDH1A and CYP26 enzymes within the immune system are a key factor modulating atRA concentrations and signaling that subsequently drives immune and inflammatory responses.
III. CYP26 and Retinoic Acid in Chronic Inflammatory Diseases
A large portion of human diseases are associated with chronic inflammation. In some of these conditions inflammation is related to the primary pathology of the disease whereas in others only clinical associations between disease progression and inflammatory markers have been observed. For example, non-alcoholic fatty liver disease (NAFLD) is defined as an excess accumulation of lipids in the liver but progression to non-alcoholic steatohepatitis (NASH) is thought to be a result of triglyceride and cholesterol accumulation in the liver leading to oxidative stress, insulin resistance and inflammation (Depner, Philbrick, & Jump, 2013). As RA and RAR activation is known to play an important role in the liver and RA is an important regulator of inflammation, it is possible that development of NASH and associated inflammation involves altered atRA signaling. In the case of NAFLD and NASH, analysis of mRNA from patient liver biopsies showed increased mRNA levels of variety of enzymes involved in regulation of atRA and vitamin A concentrations including CRBP1, LRAT, RDH5, RDH11, DHRS3, ALDH1, ALDH3, and CYP26A1 (Ashla, Hoshikawa, Tsuchiya, Hashiguchi, Enjoji, Nakamuta, et al., 2010). However, whether any of these changes are associated with altered liver atRA concentrations, play a role in disease development and progression or are a result of liver disease is not known.
Perhaps the best demonstrated connections between chronic inflammatory markers and disease progression have emerged from autoimmune diseases. Autoimmune diseases arise from an abnormal immune response of the body against its own tissues or substances (Abella, Scotece, Conde, López, Lazzaro, Pino, et al., 2014; Feldmann, Brennan, & Maini, 1996). Treatment of these diseases generally focuses on regulation of immune system activity. While autoimmune diseases as well as inflammatory conditions are a large group of diseases this section focuses on those conditions in which atRA signaling and CYP26 activity has been shown to be altered or potentially play a role in modulating the disease progression.
a) Inflammatory bowel disease
Inflammatory bowel disease (IBD) is an inflammatory disease of the gastrointestinal tract and a link may exist between regulation of intestinal immunity by RA and IBD progression. The principal forms of IBD are Crohn’s disease (CD) and ulcerative colitis (UC). The pathology of these diseases is complicated and thought to arise as a result of environmental, genetic and immunologic factors. Both CD and UC are associated with an excessive response of mucosal adaptive and innate immunity (S. J. Brown & Mayer, 2007; Talley, Abreu, Achkar, Bernstein, Dubinsky, Hanauer, et al., 2011). In active IBD increased levels of macrophages and pro-inflammatory cytokines are found in intestinal mucosa (Mahida, 2000). Ex vivo studies in cells from UC patients and in vivo mouse studies have found that increasing atRA concentrations could overcome the dysfunction of the immune system and ameliorate inflammation. For example, in an in vitro colitis model using murine macrophages, atRA treatment decreased the activation of NFκB, a macrophage nuclear transcription factor, and production of the pro-inflammatory cytokine TNF-α. In a mouse model of colitis, atRA treatment reduced symptoms of inflammation including reduced infiltration of neutrophils, decreased levels of NFκB, and lower levels of TNF-α in colon tissues in comparison to control mice (Hong, Zhang, Guo, Xie, Wang, He, et al., 2014). Similar to mouse models of colitis, treatment of cultured colonic mucosa cells from UC patients with RA decreased concentrations of TNF-α, up-regulated Foxp3 and down-regulated IL-17, returning immunologic balance. The nuclear receptor RARα was implicated in regulating these RA effects (Bai, Lu, Guo, Liu, Chen, & Peng, 2009). These studies did not evaluate whether RA was a priori decreased in the disease setting due to either decreased synthesis or increased metabolism of RA. However, these studies suggest that increasing levels of atRA may be effective in halting the acute inflammatory response in IBD patients.
Further evidence of the potential benefit of increased RA in IBD comes from studies in T cell-specific CYP26B1−/− mice (Chenery et al., 2013). Although RA concentrations were not measured, it is expected that CYP26B1−/− T-cells have increased RA concentrations compared to wild type mouse T-cells. When naïve CD4+ T-cells from T-cell-specific CYP26B1−/− mice and control mice were implanted into a murine model of T-cell dependent intestinal inflammation, inflammation and disease progression were attenuated in the presence of CYP26B1−/− T cells versus control (Chenery et al., 2013). Still, T cell-specific CYP26B1−/− mice had equivalent T-cell development as controls. In addition, IL17a and TNF-α mRNA levels were decreased in the colon of mice with CYP26B1−/− T-cells but Foxp3 mRNA was unaffected by the knock-out. Assuming that CYP26B1 metabolizes RA within the T-cells these findings are consistent with decreased Th17 cells and unaltered Treg cells. The findings in the T-cell specific CYP26B1−/− mice suggest that CYP26B1 plays an important role in modulation of T-cell homeostasis. Surprisingly the expression of RA-inducible homing signals α4β7 and CCR9 was not affected in the T-cell-specific CYP26B1−/− mice (Chenery et al., 2013).
In addition to the mouse T-cell specific CYP26B1−/− model the effect of CYP26B1 polymorphisms on CD and IBD risk was studied (Fransén, Franzén, Magnuson, Elmabsout, Nyhlin, Wickbom, et al., 2013). The CYP26B1 T to C polymorphism (rs2241057) that results in L264S amino acid change displays enhanced catabolic activity compared to the T allele suggesting concentrations of RA may be higher in patients with the T allele (Fransén, Franzén, Magnuson, Elmabsout, Nyhlin, Wickbom, et al., 2013). The frequency of the lower activity T allele was not significantly higher in CD patients compared UC patients or healthy controls. However, atRA concentrations were not measured in this study and no firm relationship between the polymorphism, RA levels and risk of developing CD could be made.
Despite a large volume of data supporting the concept that increasing RA levels would combat IBD, it has also been proposed that increased gut RA levels contribute to IBD pathogenesis. This suggestion is based on the observation that ALDH1A mRNA was increased in intestinal mucosa of CD patients compared to controls. Specifically, ALDH1A1 was predominantly expressed in macrophages from patients and ALDH1A2 was found in DCs (Sanders, McCarthy, Giles, Davidson, Haltalli, Hazell, et al., 2014). While increased ALDH1A mRNA in CD patients suggests that formation of atRA in some or all subsets of antigen presenting cells in intestinal mucosa is increased, altered RA concentrations or increased RA synthesis was not measured in this study. Hence, it is possible that ALDH1A expression is increased in the intestinal mucosa as a compensatory mechanism to low atRA or vitamin A concentrations. Overall further studies that directly measure RA concentrations in IBD and CD are needed to determine the role of atRA signaling in these diseases.
b) Psoriasis
Psoriasis is characterized by an abnormally excessive growth and aberrant differentiation of the epidermal layer of skin. In psoriasis premature maturation of keratinocytes is induced by an inflammatory cascade originating from DCs, macrophages and T-cells (Nestle, Kaplan, & Barker, 2009). The beneficial effect of oral and topical retinoids in psoriasis is well established. In general retinoids have an anti-proliferative effect in epidermal cells if the microenvironment is hyperproliferative and a proliferative effect if the microenvironment is normal (Harper, 1988; Harper & Burgoon, 1982). In normal cells RA stimulates keratinocyte growth and differentiation while in psoriasis RA is anti-proliferative. In psoriasis retinoid treatment decreases cytotoxic T-cell induction, inhibits the chemotactic responses of activated lymphocytes, and inhibits expression of migration inhibitory factor related protein-8 (a marker for hyperproliferation of keratinocytes) resulting in improvement in patient symptoms (DiSepio, Malhotra, Chandraratna, & Nagpal, 1997; Dupuy, Bagot, Heslan, & Dubertret, 1989; van de Kerkhof, 2006).
Similar to RA signaling in gut mucosal immunity, RA signaling is important in the DCs and T-cells in the skin. Similar to DCs in the GALT, DCs in the skin have been shown to express ALDH1A enzymes and to produce RA (Guilliams, Crozat, Henri, Tamoutounour, Grenot, Devilard, et al., 2010). Analogously to the gut mucosa, DCs in the skin were shown to induce Treg cell differentiation and Foxp3 expression in ALDH1A expression dependent manner (Guilliams et al., 2010). Interestingly, in contrast to the DCs in the GALT, DCs in the skin do not induce the gut homing signals such as CCR9 in CD4+ T-cells despite the fact that skin DCs also synthesize RA, demonstrating that gut homing signal generation is specific to GALT DCs (Guilliams et al., 2010; McCully, Ladell, Hakobyan, Mansel, Price, & Moser, 2012).
As in most other cells of the body, retinoid levels in human skin are under tight control. Retinoids are stored in the skin as retinyl esters and RA is produced locally in the epidermis (Fisher & Voorhees, 1996; Pavez Loriè, Li, Vahlquist, & Törmä, 2009). Expression of CYP26A1 has been confirmed in the basal layer of normal and psoriatic human epidermal keratinocytes with immunofluorescence and immunohistochemical staining (Heise et al., 2006). In addition to CYP26A1 another RA metabolizing enzyme, CYP2S1, has been identified in keratinocytes in psoriatic plaques and normal human skin (G. Smith, Ibbotson, Comrie, Dawe, Bryden, Ferguson, et al., 2006) but the quantitative role of CYP2S1 in atRA clearance is not known. Still, the expression of two RA metabolizing enzymes is indicative of the importance of RA homeostasis in skin.
Oral and topical natural and synthetic retinoids have been used in the treatment of psoriasis since the 1970s (S. Dogra & Yadav, 2014; Roos, Jugert, Merk, & Bickers, 1998). While clinical results have been positive, severe side effects such as teratogenicity, hypertriglyceridemia and dermatitis can be dose-limiting. Thus, the use of inhibitors of RA metabolism i.e. RA metabolism blocking agents (RAMBAs) has also been investigated as a means to increase endogenous RA levels in psoriasis and avoid complications from exogenous administration (Verfaille, Borgers, & van Steensel, 2008). Although RAMBAs were originally developed before the identification of CYP26 enzymes, it is now assumed that CYP26s are the primary target of these compounds (Nelson et al., 2013). Treatment of keratinocyte cultures with CYP26 inhibitors, such as talarozole (also known as R115866 or rambazole), has been shown to potentiate cell differentiation effects of RA (Giltaire, Herphelin, Frankart, Herin, Stoppie, & Poumay, 2009). At the same time treatment with RAMBAs induced only CYP26 expression whereas treatment with RA altered multiple enzymes in the retinoid synthesis pathway (Pavez Loriè, Chamcheu, Vahlquist, & Törmä, 2009; G. Smith et al., 2006). These results indicate that inhibition of CYP26 may allow obtaining the same therapeutic benefits as exogenous RA administration without the side effects observed with atRA administration. However, it is not clear how CYP26 inhibitors will affect the immune system and inflammation in the skin.
Clinical studies with CYP26 inhibitors have also been reported in psoriasis. Patients treated with oral ketoconazole, a broad CYP inhibitor that also inhibits CYP26s, had some improvement in their scalp psoriasis. However the trial was discontinued due to concerns of drug toxicity (Farr, Krause, Marks, & Shuster, 1985). A second generation RAMBA, liarozole, was developed with more specific activity towards CYP26, and it was effective in treating psoriasis in early clinical trials (Bhushan, Burden, McElhone, James, Vanhoutte, & Griffiths, 2001; Dockx, Decree, & Degreef, 1995). Further improvement in CYP26 selectivity and potency led to the development of talarozole (Pavez Loriè, Li, et al., 2009). Oral administration of talarozole significantly improved psoriasis symptoms (noted as a reduction in the Psoriasis Area Severity Index or plaque severity) in Phase I and II clinical trials. Increases in plasma concentrations of atRA were observed in a single dose escalation trial of talarozole, but RA concentrations were within or slightly above normal physiological concentrations. Talarozole was well tolerated with no severe side effects noted in Phase I or II studies (Bovenschen, Otero, Langewouters, van Vlijmen-Willems, van Rens, Seyger, et al., 2007; Verfaille, Thissen, Bovenschen, Mertens, Steijlen, & van de Kerkhof, 2007). Additionally, topical treatment with talarozole was shown to increase CRABP2 and keratin 4 and decrease keratin 2 (makers of increased RA activity) in epidermis in healthy volunteers (Pavez Loriè, Cools, Borgers, Wouters, Shroot, Hagforsen, et al., 2009). Collectively these data demonstrate the important role of CYP26 in regulation of RA metabolism in the skin and in psoriasis. Unfortunately, none of the studies with RAMBAs have assessed RA concentrations in the skin or inflammatory markers. Hence it is not possible to determine whether modulation of inflammatory responses also contributes to clinical improvement.
c) Atherosclerosis
Atherosclerosis is a slowly progressing chronic inflammatory disease of blood vessels characterized by accumulation of lipids in the arterial wall (Hansson & Hermansson, 2011; Hansson, Robertson, & Soderberg-Naucler, 2006). Atherosclerosis is a complex disease resulting from multiple risk factors such as excess lipid accumulation, coagulation and fibrosis, cell proliferation and inflammatory cell migration to the inflamed sites. During early stages of atherosclerosis, vascular smooth muscle cells migrate to the intima, promote extracellular matrix deposition and reduce the lumen size (Rhee, Nallamshetty, & Plutzky, 2012). However inflammation, including innate and adaptive immune responses, is involved in all stages of the development of atherosclerosis (Libby, Ridker, & Hansson, 2009; Wiedermann, Chen, Enerbäck, Hanson, Kahu, & Dahlgren, 1996).
RA has diverse biological effects on arterial wall function and plays an important role in the coagulation system. Treatment of human aortic smooth muscle cells with atRA decreased cell proliferation, cell migration to the lumen, and extracellular matrix formation in the lumen (Johst, Betsch, Wiskirchen, Schöber, Vonthein, Rinkert, et al., 2003). Additionally, administration of atRA attenuated pro-coagulant properties, promoted fibrinolysis, reduced the induction of monocytes and tissue factor dependent arterial thrombus formation and suppressed the expression of vasoconstrictor thromboxane A2 in vascular smooth muscle cells (Barstad, Hamers, Stephens, & Sakariassen, 1995; Bulens, Ibanez-Tallon, Van Acker, De Vriese, Nelles, Belayew, et al., 1995; van Giezen, Boon, Jansen, & Bouma, 1993; Watanabe, Kanai, Arai, Sekiguchi, Uchiyama, Nagai, et al., 2002).
Several enzymes involved in retinoid metabolism and action are expressed in the vasculature including alcohol dehydrogenases and RARs (Allali-Hassani, Martinez, Peralba, Vaglenova, Vidal, Richart, et al., 1997; Miano, Topouzis, Majesky, & Olson, 1996), and RAR activity in human smooth muscle cells was confirmed in transient transfected reporter gene assays (Ocaya, Elmabsout, Olofsson, Torma, Gidlof, & Sirsjo, 2011). Of the three CYP26 enzymes, CYP26B1 was found to be constitutively expressed in human vascular smooth cells and play a major role in atRA clearance in the arterial wall (Elmabsout, Kumawat, Saenz-Méndez, Krivospitskaya, Sävenstrand, Olofsson, et al., 2012; Krivospitskaya, Elmabsout, Sundman, Soderstrom, Ovchinnikova, Gidlof, et al., 2012; Ocaya et al., 2011). Based on this, RA may also play a role in regulating other functions in the vasculature. In human atherosclerotic arteries CYP26B1 mRNA expression was increased suggesting that RA concentrations are decreased in atherosclerosis. Murine atherosclerotic model arteries also expressed higher CYP26B1 mRNA than normal arteries (Krivospitskaya et al., 2012). Additionally, based on immunohistochemistry of arterial biopsies from atherosclerotic patients CYP26B1 co-localizes with CD68, a marker for activated macrophages, in atherosclerotic lesions (Krivospitskaya et al., 2012). The accumulation of CYP26B1 expressing macrophages may be the reason for increased CYP26B1 mRNA in the atherosclerotic arteries. When the frequency of the CYP26B1 SNP (L264S) with higher catalytic activity than wild type was tested in atherosclerotic patients and matched controls, no association of the variant allele expression between patients and matched controls and basic clinical characteristics was detected. However, patients who carried the minor allele variant and may have lower levels of atRA had a small increase in atherosclerotic lesion size (Krivospitskaya et al., 2012). Expression of CYP26B1 and RARβ was enhanced in in human aortic smooth muscle cells treated with atRA alone or with talarozole and atRA (Ocaya et al., 2011). Talarozole together with atRA treatment also increased cellular atRA concentrations and decreased DNA synthesis and cell proliferation compared to cells treated with atRA alone. In addition, transfection with CYP26B1 siRNA led to increased atRA-mediated RAR/RXR signaling.
IV. CYP26 and Retinoic Acid in Cancer
Vitamin A and RA play a crucial role in regulating cell proliferation, differentiation and apoptosis, and as early as 1925 an association between vitamin A deficiency and carcinogenesis was suggested (Wolbach & Howe, 1925). Subsequent epidemiological, preclinical and clinical studies established a relationship between vitamin A deficiency and a higher incidence of carcinogenesis in both humans and rodents (Basu, Temple, & Hodgson, 1988; Chaudhy, Jafarey, & Ibrahim, 1980; S. C. Dogra, Khanduja, & Gupta, 1985; Ito, Gajalakshmi, Sasaki, Suzuki, & Shanta, 1999; Stehr, Gloninger, Kuller, Marsh, Radford, & Weinberg, 1985). In addition, abnormal RA metabolism potentially leading to altered RA levels has also been implicated in tumorigenesis (Moulas, Gerogianni, Papadopoulos, & Gourgoulianis, 2006; Osanai & Petkovich, 2005).
Altered expression of proteins controlling RA concentrations has been associated with multiple cancers but changes in RA concentrations have not been directly measured in cancers. Significantly higher activity of alcohol dehydrogenase enzymes has been shown in breast, ovarian, colorectal, and cervical cancer tissues compared to healthy human tissues (Jelski, Chrostek, Szmitkowski, & Markiewicz, 2006; Jelski, Zalewski, Chrostek, & Szmitkowski, 2004; Orywal, Jelski, Zdrodowski, & Szmitkowski, 2011, 2013). ALDH1A3 expression was also high in breast cancer tissues and ALDH1A3 levels significantly correlated with distant metastasis (Qiu, Pu, Li, Cheng, Lu, Sun, et al., 2014). Further, ALDH1A1 expression was observed in 63.0% (92 of 146) of human breast invasive ductal carcinoma tissues (Zhong, Lin, Shen, Zhou, Mao, Guan, et al., 2013). It is possible that increases in alcohol dehydrogenase and ALDH enzymes will lead to increased RA concentrations. However, it is also possible that low RA concentrations in cancer prevent RA-mediated regulation of these enzymes or that alcohol dehydrogenase and ALDH1A enzymes are increased in an attempt to correct low RA concentrations in cancer.
The role of the retinol transport proteins RBP and STRA6 in cancer development and progression is still unclear. In human breast and colon cancers STRA6 and RBP mRNA levels were elevated in comparison to normal breast and colon tissue, and higher expression of STRA6 and RBP correlated with oncogenic properties and tumor progression suggesting an oncogenic role of STRA6 (Berry et al., 2014). In agreement, binding of holo-RBP4 (RBP4-ROH) to STRA6 was shown to trigger phosphorylation of STAT3, resulting in recruitment and activation of JAK/STAT pathway and increased oncogenic properties in tumor cell lines (Berry et al., 2014). In contrast, in human keratinocytes, knockdown of STRA6 was shown to increase keratinocyte proliferation and lead to thickening of the epidermal layer and increased proliferation (Skazik, Amann, Heise, Marquardt, Czaja, Kim, et al., 2014). Similarly, increased expression of STRA6 increased apoptosis in normal and cancer cells and influenced p53-mediated apoptosis in bladder, ovarian and colon cancer cell lines (Carrera, Cuadrado-Castano, Samuel, Jones, Villar, Lee, et al., 2013). Overall, the findings are controversial and further work is needed to determine how STRA6 expression and RA signaling affect cancer development and oncogenesis. Additionally, down regulation or loss of CRBP-1, which regulates retinoid uptake, intracellular availability and metabolism, has been shown in both human breast and ovarian cancer (Cvetković, Williams, & Hamilton, 2003; Kuppumbatti, Bleiweiss, Mandeli, Waxman, & Mira-Y-Lopez, 2000). Together these studies show that proteins controlling RA signaling play an important role in many cancers.
Increased expression of CYP26 enzymes in cancers, such as breast, colorectal, and head and neck cancers has recently been shown in several studies (Brown, Cash, Blihoghe, Johansson, Alnabulsi, & Murray, 2014; Osanai & Lee, 2014; Osanai, Sawada, & Lee, 2009). Elevated CYP26 levels in cancer tissue resulting in RA deficiency have also been linked to carcinogenesis in epidemiological studies (Berlin Grace, Niranjali Devaraj, Radhakrishnan Pillai, & Devaraj, 2006; Moulas et al., 2006). CYP26A1 was shown to be highly expressed in 42% (27/65) of surgically resected breast cancer specimens (Osanai et al., 2014). CYP26A1 expression was significantly higher in metastatic carcinomas (n=10) than in normal breast tissue suggesting that high expression of CYP26A1 is associated with decreased disease-free and overall survival in breast cancer (Osanai et al., 2014). Similarly, CYP26A1 and CYP26B1 expression was significantly increased in primary colorectal cancer compared with normal colonic mucosa (Brown et al., 2014), and CYP26A1 expression was significantly higher in sporadic human colon tumor samples than in normal tissues (Shelton, Sandoval, Eisinger, Chidester, Ratnayake, Ireland, et al., 2006). In addition to breast and colorectal cancer, CYP26A1 overexpression might also contribute to the development and progression of cervical malignancies and squamous neoplasia of the head and neck. For example, strong expression of CYP26A1 was observed in 19 of 50 (38%) cervical squamous cell carcinoma cases but no expression was found in normal cervical epithelium. In addition, strong expression of CYP26A1 was shown in 52 of 128 (41%) head and neck cancer cases with no CYP26A1 expressed in non-neoplastic tissues of the head and neck (Osanai et al., 2014). In Barrett’s carcinogenesis a significant up-regulation of CYP26A1 was observed in adenocarcinoma compared to non-dysplastic Barrett’s tissues (Chang, Hong, Lao-Sirieix, & Fitzgerald, 2008). Finally, CYP26A1 expression was significantly enhanced in primary ovarian cancers in comparison to normal ovarian tissue (Downie, McFadyen, Rooney, Cruickshank, Parkin, Miller, et al., 2005). While these studies show that CYP26 expression is elevated in various types of cancer, the underlying mechanism resulting in elevated CYP26 expression in human cancers and the exact role of CYP26 in carcinogenesis has not been fully clarified.
In vitro studies with CYP26 transfection to induce overexpression of CYP26 have been conducted and offer insights into the role of CYP26 in carcinogenesis (Chang et al., 2008; Xia et al., 2010). Increases in anti-apoptotic signals and oncogenes (e.g., epidermal growth factor receptor and c-Myc) were observed in dysplastic Barrett’s cells transfected with CYP26A1 in comparison to control cells. Cells overexpressing CYP26A1 also exhibited increased proliferation (Chang et al., 2008). In addition, down regulation of p53, an apoptotic signal and tumor suppressor gene was found following overexpression of CYP26A1 in endometrial stromal cells (Xia et al., 2010). Based on these studies, use of RAMBAs to inhibit CYP26A1 and increase tumor RA levels is being pursued as a drug target in cancer (Nelson et al., 2013).
Efforts to synthesize RAMBAs with increased potency and favorable pharmacokinetics that selectively inhibit CYP26s are ongoing in several laboratories and details of these compounds can be found in several recent reviews (Nelson et al., 2013; Njar, Gediya, Purushottamachar, Chopra, Vasaitis, Khandelwal, et al., 2006). These CYP26 inhibitors could potentially be used alone to increase RA concentrations or in combination with RA treatment to combat resistance to treatment and increase potency of RA. Preclinical and early clinical data for CYP26 inhibitors is promising (Godbole, Purushottamachar, Martin, Daskalakis, & Njar, 2012; Gomaa, Bridgens, Veal, Redfern, Brancale, Armstrong, et al., 2011). Of the well-studied RAMBAs, liarozole, an inhibitor of CYP26 (IC50 2.2–6.0 μM), reduced tumor growth in androgen-dependent and androgen-independent rat prostate carcinoma models. Liarozole also decreased risk of death compared to cyproterone acetate in patients with metastatic prostate cancer in relapse after first-line endocrine therapy (Njar et al., 2006; Stearns, Wang, & Fudge, 1993). Another CYP26 inhibitor R116010, a benzothiazolamine, inhibited atRA metabolism in intact T47D human breast cancer cells with an IC50 value of 8.7 nM (Van Heusden, Van Ginckel, Bruwiere, Moelans, Janssen, Floren, et al., 2002).
a) Acute promyelocytic leukemia
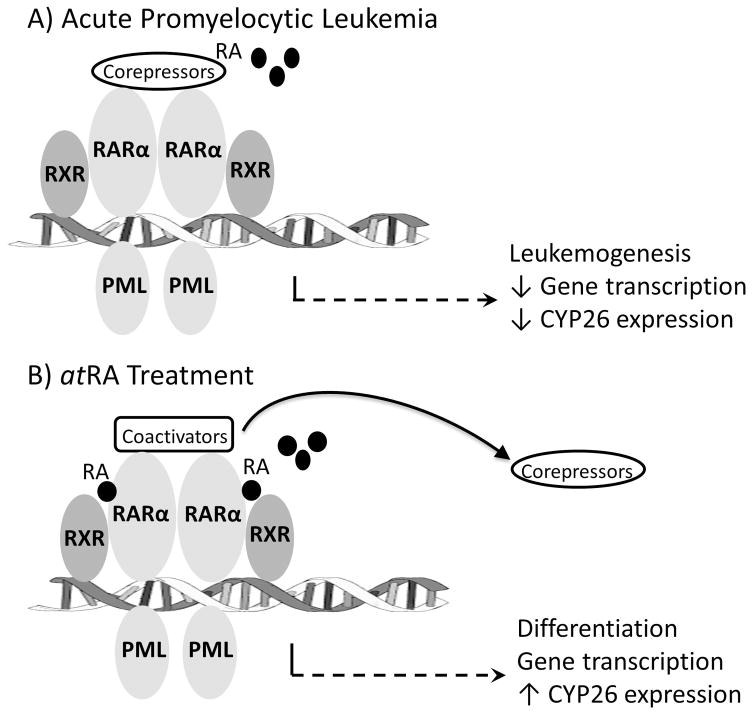
Leukemia results from an uncontrolled increase in the number of immature white blood cells. A rare subset of leukemia, acute promyelocytic leukemia (APL), is definitively marked by a chromosomal translocation affecting the RARα gene (Martens, Brinkman, Simmer, Francoijs, Nebbioso, Ferrara, et al., 2010). The predominant translocation, occurring in 90–95% of APL patients, is t(15; 17) where chromosome 15 maps to the promyelocytic leukemia gene (PML) and chromosome 17 to the RARα gene (Kakizuka, Miller Jr., Umesono, Warrell Jr., Frankel, Murty, et al., 1991; Orfali, McKenna, Cahill, Gudas, & Mongan, 2014). The t(15;17) translocation ultimately results in a PML-RARα fusion protein (Guidez, Ivins, Zhu, Söderström, Waxman, & Zelent, 1998; Kakizuka et al., 1991; Pandolfi, Grignani, Alcalay, Mencarelli, Biondi, LoCoco, et al., 1991), which binds with RXR to the retinoic acid response element of target genes (Martens et al., 2010) ultimately blocking myeloid differentiation and leading to leukemogenesis (Collins, 2002; Guidez et al., 1998) (Figure 4). With wild type RARα, physiological levels of atRA are sufficient to dissociate negative co-repressors but PML-RARα fusion proteins are less sensitive to atRA and pharmacological levels of atRA are required to dissociate negative co-repressors from the fusion protein for gene transcription and terminal myeloid differentiation (Guidez et al., 1998).
Figure 4. Retinoic acid and CYP26 signaling in acute promyelocytic leukemia.
In acute promyelocytic leukemia a chromosomal translocation forms the PML-RARα fusion protein which binds DNA as either a homodimer or multimeric complex with RXR. A) Physiological levels of the signaling molecule, RA, are insufficient to bind and promote release of corepressors from the complex which blocks gene transcription (including the gene for CYP26) and promotes leukemogenesis. B) Pharmacological levels of atRA bind the receptor, cause release of corepressors and recruit activators for gene transcription ultimately resulting in terminal myeloid differentiation.
Treatment of APL with atRA began in the 1980s and remains standard of care to date (Huang, Ye, Chen, Chai, Lu, Zhoa, et al., 1988; Watts & Tallman, 2014). atRA treatment causes terminal myeloid differentiation, degradation of the fusion protein and autophagy of APL blasts. APL is highly curable with approximately 90% complete remission following frontline therapy with atRA in combination with either anthracycline-based chemotherapy or arsenic trioxide (Tallman & Altman, 2009; Watts et al., 2014). However, despite the high remission rates with front-line treatment of APL, relapse occurs in 10–30% of patients (Idres, Marill, & Chabot, 2005; Kelaidi, Ades, Chevret, Sanz, Guerci, Thomas, et al., 2006). Several factors have been proposed to contribute to the relapse in APL patients, including mutations of the PML-RARα fusion protein blocking transcriptional activation, increased binding affinity of co-repressors to the fusion protein, and increased atRA metabolism due to induction of CYP26 (Guidez et al., 1998; Idres et al., 2005). Auto-induction of atRA metabolism and resulting resistance to atRA is the best characterized mechanism of APL relapse. In clinical pharmacokinetic studies in APL patients exposure to atRA was significantly decreased at relapse when compared to exposure after the first dose (Muindi, Frankel, Miller, Jakubowski, Scheinberg, Young, et al., 1992). Doubling the clinical dose of atRA at relapse was insufficient to match initial atRA exposures. Blasts cells were collected from patients at relapse and were sensitive in vitro to atRA differentiation and maintained the PML-RARα fusion protein indicating that decreased systemic exposure to atRA was the root cause of relapse. The authors proposed that auto-induction of a CYP enzyme responsible for atRA metabolism occurred with prolonged treatment with atRA (Muindi et al., 1992). This proposal was further confirmed by the observation that pretreatment with fluconazole, an inhibitor of CYP enzymes, caused over 4-fold increase in atRA AUC in APL patients (Schwartz, Hallam, Gallagher, & Wiernik, 1995). After identification of CYP26 as the atRA hydroxylase, atRA treatment was shown to induce CYP26 mRNA in APL patient derived model cell lines (NB4 and HL-60) (Idres et al., 2005; Ozpolat, Mehta, & Lopez-Berestein, 2005; Ozpolat, Mehta, Tari, & Lopez-Berestein, 2002). Basal CYP26 expression in NB4 cells is very low but mRNA levels can be induced up to 22-fold following 24 – 96 hours of treatment with pharmacologically relevant concentrations of atRA. Furthermore, atRA binding to the RARα nuclear receptor was shown to mediate CYP26 induction (Idres et al., 2005; Ozpolat et al., 2002; Roussel & Lanotte, 2001). These findings support the notion that therapeutic CYP26 inhibition may circumvent APL relapse following atRA treatment by preventing rapid metabolism of atRA due to increased expression of CYP26.
An alternative hypothesis for APL relapse was investigated by Quere et al., in blasts from atRA treatment-naïve APL patients. Blast cells were harvested from patients and treated in vitro with atRA for three days. Blasts with delayed maturation, marked as fewer than 50% differentiated cells on day 3, were associated with poor clinical prognosis and categorized as having low-sensitivity to atRA treatment. Blasts with rapid maturation, defined as greater than 50% differentiated cells following 3 days of in vitro incubation with atRA, were associated with significantly improved disease free survival clinically and therefore categorized as highly-sensitive to atRA treatment. In the two classes of blasts, higher transcription of atRA target genes, transcriptional regulators and chromatin remodelers was observed in low-sensitive cells. Conversely, CYP26 gene expression was limited to highly-sensitive blasts with little to no expression observed in low-sensitive blasts. The authors proposed that low expression of CYP26 in APL blasts with low-sensitivity to atRA in vitro led to increased nuclear atRA concentrations and corresponding increased atRA-target gene transcription. Further, when NB4 cells were incubated with either atRA or the CYP26 inhibitor 4-azolyl retinoic acid, accumulation of atRA and development of subclones resistant to atRA-induced differentiation were observed following NB4 cell treatment with 4-azolyl retinoic acid (Quere, Baudet, Cassinat, Bertrand, Marti, Manchon, et al., 2007). While this conflicting data of mechanisms of resistance remain to be resolved, it appears that the activity of CYP26 in regulating nuclear atRA levels is important in preventing APL relapse. Indeed, CYP26-specific RAMBAs have been developed and investigated preclinically but no clinical studies have yet shown the effects of coadministration of atRA and a RAMBA in APL (Li, Zhao, Ren, Hao, Liu, Jin, et al., 2013; Njar et al., 2006). Several other strategies have been proposed to address atRA-resistance and APL relapse. Intermittent dosing of atRA combined with chemotherapy is used in standard APL therapy during consolidation and maintenance. A significantly lower 2-year relapse rate was reported in patients receiving intermittent atRA compared to patients without atRA treatment during maintenance (Fenaux, Wang, & Degos, 2007).
b) Neuroblastoma
Neuroblastoma is a malignant tumor comprised of neuroblasts. It develops most commonly in the abdomen, but also appears in the neck, chest, and pelvis. Neuroblastoma is the most common extracranial solid tumor in childhood and accounts for 15% of oncology deaths in patients younger than 15 years (Maris, Hogarty, Bagatell, & Cohn, 2007). Treatment of neuroblastoma is based on disease risk stratification and can include surgery alone or chemotherapy and autologous bone marrow transplant. Treatment with 13-cisRA significantly improves overall survival of high risk patients when used following transplantation or chemotherapy (Maris et al., 2007; Matthay, Reynolds, Seeger, Shimada, Adkins, Haas-Kogan, et al., 2009; Matthay, Villablanca, Seeger, Stram, Harris, Ramsay, et al., 1999). In neuroblastoma cell lines, 13-cisRA and atRA have similar potency on cellular differentiation and growth arrest (Reynolds, Schindler, Jones, Gentile, Proffitt, & Einhorn, 1994) but 13-cisRA is superior to atRA in the treatment of neuroblastoma due to its favorable pharmacokinetic and toxicological properties (Reynolds, Matthay, Villablanca, & Maurer, 2003).
Disease relapse is common in neuroblastoma. One approach to improve clinical outcomes is identifying an optimal dosing regimen of 13-cisRA. Intermittent high dose administration of 13-cisRA improved clinical outcomes when compared to chronic low-dose administration but significant variability in 13-cisRA exposures was still observed causing suboptimal concentrations in some patients (Matthay, 2013; Matthay et al., 2009; Villablanca, Khan, Avramis, Seeger, Matthay, Ramsay, et al., 1995). Polymorphisms in several enzymes that clear 13-cis-RA such as CYP2C8, CYP3A5, CYP3A7 and UGT2B1 have been studied as the cause of variability in 13-cisRA exposures. 4-oxo-13-cisRA is the major 13-cisRA metabolite observed in neuroblastoma patients. While 4-oxo-13-cisRA exposure was associated with CYP2C8 and CYP3A7 polymorphisms, variability in 13-cisRA exposure and 13-cisRA:4-oxo-13-cisRA ratio could not be attributed to any of the polymorphisms investigated (Veal, Errington, Rowbotham, Illingworth, Malik, Cole, et al., 2013). It is reasonable to suggest that CYP26 plays a role in the metabolism of 13-cisRA since CYP26 is the major catabolic enzyme of atRA and isomerization between atRA and 13-cisRA has been observed (Tsukada, Schröder, Roos, Chandraratna, Reichert, Merk, et al., 2000).
Given that 13-cisRA is generally considered to be devoid of biological activity due to its low affinity for RARs, neuroblastoma cellular differentiation and growth arrest in response to 13-cisRA treatment (Reynolds et al., 2003) can be attributed to isomerization of 13-cisRA to atRA. However, this has not been directly proven. Determination of retinoid levels following treatment of neuroblastoma cell lines with 13-cisRA revealed little extracellular atRA but increased intracellular atRA due to either intracellular isomerization or selective uptake of atRA (Veal, Errington, Redfern, Pearson, & Boddy, 2002). Furthermore, incubation with 13-cisRA alone in neuroblastoma cell lines resulted in atRA accounting for 15–31% of the total RA. In contrast, after incubation with atRA, 13-cisRA accounted for <10% of total RA (Armstrong, Taylor, Thomas, Boddy, Redfern, & Veal, 2007). Intracellular atRA concentrations but not 13-cisRA concentrations were increased in neuroblastoma cell lines following administration of the CYP26 inhibitor R116010 following either atRA or 13-cisRA treatment (Armstrong, Ruiz, Boddy, Redfern, Pearson, & Veal, 2005; Armstrong et al., 2007). This suggests that coadministration of a CYP26 inhibitor may improve clinical outcomes in neuroblastoma patients with low, sub-therapeutic 13-cisRA concentrations. Surprisingly and in contrast to preclinical results, overexpression of the CYP26A1 gene in neuroblastoma tumors from over 100 patients was found to be significantly associated with favorable clinical outcomes (Kamei, Hiyama, Yamaoka, Kamimatsuse, Onitake, Sueda, et al., 2009). However, no concentrations of atRA or 13-cisRA were reported in this study. It is possible that higher CYP26A1 expression in the neuroblastoma tumors in clinical samples is indicative of higher RA exposure upon treatment as CYP26A1 is induced by RA. Collectively, these findings highlight the need for more investigation of the concentrations of RA in neuroblastoma and the effects of altered RA exposures to disease outcomes.
V. Conclusions
There is considerable evidence that RA plays an important role in modulating innate and adaptive immunity and inflammation, and studies in various disease models suggest that increasing atRA concentrations will be beneficial in inflammatory diseases. The most important role of atRA in the immune system is perhaps inducing T-cell differentiation to Treg cells and suppressing T-cell differentiation to Th17 cells. This activity is also likely important for the anti-inflammatory actions of atRA. In addition, RA has a critical role in inducing the gut homing signals in T-cells. It is not clear how altered expression of RA synthesizing and metabolizing enzymes modulates RA concentrations in various immune cells, but there is emerging evidence that CYP26B1 is the predominant enzyme clearing RA in the T- and B-cells and ALDH1A2 appears to be mainly responsible for synthesizing RA in these cells and in DCs. Therefore alterations in the activity of these enzymes are expected to affect immune homeostasis. However, whether the expression of these enzymes varies dynamically with immune responses and in inflammation is not known. Thus the endogenous roles of CYP26s and ALDHs in immune modulation are not yet established. It is important to note that endogenous RA is generally synthesized within target cells and RA signaling appears to be modulated by highly specific gradients of RA concentrations (Hogarth, Arnold, Kent, Mitchell, Isoherranen, & Griswold, 2015). In contrast, when RA is administered exogenously for pharmacological studies RA gradients are not necessarily generated which may confound the mechanistic information obtained in regards of the endogenous regulatory systems and the role of RA in inflammatory processes.
atRA and its stereoisomer 13-cisRA are useful therapeutic agents in the treatment of APL and neuroblastoma, respectively. However, resistance to RA treatment is observed in both diseases and appears to involve induction of the CYP26 enzymes, likely CYP26A1, and increased clearance of RA. Therefore inhibition of the CYP26s in these cancers is predicted to improve therapy outcomes. However, some of the mechanistic data of resistance development is controversial and challenging to interpret, as RA induces CYP26 expression but CYP26s also clear RA and likely reduce its concentrations in target cells. Several studies have also suggested that RA signaling and aberrant synthesis and metabolism of RA play a role in other cancers such as breast, prostate, head and neck, colorectal and ovarian cancers. In many in vitro models of these cancers increased expression of CYP26A1 appears to promote tumorigenesis while increased concentrations of RA induce apoptotic pathways. Yet, evidence from animal and human studies is incomplete to demonstrate that altered CYP26A1 expression will cause cancer or contribute to cancer development. In addition, it has not been directly shown that RA concentrations are altered in cancer simultaneously with increased CYP26 expression in malignant cells.
Overall it appears that increasing RA concentrations via inhibition of CYP26 enzymes will have many positive effects in inflammatory diseases such as IBD, psoriasis and atherosclerosis and in various cancers by promoting apoptosis and cell cycle arrest. However, potent inhibitors of CYP26 enzymes that have suitable in vivo pharmacokinetics to use in disease models or humans have not yet been developed or approved. Therefore the effect of altered RA homeostasis and the magnitude of required change in RA concentrations to have therapeutic benefit are not well defined. While many of the beneficial effects on the immune system and cancer appear to be associated with increasing RA concentrations, in many other situations, such as fetal development, both too high and too low RA concentrations are detrimental and manifest themselves with similar phenotypes. This may in part explain some of the controversies observed in different inflammatory diseases and cancers and may affect future strategies for development of therapies relating to retinoids.
Acknowledgments
This work was supported in part by an NIH NIGMS grant R01 GM111772.
Nonstandard abbreviations
- 13-cisRA
13-cis-retinoic acid
- 9-cisRA
9-cis-retinoic acid
- ALDH
aldehyde dehydrogenase
- APL
acute promyelocytic leukemia
- atRA
all-trans-retinoic acid
- BCDO2
β,β-carotene-9,10-dioxygenase 2
- BCMO1
β,β-carotene-15,15′-monooxygenase 1
- CD
Crohn’s disease
- CRABP
cellular retinoic acid binding protein
- CRBP
cellular retinol binding protein
- CYP26
cytochrome P450 family 26
- DC
dendritic cell
- ER
endoplasmic reticulum
- FABP
fatty acid binding protein
- GALT
gut-associated lymphoid tissue
- IBD
inflammatory bowel disease
- LRAT
lecithin retinol acyltransferase
- NAFLD
non-alcoholic fatty liver disease
- NASH
non-alcoholic steatohepatitis
- PML
promyelocytic leukemia gene
- PPAR
peroxisome proliferator-activated receptor
- RA
retinoic acid
- RAMBA
retinoic acid metabolism blocking agent
- RAR
retinoic acid receptor
- RBP
retinol binding protein
- RDH1
retinol dehydrogenase 1
- REH
retinyl ester hydrolase
- RXR
retinoid X receptor
- UC
ulcerative colitis
Footnotes
Conflict of interest statement: The authors have no conflicts of interest to declare.
References
- Abella V, Scotece M, Conde J, López V, Lazzaro V, Pino J, Gómez-Reino JJ, Gualillo O. Adipokines, metabolic syndrome and rheumatic diseases. Journal of Immunology Research. 2014;2014:343746. doi: 10.1155/2014/343746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abu-Abed S, Dollé P, Metzger D, Beckett B, Chambon P, Petkovich M. The retinoic acid-metabolizing enzyme, CYP26A1, is essential for normal hindbrain patterning, vertebral identity, and development of posterior structures. Genes & Development. 2001;15:226–240. doi: 10.1101/gad.855001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahluwalia B, Gambhir K, Sekhon H. Distribution of labeled retinyl acetate and retinoic acid in rat and human testes. A possible site of retinyl acetate incorporation in rat testes. The Journal of Nutrition. 1975;105:467–474. doi: 10.1093/jn/105.4.467. [DOI] [PubMed] [Google Scholar]
- Allali-Hassani A, Martinez SE, Peralba JM, Vaglenova J, Vidal F, Richart C, Farrés J, Parés X. Alcohol dehydrogenase of human and rat blood vessels. Role in ethanol metabolism. FEBS Letters. 1997;405:26–30. doi: 10.1016/s0014-5793(97)00151-8. [DOI] [PubMed] [Google Scholar]
- Altucci L, Leibowitz MD, Ogilvie KM, de Lera AR, Gronemeyer H. RAR and RXR modulation in cancer and metabolic disease. Nature Reviews. Drug Discovery. 2007;6:793–810. doi: 10.1038/nrd2397. [DOI] [PubMed] [Google Scholar]
- Ambroziak W, Izaguirre G, Pietruszko R. Metabolism of Retinaldehyde and Other Aldehydes in Soluble Extracts of Human Liver and Kidney. Journal of Biological Chemistry. 1999;274:33366–33373. doi: 10.1074/jbc.274.47.33366. [DOI] [PubMed] [Google Scholar]
- Armstrong JL, Ruiz M, Boddy AV, Redfern CPF, Pearson ADJ, Veal GJ. Increasing the intracellular availability of all-trans retinoic acid in neuroblastoma cells. British Journal of Cancer. 2005;92:696–704. doi: 10.1038/sj.bjc.6602398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong JL, Taylor GA, Thomas HD, Boddy AV, Redfern CPF, Veal GJ. Molecular targeting of retinoic acid metabolism in neuroblastoma: the role of the CYP26 inhibitor R116010 in vitro and in vivo. British Journal of Cancer. 2007;96:1675–1683. doi: 10.1038/sj.bjc.6603779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold SL, Kent T, Hogarth CA, Schlatt S, Prasad B, Haenisch M, Walsh T, Muller CH, Griswold MD, Amory JK, Isoherranen N. Importance of ALDH1A enzymes in determining human testicular retinoic acid concentrations. Journal of Lipid Research. 2015;56:342–357. doi: 10.1194/jlr.M054718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold SLM, Amory JK, Walsh TJ, Isoherranen N. A sensitive and specific method for measurement of multiple retinoids in human serum with UHPLC-MS/MS. Journal of Lipid Research. 2012;53:587–598. doi: 10.1194/jlr.D019745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold SLM, Kent T, Hogarth CA, Griswold MD, Amory JK, Isoherranen N. Pharmacological inhibition of ALDH1A in mice decreases all-trans retinoic acid concentrations in a tissue specific manner. Biochemical Pharmacology. 2015 doi: 10.1016/j.bcp.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashla AA, Hoshikawa Y, Tsuchiya H, Hashiguchi K, Enjoji M, Nakamuta M, Taketomi A, Maehara Y, Shomori K, Kurimasa A, Hisatome I, Ito H, Shiota G. Genetic analysis of expression profile involved in retinoid metabolism in non-alcoholic fatty liver disease. Hepatology Research. 2010;40:594–604. doi: 10.1111/j.1872-034X.2010.00646.x. [DOI] [PubMed] [Google Scholar]
- Aström A, Pettersson U, Krust A, Chambon P, Voorhees JJ. Retinoic acid and synthetic analogs differentially activate retinoic acid receptor dependent transcription. Biochemical and Biophysical Research Communications. 1990;173:339–345. doi: 10.1016/s0006-291x(05)81062-9. [DOI] [PubMed] [Google Scholar]
- Bai A, Lu N, Guo Y, Liu Z, Chen J, Peng Z. All-trans retinoic acid down-regulates inflammatory responses by shifting the Treg/Th17 profile in human ulcerative and murine colitis. Journal of Leukocyte Biology. 2009;86:959–969. doi: 10.1189/jlb.0109006. [DOI] [PubMed] [Google Scholar]
- Barstad RM, Hamers MJ, Stephens RW, Sakariassen KS. Retinoic acid reduces induction of monocyte tissue factor and tissue factor/factor VIIa-dependent arterial thrombus formation. Blood. 1995;86:212–8. [PubMed] [Google Scholar]
- Basu TK, Temple NJ, Hodgson AM. Vitamin A, beta-carotene and cancer. Progress in Clinical and Biological Research. 1988;259:217–228. [PubMed] [Google Scholar]
- Berlin Grace VM, Niranjali Devaraj S, Radhakrishnan Pillai M, Devaraj H. HPV-induced carcinogenesis of the uterine cervix is associated with reduced serum ATRA level. Gynecologic Oncology. 2006;103:113–119. doi: 10.1016/j.ygyno.2006.01.057. [DOI] [PubMed] [Google Scholar]
- Berry DC, Levi L, Noy N. Holo-retinol-binding protein and its receptor STRA6 drive oncogenic transformation. Cancer Research. 2014;74:6341–6351. doi: 10.1158/0008-5472.CAN-14-1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhushan M, Burden AD, McElhone K, James R, Vanhoutte FP, Griffiths CE. Oral liarozole in the treatment of palmoplantar pustular psoriasis: a randomized, double-blind, placebo-controlled study. The British Journal of Dermatology. 2001;145:546–553. doi: 10.1046/j.1365-2133.2001.04411.x. [DOI] [PubMed] [Google Scholar]
- Bonet ML, Ribot J, Palou A. Lipid metabolism in mammalian tissues and its control by retinoic acid. Biochimica Et Biophysica Acta. 2012;1821:177–189. doi: 10.1016/j.bbalip.2011.06.001. [DOI] [PubMed] [Google Scholar]
- Bovenschen HJ, Otero ME, Langewouters AMG, van Vlijmen-Willems IMJJ, van Rens DWA, Seyger MMB, van de Kerkhof PCM. Oral retinoic acid metabolism blocking agent Rambazole for plaque psoriasis: an immunohistochemical study. The British Journal of Dermatology. 2007;156:263–270. doi: 10.1111/j.1365-2133.2006.07660.x. [DOI] [PubMed] [Google Scholar]
- Brown GT, Cash BG, Blihoghe D, Johansson P, Alnabulsi A, Murray GI. The expression and prognostic significance of retinoic acid metabolising enzymes in colorectal cancer. PloS One. 2014;9:e90776. doi: 10.1371/journal.pone.0090776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SJ, Mayer L. The Immune Response in Inflammatory Bowel Disease. The American Journal of Gastroenterology. 2007;102:2058–2069. doi: 10.1111/j.1572-0241.2007.01343.x. [DOI] [PubMed] [Google Scholar]
- Bulens F, Ibanez-Tallon I, Van Acker P, De Vriese A, Nelles L, Belayew A, Collen D. Retinoic acid induction of human tissue-type plasminogen activator gene expression via a direct repeat element (DR5) located at -7 kilobases. Journal of Biological Chemistry. 1995;270:7167–75. doi: 10.1074/jbc.270.13.7167. [DOI] [PubMed] [Google Scholar]
- Cantorna MT, Nashold FE, Hayes CE. Vitamin A deficiency results in a priming environment conducive for Th1 cell development. European Journal of Immunology. 1995;25:1673–1679. doi: 10.1002/eji.1830250629. [DOI] [PubMed] [Google Scholar]
- Carrera S, Cuadrado-Castano S, Samuel J, Jones GDD, Villar E, Lee SW, Macip S. Stra6, a retinoic acid-responsive gene, participates in p53-induced apoptosis after DNA damage. Cell Death and Differentiation. 2013;20:910–919. doi: 10.1038/cdd.2013.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang CL, Hong E, Lao-Sirieix P, Fitzgerald RC. A novel role for the retinoic acid-catabolizing enzyme CYP26A1 in Barrett’s associated adenocarcinoma. Oncogene. 2008;27:2951–2960. doi: 10.1038/sj.onc.1210969. [DOI] [PubMed] [Google Scholar]
- Chaudhy NA, Jafarey NA, Ibrahim K. Plasma vitamin A and carotene levels in relation to the clinical stages of carcinoma of the oral cavity and oropharynx. JPMA. The Journal of the Pakistan Medical Association. 1980;30:221–223. [PubMed] [Google Scholar]
- Chenery A, Burrows K, Antignano F, Underhill TM, Petkovich M, Zaph C. The retinoic acid-metabolizing enzyme Cyp26b1 regulates CD4 T cell differentiation and function. PloS One. 2013;8:e72308. doi: 10.1371/journal.pone.0072308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H, Juchau MR. Glutathione S-transferases act as isomerases in isomerization of 13-cis-retinoic acid to all-trans-retinoic acid in vitro. Biochemical Journal. 1997;327:721–726. doi: 10.1042/bj3270721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen WC, Sass JO, Seltmann H, Nau H, Orfanos CE, Zouboulis CC. Biological effects and metabolism of 9-cis-retinoic acid and its metabolite 9,13-di-cis-retinoic acid in HaCaT keratinocytes in vitro: comparison with all-trans-retinoic acid. Archives of Dermatological Research. 2000;292:612–620. doi: 10.1007/s004030000189. [DOI] [PubMed] [Google Scholar]
- Chung SSW, Wolgemuth DJ. Role of retinoid signaling in the regulation of spermatogenesis. Cytogenetic and Genome Research. 2004;105:189–202. doi: 10.1159/000078189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chytil F. The lungs and vitamin A. The American Journal of Physiology. 1992;262:L517–527. doi: 10.1152/ajplung.1992.262.5.L517. [DOI] [PubMed] [Google Scholar]
- Collins S. The role of retinoids and retinoic acid receptors in normal hematopoiesis. Leukemia. 2002:16. doi: 10.1038/sj.leu.2402718. Published Online: 25 September 2002. [DOI] [PubMed] [Google Scholar]
- Cvetković D, Williams SJ, Hamilton TC. Loss of cellular retinol-binding protein 1 gene expression in microdissected human ovarian cancer. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 2003;9:1013–1020. [PubMed] [Google Scholar]
- D’Ambrosio DN, Clugston RD, Blaner WS. Vitamin A Metabolism: An Update. Nutrients. 2011;3:63–103. doi: 10.3390/nu3010063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bruijn DR, Oerlemans F, Hendriks W, Baats E, Ploemacher R, Wieringa B, Geurts van Kessel A. Normal development, growth and reproduction in cellular retinoic acid binding protein-I (CRABPI) null mutant mice. Differentiation; Research in Biological Diversity. 1994;58:141–148. doi: 10.1046/j.1432-0436.1995.5820141.x. [DOI] [PubMed] [Google Scholar]
- De Pee S, Dary O. Biochemical indicators of vitamin A deficiency: serum retinol and serum retinol binding protein. The Journal of Nutrition. 2002;132:2895S–2901S. doi: 10.1093/jn/132.9.2895S. [DOI] [PubMed] [Google Scholar]
- Depner CM, Philbrick KA, Jump DB. Docosahexaenoic Acid Attenuates Hepatic Inflammation, Oxidative Stress, and Fibrosis without Decreasing Hepatosteatosis in a Ldlr−/− Mouse Model of Western Diet-Induced Nonalcoholic Steatohepatitis. The Journal of Nutrition. 2013;143:315–323. doi: 10.3945/jn.112.171322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiSepio D, Malhotra M, Chandraratna RA, Nagpal S. Retinoic acid receptor- nuclear factor-interleukin 6 antagonism. A novel mechanism of retinoid-dependent inhibition of a keratinocyte hyperproliferative differentiation marker. The Journal of Biological Chemistry. 1997;272:25555–25559. doi: 10.1074/jbc.272.41.25555. [DOI] [PubMed] [Google Scholar]
- Dockx P, Decree J, Degreef H. Inhibition of the metabolism of endogenous retinoic acid as treatment for severe psoriasis: an open study with oral liarozole. The British Journal of Dermatology. 1995;133:426–432. doi: 10.1111/j.1365-2133.1995.tb02672.x. [DOI] [PubMed] [Google Scholar]
- Dogra SC, Khanduja KL, Gupta MP. The effect of vitamin A deficiency on the initiation and postinitiation phases of benzo(a)pyrene-induced lung tumourigenesis in rats. British Journal of Cancer. 1985;52:931–935. doi: 10.1038/bjc.1985.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dogra S, Yadav S. Acitretin in psoriasis: an evolving scenario. International Journal of Dermatology. 2014;53:525–538. doi: 10.1111/ijd.12365. [DOI] [PubMed] [Google Scholar]
- Dong D, Ruuska SE, Levinthal DJ, Noy N. Distinct roles for cellular retinoic acid-binding proteins I and II in regulating signaling by retinoic acid. The Journal of Biological Chemistry. 1999;274:23695–23698. doi: 10.1074/jbc.274.34.23695. [DOI] [PubMed] [Google Scholar]
- Downie D, McFadyen MCE, Rooney PH, Cruickshank ME, Parkin DE, Miller ID, Telfer C, Melvin WT, Murray GI. Profiling cytochrome P450 expression in ovarian cancer: identification of prognostic markers. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 2005;11:7369–7375. doi: 10.1158/1078-0432.CCR-05-0466. [DOI] [PubMed] [Google Scholar]
- Duester G. Retinoic Acid Synthesis and Signaling during Early Organogenesis. Cell. 2008;134:921–931. doi: 10.1016/j.cell.2008.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupuy P, Bagot M, Heslan M, Dubertret L. Synthetic retinoids inhibit the antigen presenting properties of epidermal cells in vitro. The Journal of Investigative Dermatology. 1989;93:455–459. doi: 10.1111/1523-1747.ep12284027. [DOI] [PubMed] [Google Scholar]
- Elmabsout AA, Kumawat A, Saenz-Méndez P, Krivospitskaya O, Sävenstrand H, Olofsson PS, Eriksson LA, Strid A, Valen G, Törmä H, Sirsjö A. Cloning and functional studies of a splice variant of CYP26B1 expressed in vascular cells. PloS One. 2012;7:e36839. doi: 10.1371/journal.pone.0036839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farr PM, Krause LB, Marks JM, Shuster S. Response of scalp psoriasis to oral ketoconazole. Lancet. 1985;2:921–922. doi: 10.1016/s0140-6736(85)90853-0. [DOI] [PubMed] [Google Scholar]
- Feldmann M, Brennan FM, Maini RN. Rheumatoid arthritis. Cell. 1996;85:307–10. doi: 10.1016/s0092-8674(00)81109-5. [DOI] [PubMed] [Google Scholar]
- Fenaux P, Wang ZZ, Degos L. Treatment of acute promyelocytic leukemia by retinoids. Current Topics in Microbiology and Immunology. 2007;313:101–128. doi: 10.1007/978-3-540-34594-7_7. [DOI] [PubMed] [Google Scholar]
- Fiorella PD, Napoli JL. Microsomal retinoic acid metabolism. Effects of cellular retinoic acid-binding protein (type I) and C18-hydroxylation as an initial step. The Journal of Biological Chemistry. 1994;269:10538–10544. [PubMed] [Google Scholar]
- Fisher GJ, Voorhees JJ. Molecular mechanisms of retinoid actions in skin. FASEB Journal: Official Publication of the Federation of American Societies for Experimental Biology. 1996;10:1002–1013. doi: 10.1096/fasebj.10.9.8801161. [DOI] [PubMed] [Google Scholar]
- Fransén K, Franzén P, Magnuson A, Elmabsout AA, Nyhlin N, Wickbom A, Curman B, Törkvist L, D’Amato M, Bohr J, Tysk C, Sirsjö A, Halfvarson J. Polymorphism in the Retinoic Acid Metabolizing Enzyme CYP26B1 and the Development of Crohn’s Disease. PLoS ONE. 2013;8:e72739. doi: 10.1371/journal.pone.0072739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamble MV, Ramakrishnan R, Palafox NA, Briand K, Berglund L, Blaner WS. Retinol binding protein as a surrogate measure for serum retinol: studies in vitamin A-deficient children from the Republic of the Marshall Islands. The American Journal of Clinical Nutrition. 2001;73:594–601. doi: 10.1093/ajcn/73.3.594. [DOI] [PubMed] [Google Scholar]
- Giltaire S, Herphelin F, Frankart A, Herin M, Stoppie P, Poumay Y. The CYP26 inhibitor R115866 potentiates the effects of all-trans retinoic acid on cultured human epidermal keratinocytes. British Journal of Dermatology. 2009;160:505–13. doi: 10.1111/j.1365-2133.2008.08960.x. [DOI] [PubMed] [Google Scholar]
- Godbole AM, Purushottamachar P, Martin MS, Daskalakis C, Njar VCO. Autophagy inhibition synergistically enhances anticancer efficacy of RAMBA, VN/12-1 in SKBR-3 cells, and tumor xenografts. Molecular Cancer Therapeutics. 2012;11:898–908. doi: 10.1158/1535-7163.MCT-11-0860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomaa MS, Bridgens CE, Veal GJ, Redfern CPF, Brancale A, Armstrong JL, Simons C. Synthesis and biological evaluation of 3-(1H-imidazol- and triazol-1-yl)-2,2-dimethyl-3-[4-(naphthalen-2-ylamino)phenyl]propyl derivatives as small molecule inhibitors of retinoic acid 4-hydroxylase (CYP26) Journal of Medicinal Chemistry. 2011;54:6803–6811. doi: 10.1021/jm200695m. [DOI] [PubMed] [Google Scholar]
- Gudas LJ. Emerging roles for retinoids in regeneration and differentiation in normal and disease states. Biochimica Et Biophysica Acta. 2012;1821:213–221. doi: 10.1016/j.bbalip.2011.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudas LJ, Wagner JA. Retinoids regulate stem cell differentiation. Journal of Cellular Physiology. 2011;226:322–330. doi: 10.1002/jcp.22417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guidez F, Ivins S, Zhu J, Söderström M, Waxman S, Zelent A. Reduced Retinoic Acid-Sensitivities of Nuclear Receptor Corepressor Binding to PML- and PLZF-RARα Underlie Molecular Pathogenesis and Treatment of Acute Promyelocytic Leukemia. Blood. 1998;91:2634–2642. [PubMed] [Google Scholar]
- Guilliams M, Crozat K, Henri S, Tamoutounour S, Grenot P, Devilard E, de Bovis B, Alexopoulou L, Dalod M, Malissen B. Skin-draining lymph nodes contain dermis-derived CD103(-) dendritic cells that constitutively produce retinoic acid and induce Foxp3(+) regulatory T cells. Blood. 2010;115:1958–1968. doi: 10.1182/blood-2009-09-245274. [DOI] [PubMed] [Google Scholar]
- Hall JA, Grainger JR, Spencer SP, Belkaid Y. The role of retinoic acid in tolerance and immunity. Immunity. 2011;35:13–22. doi: 10.1016/j.immuni.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen W, Westendorf AM, Buer J. Regulatory T cells as targets for immunotherapy of autoimmunity and inflammation. Inflamm Allergy Drug Targets. 2008;7:217–23. doi: 10.2174/187152808786848360. [DOI] [PubMed] [Google Scholar]
- Hansson GK, Hermansson A. The immune system in atherosclerosis. Nat Immunol. 2011;12:204–12. doi: 10.1038/ni.2001. [DOI] [PubMed] [Google Scholar]
- Hansson GK, Robertson AK, Soderberg-Naucler C. Inflammation and atherosclerosis. Annu Rev Pathol. 2006;1:297–329. doi: 10.1146/annurev.pathol.1.110304.100100. [DOI] [PubMed] [Google Scholar]
- Harper RA. Specificity in the synergism between retinoic acid and EGF on the growth of adult human skin fibroblasts. Experimental Cell Research. 1988;178:254–263. doi: 10.1016/0014-4827(88)90396-5. [DOI] [PubMed] [Google Scholar]
- Harper RA, Burgoon T. Differential effects of retinoic acid on the growth of normal fibroblast-like cells in vitro from human, swine and rabbit skin. Cell Biology International Reports. 1982;6:163–170. doi: 10.1016/0309-1651(82)90093-5. [DOI] [PubMed] [Google Scholar]
- Heise R, Mey J, Neis MM, Marquardt Y, Joussen S, Ott H, Wiederholt T, Kurschat P, Megahed M, Bickers DR, Merk HF, Baron JM. Skin retinoid concentrations are modulated by CYP26AI expression restricted to basal keratinocytes in normal human skin and differentiated 3D skin models. The Journal of Investigative Dermatology. 2006;126:2473–2480. doi: 10.1038/sj.jid.5700432. [DOI] [PubMed] [Google Scholar]
- Hogarth CA, Arnold S, Kent T, Mitchell D, Isoherranen N, Griswold MD. Processive pulses of retinoic acid propel asynchronous and continuous murine sperm production. Biology of Reproduction. 2015;92:37. doi: 10.1095/biolreprod.114.126326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogarth CA, Griswold MD. Retinoic acid regulation of male meiosis. Current Opinion in Endocrinology, Diabetes, and Obesity. 2013;20:217–223. doi: 10.1097/MED.0b013e32836067cf. [DOI] [PubMed] [Google Scholar]
- Hong K, Zhang Y, Guo Y, Xie J, Wang J, He X, Lu N, Bai A. All-trans retinoic acid attenuates experimental colitis through inhibition of NF-κB signaling. Immunology Letters. 2014;162:34–40. doi: 10.1016/j.imlet.2014.06.011. [DOI] [PubMed] [Google Scholar]
- Huang ME, Ye YC, Chen SR, Chai JR, Lu JX, Zhoa L, Gu LJ, Wang ZY. Use of all-trans retinoic acid in the treatment of acute promyelocytic leukemia. Blood. 1988;72:567–572. [PubMed] [Google Scholar]
- Idres N, Marill J, Chabot GG. Regulation of CYP26A1 expression by selective RAR and RXR agonists in human NB4 promyelocytic leukemia cells. Biochemical Pharmacology. 2005;69:1595–1601. doi: 10.1016/j.bcp.2005.02.024. [DOI] [PubMed] [Google Scholar]
- Ito Y, Gajalakshmi KC, Sasaki R, Suzuki K, Shanta V. A study on serum carotenoid levels in breast cancer patients of Indian women in Chennai (Madras), India. Journal of Epidemiology/Japan Epidemiological Association. 1999;9:306–314. doi: 10.2188/jea.9.306. [DOI] [PubMed] [Google Scholar]
- Iwata M, Hirakiyama A, Eshima Y, Kagechika H, Kato C, Song SY. Retinoic Acid Imprints Gut-Homing Specificity on T Cells. Immunity. 2004;21:527–538. doi: 10.1016/j.immuni.2004.08.011. [DOI] [PubMed] [Google Scholar]
- Jelski W, Chrostek L, Szmitkowski M, Markiewicz W. The activity of class I, II, III and IV alcohol dehydrogenase isoenzymes and aldehyde dehydrogenase in breast cancer. Clinical and Experimental Medicine. 2006;6:89–93. doi: 10.1007/s10238-006-0101-z. [DOI] [PubMed] [Google Scholar]
- Jelski W, Zalewski B, Chrostek L, Szmitkowski M. The activity of class I, II, III, and IV alcohol dehydrogenase isoenzymes and aldehyde dehydrogenase in colorectal cancer. Digestive Diseases and Sciences. 2004;49:977–981. doi: 10.1023/b:ddas.0000034557.23322.e0. [DOI] [PubMed] [Google Scholar]
- Johst U, Betsch A, Wiskirchen J, Schöber W, Vonthein R, Rinkert N, Kehlbach R, Claussen CD, Duda SH. All-trans and 9-cis retinoid acids inhibit proliferation, migration, and synthesis of extracellular matrix of human vascular smooth muscle cells by inducing differentiation in vitro. Journal of Cardiovascular Pharmacology. 2003;41:526–535. doi: 10.1097/00005344-200304000-00004. [DOI] [PubMed] [Google Scholar]
- Kakizuka A, Miller WH, Jr, Umesono K, Warrell RP, Jr, Frankel SR, Murty VVVS, Dmitrovsky E, Evans RM. Chromosomal translocation t(15;17) in human acute promyelocytic leukemia fuses RARα with a novel putative transcription factor, PML. Cell. 1991;66:663–674. doi: 10.1016/0092-8674(91)90112-c. [DOI] [PubMed] [Google Scholar]
- Kamei N, Hiyama K, Yamaoka H, Kamimatsuse A, Onitake Y, Sueda T, Hiyama E. Evaluation of genes identified by microarray analysis in favorable neuroblastoma. Pediatric Surgery International. 2009;25:931–937. doi: 10.1007/s00383-009-2448-1. [DOI] [PubMed] [Google Scholar]
- Kane MA, Folias AE, Pingitore A, Perri M, Obrochta KM, Krois CR, Cione E, Ryu JY, Napoli JL. Identification of 9-cis-retinoic acid as a pancreas- specific autacoid that attenuates glucose-stimulated insulin secretion. Proceedings of the National Academy of Sciences. 2010;107:21884–21889. doi: 10.1073/pnas.1008859107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane MA, Folias AE, Wang C, Napoli JL. Quantitative Profiling of Endogenous Retinoic Acid in Vivo and in Vitro by Tandem Mass Spectrometry. Analytical Chemistry. 2008;80:1702–1708. doi: 10.1021/ac702030f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang SG, Park J, Cho JY, Ulrich B, Kim CH. Complementary roles of retinoic acid and TGF-β1 in coordinated expression of mucosal integrins by T cells. Mucosal Immunology. 2011;4:66–82. doi: 10.1038/mi.2010.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kedishvili NY. Enzymology of retinoic acid biosynthesis and degradation. Journal of Lipid Research. 2013;54:1744–1760. doi: 10.1194/jlr.R037028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelaidi C, Ades L, Chevret S, Sanz M, Guerci A, Thomas X, de Botton S, Raffoux E, Rayon C, Fegueux N, Bordessoule D, Rigal-Huguet F, Link H, … Fenaux P. Late first relapses in APL treated with all-trans-retinoic acid- and anthracycline- based chemotherapy: the European APL group experience (APL 91 and APL 93 trials) Leukemia. 2006;20:905–907. doi: 10.1038/sj.leu.2404158. [DOI] [PubMed] [Google Scholar]
- Krivospitskaya O, Elmabsout AA, Sundman E, Soderstrom LA, Ovchinnikova O, Gidlof AC, Scherbak N, Norata GD, Samnegard A, Torma H, Abdel-Halim SM, Jansson JH, Eriksson P, … Olofsson PS. A CYP26B1 polymorphism enhances retinoic acid catabolism and may aggravate atherosclerosis. Molecular Medicine. 2012;18:712–8. doi: 10.2119/molmed.2012.00094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S, Sandell LL, Trainor PA, Koentgen F, Duester G. Alcohol and aldehyde dehydrogenases: Retinoid metabolic effects in mouse knockout models. Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids. 2012;1821:198–205. doi: 10.1016/j.bbalip.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuppumbatti YS, Bleiweiss IJ, Mandeli JP, Waxman S, Mira-Y-Lopez R. Cellular retinol-binding protein expression and breast cancer. Journal of the National Cancer Institute. 2000;92:475–480. doi: 10.1093/jnci/92.6.475. [DOI] [PubMed] [Google Scholar]
- Kurlandsky SB, Gamble MV, Ramakrishnan R, Blaner WS. Plasma delivery of retinoic acid to tissues in the rat. The Journal of Biological Chemistry. 1995;270:17850–17857. doi: 10.1074/jbc.270.30.17850. [DOI] [PubMed] [Google Scholar]
- Lampron C, Rochette-Egly C, Gorry P, Dollé P, Mark M, Lufkin T, LeMeur M, Chambon P. Mice deficient in cellular retinoic acid binding protein II (CRABPII) or in both CRABPI and CRABPII are essentially normal. Development (Cambridge, England) 1995;121:539–548. doi: 10.1242/dev.121.2.539. [DOI] [PubMed] [Google Scholar]
- Libby P, Ridker PM, Hansson GK. Inflammation in atherosclerosis: from pathophysiology to practice. Journal of the American College of Cardiology. 2009;54:2129–38. doi: 10.1016/j.jacc.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li F, Zhao D, Ren J, Hao F, Liu G, Jin S, Jing Y, Cheng M. 2-(2-Methylfuran-3-carboxamido)-3-phenylpropanoic acid, a potential CYP26A1 inhibitor to enhance all-trans retinoic acid-induced leukemia cell differentiation based on virtual screening and biological evaluation. Bioorganic & Medicinal Chemistry. 2013;21:3256–3261. doi: 10.1016/j.bmc.2013.03.044. [DOI] [PubMed] [Google Scholar]
- Lobo GP, Amengual J, Palczewski G, Babino D, von Lintig J. Mammalian carotenoid-oxygenases: key players for carotenoid function and homeostasis. Biochimica Et Biophysica Acta. 2012;1821:78–87. doi: 10.1016/j.bbalip.2011.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutz JD, Dixit V, Yeung CK, Dickmann LJ, Zelter A, Thatcher JE, Nelson WL, Isoherranen N. Expression and functional characterization of cytochrome P450 26A1, a retinoic acid hydroxylase. Biochemical Pharmacology. 2009;77:258–268. doi: 10.1016/j.bcp.2008.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLean G, Abu-Abed S, Dollé P, Tahayato A, Chambon P, Petkovich M. Cloning of a novel retinoic-acid metabolizing cytochrome P450, Cyp26B1, and comparative expression analysis with Cyp26A1 during early murine development. Mechanisms of Development. 2001;107:195–201. doi: 10.1016/s0925-4773(01)00463-4. [DOI] [PubMed] [Google Scholar]
- Maden M. Retinoic acid in the development, regeneration and maintenance of the nervous system. Nature Reviews. Neuroscience. 2007;8:755–765. doi: 10.1038/nrn2212. [DOI] [PubMed] [Google Scholar]
- Mahida YR. The key role of macrophages in the immunopathogenesis of inflammatory bowel disease. Inflammatory Bowel Diseases. 2000;6:21–33. doi: 10.1097/00054725-200002000-00004. [DOI] [PubMed] [Google Scholar]
- Marill J, Cresteil T, Lanotte M, Chabot GG. Identification of human cytochrome P450s involved in the formation of all-trans-retinoic acid principal metabolites. Molecular Pharmacology. 2000;58:1341–1348. doi: 10.1124/mol.58.6.1341. [DOI] [PubMed] [Google Scholar]
- Maris JM, Hogarty MD, Bagatell R, Cohn SL. Neuroblastoma. The Lancet. 2007;369:2106–2120. doi: 10.1016/S0140-6736(07)60983-0. [DOI] [PubMed] [Google Scholar]
- Martens JHA, Brinkman AB, Simmer F, Francoijs KJ, Nebbioso A, Ferrara F, Altucci L, Stunnenberg HG. PML-RARα/RXR Alters the Epigenetic Landscape in Acute Promyelocytic Leukemia. Cancer Cell. 2010;17:173–185. doi: 10.1016/j.ccr.2009.12.042. [DOI] [PubMed] [Google Scholar]
- Marwarha G, Berry DC, Croniger CM, Noy N. The retinol esterifying enzyme LRAT supports cell signaling by retinol-binding protein and its receptor STRA6. FASEB Journal: Official Publication of the Federation of American Societies for Experimental Biology. 2014;28:26–34. doi: 10.1096/fj.13-234310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthay KK. Targeted isotretinoin in neuroblastoma: kinetics, genetics, or absorption. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 2013;19:311–313. doi: 10.1158/1078-0432.CCR-12-3313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthay KK, Reynolds CP, Seeger RC, Shimada H, Adkins ES, Haas-Kogan D, Gerbing RB, London WB, Villablanca JG. Long-Term Results for Children With High-Risk Neuroblastoma Treated on a Randomized Trial of Myeloablative Therapy Followed by 13-cis-Retinoic Acid: A Children’s Oncology Group Study. Journal of Clinical Oncology. 2009;27:1007–1013. doi: 10.1200/JCO.2007.13.8925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthay KK, Villablanca JG, Seeger RC, Stram DO, Harris RE, Ramsay NK, Swift P, Shimada H, Black CT, Brodeur GM, Gerbing RB, Reynolds CP. Treatment of High-Risk Neuroblastoma with Intensive Chemotherapy, Radiotherapy, Autologous Bone Marrow Transplantation, and 13-cis-Retinoic Acid. New England Journal of Medicine. 1999;341:1165–1173. doi: 10.1056/NEJM199910143411601. [DOI] [PubMed] [Google Scholar]
- McBee JK, Kuksa V, Alvarez R, de Lera AR, Prezhdo O, Haeseleer F, Sokal I, Palczewski K. Isomerization of all-trans-Retinol to cis-Retinols in Bovine Retinal Pigment Epithelial Cells: Dependence on the Specificity of Retinoid-Binding Proteins. Biochemistry. 2000;39:11370–11380. doi: 10.1021/bi001061c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormick AM, Kroll KD, Napoli JL. 13-cis-Retinoic acid metabolism in vivo. The major tissue metabolites in the rat have the all-trans configuration. Biochemistry. 1983;22:3933–3940. doi: 10.1021/bi00285a032. [DOI] [PubMed] [Google Scholar]
- McCully ML, Ladell K, Hakobyan S, Mansel RE, Price DA, Moser B. Epidermis instructs skin homing receptor expression in human T cells. Blood. 2012;120:4591–4598. doi: 10.1182/blood-2012-05-433037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McSorley LC, Daly AK. Identification of human cytochrome P450 isoforms that contribute to all-trans-retinoic acid 4-hydroxylation. Biochemical Pharmacology. 2000;60:517–526. doi: 10.1016/s0006-2952(00)00356-7. [DOI] [PubMed] [Google Scholar]
- Miano JM, Topouzis S, Majesky MW, Olson EN. Retinoid receptor expression and all-trans retinoic acid-mediated growth inhibition in vascular smooth muscle cells. Circulation. 1996;93:1886–1895. doi: 10.1161/01.cir.93.10.1886. [DOI] [PubMed] [Google Scholar]
- Moulas AN, Gerogianni IC, Papadopoulos D, Gourgoulianis KI. Serum retinoic acid, retinol and retinyl palmitate levels in patients with lung cancer. Respirology (Carlton, Vic.) 2006;11:169–174. doi: 10.1111/j.1440-1843.2006.00833.x. [DOI] [PubMed] [Google Scholar]
- Mucida D, Park Y, Kim G, Turovskaya O, Scott I, Kronenberg M, Cheroutre H. Reciprocal TH17 and Regulatory T Cell Differentiation Mediated by Retinoic Acid. Science. 2007;317:256–260. doi: 10.1126/science.1145697. [DOI] [PubMed] [Google Scholar]
- Muindi J, Frankel SR, Miller WJ, Jakubowski A, Scheinberg DA, Young CW, Dmitrovsky E, Warrell RJ. Continuous treatment with all-trans retinoic acid causes a progressive reduction in plasma drug concentrations: implications for relapse and retinoid “resistance” in patients with acute promyelocytic leukemia [published erratum appears in Blood 1992 Aug 1;80(3):855] Blood. 1992;79:299–303. [PubMed] [Google Scholar]
- Nadin L, Murray M. Participation of CYP2C8 in retinoic acid 4-hydroxylation in human hepatic microsomes. Biochemical Pharmacology. 1999;58:1201–1208. doi: 10.1016/s0006-2952(99)00192-6. [DOI] [PubMed] [Google Scholar]
- Napoli JL. Physiological insights into all-trans-retinoic acid biosynthesis. Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids. 2012;1821:152–167. doi: 10.1016/j.bbalip.2011.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson CH, Buttrick BR, Isoherranen N. Therapeutic potential of the inhibition of the retinoic acid hydroxylases CYP26A1 and CYP26B1 by xenobiotics. Current Topics in Medicinal Chemistry. 2013;13:1402–1428. doi: 10.2174/1568026611313120004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nestle FO, Kaplan DH, Barker J. Psoriasis. New England Journal of Medicine. 2009;361:496–509. doi: 10.1056/NEJMra0804595. [DOI] [PubMed] [Google Scholar]
- Njar VCO, Gediya L, Purushottamachar P, Chopra P, Vasaitis TS, Khandelwal A, Mehta J, Huynh C, Belosay A, Patel J. Retinoic acid metabolism blocking agents (RAMBAs) for treatment of cancer and dermatological diseases. Bioorganic & Medicinal Chemistry. 2006;14:4323–4340. doi: 10.1016/j.bmc.2006.02.041. [DOI] [PubMed] [Google Scholar]
- Nonnecke BJ, Horst RL, Dubeski PL, Reinhardt TA. Reactivity and Phenotype of Mononuclear Leukocytes from Nongravid Heifers After In Vitro Exposure to 9,13-di-cis-Retinoic Acid. Journal of Dairy Science. 1997;80:2833–2841. doi: 10.3168/jds.S0022-0302(97)76248-9. [DOI] [PubMed] [Google Scholar]
- Noy N. Retinoid-binding proteins: mediators of retinoid action. The Biochemical Journal. 2000;348(Pt 3):481–495. [PMC free article] [PubMed] [Google Scholar]
- Noy N. Between death and survival: retinoic acid in regulation of apoptosis. Annual Review of Nutrition. 2010;30:201–217. doi: 10.1146/annurev.nutr.28.061807.155509. [DOI] [PubMed] [Google Scholar]
- Ocaya PA, Elmabsout AA, Olofsson PS, Torma H, Gidlof AC, Sirsjo A. CYP26B1 plays a major role in the regulation of all-trans-retinoic acid metabolism and signaling in human aortic smooth muscle cells. Journal of Vascular Research. 2011;48:23–30. doi: 10.1159/000317397. [DOI] [PubMed] [Google Scholar]
- Orfali N, McKenna SL, Cahill MR, Gudas LJ, Mongan NP. Retinoid receptor signaling and autophagy in acute promyelocytic leukemia. Experimental Cell Research. 2014;324:1–12. doi: 10.1016/j.yexcr.2014.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orywal K, Jelski W, Zdrodowski M, Szmitkowski M. The activity of class I, II, III and IV alcohol dehydrogenase isoenzymes and aldehyde dehydrogenase in cervical cancer. Clinical Biochemistry. 2011;44:1231–1234. doi: 10.1016/j.clinbiochem.2011.07.004. [DOI] [PubMed] [Google Scholar]
- Orywal K, Jelski W, Zdrodowski M, Szmitkowski M. The activity of class I, II, III and IV alcohol dehydrogenase isoenzymes and aldehyde dehydrogenase in ovarian cancer and ovarian cysts. Advances in Medical Sciences. 2013;58:216–220. doi: 10.2478/ams-2013-0012. [DOI] [PubMed] [Google Scholar]
- Osanai M, Lee GH. Increased expression of the retinoic acid-metabolizing enzyme CYP26A1 during the progression of cervical squamous neoplasia and head and neck cancer. BMC Research Notes. 2014;7:697. doi: 10.1186/1756-0500-7-697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osanai M, Petkovich M. Expression of the Retinoic Acid-Metabolizing Enzyme CYP26A1 Limits Programmed Cell Death. Molecular Pharmacology. 2005;67:1808–1817. doi: 10.1124/mol.104.005769. [DOI] [PubMed] [Google Scholar]
- Osanai M, Sawada N, Lee GH. Oncogenic and cell survival properties of the retinoic acid metabolizing enzyme, CYP26A1. Oncogene. 2009;29:1135–1144. doi: 10.1038/onc.2009.414. [DOI] [PubMed] [Google Scholar]
- Ozpolat B, Mehta K, Lopez-Berestein G. Regulation of a highly specific retinoic acid-4-hydroxylase (CYP26A1) enzyme and all-trans-retinoic acid metabolism in human intestinal, liver, endothelial, and acute promyelocytic leukemia cells. Leukemia & Lymphoma. 2005;46:1497–1506. doi: 10.1080/10428190500174737. [DOI] [PubMed] [Google Scholar]
- Ozpolat B, Mehta K, Tari AM, Lopez-Berestein G. all-trans-Retinoic acid-induced expression and regulation of retinoic acid 4-hydroxylase (CYP26) in human promyelocytic leukemia. American Journal of Hematology. 2002;70:39–47. doi: 10.1002/ajh.10099. [DOI] [PubMed] [Google Scholar]
- Pandolfi PP, Grignani F, Alcalay M, Mencarelli A, Biondi A, LoCoco F, Grignani F, Pelicci PG. Structure and origin of the acute promyelocytic leukemia myl/RAR alpha cDNA and characterization of its retinoid-binding and transactivation properties. Oncogene. 1991;6:1285–1292. [PubMed] [Google Scholar]
- Pavez Loriè E, Chamcheu JC, Vahlquist A, Törmä H. Both all-trans retinoic acid and cytochrome P450 (CYP26) inhibitors affect the expression of vitamin A metabolizing enzymes and retinoid biomarkers in organotypic epidermis. Archives for Dermatological Research. Archiv Fur Dermatologische Forschung. 2009;301:475–85. doi: 10.1007/s00403-009-0937-7. [DOI] [PubMed] [Google Scholar]
- Pavez Loriè E, Cools M, Borgers M, Wouters L, Shroot B, Hagforsen E, Törmä H, Vahlquist A. Topical treatment with CYP26 inhibitor talarozole (R115866) dose dependently alters the expression of retinoid-regulated genes in normal human epidermis. The British Journal of Dermatology. 2009;160:26–36. doi: 10.1111/j.1365-2133.2008.08895.x. [DOI] [PubMed] [Google Scholar]
- Pavez Loriè E, Li H, Vahlquist A, Törmä H. The involvement of cytochrome p450 (CYP) 26 in the retinoic acid metabolism of human epidermal keratinocytes. Biochimica Et Biophysica Acta. 2009;1791:220–228. doi: 10.1016/j.bbalip.2008.12.004. [DOI] [PubMed] [Google Scholar]
- Qiu Y, Pu T, Li L, Cheng F, Lu C, Sun L, Teng X, Ye F, Bu H. The expression of aldehyde dehydrogenase family in breast cancer. Journal of Breast Cancer. 2014;17:54–60. doi: 10.4048/jbc.2014.17.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quere R, Baudet A, Cassinat B, Bertrand G, Marti J, Manchon L, Piquemal D, Chomienne C, Commes T. Pharmacogenomic analysis of acute promyelocytic leukemia cells highlights CYP26 cytochrome metabolism in differential all-trans retinoic acid sensitivity. Blood. 2007;109:4450–4460. doi: 10.1182/blood-2006-10-051086. [DOI] [PubMed] [Google Scholar]
- Raner GM, Vaz AD, Coon MJ. Metabolism of all-trans, 9-cis, and 13-cis isomers of retinal by purified isozymes of microsomal cytochrome P450 and mechanism-based inhibition of retinoid oxidation by citral. Molecular Pharmacology. 1996;49:515–522. [PubMed] [Google Scholar]
- Raverdeau M, Mills KHG. Modulation of T cell and innate immune responses by retinoic acid. Journal of Immunology (Baltimore, Md.: 1950) 2014;192:2953–2958. doi: 10.4049/jimmunol.1303245. [DOI] [PubMed] [Google Scholar]
- Reynolds CP, Matthay KK, Villablanca JG, Maurer BJ. Retinoid therapy of high-risk neuroblastoma. Cancer Letters. 2003;197:185–192. doi: 10.1016/s0304-3835(03)00108-3. [DOI] [PubMed] [Google Scholar]
- Reynolds CP, Schindler PF, Jones DM, Gentile JL, Proffitt RT, Einhorn PA. Comparison of 13-cis-retinoic acid to trans-retinoic acid using human neuroblastoma cell lines. Progress in Clinical and Biological Research. 1994;385:237–244. [PubMed] [Google Scholar]
- Rhee EJ, Nallamshetty S, Plutzky J. Retinoid metabolism and its effects on the vasculature. Biochimica et Biophysica Acta. 2012;1821:230–40. doi: 10.1016/j.bbalip.2011.07.001. [DOI] [PubMed] [Google Scholar]
- Roos TC, Jugert FK, Merk HF, Bickers DR. Retinoid Metabolism in the Skin. Pharmacological Reviews. 1998;50:315–333. [PubMed] [Google Scholar]
- Rosenberger M, Neukom C. Retinoic acid metabolites. 3. Total synthesis of (2E,4E,6E,8E)-3,7-dimethyl-9-[6,6-dimethyl-2-(hydroxymethyl)-1-cyclohexen-1-yl]-2,4,6,8-nonatetraenoic acid. Journal of Organic Chemistry. 1982;47:1782–1785. [Google Scholar]
- Ross AC. Retinoid Production and Catabolism: Role of Diet in Regulating Retinol Esterification and Retinoic Acid Oxidation. The Journal of Nutrition. 2003;133:291S–296S. doi: 10.1093/jn/133.1.291S. [DOI] [PubMed] [Google Scholar]
- Ross AC. Vitamin A and retinoic acid in T cell-related immunity. The American Journal of Clinical Nutrition. 2012;96:1166S–72S. doi: 10.3945/ajcn.112.034637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roussel MJ, Lanotte M. Maturation sensitive and resistant t(15;17) NB4 cell lines as tools for APL physiopathology: nomenclature of cells and repertory of their known genetic alterations and phenotypes. Oncogene. 2001;20:7287–7291. doi: 10.1038/sj.onc.1204863. Published Online: 29 October 2001. [DOI] [PubMed] [Google Scholar]
- Ruzicka T, Larsen FG, Galewicz D, Horváth A, Coenraads PJ, Thestrup-Pedersen K, Ortonne JP, Zouboulis CC, Harsch M, Brown TC, Zultak M. Oral alitretinoin (9-cis-retinoic acid) therapy for chronic hand dermatitis in patients refractory to standard therapy: results of a randomized, double-blind, placebo-controlled, multicenter trial. Archives of Dermatology. 2004;140:1453–1459. doi: 10.1001/archderm.140.12.1453. [DOI] [PubMed] [Google Scholar]
- Samokyszyn VM, Gall WE, Zawada G, Freyaldenhoven MA, Chen G, Mackenzie PI, Tephly TR, Radominska-Pandya A. 4-hydroxyretinoic acid, a novel substrate for human liver microsomal UDP-glucuronosyltransferase(s) and recombinant UGT2B7. The Journal of Biological Chemistry. 2000;275:6908–6914. doi: 10.1074/jbc.275.10.6908. [DOI] [PubMed] [Google Scholar]
- Sanders TJ, McCarthy NE, Giles EM, Davidson KL, Haltalli ML, Hazell S, Lindsay JO, Stagg AJ. Increased production of retinoic acid by intestinal macrophages contributes to their inflammatory phenotype in patients with Crohn’s disease. Gastroenterology. 2014;146:1278–88. e1–2. doi: 10.1053/j.gastro.2014.01.057. [DOI] [PubMed] [Google Scholar]
- Sass JO, Forster A, Bock KW, Nau H. Glucuronidation and isomerization of all-trans- and 13-CIS-retinoic acid by liver microsomes of phenobarbital- or 3-methylcholanthrene-treated rats. Biochemical Pharmacology. 1994;47:485–492. doi: 10.1016/0006-2952(94)90179-1. [DOI] [PubMed] [Google Scholar]
- Sauvant P, Cansell M, Atgié C. Vitamin A and lipid metabolism: relationship between hepatic stellate cells (HSCs) and adipocytes. Journal of Physiology and Biochemistry. 2011;67:487–496. doi: 10.1007/s13105-011-0101-7. [DOI] [PubMed] [Google Scholar]
- Schoeff L. Vitamin A. The American Journal of Medical Technology. 1983;49:447–452. [PubMed] [Google Scholar]
- Schug TT, Berry DC, Shaw NS, Travis SN, Noy N. Opposing effects of retinoic acid on cell growth result from alternate activation of two different nuclear receptors. Cell. 2007;129:723–733. doi: 10.1016/j.cell.2007.02.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz EL, Hallam S, Gallagher RE, Wiernik PH. Inhibition of all-trans-retinoic acid metabolism by fluconazole in vitro and in patients with acute promyelocytic leukemia. Biochemical Pharmacology. 1995;50:923–928. doi: 10.1016/0006-2952(95)00213-j. [DOI] [PubMed] [Google Scholar]
- Shelton DN, Sandoval IT, Eisinger A, Chidester S, Ratnayake A, Ireland CM, Jones DA. Up-regulation of CYP26A1 in adenomatous polyposis coli-deficient vertebrates via a WNT-dependent mechanism: implications for intestinal cell differentiation and colon tumor development. Cancer Research. 2006;66:7571–7577. doi: 10.1158/0008-5472.CAN-06-1067. [DOI] [PubMed] [Google Scholar]
- Skazik C, Amann PM, Heise R, Marquardt Y, Czaja K, Kim A, Rühl R, Kurschat P, Merk HF, Bickers DR, Baron JM. Downregulation of STRA6 expression in epidermal keratinocytes leads to hyperproliferation-associated differentiation in both in vitro and in vivo skin models. The Journal of Investigative Dermatology. 2014;134:1579–1588. doi: 10.1038/jid.2013.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sklan D. Vitamin A in human nutrition. Progress in Food & Nutrition Science. 1987;11:39– 55. [PubMed] [Google Scholar]
- Smith G, Ibbotson SH, Comrie MM, Dawe RS, Bryden A, Ferguson J, Wolf CR. Regulation of cutaneous drug-metabolizing enzymes and cytoprotective gene expression by topical drugs in human skin in vivo. The British Journal of Dermatology. 2006;155:275–281. doi: 10.1111/j.1365-2133.2006.07317.x. [DOI] [PubMed] [Google Scholar]
- Smith JE, Milch PO, Muto Y, Goodman DS. The plasma transport and metabolism of retinoic acid in the rat. The Biochemical Journal. 1973;132:821–827. doi: 10.1042/bj1320821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stearns ME, Wang M, Fudge K. Liarozole and 13-cis-retinoic acid anti-prostatic tumor activity. Cancer Research. 1993;53:3073–3077. [PubMed] [Google Scholar]
- Stehr PA, Gloninger MF, Kuller LH, Marsh GM, Radford EP, Weinberg GB. Dietary vitamin A deficiencies and stomach cancer. American Journal of Epidemiology. 1985;121:65–70. doi: 10.1093/oxfordjournals.aje.a113984. [DOI] [PubMed] [Google Scholar]
- Stoppie P, Borgers M, Borghgraef P, Dillen L, Goossens J, Sanz G, Szel H, Van Hove C, Van Nyen G, Nobels G, Vanden Bossche H, Venet M, Willemsens G, Van Wauwe J. R115866 inhibits all-trans-retinoic acid metabolism and exerts retinoidal effects in rodents. The Journal of Pharmacology and Experimental Therapeutics. 2000;293:304–312. [PubMed] [Google Scholar]
- Taibi G, Nicotra CMA. Xanthine oxidase catalyzes the oxidation of retinol. Journal of Enzyme Inhibition and Medicinal Chemistry. 2007;22:471–476. doi: 10.1080/14756360701408739. [DOI] [PubMed] [Google Scholar]
- Takeuchi H, Yokota A, Ohoka Y, Iwata M. Cyp26b1 regulates retinoic acid- dependent signals in T cells and its expression is inhibited by transforming growth factor-β. PloS One. 2011;6:e16089. doi: 10.1371/journal.pone.0016089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talley NJ, Abreu MT, Achkar JP, Bernstein CN, Dubinsky MC, Hanauer SB, Kane SV, Sandborn WJ, Ullman TA, Moayyedi P. An Evidence-Based Systematic Review on Medical Therapies for Inflammatory Bowel Disease. The American Journal of Gastroenterology. 2011;106:S2–S25. doi: 10.1038/ajg.2011.58. [DOI] [PubMed] [Google Scholar]
- Tallman MS, Altman JK. How I treat acute promyelocytic leukemia. Blood. 2009;114:5126–5135. doi: 10.1182/blood-2009-07-216457. [DOI] [PubMed] [Google Scholar]
- Tang XH, Gudas LJ. Retinoids, Retinoic Acid Receptors, and Cancer. Annual Review of Pathology: Mechanisms of Disease. 2011;6:345–364. doi: 10.1146/annurev-pathol-011110-130303. [DOI] [PubMed] [Google Scholar]
- Terao M, Kurosaki M, Barzago MM, Fratelli M, Bagnati R, Bastone A, Giudice C, Scanziani E, Mancuso A, Tiveron C, Garattini E. Role of the molybdoflavoenzyme aldehyde oxidase homolog 2 in the biosynthesis of retinoic acid: generation and characterization of a knockout mouse. Molecular and Cellular Biology. 2009;29:357–377. doi: 10.1128/MCB.01385-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thatcher JE, Buttrick B, Shaffer SA, Shimshoni JA, Goodlett DR, Nelson WL, Isoherranen N. Substrate specificity and ligand interactions of CYP26A1, the human liver retinoic acid hydroxylase. Molecular Pharmacology. 2011;80:228–239. doi: 10.1124/mol.111.072413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thatcher JE, Isoherranen N. The role of CYP26 enzymes in retinoic acid clearance. Expert Opinion on Drug Metabolism & Toxicology. 2009;5:875–886. doi: 10.1517/17425250903032681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thatcher JE, Zelter A, Isoherranen N. The relative importance of CYP26A1 in hepatic clearance of all-trans retinoic acid. Biochemical Pharmacology. 2010;80:903–912. doi: 10.1016/j.bcp.2010.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomita S, Okuyama E, Ohnishi T, Ichikawa Y. Characteristic properties of a retinoic acid synthetic cytochrome P-450 purified from liver microsomes of 3- methylcholanthrene-induced rats. Biochimica et Biophysica Acta (BBA) - General Subjects. 1996;1290:273–281. doi: 10.1016/0304-4165(96)00030-x. [DOI] [PubMed] [Google Scholar]
- Topletz AR, Thatcher JE, Zelter A, Lutz JD, Tay S, Nelson WL, Isoherranen N. Comparison of the function and expression of CYP26A1 and CYP26B1, the two retinoic acid hydroxylases. Biochemical Pharmacology. 2012;83:149–163. doi: 10.1016/j.bcp.2011.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topletz AR, Tripathy S, Foti RS, Shimshoni JA, Nelson WL, Isoherranen N. Induction of CYP26A1 by Metabolites of Retinoic Acid: Evidence That CYP26A1 Is an Important Enzyme in the Elimination of Active Retinoids. Molecular Pharmacology. 2015;87:430–441. doi: 10.1124/mol.114.096784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsukada M, Schröder M, Roos TC, Chandraratna RA, Reichert U, Merk HF, Orfanos CE, Zouboulis CC. 13-cis retinoic acid exerts its specific activity on human sebocytes through selective intracellular isomerization to all-trans retinoic acid and binding to retinoid acid receptors. The Journal of Investigative Dermatology. 2000;115:321–327. doi: 10.1046/j.1523-1747.2000.00066.x. [DOI] [PubMed] [Google Scholar]
- Uehara M, Yashiro K, Mamiya S, Nishino J, Chambon P, Dolle P, Sakai Y. CYP26A1 and CYP26C1 cooperatively regulate anterior-posterior patterning of the developing brain and the production of migratory cranial neural crest cells in the mouse. Developmental Biology. 2007;302:399–411. doi: 10.1016/j.ydbio.2006.09.045. [DOI] [PubMed] [Google Scholar]
- Van de Kerkhof PCM. Update on retinoid therapy of psoriasis in: an update on the use of retinoids in dermatology. Dermatologic Therapy. 2006;19:252–263. doi: 10.1111/j.1529-8019.2006.00082.x. [DOI] [PubMed] [Google Scholar]
- Van Giezen JJ, Boon GI, Jansen JW, Bouma BN. Retinoic acid enhances fibrinolytic activity in-vivo by enhancing tissue type plasminogen activator (t-PA) activity and inhibits venous thrombosis. Thrombosis and Haemostasis. 1993;69:381–6. [PubMed] [Google Scholar]
- Van Heusden J, Van Ginckel R, Bruwiere H, Moelans P, Janssen B, Floren W, van der Leede BJ, van Dun J, Sanz G, Venet M, Dillen L, Van Hove C, Willemsens G, … Wouters W. Inhibition of all-TRANS-retinoic acid metabolism by R116010 induces antitumour activity. British Journal of Cancer. 2002;86:605–611. doi: 10.1038/sj.bjc.6600056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Wauwe JP, Coene MC, Goossens J, Cools W, Monbaliu J. Effects of cytochrome P-450 inhibitors on the in vivo metabolism of all-trans-retinoic acid in rats. The Journal of Pharmacology and Experimental Therapeutics. 1990;252:365–369. [PubMed] [Google Scholar]
- Veal GJ, Cole M, Errington J, Pearson ADJ, Foot ABM, Whyman G, Boddy AV UKCCSG Pharmacology Working Group. Pharmacokinetics and metabolism of 13-cis-retinoic acid (isotretinoin) in children with high-risk neuroblastoma - a study of the United Kingdom Children’s Cancer Study Group. British Journal of Cancer. 2007;96:424–431. doi: 10.1038/sj.bjc.6603554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veal GJ, Errington J, Redfern CPF, Pearson ADJ, Boddy AV. Influence of isomerisation on the growth inhibitory effects and cellular activity of 13-cis and all-trans retinoic acid in neuroblastoma cells. Biochemical Pharmacology. 2002;63:207–215. doi: 10.1016/s0006-2952(01)00844-9. [DOI] [PubMed] [Google Scholar]
- Veal GJ, Errington J, Rowbotham SE, Illingworth NA, Malik G, Cole M, Daly AK, Pearson ADJ, Boddy AV. Adaptive dosing approaches to the individualization of 13-cis-retinoic acid (isotretinoin) treatment for children with high- risk neuroblastoma. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 2013;19:469–479. doi: 10.1158/1078-0432.CCR-12-2225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verfaille CJ, Borgers M, van Steensel MAM. Retinoic acid metabolism blocking agents (RAMBAs): a new paradigm in the treatment of hyperkeratotic disorders. Journal Der Deutschen Dermatologischen Gesellschaft = Journal of the German Society of Dermatology: JDDG. 2008;6:355–364. doi: 10.1111/j.1610-0387.2007.06541.x. [DOI] [PubMed] [Google Scholar]
- Verfaille CJ, Thissen CaCB, Bovenschen HJ, Mertens J, Steijlen PM, van de Kerkhof PCM. Oral R115866 in the treatment of moderate to severe plaque- type psoriasis. Journal of the European Academy of Dermatology and Venereology: JEADV. 2007;21:1038–1046. doi: 10.1111/j.1468-3083.2007.02158.x. [DOI] [PubMed] [Google Scholar]
- Vernet N, Dennefeld C, Rochette-Egly C, Oulad-Abdelghani M, Chambon P, Ghyselinck NB, Mark M. Retinoic Acid Metabolism and Signaling Pathways in the Adult and Developing Mouse Testis. Endocrinology. 2006;147:96–110. doi: 10.1210/en.2005-0953. [DOI] [PubMed] [Google Scholar]
- Villablanca JG, Khan AA, Avramis VI, Seeger RC, Matthay KK, Ramsay NK, Reynolds CP. Phase I trial of 13-cis-retinoic acid in children with neuroblastoma following bone marrow transplantation. Journal of Clinical Oncology. 1995;13:894–901. doi: 10.1200/JCO.1995.13.4.894. [DOI] [PubMed] [Google Scholar]
- Watanabe A, Kanai H, Arai M, Sekiguchi K, Uchiyama T, Nagai R, Kurabayashi M. Retinoids induce the PAI-1 gene expression through tyrosine kinase-dependent pathways in vascular smooth muscle cells. Journal of Cardiovascular Pharmacology. 2002;39:503–12. doi: 10.1097/00005344-200204000-00006. [DOI] [PubMed] [Google Scholar]
- Watts JM, Tallman MS. Acute promyelocytic leukemia: What is the new standard of care? Blood Reviews. 2014;28:205–212. doi: 10.1016/j.blre.2014.07.001. [DOI] [PubMed] [Google Scholar]
- Wen J, Lopes F, Soares G, Farrell SA, Nelson C, Qiao Y, Martell S, Badukke C, Bessa C, Ylstra B, Lewis S, Isoherranen N, Maciel P, Rajcan-Separovic E. Phenotypic and functional consequences of haploinsufficiency of genes from exocyst and retinoic acid pathway due to a recurrent microdeletion of 2p13.2. Orphanet Journal of Rare Diseases. 2013;8:100. doi: 10.1186/1750-1172-8-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiedermann U, Chen XJ, Enerbäck L, Hanson LA, Kahu H, Dahlgren UI. Vitamin A deficiency increases inflammatory responses. Scandinavian Journal of Immunology. 1996;44:578–584. doi: 10.1046/j.1365-3083.1996.d01-351.x. [DOI] [PubMed] [Google Scholar]
- Wolbach SB, Howe PR. TISSUE CHANGES FOLLOWING DEPRIVATION OF FAT-SOLUBLE A VITAMIN. The Journal of Experimental Medicine. 1925;42:753–777. doi: 10.1084/jem.42.6.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia HF, Ma JJ, Sun J, Yang Y, Peng JP. Retinoic acid metabolizing enzyme CYP26A1 is implicated in rat embryo implantation. Human Reproduction (Oxford, England) 2010;25:2985–2998. doi: 10.1093/humrep/deq268. [DOI] [PubMed] [Google Scholar]
- Xi J, Yang Z. Expression of RALDHs (ALDH1As) and CYP26s in human tissues and during the neural differentiation of P19 embryonal carcinoma stem cell. Gene Expression Patterns: GEP. 2008;8:438–442. doi: 10.1016/j.gep.2008.04.003. [DOI] [PubMed] [Google Scholar]
- Yashiro K, Zhao X, Uehara M, Yamashita K, Nishijima M, Nishino J, Saijoh Y, Sakai Y, Hamada H. Regulation of retinoic acid distribution is required for proximodistal patterning and outgrowth of the developing mouse limb. Developmental Cell. 2004;6:411–422. doi: 10.1016/s1534-5807(04)00062-0. [DOI] [PubMed] [Google Scholar]
- Zhang QY, Dunbar D, Kaminsky L. Human Cytochrome P-450 Metabolism of Retinals to Retinoic Acids. Drug Metabolism and Disposition. 2000;28:292–297. [PubMed] [Google Scholar]
- Zhong Y, Lin Y, Shen S, Zhou Y, Mao F, Guan J, Sun Q. Expression of ALDH1 in breast invasive ductal carcinoma: an independent predictor of early tumor relapse. Cancer Cell International. 2013;13:60. doi: 10.1186/1475-2867-13-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zile MH, Emerick RJ, DeLuca HF. Identification of 13-cis retinoic acid in tissue extracts and its biological activity in rats. Biochimica Et Biophysica Acta. 1967;141:639–641. doi: 10.1016/0304-4165(67)90194-8. [DOI] [PubMed] [Google Scholar]