Abstract
Background
Mental disorders account for considerable suffering and societal burden. Prospective alternative decision-makers may be engaged in helping make treatment decisions for those who live with serious mental disorders. Little is known about the ways in which alternative decision makers arrive at treatment recommendations and whether the perspectives of alternative decision makers and ill individuals are aligned.
Methods
The authors queried community-dwelling individuals diagnosed with schizophrenia, anxiety, or mood disorders and their preferred alternative decision-makers on issues regarding treatment decisions and underlying ethically-salient perspectives using a written survey instrument. Complete data were obtained on 26 pairs (n=52, total). Outcomes included perspectives on clinical decision-making and underlying values that may shape their life choices. Two-sided paired t-tests and graphical representations were used.
Results
We found that preferred alternative decision-makers overall accurately predicted the views of ill individuals with respect to the role of the individual and of family in treatment decision making. Preferred alternative decision-makers slightly overestimated autonomy-related perspectives. The personal views of ill individuals and preferred alternative decision-makers were aligned with respect to different physical and mental disorders, except in relation to alcohol and substance use where alternative decision-makers placed greater emphasis on autonomy. Alignment was also discovered on underlying life values, except the role of spirituality which was greater among alternative decision-makers.
Conclusion
Preferred alternative decision-makers are an ethical safeguard to ensure the wellbeing and rights of seriously ill individuals. In this pilot study, preferred alternative decision makers were aligned with their ill family members concerning treatment-related decisions and underlying life values. Future research should continue to explore and clarify the views of ill individuals and alternative decision makers to determine the quality of this safeguard used in clinical settings.
Mental disorders cause great suffering and represent the second-leading cause of years of life lost to disability and premature mortality throughout the world – first leading among economically WHO established countries (WHO, 2011). The need to discover the causes and most effective treatments of mental disorders is a global health imperative and it is increasingly recognized. Schizophrenia is among the most devastating of all mental and physical health conditions, and the 1% of the world’s population who live with this condition may experience periods of diminished or compromised decisional capacity (American Psychiatric Association, 2013). Anxiety and mood disorders, similarly, account for 10% of the total burden of all mental, neurological, and substance use disorders as measured by disability-adjusted life years, and may be characterized by periods of uncertainty, emotional lability, and cognitive distortions, which can compromise the ability to provide authentic informed consent for treatment decisions (Cassem et al., 1998; Carpenter et al., 2000; Dunn et al., 2006; President’s National Bioethics Advisory Commission Report, 1998).
Clinicians routinely engage family members and others involved in the lives of people with mental disorders regarding their health care decisions (Dunn et al., 2011; Dunn et al., 2013; Overton et al., 2013). These individuals may become alternative decision-makers in clinical situations, a safeguard relied upon clinically and legally to protect the wellbeing and rights of the seriously ill (Roberts and Dyer, 2004). In an ethical framework, alternative decision-makers may follow two different approaches or legal standards. One approach is to try to identify what the patient himself or herself would choose (“substituted judgment”), and the other approach seeks to protect and advance the objective interests of the patient (“best interests”). The substituted judgment approach emphasizes individual autonomy whereas the best interests approach emphasizes anticipated benefit and minimization of risk. Little is known about the attitudes of individuals who may undertake the role of alternative decision-maker and how well aligned their views are with ill individuals. Moreover, little guidance exists to help alternative decision-makers as they shoulder this important responsibility.
To better understand the views of community-residing individuals diagnosed with psychotic, mood, and anxiety disorders, we conducted a novel pilot study to evaluate if their personal perspectives were similar to (“alignment”) and well understood by (“attunement”) the individuals whom they preferred to serve as their alternative decision-makers. We queried ill individuals regarding several attitudes and issues that are salient to the process of alternative decision making, such as the role of the ill individual and of family in arriving at treatment decisions. In addition, we asked specifically about the importance of autonomy and the role of family members and other stakeholders across several mental health conditions. We also asked about ethically important values shaping aspects of one’s personal life that may have salience for treatment decisions.
To test alignment, we compared the views of the ill individuals and their linked preferred alternative decision-maker for similarities and differences. To test attunement, we asked the preferred alternative decision-makers to predict the beliefs of the ill individual for whom he or she might be entrusted with decision making. In this report, we present a descriptive and unique graphical summary of our findings.
METHODS
The National Alliance for Research on Schizophrenia and Depression and the National Institute of Mental Health (K02 MH001918) funded this IRB-approved project. Informed consent was carefully obtained through verbal and written procedures.
Survey Instrument
A new written survey instrument was developed for this project, as described in further detail in Roberts and Kim (2015), and was informed by community-based participatory research methods (Roberts et al., 2013). The written survey was based on prior work in the area of informed consent and alternative decision-making (Roberts et al., 2000; Roberts, 2002, Roberts et al. 2004).
The survey consisted of 63 items overall, with 8 items on the characteristics of the dyad relationship, 13 items of demographic and background information, 20 items on decisions related to treatment, and 22 items on decisions related to research. One survey form was administered to ill individuals, and a parallel version of the survey was administered to alternative decision-makers. Items were rated on a 9-point scale ranging from not at all important (1) to very important (9). Data presented here are based on responses to Likert-scaled attitude items and participant background information.
Study population
Eligible adults included those who were invited via printed ads that were circulated through the local chapter at the National Alliance of Mental Illness in Albuquerque, NM, and posted at the University of New Mexico Mental Health Center, the Albuquerque Veterans Administration (VA) Medical Center, and/or community mental health organizations. We conducted the written survey at a routine evening meeting at the invitation of a local chapter of the National Alliance for the Mentally Ill in the community of Albuquerque, New Mexico, and in convenient locations nearby.
Of the 39 complete pairs who expressed interest in participating, 27 pairs fully consented to participate in this study. For analysis, 1 record was excluded from the final analytic cohort.
Outcome measures
Ill individuals and linked preferred alternative decision-makers were queried on their perspectives pertaining to three domains.
Domain 1
Ill individuals were asked to rate the importance of several issues in relation to treatment decisions. These issues fell into two categories: issues related to the role of the individual, and issues related to the role of the family. The former category included the questions on the importance of: “including the ill individual in treatment decisions”, “ill individual is free to do what he wants”, and “ill individual is able to decide to continue or stop treatment”. The second category included questions on the importance of: “including family members in decisions”, “family’s understanding of how the treatment will affect patient”, “family having to take care of ill individual during the treatment”, “what family recommends”, and “family able to decide to continue or stop treatment”. Preferred alternative decision-makers were then asked to predict the perspectives of the ill person to whom they were linked, thus allowing us to compare the predictions of the alternative decision-makers to the actual perspectives of the ill individuals (“attunement”).
Domain 2
Ill individuals and preferred alternative decision-makers were asked about the importance of family members and other stakeholders in clinical decisions related to different health conditions. They were asked: “How important is it for the following people to be involved in making treatment decisions?” in the following health conditions: serious physical illness, serious mental illness, serious alcohol abuse, serious drug abuse, Alzheimer’s disease, and developmental disability. Responses related to personal views, thus allowing the comparison of personal perspectives (“alignment”).
Domain 3
Ill individuals and preferred alternative decision-makers were asked to rate the importance of several ethically-important issues and values shaping every day life. These issues were organized into 5 main themes: trust and respect, autonomy, comfort and compassion, issues related to responsibility to others, and religious or spirituality related issues. Responses related to personal perspectives, thus allowing the comparison of personal perspectives (“alignment”).
All responses were measured on a 9-point Likert scale.
Statistical analysis
Statistical aims
Our aims were to assess attunement in domain 1, and alignment in domains 2 and 3.
Tools
We used two sample t-tests and Pearson’s Chi-squared tests as appropriate.
Software
We used R (version 3.0.0, GNU project) for all statistical analyses.
RESULTS
Characteristics of respondents (Table 1)
Table 1.
Characteristics of participants
| Individuals living with mental illness† N = 26 |
Preferred Alternative Decision-maker N = 26 |
p-value | |
|---|---|---|---|
| Living with | |||
| Psychosis symptoms | 77% (20) | – | N/A |
| Mood or anxiety symptoms | 23% (6) | – | |
| Gender | |||
| Women | 15% (4) | 73% (19) | P < 0.0011 |
| Men | 81% (21) | 27% (7) | |
| Mean age in years* | 35 (10) | 52 (17) | P = 0.0012 |
| Ethnicity** | |||
| American Indian or Alaskan | 0% (0) | 5% (1) | P = 1.001 |
| White | 58% (15) | 54% (14) | |
| Other | 35% (9) | 31% (8) | |
| Currently living*** | |||
| Alone | 42% (11) | 4% (1) | P < 0.0011 |
| With family | 49% (10) | 81% (21) | |
| With friends | 3% (1) | 12% (3) | |
| Group home or halfway house | 4% (1) | 0% (0) | |
| Marital Status†† | |||
| Single | 70% (18) | 12% (3) | P < 0.0011 |
| Divorced or widowed | 8% (2) | 23% (6) | |
| Married or living with partner | 15% (4) | 65% (17) | |
m = number of missing observations = 4
Preferred Alternative Decision-makers, m = 2; ill individuals, m = 2
Preferred Alternative Decision-maker, m = 1; and ill individual, m = 3
Community-dwelling Individuals living with psychosis, mood or anxiety disorder by self-report
Ill individual, m = 2
Tests used:
Fisher’s test;
t-test
Complete data were obtained from 26 dyads, consisting of 20 individuals with schizophrenia and 6 individuals with other psychosis or mood/anxiety disorder, and the linked preferred alternative decision-makers of these 26 individuals. Of these, half were queried at the National Alliance for the Mentally Ill evening meeting, and the other half at sites nearby. Our volunteers with symptoms of anxiety and schizophrenia were mostly men (21, 81%) with a mean age of 35 years (sd = 10 years). Alternative decision-maker volunteers included were mostly women (19, 73%), with a mean age of 52 years (sd = 17 years). Other characteristics of dyads are presented in Table 1.
Overall trends
Among the highest issues of priority to patients were issues related to the “patient’s ability to take care of [ones] self during treatment” [means; 7.9 (2.1), 8.2 (1.5)], and “patient’s understanding of how the treatment will affect patient” [means: 7.8 (2.0), 8.0 (1.4)], and “patient having a good relationship with family” [means” 7.8 (1.9); 8.2 (1.3)]. Interestingly, for preferred alternative decision-makers, there were several issues that mattered more relating to autonomy: “patient being free to do what he wants” (mean = 8.8 (0.4)), “patient’s ability to do normal things” (mean = 8.3 [1.2]), “patient able to decide to continue or stop treatment” (means = 8.3 (1.0)), and “patient being a productive member of society.” There was a significant difference between ill patients and their linked preferred alternative decision-makers in the way they viewed “patient being free to do what he wants.” (ill patient mean= 7.5 [2.3]; p-value = 0.01). Not surprisingly, preferred alternative decision-makers also highly valued “chance for symptom improvement” and “hope for a cure” (means 8.2, 7.7, respectively).
Of least importance to ill individuals, among all issues queried, was that of “treatment costs to patient or family” and of “family able to decide to continue or stop treatment” (means = 6.4 [2.8], 6.0 [2.8]). Of least importance to preferred alternative decision-makers were the issues “treatment costs to patient or family” and “family having to take care of patient during the treatment” (means = 6.9 [2.4], 6.6 [2.5]).
Respondents were also queried on a range of issues relating to treatment decisions, i.e. importance of a certain issue to themselves for treatment decisions relating to the ill individual. A majority of issues were rated similarly and highly. Among the top rated issues were “doctors serve best interests of ill person”, “skill and knowledge of research doctor”, “include ill person in decisions”, “privacy protection efforts”, “quality of clinic or hospital”, “ethical and moral standards of research doctor”, and “doctor establish trust with ill person” [range of means = (8.2, 8.6) ill; (8.0,8.6) ADM]. Of least importance to the ill patient was the issue “doctor serve best interests of family” (mean 6.9 [2.6]) and to the preferred alternative decision-maker was the issue “source of payment” (6.9 [2.6]).
I. Attunement of perspectives of individuals living with mental illness and the predictions of their linked preferred alternative decision-makers regarding the role of the individual and the family on treatment decisions (Table 2)
Table 2.
Perspectives of individuals living with mental illness and attitudes as predicted by their preferred alternative decision-makers
| Attitudes expressed by Ill individuals† | Preferred alternative decision maker predictions of attitudes expressed by ill individuals†† | ||||
|---|---|---|---|---|---|
|
| |||||
| Importance of issue in relation to treatment decisions* | mean | sd | mean | sd | p-value |
| Issues related to the role of the ill individual | |||||
| include ill person in decisions | 8.5 | (0.8) | 8.6 | (0.6) | 0.76 |
| ill person free to do what he wants | 7.5 | (2.3) | 8.8 | (0.4) | 0.01** |
| ill person able to decide to continue or stop treatment | 7.2 | (2.7) | 8.3 | (1.0) | 0.09 |
| Overall mean*** | 7.7 | (0.7) | 8.6 | (0.3) | 0.15 |
| Issues related to the role of family | |||||
| include family members in decisions | 7.3 | (1.7) | 7.8 | (1.7) | 0.13 |
| family’s understanding of how the treatment will affect ill person | 7.1 | (2.5) | 6.9 | (2.4) | 0.74 |
| family having to take care of ill person during the treatment | 6.9 | (2.3) | 6.6 | (2.5) | 0.60 |
| what family recommends | 6.8 | (1.7) | 7.1 | (2.0) | 0.15 |
| family able to decide to continue or to stop treatment | 6.0 | (2.8) | 6.9 | (2.4) | 0.13 |
| Overall mean** | 6.8 | (0.5) | 7.1 | (0.5) | 0.34 |
1 missing observation from ill individual;
1 missing observation from alternative decision maker
Items were rated on a 9-point scale ranging from “not at all important” = 1 to “very important” = 9
Statistically significant with α = 0.05
Accuracy of prediction by preferred alternative decision makers of people with mental illness regarding treatment decisions, as evidenced by lack of differences
With respect to the role of the ill individual in making treatment decisions, ill individuals and the predictions of preferred alternative decision-makers ranked issues differently yet both highly endorsed the theme of autonomy. Respondents expressed strong endorsement of a range of issues related to the role of the ill individual (range of means [7.2, 8.8]). Ill people living with mental illness ranked “includ[ing] the ill person in decisions” as the most important issue (mean 8.5 sd =[0.8]), followed by “ill individual being free to do what [he] wants” (mean 7.5 sd =[2.3]), and finally “ill person able to decide to continue or stop treatment” (mean 7.5 sd =[2.3]). Preferred alternative decision-makers predicted that ill individuals would endorse the issue “ill person being free to do what [he] wants” (mean 8.8, sd [0.4]) on a greater level than the ill individuals themselves (p=0.01). They also ranked the issues “ill individual being free to do what [he] wants” and “ill person able to decide to continue or stop treatment” highly (means 8.3 [0.4]; 8.3 [1.0]).
To a lesser degree, ill respondents expressed moderate to strong endorsement of a range of issues related to the role of the family in treatment decisions (range of means [6.0, 7.1]). They ranked “include family members in decisions” (mean 7.3 [1.7]) as the most important issue in this group, followed by “family’s understanding of how the treatment will affect ill individuals” (mean 7.1 [2.5]), “family having to take care of ill individual during the treatment” (mean 6.9 [2.3]), and “what family recommends” (mean 6.8 [1.7]). The issue garnering least endorsement was “family able to decide to continue or to stop treatment” (mean 6.0 sd [2.8]).
Preferred alternative decision-makers similarly expressed moderate to strong endorsement of a range of issues related to the role of the family (range of means [6.9, 7.9]). Preferred alternative decision-makers also ranked “include family members in decisions” (mean 7.8 [1.7]) as the most important issue in this group, followed by “what family recommends” (mean 7.1 [2.0]), and “family’s understanding of how the treatment will affect ill individuals” (mean 6.9 [2.4]), along with “family able to decide to continue or to stop treatment” (mean 6.9 sd [2.4]). Ranked lower than these issues was the importance of the issue “family having to take care of ill individual during the treatment” (mean 6.6 [2.5]).
Table 2 indicates the accuracy of prediction of preferred alternative decision-makers of people with mental illness regarding treatment decisions, i.e., attunement.
II. Alignment of perspectives of ill individuals and their preferred alternative decision-makers regarding treatment decisions made in the context of different health conditions (Figure 1)
Figure 1.
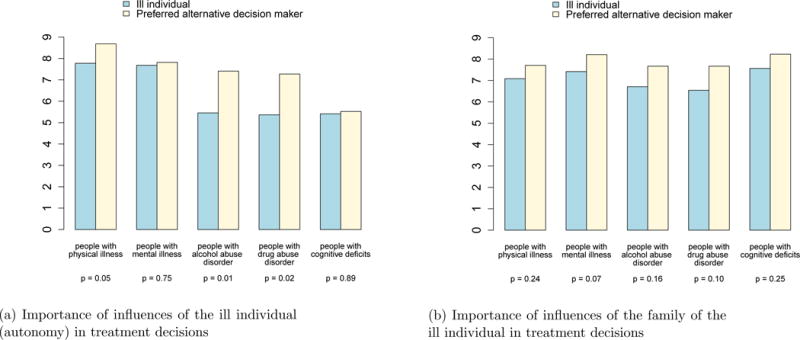
Alignment of perspectives of ill individuals and their preferred alternative decision-makers regarding the role of influences on treatment decisions made by people living with different health conditions
Ill individuals and their preferred alternative decision-makers were aligned in their perspectives regarding the role of the ill individual (autonomy) in treatment decisions for people with different health conditions with the exception of health conditions related to alcohol or drug abuse disorder (p-values 0.01, 0.02 respectively). Preferred alternative decision-makers of people with mental illness more greatly endorse the importance of autonomy for those people with alcohol or drug abuse disorder than did mentally ill individuals (means = 7.4 vs 5.5; 7.3 vs 5.4; p-values = 0.01, 0.02 respectively).
Ill individuals and their preferred alternative decision-makers were aligned in their perspectives regarding the role of autonomy in treatment decisions for people with different health conditions. The importance of the influence of family of the ill individual in treatment decisions was uniformly endorsed regardless of the kind of health condition (all p-values > 0.05).
Figure 1 graphically reflects the alignment in attitudes regarding the importance of influence of the family of the ill individual in treatment decisions in different health conditions.
III. Alignment of perspectives of ill individuals and their preferred alternative decision-makers regarding ethically-important issues and values in their lives generally (Figure 2)
Figure 2.
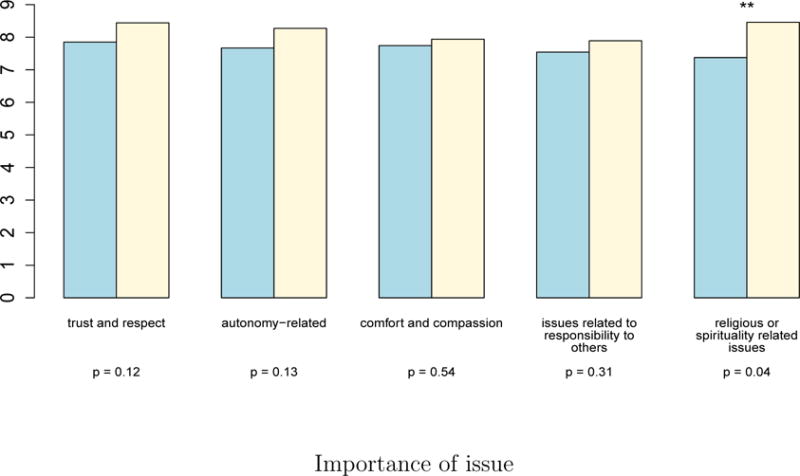
Alignment of perspectives of ill individuals and their preferred alternative decision makers regarding ethically-important issues in their lives generally
Ill individuals and their preferred alternative decision-makers were aligned in their perspectives regarding ethically important issues in their lives in general. That is, ill individuals and their preferred alternative decision-makers were aligned with respect to “trust and respect”, “autonomy”, “comfort and compassion”, as well as issues related to “responsibility to others” (p-values > 0.05). The one exception to this trend was that preferred alternative decision-makers more greatly endorsed religious or spirituality related issues than did their linked ill individuals (p-value = 0.04).
Figure 2 graphically reflects the alignment in attitudes regarding the importance of ethically-important issues generally.
DISCUSSION
This study, though preliminary by its nature, is to our knowledge the first to examine the views held by community-dwelling individuals diagnosed with mood/anxiety disorder or schizophrenia and those of their preferred potential alternative decision-makers, focusing specifically on treatment decision-making Our goal was to assess the attunement and alignment of potential alternative decision-makers with respect to the preferences of ill individuals regarding many issues that are vital to clinical care choices. We queried study volunteers regarding the role of the ill individual and the role of family in making treatment decisions, differences in views depending on the nature of the health condition, and the importance of principles and values such as trust and respect, autonomy, comfort and compassion, responsibility to others, and religious or spirituality-related issues. It is rare to have data from a project in which a decisionally-capable mentally ill person and his or her preferred alternative decision-maker have been queried and their responses compared. These findings have genuine salience for the ethical safeguard of alternative decision-making that is employed routinely in clinical practice and relied upon by law, but without much evidence base to support whether the standard of substituted judgment is fulfilled or feasible.
The perspectives of mentally ill individuals regarding the role of the ill person and of family members in treatment decisions were well understood by their preferred alternative decision-makers in this study. Alternative decision-makers accurately predicted responses to all but one issue we queried, affirming the importance of the ill individual and of the family being included in treatment decisions, of the ill individual being able to decide to continue or stop treatment, the family’s understanding of how the treatment will affect the ill individual, the role of the family in caring for the ill individual, and the influence of the family’s recommendations and choices regarding continuing or stopping treatment. The one exception where preferred alternative decision-makers did not accurately predict ill individuals’ views related to the concept of personal autonomy: ill individuals in this pilot study did not as strongly endorse the statement that an ill individual is “free to do what he wants” as was predicted by the preferred alternative decision-makers. This finding in which ill individuals are less vehement about individual freedom was documented in a prior study where physicians similarly overestimated the value schizophrenia patients placed on autonomy (Roberts et al., 2000). This degree of attunement is striking. Furthermore, this finding lends support to the idea that substituted judgment is feasible amongst at least a subset of preferred alternative decision-makers of individuals with mental disorders.
Very few differences in personal views of ill individuals and their preferred alternative decision-makers were identified when we examined responses to different health conditions. Overall, ill individuals and their preferred alternative decision-makers assessed similarly the degree of importance of autonomy and of the role of family for physical and mental illness, addiction conditions, and conditions characterized by cognitive deficits. Both ill individuals and preferred alternative decision-makers endorsed the importance of family influence upon treatment decisions. For decisions related to physically ill populations and populations with either drug or alcohol abuse, individual autonomy was more strongly endorsed as important by preferred alternative decision-makers than by the individuals with mental illness in this study.
Even more impressive was the alignment of personal views held by ill individuals and their preferred alternative decision-makers regarding the importance of ethical principles and values such as comfort and compassion, trust and respect, autonomy, and personal accountability. It is intriguing that the one area of difference in this domain pertained to religious attitudes and spirituality, which was important to ill individuals but was endorsed more strongly by the alternative decision-makers. This topic should be explored further given that religious values may greatly affect treatment choices, such as end of life care. The differences we found should be examined. It may be that those individuals who are drawn to the alternative decision-maker role, and who are trusted by others, hold religious attitudes and spirituality more dear. This finding suggests the salience of physicians’ efforts to foster dialogue with patients and potential alternative decision-makers, particularly on those matters where religious beliefs may be highly relevant to clinical care choices and therapeutic goals.
Our findings have important implications for patient-centered clinical care practices involving individuals living with mental disorders. Individuals with mental disorders are often at life-long risk for recurrence or progression of their conditions, and they are also at risk for co-occurring disorders. Patient-centered clinical care emphasizes the perspectives, preferences, and values of the ill individual, and may involve extensive family engagement in clinical decision-making. Our study reaffirms the value of speaking with patients about their wishes and, with their consent, of inviting others into the dialogue. Ideally, clinicians will clarify with their patients the importance placed on personal independence or autonomy in relation to other values. The impact of religious values in key decisions related to reproductive health or end-of-life interventions should also be explored explicitly in an effort to fulfill the goals of patient-centered care. Psychiatric advance directives may prove to be a useful exercise in care when working with patients who experience periods of diminished decisional capacity. As a patient-centered safeguard that is underutilized despite support amongst clinicians, researchers, and bioethicists, a psychiatric advance directive need not be highly elaborate, but can be a useful starting point for generating dialogue that is needed.
Our results hold promise with respect to establishing an empirical basis for the substituted judgment standard for alternative decision-making, but this study should properly be viewed as preliminary. Its limitations include the fact that the participants were not a random sample and that men and people living with schizophrenia were the majority of ill patients in this study. We suggest that this study adds important empirical findings to the literature, a body of scholarship which has yet to characterize the views of people living with mental illness and who commonly need to rely on others to help with or make decisions regarding treatment. This project should serve as a springboard for future studies that help provide a deeper evidence base regarding the views of stakeholders in clinical care and optimal practices for training physicians to engage in optimal patient-centered care.
Highlights.
We surveyed people with schizophrenia or anxiety and mood disorder and their preferred alternative decision-makers.
We examined the attunement and alignment of perspectives between dyads.
Both groups were attuned with respect to the role of the individual and of family in treatment decision making.
Views of both groups were aligned with respect to different physical and mental disorders, except in relation to alcohol and substance use.
Both groups were aligned in their views of underlying life values, except the role of spirituality.
Acknowledgments
The authors gratefully acknowledge the National Alliance for Research on Schizophrenia and Depression, the National Institute on Mental Health, and NAMI-Albuquerque. We also express our thanks to Teddy Warner, Ph.D., who provided consultation on the instrument used in this project.
This IRB-approved project was funded in part by the National Alliance for Research on Schizophrenia and Depression and by NIMH K02 MH001918.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
My coauthor and I have no conflicts of interest to disclose.
Author Dr. Laura Roberts designed the study and wrote the protocol, managed the literature searches and analyses. Author Dr. Jane Kim managed and undertook the statistical analyses, and Dr. Laura Roberts wrote the first draft of the manuscript. Both authors contributed to and have approved the final manuscript.
Contributor Information
Laura Weiss Roberts, Chairman and Katharine Dexter McCormick and Stanley McCormick Memorial Professor, Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine
Jane Paik Kim, Instructor, Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. American Psychiatric Publishing; Washington, DC: 2013. [Google Scholar]
- Carpenter WT, Gold JM, Lahti AC, et al. Decisional capacity for informed consent in schizophrenia research. Archives of General Psychiatry. 2000;57(6):533–538. doi: 10.1001/archpsyc.57.6.533. [DOI] [PubMed] [Google Scholar]
- Cassem N, Jeste DV, Roberts LW, et al. Research involving individuals with questionable capacity to consent: ethical issues and practical considerations for institutional review boards (IRBs) Expert Panel Report to the National Institutes of Health (NIH); 1998. [Google Scholar]
- Dunn LB, Candilis PJ, Roberts LW. Emerging empirical evidence on the ethics of schizophrenia research. Schizophr Bull. 2006;32(1):47–68. doi: 10.1093/schbul/sbj012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn LB, Fisher SR, Hantke M, et al. “Thinking about it for somebody else”: Alzheimer’s disease research and proxy decision-makers’ translation of ethical principles into practice. Am J Geriatr Psychiatry. 2013;21(4):337–345. doi: 10.1016/j.jagp.2012.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn LB, Hoop JG, Misra S, Fisher SR, Roberts LW. “A feeling that you’re helping”: proxy decision making for Alzheimer’s research. Narrative Inquiry in Bioethics. 2011;1(2):107–122. doi: 10.1353/nib.2011.0034. [DOI] [PubMed] [Google Scholar]
- Jaworska A. Advance Directives and Substitute Decision-Making. Zalta EN, editor. The Stanford Encyclopedia of Philosophy (Summer 2009) 2009 Retrieved from http://plato.stanford.edu/archives/sum2009/entries/advance-directives/
- Overton E, Applebaum PS, Fisher SR, Dohan D, Roberts LW, Dunn LB. Alternative decision-makers perspectives on assent and dissent for dementia research. Am J Geriatr Psychiatry. 2013;21(4):346–54. doi: 10.1016/j.jagp.2013.01.027. [DOI] [PubMed] [Google Scholar]
- President’s National Bioethics Advisory Commission Report. Research Involving Subjects with Mental Disorders That May Affect Decision making Capacity-A Draft Report of the National Bioethics Advisory Commission. 1998 Dec; www.bioethics.gov.
- Roberts LW. Informed consent and the capacity for voluntarism. Am J Psychiatry. 2002;159(5):705–712. doi: 10.1176/appi.ajp.159.5.705. [DOI] [PubMed] [Google Scholar]
- Roberts LW, Brems C, Johnson ME, Smikowski J. Community-based participatory research for improved mental health care: A manual for clinicians and researchers. Springer; New York: 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts LW, Dyer AR. Concise Guide to Ethics in Mental Health Care. American Psychiatric Publishing; Washington, DC: 2004. [Google Scholar]
- Roberts LW, Hammond KAG, Warner TD, Lewis R. Influence of ethical safeguards on research participation: comparison of perspectives of people with schizophrenia and psychiatrists. Am J Psychiatry. 2004;161(12):2309–2311. doi: 10.1176/appi.ajp.161.12.2309. [DOI] [PubMed] [Google Scholar]
- Roberts LW, Kim JP. Attunement and alignment of people with schizophrenia and their preferred alternative decision-makers: An exploratory pilot study comparing treatment and research decisions. J Psychiatric Res. 2015;71:70–7. doi: 10.1016/j.jpsychires.2015.09.014. [DOI] [PubMed] [Google Scholar]
- Roberts LW, Warner TD, Brody JL. Perspectives of schizophrenia patients and psychiatrists regarding ethical aspects of research participation. Am J Psychiatry. 2000;157(1):67–74. doi: 10.1176/ajp.157.1.67. [DOI] [PubMed] [Google Scholar]
- Roberts LW, Warner TD, Brody JL, Roberts B, Lauriello J, Lyketsos C. Patient and psychiatrist ratings of hypothetical schizophrenia research protocols: assessment of harm potential and factors influencing participation decisions. Am J Psychiatry. 2002;159(4):573–84. doi: 10.1176/appi.ajp.159.4.573. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Scaling up action against non-communicable diseases: How much will it cost? Geneva, Switzerland: 2011. [Google Scholar]


