Abstract
Chronic kidney disease (CKD) is associated with a decline in muscle mass, strength, and function, collectively called “sarcopenia.” Sarcopenia is associated with hospitalizations and mortality in CKD and is therefore important to understand and characterize. While the focus of skeletal health in CKD has traditionally focused on bone and mineral aberrations, it is now recognized that sarcopenia must also play a role in poor musculoskeletal health in this population. In this paper, we present an overview of skeletal muscle changes in CKD, including defects in skeletal muscle catabolism and anabolism in uremic tissue. There are many gaps in knowledge in this field that should be the focus for future research to unravel pathogenesis and therapies for musculoskeletal health in CKD.
Keywords: Skeletal muscle, Myogenesis, Myostatin, Sarcopenia, Atrophy
Muscle and Its Effect on the Bone in CKD
Chronic Kidney Disease (CKD) is common, affecting more than 26 million Americans [1]. CKD has striking similarities with aging; both carry increased burden of falls, fractures, immobility, loss of functional independence, and frailty that leads to hospitalizations and mortality [2–5]. Bone changes in CKD have been described in detail by others in this series. Associated with these bone abnormalities is also significant skeletal muscle loss, termed “sarcopenia” in CKD. Sarcopenia is widely prevalent in patients undergoing dialysis and is associated with increased hospitalizations and mortality [6, 7•, 8, 9, 10•]. Skeletal muscle is attached to the bone, and forces arc transmitted from the altered muscle to the altered bone in CKD. Tests of muscle function have been shown to be associated with increased fracture risk in dialysis patients [11], as well as in earlier stages of CKD [12]. These biomechanical relationships are not yet fully characterized in CKD.
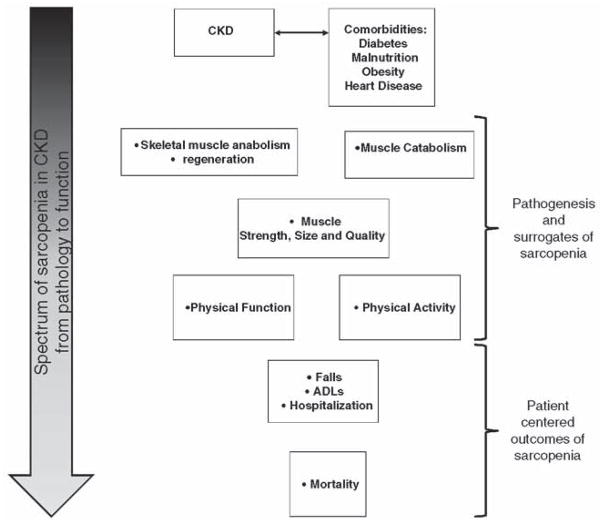
Both the muscle and bone are subjected to the uremic environment in CKD, with its attendant inflammation, insulin resistance, metabolic acidosis, and alterations of mineral metabolism. Further, there are various muscle-derived factors such as insulin-like growth factor (IGF-1), myostatin, etc. that have effects on bone metabolism and form part of the bone-muscle connection in aging [13•, 14•]. Additionally, loss of skeletal muscle (due to CKD and its comorbid conditions) also predisposes a person to a more sedentary lifestyle [15] and increased risk of falls and frailty that in turn leads to more fractures, hospitalizations, and poorer quality of life [16], There-fore, sarcopenia in CKD is not a benign consequence of uremia, and skeletal muscle and bone loss are interrelated by both biomechanics and common exposure to uremic toxins to cause adverse outcomes in CKD. In this review, we present an over-view of changes in skeletal muscle in CKD (see Fig. 1) and their assessment. The goal of understanding sarcopenia in CKD is to eventually develop and test interventions for sarcopenia that improve immobility, disability, falls, fractures, and mortality.
Fig. 1.
Spectrum of sarcopenia in CKD— The spectrum of C KD and associated comorbidities can ultimately influence mortality. This is evident by increased muscle catabolism and decreased regeneration that leads to reduced muscle strength, size, quality (i.e. collectively known as sarcopenia), and consequently limiations in function and activity. Key consequences of sarcopenia in patients with CKD are increased falls, fractures, immobility, disability, and hospitalizations. These ramifications ultimately will influence mortality
Assessment of Skeletal Muscle Loss in Chronic Kidney Disease
The definition of sarcopenia is very variable in the literature. Whereas sarcopenia literally translates to paucity of muscle, others in the literature use the term “sarcopenia” for loss of muscle mass and the term “dynapenia” for loss of muscle strength. Both of these may occur concurrently in CKD, though these losses may occur at different rates. Strength can diminish at a greater rate than muscle mass [17] and vice versa [18], and the interplay between these two concepts is important. In CKD, the term “protein-energy wasting” (PEW) has been proposed to represent a combination of poor nutritional status (low serum levels of albumin, transthyretin, or cholesterol), decreased body mass (low or reduced body or fat mass or weight loss with reduced intake of protein and energy), and decreased muscle mass (muscle wasting or sarcopenia, reduced mid-arm muscle circumference) [19]. In this review, we will use the term sarcopenia to refer to changes in muscle mass, strength, or physical function.
In the aging population, operational definitions for sarcopenia include various cutoffs for lean muscle mass, muscle strength, and physical function (see Table 1). There are three major definitions currently in use: the Foundation of the NIH, the International Working Group on Sarcopenia. and the European Working Group [10•, 20, 21, 22•]. There are no comprehensive operational definitions or specific cutoffs for these measures that have been validated longitudinally in CKD, but declining trends in individual parameters are associated with poor outcomes. In a prospective study of 323 patients with mean GFR of 41.3±19.3 ml/min per 1.73 m2 at the start, Roshanravan et al. showed that a 0.1 m/s decrease in gait speed is associated with a 26 % increased risk of mortality over 3 years [23•]. This is consistent with the data in the general population showing increased risk of mortality with lower values on measures of physical function (gait speed) [24]. A study in 103 incident peritoneal dialysis patients from China similarly demonstrated that lean body mass assessed by creatinine kinetics decreased over 12 months, and low lean mass predicted poor ability to self-perform peritoneal dialysis and decreased patient survival [25]. A recent study from the UK evaluated 60 patients with CKD 4–5 and 74 prevalent patients on dialysis (28 peritoneal and 46 hemodialysis, with average duration on dialysis of 3 years). They assessed serial measures of both muscle mass (muscle cross-sectional area on CT) and physical performance (sit-to-stand testing) and demonstrated that 35 % of patients lost muscle mass in the first year [26]. A study of 128 patients with pre-dialysis CKD followed for a mean of 33 months showed that hand-grip strength is a significant predictor of poor renal outcomes (pre-dialysis mortality or dialysis-dependent end-stage renal disease) [27]. Therefore, patients with kidney disease progressively lose skeletal muscle mass, strength, and function, and this loss is associated with poor outcomes.
Table 1.
Objective assessment of muscle mass, strength, and function
| CKDa/dialysis considerations | ||
|---|---|---|
| Muscle mass | Bioelectrical impedance (BIA) | BIA—measured after midweek session (in dialysis) |
| Dual X-ray absorptiometry (DXA) | Significant atrophy of skeletal muscle may interfere with measurements in some patients | |
| Computerized tomography (CT) | ||
| Magnetic resonance imaging (MRI) | ||
| Strength | Isotonic (constant load) Dynamometry, free weights | Using limb contralateral to dialysis access |
| Isometric (constant angle) Hand-held dynamometry, computerized dynamometry, manual testing | Timing test with dialysis (pre-or post-dialysis) | |
| Isokinetic (constant velocity) Computerized dynamometry | ||
| Function | Gait Speed (4 m walk) | Vascular complications, amputations, and neuropathy in CKD patients may limit use of certain tests. |
| 6 min walk test | ||
| Repeated chair stand | ||
| Timed up and go | ||
| Upper body ergometer |
Reference values/cutoffs from healthy populations are likely different from those from CKD patients
There are multiple ways to assess each component of sarcopenia, as shown in Table 1. Considerations in CKD for these measures are listed. Urine creatinine excretion in 24 h urine collections is a measure of skeletal muscle mass in those with normal kidney function, but is not as useful in CKD where tubular excretion and handling of creatinine are altered or urinary output decreased. Patients with kidney disease have reduced values for all of these muscle measures, and cutoffs established in the literature for aging elders may not apply.
Pathophysiology of CKD-Associated Sarcopenia
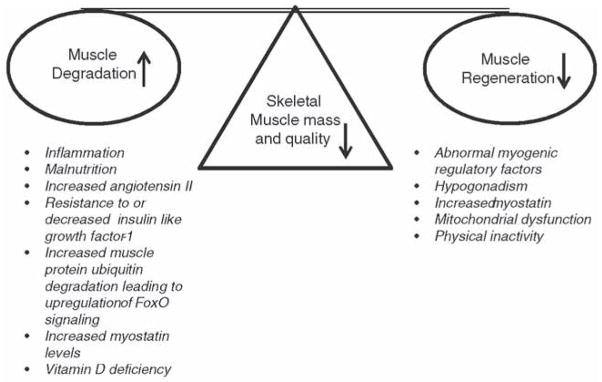
CKD-associated sarcopenia is the result of an altered balance among catabolic and anabolic processes to control muscle homeostasis (Fig. 2). Controlling homeostasis is an extraordinarily complex process made up of hormonal, immunologic, progenitor cell function, mitochondrial dysfunction, inflammation, metabolic acidosis, malnutrition, physical inactivity, excess angiotensin II, and growth factors (insulin/insulin-like growth factor 1 (IGF-I), myostatin), all of which are altered to variable extents from early CKD to dialysis.
Fig. 2.
Skeletal muscle loss in CKD is a result of increased muscle degradation and impaired regeneration
Skeletal Muscle Regeneration
The ability of an aging system absence of comorbidity to regenerate or maintain skeletal muscle mass is quite complex. In response to a stressor (i.e., muscle injury, inflammation), myogenic regulatory factors (MRFs) alter expression to activate satellite cells (aka. muscle stem cells (MuSCs)), differentiate into myotubes, and eventually form a myofiber [28]. The ability of MuSCs to respond in the “normal” aging system has demonstrated contrasting results with a reduced [29] or normal/no change [30] in number of MuSCs. Some have shown impaired function is associated with decreased or delayed expression of myogenic regulatory factors, which regulate satellite cell proliferation and differentiation. Clinically, there is little known regarding myogenic regulation in the CKD population. Studies in CKD (5/6 nephrectomy) animal model demonstrated impaired MuSC activation and reduced MRFs in CKD (as compared to normal aging) both at basal level and in response to injury [31]. To date, little is known regarding how the satellite cell functions in CKD and whether progression of diseases correlates with progressive changes in cell function. However, many of the factors known to regulate MuSCs are abnormal in CKD.
Androgens
The ability to maintain muscle mass through protein formation may be mediated though testosterone. Testosterone may influence skeletal muscle formation/regeneration as it has been shown to increase the number of satellite cells [32•] and stimulate muscle protein synthesis [33]. In CKD, hypogonadism is common and may be exacerbated by other common CKD comorbidities (i.e., obesity, diabetes mellitus, and hypertension) [34]. Serum testosterone levels have been associated with reduced muscle mass and strength in CKD [34, 35]. In randomized controlled trials in dialysis patients, nandrolone decanoate alone has been associated with improvements in skeletal muscle mass [36], as well as when combined with resistance exercise [37]. Longer term studies in CKD are needed, especially to establish the risk benefit ratio with androgen supplementation, given adverse events have been noted with testosterone replacement for other indications [38].
Vitamin D
Although vitamin D is largely thought of as a regulator of the bone, recent studies indicate that vitamin D may also be important in skeletal muscle maintenance and regeneration. In C2C12 myoblasts, treatment with 1,25 Vitamin D resulted in increased myogenesis [39], protein synthesis [40], and myotube diameter [41]. Conversely, vitamin D deficiency can induce muscle wasting acting primarily through the ubiquitin-proteasome pathway [42]. Overcoming vitamin D deficiency with supplementation increased muscle size and strength in patients on hemodialysis [43]. Further, supplementation increased mobility and function (i.e., the timed up and go test, gait velocity test, timed chair stand test, and stair climb test) in both CKD and dialysis patients [44]. Therefore, the prevalence of vitamin D deficiency in CKD may contribute to skeletal muscle atrophy and impaired muscle performance.
Renin-Angiotensin System
The renin-angiotensin (RAS) is upregulated in CKD [451 as well as in sarcopenia in aging [46]. This is important as angiotensin peptides (i.e., angiotensin I (Ang I), angiotensin II (Ang II)) are produced by skeletal muscle [47], but there is little to no expression of Ang I and II receptors in the muscle [48]. Despite the poor expression of Ang II receptors in adult muscle fibers, Ang II contributes directly and indirectly to muscle atrophy. Increased Ang II expression reduces the satellite cell pool and muscle regenerative capacity [49•] and upregulates caspase-3 and the ubiquitin-proteasome proteolytic pathways [50, 51]. Indirect effects of Ang II on skeletal muscle atrophy occur through intermediate molecules such as interleukin-6 that impair insulin/IGF-1 signaling and decreased Akt phosphorylation [48].
IGF/Insulin
A simplistic take upon a complex system is that, in skeletal muscle, insulin and insulin-like growth factor (IGF) interact with anabolic (extracellular response kinases (ERKs) and phosphatidylinositol 3-kinase (P13K)), and catabolic (ubiquitin-proteasome) pathways to regulate skeletal muscle mass and subsequent muscle performance. Activation of the ERK and PI3K pathways has been shown to increase proliferation [52], differentiation [53], and maintenance of muscle fiber growth [54]. In end-stage renal disease, patients develop resistance to insulin/IGF that modulates protein metabolism [55]. Protein metabolism, impaired regeneration, and increased fibrosis were demonstrated in a mouse model of CKD [31]. Growth hormone supplementation increases serum IGF-1 levels; it is used in children with CKD to normalize linear growth, and it is associated with increase in muscle mass [56]. The muscle anabolic effect of growth hormone with IGF-1 in CKD has been shown [57], including the benefits on lean muscle mass increase and fat mass reduction [58]; however, the use of growth hormone in adults with CKD and sarcopenia has not been adequately studied.
Ubiquitin-Proteasome Pathway
The ubiquitin-proteasome pathway (UPP) may interact with the IGF pathway via insulin resistance activating the UPP to promote catabolic conditions that lead to muscle atrophy in CKD [59]. In the UPP target, proteins are ubiquitinated and fed into the proteasome to be digested and degraded. Protein degradation (i.e., muscle atrophy) occurs when activated (i.e., dephosphorylated) nuclear forkhead box member (FOXOs) increases the expression of atrogin-1 and MuRF1 E3 ligases [60]. The FOXO proteins are a subgroup of the forkhead family of transcription factors; the “O” distinction indicates regulation by the insulin/PI3K/Akt pathway [61]. Of the four FOXOs (i.e., 1, 3, 4, 6), FOXO1 was identified to be the primary mediator of muscle wasting in an animal model of CKD [62]. The process degrading actomyosin complexes occurs through when caspase-3 is cleaved, then in turn is removed though the UPP. Caspase-3 is identified by the presence of an insoluble, 14 kDa remnant of actin. This biomarker has been found to increase in a number of catabolic conditions including osteoarthritis, burns, and in patients on dialysis [63].
Myostatin
Myostatin is a myokine that acts as a negative regulator of skeletal muscle mass through the upregulation of atrogenes (atrogin-1 and MuRF1) and downregulation of myogenesis genes (i.e., MyoD, myogenin) [64]. Myostatin levels are elevated in a number of diseases that demonstrate skeletal muscle wasting, including, liver disease [65], chronic obstructive pulmonary disease [66], and in CKD patients [67]. In a 5/6 nephrectomy mouse model of CKD mice, anti-myostatin treatment, a) increased body weight, muscle mass, and protein synthesis; b) reduced protein degradation; and c) improved satellite cell function [31]. In humans, drugs that bind to the myostatin receptor activin IIB have been shown to increase muscle mass and are currently in early-phase clinical trials in the elderly, offering a novel potential pharmacologic therapy to improve muscle mass [68, 69]. A trial of an anti-myostatin peptibody in CKD is currently enrolling (NCT01958970 www.clinicaltrials.gov).
Conclusion
There appears to be disruption of skeletal muscle homeostasis in CKD, with increased catabolism and decreased anabolism: the sum of these phenomena is the sarcopenia that occurs in CKD and progresses with time. Studies to unravel the pathogenesis of sarcopenia in animal models of CKD and in humans are extremely important, especially if targets for future interventions are to be identified. Clinical biomarkers of sarcopenia, i.e., measures of muscle mass, strength, and function, need to be validated overtime in CKD and related to patient-centered outcome measures such as disability, quality of life, and mortality. Ultimately, therapies that are developed will be useful and widely accepted only if they improve patient-centered outcomes of sarcopenia in CKD.
Footnotes
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest KG Avin and RN Moorthi both declare no conflicts of interest.
Contributor Information
Keith G. Avin, Indiana University School of Health and Rehabilitation Sciences, Indianapolis, IN 46202, USA
Ranjani N. Moorthi, Email: rmoorthi@iu.edu, Division of Nephrology, Department of Medicine, Indiana University School of Medicine, 950 W. Walnut St, R2-202, Indianapolis, IN 46202, USA
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
- 1.Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298(17):2038–47. doi: 10.1001/jama.298.17.2038. [DOI] [PubMed] [Google Scholar]
- 2.Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE. Functional status of elderly adults before and after initiation of dialysis. N Engl J Med. 2009;361(16):1539–47. doi: 10.1056/NEJMoa0904655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ulutas O, Farragher J, Chiu E, Cook WL, Jassal SV. Functional disability in older adults maintained on peritoneal dialysis therapy. Perit Dial Int. 2014 doi: 10.3747/pdi.2013.00293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Farragher J, Chiu E, Ulutas O, Tomlinson G, Cook WL, Jassal SV. Accidental falls and risk of mortality among older adults on chronic peritoneal dialysis. Clin J Am Soc Nephrol. 2014;9(7):1248–53. doi: 10.2215/CJN.11001013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cook WL, Tomlinson G, Donaldson M, et al. Falls and fall-related injuries in older dialysis patients. Clin J Am Soc Nephrol. 2006;1(6):1197–204. doi: 10.2215/CJN.01650506. [DOI] [PubMed] [Google Scholar]
- 6.Johansen KL, Chertow GM, Jin C, Kutner NG. Significance of frailty among dialysis patients. J Am Soc Nephrol. 2007;18(11):2960–7. doi: 10.1681/ASN.2007020221. [DOI] [PubMed] [Google Scholar]
- 7•.Bao Y, Dalrymple L, Chertow GM, Kaysen GA, Johansen KL. Frailty, dialysis initiation, and mortality in end-stage renal disease. Arch Intern Med. 2012;172(14):1071–7. doi: 10.1001/archinternmed.2012.3020. Describes the extent of frailty and its important consequences in dialysis patients. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mushnick R, Fein PA, Mittman N, Goel N, Chattopadhyay J, Avram MM. Relationship of bioelectrical impedance parameters to nutrition and survival in peritoneal dialysis patients. Kidney Int Suppl. 2003;87:S53–6. doi: 10.1046/j.1523-1755.64.s87.22.x. [DOI] [PubMed] [Google Scholar]
- 9.de Araujo Antunes A, Vannini FD, de Arruda Silveira LV, Barretti P, Martin LC, Caramori JC. Associations between bioelectrical impedance parameters and cardiovascular events in chronic dialysis patients. Int Urol Nephrol. 2013;45(5):1397–40. doi: 10.1007/s11255-012-0337-3. [DOI] [PubMed] [Google Scholar]
- 10•.Dam TT, Peters KW, Fragala M, et al. An evidence-based comparison of operational criteria for the presence of sarcopenia. J Gerontol A: Biol Med Sci. 2014;69(5):584–90. doi: 10.1093/gerona/glu013. Reviews criteria that can be used in practice to define sarcopenia. This article provides a summary of the three major classifications of sarcopenia used worldwide. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jamal SA, Leiter RE, Jassal V, Hamilton CJ, Bauer DC. Impaired muscle strength is associated with fractures in hemodialysis patients. Osteoporos Int. 2006;17(9):1390–7. doi: 10.1007/s00198-006-0133-y. [DOI] [PubMed] [Google Scholar]
- 12.West SL, Jamal SA, Lok CE. Tests of neuromuscular function are associated with fractures in patients with chronic kidney disease. Nephrol Dial Transplant. 2012;27(6):2384–8. doi: 10.1093/ndt/gfr620. [DOI] [PubMed] [Google Scholar]
- 13•.Hamrick MW. The skeletal muscle secretome: an emerging player in muscle-bone crosstalk. Bone Key Rep. 2012;1:60. doi: 10.1038/bonekey.2012.60. Provides a useful summary of the paracrine and endocrine effects of muscle on bone knowledge of the muscle-bone interaction, including areas requiring further exploration. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14•.Bowser M, Herberg S, Arounleut P, et al. Effects of the activin A-myostatin-follistatin system on aging bone and muscle progenitor cells. Exp Gerontol. 2013;48(2):290–7. doi: 10.1016/j.exger.2012.11.004. Investigated the activin A-myostatin-follistatin system in muscle and bone. They found activin A increased mineralization, and follistatin increased the proliferation of young and old primary myoblasts. While myostatin reduced proliferation in aged muscle and bone primary cells: an effect not seen in young myoblasts. Overall, myostatin is thought to impair muscle and bone progenitor cells from aged mice. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johansen KL, Kaysen GA, Young BS, Hung AM, da Silva M, Chertow GM. Longitudinal study of nutritional status, body composition, and physical function in hemodialysis patients. Am J Clin Nutr. 2003;77(4):842–6. doi: 10.1093/ajcn/77.4.842. [DOI] [PubMed] [Google Scholar]
- 16.Lopes AA, Lantz B, Morgenstern H, et al. Associations of self-reported physical activity types and levels with quality of life, depression symptoms, and mortality in hemodialysis patients: the DOPPS. Clin J Am Soc Nephrol. 2014;9(10):1702–12. doi: 10.2215/CJN.12371213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goodpaster BH, Park SW, Harris TB, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006;61(10):1059–64. doi: 10.1093/gerona/61.10.1059. [DOI] [PubMed] [Google Scholar]
- 18.Hughes VA, Frontera WR, Wood M, et al. Longitudinal muscle strength changes in older adults: influence of muscle mass, physical activity, and health. J Gerontol A: Biol Med Sci. 2001;56(5):B209–17. doi: 10.1093/gerona/56.5.b209. [DOI] [PubMed] [Google Scholar]
- 19.Fouque D, Kalantar-Zadeh K, Kopple J, et al. A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int. 2008;73(4):391–8. doi: 10.1038/sj.ki.5002585. [DOI] [PubMed] [Google Scholar]
- 20.Studenski SA, Peters KW, Alley DE, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A: Biol Med Sci. 2014;69(5):547–58. doi: 10.1093/gerona/glu010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39(4):412–23. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22•.Cesari M, Fielding RA, Pahor M, et al. Biomarkers of sarcopenia in clinical trials–recommendations from the International Working Group on Sarcopenia. J Cachex Sarcopenia Muscle. 2012;3(3):181–90. doi: 10.1007/s13539-012-0078-2. The cumulative efforts from the International Working Group on Sarcopenia. This report is helpful for those interested in sarcopenia by providing the current consensus definitions of sarcopenia. discussing the importance of muscle performance and quality, chronic disease and sarcopenia biomarkers, and applications in clinical trials and studies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23•.Roshanravan B, Robinson-Cohen C, Patel KV, et al. Association between physical performance and all-cause mortality in CKD. J Am Soc Nephrol. 2013;24(5):822–30. doi: 10.1681/ASN.2012070702. Investigates the profound consequences of loss of physical performance in CKD patients over time. This study follows patients over a relatively long period of time i.e., 3years. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.AbellanvanKan G, Rolland Y, Andrieu S, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009;13(10):881–9. doi: 10.1007/s12603-009-0246-z. [DOI] [PubMed] [Google Scholar]
- 25.Huang JW, Lien YC, Wu HY, et al. Lean body mass predicts long-term survival in Chinese patients on peritoneal dialysis. PLoS One. 2013;8(l):e54976. doi: 10.1371/journal.pone.0054976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.John SG, Sigrist MK, Taal MW, McIntyre CW. Natural history of skeletal muscle mass changes in chronic kidney disease stage 4 and 5 patients: an observational study. PLoS One. 2013;8(5):e65372. doi: 10.1371/journal.pone.0065372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Han DS, Chen YM, Lin SY, et al. Serum myostatin levels and grip strength in normal subjects and patients on maintenance haemodialysis. Clin Endocrinol (Oxf) 2011;75(6):857–63. doi: 10.1111/j.1365-2265.2011.04120.x. [DOI] [PubMed] [Google Scholar]
- 28.Turner NJ, Badylak SF. Regeneration of skeletal muscle. Cell Tissue Res. 2012;347(3):759–74. doi: 10.1007/s00441-011-1185-7. [DOI] [PubMed] [Google Scholar]
- 29.Conboy IM, Conboy MJ, Smythe GM, Rando TA. Notch-mediated restoration of regenerative potential to aged muscle. Science. 2003;302(5650):1575–7. doi: 10.1126/science.1087573. [DOI] [PubMed] [Google Scholar]
- 30.Nnodim JO. Satellite cell numbers in senile rat levator ani muscle. Mech Ageing Dev. 2000;112(2):99–111. doi: 10.1016/s0047-6374(99)00076-7. [DOI] [PubMed] [Google Scholar]
- 31.Zhang L, Wang XH, Wang H, Du J, Mitch WE. Satellite cell dysfunction and impaired IGF-1 signaling cause CKD-induced muscle atrophy. J Am Soc Nephrol. 2010;21(3):419–27. doi: 10.1681/ASN.2009060571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32•.Serra C, Tangherlini F, Rudy S, et al. Testosterone improves the regeneration of old and young mouse skeletal muscle. J Gerontol A: Biol Med Sci. 2013;68(1):17–26. doi: 10.1093/gerona/gls083. Investigated if the well-known androgen, testosterone, improves skeletal muscle regeneration. Following cardiotoxin injury to the tibialis anterior in young (2-month-old) and aged (24-month-old) male mice, testosterone increased the number of proliferating satellite cells, and the number and cross-sectional area of regenerating fibers. This study lends to potential benefit of testosterone in skeletal muscle with impaired regeneration. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Griggs RC, Kingston W, Jozefowicz RF, Herr BE, Forbes G, Halliday D. Effect of testosterone on muscle mass and muscle protein synthesis. J Appl Physiol. 1989;66(1):498–503. doi: 10.1152/jappl.1989.66.1.498. [DOI] [PubMed] [Google Scholar]
- 34.Carrero JJ, Qureshi AR, Nakashima A, et al. Prevalence and clinical implications of testosterone deficiency in men with end-stage renal disease. Nephrol Dial Transplant. 2011;26(1):184–90. doi: 10.1093/ndt/gfq397. [DOI] [PubMed] [Google Scholar]
- 35.Cigarran S, Pousa M, Castro MJ, et al. Endogenous testosterone, muscle strength, and fat-free mass in men with chronic kidney disease. J Ren Nutr. 2013;23(5):e89–95. doi: 10.1053/j.jrn.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 36.Johansen KL, Mulligan K, Schambelan M. Anabolic effects of nandrolone decanoate in patients receiving dialysis: a randomized controlled trial. JAMA. 1999;281(14):1275–81. doi: 10.1001/jama.281.14.1275. [DOI] [PubMed] [Google Scholar]
- 37.Johansen KL, Painter PL, Sakkas GK, Gordon P, Doyle J, Shubert T. Effects of resistance exercise training and nandrolone decanoate on body composition and muscle function among patients who receive hemodialysis: a randomized, controlled trial. J Am Soc Nephrol. 2006;17(8):2307–14. doi: 10.1681/ASN.2006010034. [DOI] [PubMed] [Google Scholar]
- 38.Borst SE, Shuster JJ, Zou B, et al. Cardiovascular risks and elevation of serum DHT vary by route of testosterone administration: a systematic review and meta-analysis. BMC Med. 2014;12:211. doi: 10.1186/s12916-014-0211-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Garcia LA, Ferrini MG, Norris KC, Artaza JN. 1,25(OH)(2)vitamin D(3) enhances myogenic differentiation by modulating the expression of key angiogenic growth factors and angiogenic inhibitors in C(2)C(12) skeletal muscle cells. J Steroid Biochem Mol Biol. 2013;133:1–11. doi: 10.1016/j.jsbmb.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Salles J, Chanet A, Giraudet C, et al. 1,25(OH)2-vitamin D3 enhances the stimulating effect of leucine and insulin on protein synthesis rate through Akt/PKB and mTOR mediated pathways in murine C2C12 skeletal myotubes. Mol Nutr Food Res. 2013;57(12):2137–46. doi: 10.1002/mnfr.201300074. [DOI] [PubMed] [Google Scholar]
- 41.Girgis CM, Clifton-Bligh RJ, Mokbel N, Cheng K, Gunton JE. Vitamin D signaling regulates proliferation, differentiation, and myotube size in C2C12 skeletal muscle cells. Endocrinology. 2014;155(2):347–57. doi: 10.1210/en.2013-1205. [DOI] [PubMed] [Google Scholar]
- 42.Bhat M, Kalam R, Qadri SS, Madabushi S, Ismail A. Vitamin D deficiency-induced muscle wasting occurs through the ubiquitin proteasome pathway and is partially corrected by calcium in male rats. Endocrinology. 2013;154(11):4018–29. doi: 10.1210/en.2013-1369. [DOI] [PubMed] [Google Scholar]
- 43.Gordon PL, Sakkas GK, Doyle JW, Shubert T, Johansen KL. Relationship between vitamin D and muscle size and strength in patients on hemodialysis. J Ren Nutr. 2007;17(6):397–407. doi: 10.1053/j.jrn.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Taskapan H, Baysal O, Karahan D, Durmus B, Altay Z, Ulutas O. Vitamin D and muscle strength, functional ability and balance in peritoneal dialysis patients with vitamin D deficiency. Clin Nephrol. 2011;76(2):110–6. doi: 10.5414/cn107160. [DOI] [PubMed] [Google Scholar]
- 45.Graziani G, Badalamenti S, Del Bo A, et al. Abnormal hemodynamics and elevated angiotensin II plasma levels in polydipsic patients on regular hemodialysis treatment. Kidney Int. 1993;44(1):107–14. doi: 10.1038/ki.1993.219. [DOI] [PubMed] [Google Scholar]
- 46.Wray DW, Nishiyama SK, Harris RA, Richardson RS. Angiotensin II in the elderly: impact of angiotensin II type 1 receptor sensitivity on peripheral hemodynamics. Hypertension. 2008;51(6):1611–6. doi: 10.1161/HYPERTENSIONAHA.108.111294. [DOI] [PubMed] [Google Scholar]
- 47.Danser AH, Koning MM, Admiraal PJ, et al. Production of angiotensins I and II at tissue sites in intact pigs. Am J Physiol. 1992;263(2 Pt 2):H429–37. doi: 10.1152/ajpheart.1992.263.2.H429. [DOI] [PubMed] [Google Scholar]
- 48.Zhang L, Du J, Hu Z, et al. IL-6 and serum amyloid A synergy mediates angiotensin II-induced muscle wasting. J Am Soc Nephrol. 2009;20(3):604–12. doi: 10.1681/ASN.2008060628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49•.Yoshida T, Galvez S, Tiwari S, et al. Angiotensin II inhibits satellite cell proliferation and prevents skeletal muscle regeneration. J Biol Chem. 2013;288(33):23823–32. doi: 10.1074/jbc.M112.449074. Explored if skeletal muscle regeneration is impaired by increased expression of angiotensin II. This is important because angiotensin II is often increased in CKD patients. They found using in vitro and in vivo techniques, that angiotensin does impair regeneration; resulting in a reduced number of regenerating myofibers and decreased expression of myogenic-related factors. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sanders PM, Russell ST, Tisdale MJ. Angiotensin II directly induces muscle protein catabolism through the ubiquitin-proteasome proteolytic pathway and may play a role in cancer cachexia. Br J Cancer. 2005;93(4):425–34. doi: 10.1038/sj.bjc.6602725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Song YH, Li Y, Du J, Mitch WE, Rosenthal N, Delafontaine P. Muscle-specific expression of IGF-1 blocks angiotensin II-induced skeletal muscle wasting. J Clin Invest. 2005;115(2):451–8. doi: 10.1172/JCI22324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Coolican SA, Samuel DS, Ewton DZ, McWade FJ, Florini JR. The mitogenic and myogenic actions of insulin-like growth factors utilize distinct signaling pathways. J Biol Chem. 1997;272(10):6653–62. doi: 10.1074/jbc.272.10.6653. [DOI] [PubMed] [Google Scholar]
- 53.Tureckova J, Wilson EM, Cappalonga JL, Rotwein P. Insulin-like growth factor-mediated muscle differentiation: collaboration between phosphatidylinositol 3-kinase-Akt-signaling pathways and myogenin. J Biol Chem. 2001;276(42):39264–70. doi: 10.1074/jbc.M104991200. [DOI] [PubMed] [Google Scholar]
- 54.Lewis MI, Horvitz GD, Clemmons DR, Foumier M. Role of IGF-I and IGF-binding proteins within diaphragm muscle in modulating the effects of nandrolone. Am J Physiol Endocrinol Metab. 2002;282(2):E483–90. doi: 10.1152/ajpendo.00191.2001. [DOI] [PubMed] [Google Scholar]
- 55.da Costa JAC, Ikizler TA. Inflammation and insulin resistance as novel mechanisms of wasting in chronic dialysis patients. Semin Dial. 2009;22(6):652–7. doi: 10.1111/j.1525-139X.2009.00664.x. [DOI] [PubMed] [Google Scholar]
- 56.Mahan JD, Warady BA, Consensus C. Assessment and treatment of short stature in pediatric patients with chronic kidney disease: a consensus statement. Pediatr Nephrol. 2006;21(7):917–30. doi: 10.1007/s00467-006-0020-y. [DOI] [PubMed] [Google Scholar]
- 57.Guebre-Egziabher F, Juillard L, Boirie Y, Laville M, Beaufrere B, Fouque D. Short-term administration of a combination of recombinant growth hormone and insulin-like growth factor-1 induces anabolism in maintenance hemodialysis. J Clin Endocrinol Metab. 2009;94(7):2299–305. doi: 10.1210/jc.2008-2262. [DOI] [PubMed] [Google Scholar]
- 58.Hansen TB, Gram J, Jensen PB, et al. Influence of growth hormone on whole body and regional soft tissue composition in adult patients on hemodialysis. A double-blind, randomized, placebo-controlled study. Clin Nephrol. 2000;53(2):99–107. [PubMed] [Google Scholar]
- 59.Siew ED, Pupim LB, Majchrzak KM, Shintani A, Flakoll PJ, Ikizler TA. Insulin resistance is associated with skeletal muscle protein breakdown in non-diabetic chronic hemodialysis patients. Kidney Int. 2007;71(2):146–52. doi: 10.1038/sj.ki.5001984. [DOI] [PubMed] [Google Scholar]
- 60.Sandri M, Sandri C, Gilbert A, et al. Foxo transcription factors induce the atrophy-related ubiquitin ligase atrogin-1 and cause skeletal muscle atrophy. Cell. 2004;117(3):399–412. doi: 10.1016/s0092-8674(04)00400-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Carter ME, Brunet A. FOXO transcription factors. Curr Biol. 2007;17(4):R113–4. doi: 10.1016/j.cub.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 62.Xu J, Li R, Workeneh B, Dong Y, Wang X, Hu Z. Transcription factor FoxOl, the dominant mediator of muscle wasting in chronic kidney disease, is inhibited by microRNA-486. Kidney Int. 2012;82(4):401–11. doi: 10.1038/ki.2012.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Workeneh BT, Rondon-Berrios H, Zhang L, et al. Development of a diagnostic method for detecting increased muscle protein degradation in patients with catabolic conditions. J Am Soc Nephrol. 2006;17(11):3233–9. doi: 10.1681/ASN.2006020131. [DOI] [PubMed] [Google Scholar]
- 64.Elkina Y, von Haehling S, Anker SD, Springer J. The role of myostatin in muscle wasting: an overview. J Cachex Sarcopenia Muscle. 2011;2(3):143–51. doi: 10.1007/s13539-011-0035-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Garcia PS, Cabbabe A, Kambadur R, Nicholas G, Csete M. Brief-reports: elevated myostatin levels in patients with liver disease: a potential contributor to skeletal muscle wasting. Anesth Analg. 2010;111(3):707–9. doi: 10.1213/ANE.0b013e3181eac1c9. [DOI] [PubMed] [Google Scholar]
- 66.Ju CR, Chen RC. Serum myostatin levels and skeletal muscle wasting in chronic obstructive pulmonary disease. Respir Med. 2012;106(1):102–8. doi: 10.1016/j.rmed.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 67.Verzola D, Procopio V, Sofia A, et al. Apoptosis and myostatin mRNA are upregulated in the skeletal muscle of patients with chronic kidney disease. Kidney Int. 2011;79(7):773–82. doi: 10.1038/ki.2010.494. [DOI] [PubMed] [Google Scholar]
- 68.Hamrick MW, Arounleut P, Kellum E, Cain M, Immel D, Liang LF. Recombinant myostatin (GDF-8) propeptide enhances the repair and regeneration of both muscle and bone in a model of deep penetrant musculoskeletal injury. J Trauma. 2010;69(3):579–83. doi: 10.1097/TA.0b013e3181c451f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Attie KM, Borgstein NG, Yang Y, et al. A single ascending-dose study of muscle regulator ACE-031 in healthy volunteers. Muscle Nerve. 2013;47(3):416–23. doi: 10.1002/mus.23539. [DOI] [PubMed] [Google Scholar]