Abstract
Objective
To evaluate the effects of overweight/obese versus normal weight on symptoms, activity limitation and health care utilization among a group of urban children with persistent asthma.
Methods
Data were obtained from the School-Based Asthma Therapy Trial. We enrolled 530 children ages 3–10 with persistent asthma from 2006–2009 (response rate: 74%). We conducted in-home interviews to assess symptoms and health care utilization. We measured height and weight in school nurse offices to determine BMI percentile, and compared normal weight children to overweight/obese (BMI >85th percentile) children. Bivariate and multivariate analyses were used.
Results
We collected BMI data from 472 children (89%); 49% were overweight/obese. When controlling for child race, child ethnicity, intervention group, caregiver age, and screen time, overweight/obese children had more days with asthma symptoms (4.25 vs. 3.42/2 weeks, p=.035) and more activity limitation (3.43 vs. 2.55/2 weeks, p=0.013) compared to normal weight children. Overweight/obese children were more likely to have had an ED visit or hospitalization for any reason (47% vs. 36%, OR 1.5, 95% CI 1.01, 2.19), and there was a trend for overweight/obese children to have more acute asthma visits in the past year (1.68 vs. 1.31, p=.090). Overweight/obese children were not more likely to be taking a daily preventive inhaled corticosteroid (OR 1.0, 95% CI 0.68, 1.56).
Conclusions
Overweight/obese children with persistent asthma experience more asthma symptoms, activity limitation and health care utilization compared to normal weight children, with no increased use of inhaled corticosteroids. Further efforts are needed to improve the health of these children.
Keywords: overweight children, school age children, Body Mass Index–BMI, preventive medicine, health care utilization
Introduction
Asthma is one of the most common chronic illnesses of childhood, affecting almost 10% of children in the United States.(1, 2) Despite advancements in medicine and public health initiatives, the national prevalence of pediatric asthma has continued to rise, and poor urban children suffer disproportionately.(1, 3) Poorly controlled pediatric asthma continues to be a leading cause of missed school days, missed work days, emergency room visits and hospitalizations in the United States.(3, 4) Although the National Heart Lung and Blood Institute has published guidelines to support the management of asthma in children, under treatment (through insufficient prescribing or poor adherence) with effective preventive medications remains common.(5)
In recent years, the United States has also seen significant increases in rates of childhood overweight and obesity.(6) Overweight and obese status in childhood is associated with increased risk of sleep apnea, cardiovascular disease and diabetes in childhood as well as later in life.(7, 8) Health care utilization is also higher in overweight and obese children than normal weight children.(9) Ultimately, being overweight or obese in childhood can lead to increased health risks throughout adolescence and adulthood, causing substantial morbidity and increased long-term health care costs in this population.(10)
Evidence supports the comorbidity of asthma and overweight in the general population.(11, 12) Studies have demonstrated higher rates of overweight/obesity in asthmatic children than in non-asthmatic children,(11) as well as higher incidence of asthma in overweight/obese children than normal weight children.(12) Less is known about the association of overweight status among children with persistent asthma symptoms. Further, the mechanisms linking weight status and pediatric asthma symptoms remain unclear,(11, 12) and clear directionality has yet to be established, however bi-directionality is likely at work in the relationship between asthma and obesity. (13) Asthma may contribute to increased overweight/obesity(14) due to an influence on activity limitation,(15) or by inflammatory mechanisms.(16) However overweight/obesity may also be related to an increased incidence of new asthma diagnosis and wheezing.(12, 16) In this study we sought to determine the associations of being overweight/obese (BMI ≥85th percentile) and reported asthma symptoms, activity limitation, and health care utilization. We hypothesized that compared to normal weight children, overweight/obese children with persistent asthma experience more asthma symptoms, experience more asthma-related limitation in activities, are more likely to use the healthcare system for asthma, and are more likely to use preventive asthma medications.
Methods
SETTINGS AND PARTICIPANTS
We obtained data for this study from a larger study, the School-Based Asthma Therapy (SBAT) Trial, which enrolled 530 children ages 3–10 with persistent asthma at the start of each school year, from 2006–2009.(17) Potential subjects were recruited from 67 elementary schools and preschools in the Rochester City School District, and were identified by review of school medical-alert forms filled out by parents at the start of each school year (response rate: 74%). As described in prior work(17), eligible participants had a physician diagnosis of asthma and parent report of symptoms indicating persistent asthma based on the National Heart Lung and Blood Institute guidelines.(5) Exclusion criteria included medical conditions that may interfere with the assessment of outcomes (i.e. cystic fibrosis, sickle cell disease, and heart disease), a caregiver who could not read/understand English, no telephone access, and plans to move out of the district within 6 months. We obtained written informed consent from caregivers and verbal assent from children ≥7 years old. The study protocol was approved by the University of Rochester Institutional Review Board.
All data for this analysis, with the exception of BMI, were collected through interviews with primary caregivers in the home at the beginning of each school year (September through mid-November). New participants were enrolled for three consecutive years. At the initial home visit, subjects were randomly assigned to an intervention or control condition, and randomization was stratified by secondhand smoke exposure status. The intervention continued for the duration of one school year, and included directly observed administration of preventive medicine daily at the school nurse’s office, as well as an environmental tobacco smoke reduction component for caregivers of smoke exposed children. Further details of the intervention and results have been published elsewhere.(17, 18) While the data presented was collected as part of a large randomized control trial, this study is a cross-sectional analysis of initial symptom assessments which occurred prior to the initiation of any intervention procedures.
Assessment of Asthma Symptoms
We used structured interviews to ask caregivers about their child’s asthma symptoms over the past two weeks. Symptom free days were defined as a 24-hour period in which the child did not experience any cough, wheeze or breathlessness. We also asked caregivers to identify the number of days the child had any daytime asthma symptoms, nighttime asthma symptoms, and rescue medication use to relieve symptoms over the past two weeks.
Assessment of Activity Limitation due to Asthma
We asked caregivers to report the number of days their child experienced any activity limitation due to asthma over the prior two weeks. We also used the Child Activities subscale from the Children’s Health Survey for Asthma(19) to assess limitation over the past two weeks during mild activities (i.e. walking) due to asthma. Parents were asked to report the extent of limitation on a 5-point scale (1=Not Limited, 5=Totally Limited).(19) Responses were dichotomized to Not Limited vs. Any Limitation.
Assessment of Health Care Utilization
Caregivers reported their child’s health care utilization over the prior year. We asked them to identify visits to a doctor, emergency room visits, and hospitalizations for any reason. We asked caregivers to identify the purpose of the visit (well-child visit, visit for an asthma exacerbation, asthma follow-up, other), the date of the visit, and whether or not asthma was discussed at the visit. We defined an “acute” asthma visit as any hospitalization, emergency room visit or doctor’s visit for an asthma exacerbation. Caregivers also reported all current asthma medication prescriptions (i.e. inhaled corticosteroid, bronchodilators, etc.), and we requested to see the medication canisters when available.
Assessment of Body Mass Index Percentile
During the last few months of school (at the end of the school-based intervention), we measured children’s height and weight in the school nurse offices using standardized equipment and techniques. We used these measurements to determine Body Mass Index (BMI) percentile using the Centers for Disease Control and Prevention growth charts and SAS coding schematic. Children’s weight status was categorized by BMI percentile ranges. Measurements were dichotomized to compare normal weight children (BMI ≥5th–<85th percentile) to overweight and obese children (BMI ≥85th percentile). Underweight children (BMI <5th percentile, n=12) were excluded from these analyses.
Assessment of Covariates
At the initial survey, we collected demographic information including gender, age, race (White, Black or Other), ethnicity (Hispanic or not Hispanic), Medicaid insurance coverage (yes/no), caregiver age (≤30 or >30 years), caregiver education (<high school or ≥high school), caregiver marital status (single or married/domestic partner), caregiver employment (yes/no), and caregiver gender. We also explored covariates that have been previously found to be associated with asthma and overweight/obese. We asked caregivers to identify if their child was born prematurely (yes/no). We asked caregivers to report the number of minutes spent watching TV, playing video games, or using a computer on a typical weekday and typical weekend day to determine average screen time, and dichotomized responses to ≤3 hours/day and >3 hours/day. Additionally, we collected salivary cotinine (a metabolite of nicotine, reported in ng/ml) as an objective measurement of environmental tobacco smoke (ETS) exposure.
ANALYSIS
We performed analyses for this study using PASW version 20.0 software (Predictive Analytics SoftWare 20.0; SPSS Inc, Chicago, IL). We used bivariate statistics and the non-parametric Mann-Whitney test to compare weight status to asthma outcomes including symptoms, limitation of activities, and health care utilization. We used linear and logistic regression analyses to assess the independent effect of weight status on asthma outcomes, controlling for child race, child ethnicity, intervention group, and potentially confounding variables that were different between groups including caregiver age and screen time. A 2-sided alpha <.05 was considered statistically significant.
Results
Of the 530 children enrolled in the School-Based Asthma Therapy (SBAT) trial, BMI data were collected for 472 children (89%); 19% were overweight (BMI 85th–95th percentile); and 30% were obese (BMI ≥95th percentile). We combined overweight and obese children into one group. We excluded underweight children from analyses (BMI <5th percentile, n=12). As shown in Table 1, 57% of children were male, 65% Black, 28% Hispanic, and 72% used Medicaid as their primary medical insurance. Among the primary caregivers in this study, almost all (96%) were female, 62% were employed, and 40% had not completed a high school education.
Table 1.
Demographic Characteristics
| Overall (BMI ≥5th percentile) | Normal Weight (BMI ≥5th and <85th percentile) | Overweight/Obese (BMI ≥85th percentile) | ||
|---|---|---|---|---|
|
| ||||
| n=460 | n=227 | n=233 | p-value | |
|
| ||||
| Child Characteristics | ||||
|
| ||||
| Male | 264 (57%) | 132 (58%) | 132 (57%) | 0.778 |
|
| ||||
| Age | 7.16 (1.87) | 7.11 (1.89) | 7.21 (1.86) | 0.475 |
|
| ||||
| Race | ||||
| White | 36 (8%) | 15 (7%) | 21 (9%) | |
| Black | 298 (65%) | 157 (69%) | 141 (60%) | |
| Other | 126 (27%) | 55 (24%) | 71 (30%) | 0.152 |
|
| ||||
| Hispanic | 128 (28%) | 54 (24%) | 74 (32%) | 0.061 |
|
| ||||
| Treatment Group | 223 (48%) | 107 (47%) | 116 (50%) | 0.577 |
|
| ||||
| Medicaid | 333 (72%) | 164 (72%) | 169 (72%) | 1.000 |
|
| ||||
| Child was born premature | 54 (12%) | 27 (12%) | 27 (12%) | 1.000 |
|
| ||||
| Salivary Cotinine (ng/ml) | 1.41 (2.43) | 1.15 (1.58) | 1.66 (3.02) | 0.478 |
|
| ||||
| Screen Time >3 hrs/daya | 227 (50%) | 100 (46%) | 127 (55%) | 0.048 |
|
| ||||
| Caregiver Characteristics | ||||
|
| ||||
| Female Caregiver | 441 (96%) | 221 (97%) | 220 (94%) | 0.159 |
|
| ||||
| Single Caregiver | 339 (74%) | 167 (74%) | 172 (74%) | 1.000 |
|
| ||||
| Caregiver >30 yearsa | 306 (66%) | 136 (60%) | 170 (73%) | 0.004 |
|
| ||||
| Caregiver Education <HS | 182 (40%) | 88 (39%) | 94 (40%) | 0.775 |
|
| ||||
| Employed Caregiver | 286 (62%) | 142 (65%) | 144 (66%) | 0.920 |
p-value <0.05
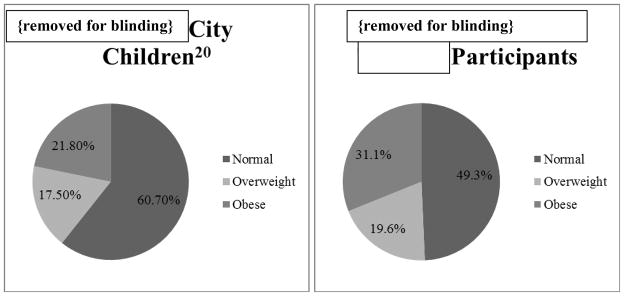
In Figure 1, we show the prevalence of weight status among the SBAT, participants compared to the same age group of children from the city of Rochester, (part of a county wide obesity prevalence report).(20) The prevalence of both overweight and obesity among study participants was higher than the prevalence among children in the city.
Figure 1.
Overweight/Obesity Prevalence: (in order left to right, top to bottom): Rochester; SBAT; Children vs. Rochester; School Based Asthma Therapy Participants
Figure 1 excludes data from underweight children.
There were no differences between overweight/obese and normal weight children in gender, age, race, ethnicity, or treatment group assignment. Overweight/obese children were significantly more likely than their normal weight peers to have a caregiver older than 30 years (p=.004), and were more likely to have more than 3 hours of screen time viewing per day (55% vs. 46%, p=.048). There were no differences between groups in caregiver education, caregiver employment, caregiver gender, smoke exposure, or prematurity.
Asthma symptoms and activity limitation due to asthma within the prior two weeks are shown in Table 2. Overweight/obese children had significantly more days with daytime asthma symptoms than their normal weight peers (4.25 vs. 3.42 days/2 weeks, adjusted p=.035). Overweight/obese children also experienced more days with activity limitation due to asthma (3.43 vs. 2.55, adjusted p=.013) in past 2 weeks, and were more likely to report any limitation due to asthma in mild activities over the past week (27% vs. 18%, OR 1.5, 95% CI 0.92–2.37). In regression analyses controlling for child race, ethnicity, screen time, and caregiver age, the majority of these findings remained significant. There were no significant differences between groups in symptom free days or nights with symptoms.
Table 2.
Asthma Symptoms over 2 weeks by Weight Status
| Overall (BMI ≥5th percentile) | Normal Weight (BMI ≥5th and <85th percentile) | Overweight/Obese (BMI ≥85th percentile) | |||
|---|---|---|---|---|---|
| n=460 | n=227 | n=233 | p-value | Adjusted p-value | |
| Symptom Free Days mean(SD), range 0–14 | 8.07 (4.82) | 8.34 (4.86) | 7.81 (4.78) | 0.194 | .153 |
| Symptom Daysab mean(SD), range 0–14 | 3.89 (4.22) | 3.52 (4.26) | 4.25 (4.15) | 0.005 | .035 |
| Symptom Nights mean(SD), range 0–14 | 4.07 (4.48) | 4.11 (4.56) | 4.04 (4.42) | 0.984 | .987 |
| Days requiring rescue medication mean(SD), range 0–14 | 4.03 (4.67) | 3.70 (4.48) | 4.34 (4.84) | 0.131 | 0.153 |
| Activity Limited Days due to asthmaab mean(SD), range 0–14 | 2.99 (3.78) | 2.55 (3.50) | 3.43 (3.99) | 0.004 | 0.013 |
| Limited in Mild Activitiesa N(%) | 104 (23%) | 41 (18%) | 63 (27%) | 0.026 | OR (95% CI) 1.5 (0.92–2.37) |
p-value <0.05
p-value <0.05 in regression analyses
Multivariate analyses controlled for child race, child ethnicity, intervention group, caregiver age, and screen time.
Table 3 shows health care utilization and preventive medication use for overweight/obese and normal weight children. Children who were overweight/obese were significantly more likely to visit the emergency department or be hospitalized for any reason in the past year (47% vs. 36%, OR 1.5, 95% CI 1.01–2.19) compared to normal weight children. While significantly different in bivariate analyses, in a multivariate regression did not show significant differences between acute asthma visits in the prior year (1.68 vs. 1.31, adjusted p=.090) or having had ≥2 acute asthma visits (41% vs. 32%, OR 1.3, 95% CI 0.87–1.93). Overweight/obese children did not have significantly more primary care doctor’s visits (6.39 vs. 4.61, p=.184), and were not more likely to use a daily inhaled corticosteroid (61% vs. 61%, p=0.924) than their normal weight peers. In a logistic regression including child race, ethnicity, screen time, and caregiver age, overweight/obese children had 1.5 greater odds of having an ED visit or hospitalization (95% CI:1.01–2.16) in the prior year. We also conducted a secondary analysis comparing normal weight children to obese children (excluding the smaller group of overweight/obese children), and all results remained statistically significant.
Table 3.
Health Care Utilization and Preventive Medication Use by Weight Status
| Overall (BMI ≥5th percentile) | Normal Weight (BMI ≥5th and <85th percentile) | Overweight/Obese (BMI ≥85th percentile) | |||
|---|---|---|---|---|---|
| n=460 | n=227 | n=233 | p-value | OR (95% CI)/Adjusted p-value | |
| Any ED Visit/Hospitalization in Prior Yearab N(%) | 191 (42%) | 82 (36%) | 109 (47%) | 0.023 | 1.5 (1.01–2.19) |
| Doctor’s Visits for any reason in Prior Year mean(SD) | 5.51 (9.35) | 4.61 (5.42) | 6.39 (11.95) | 0.184 | 0.118 |
| Total Acute Asthma Visits in Prior Yeara mean(SD), | 1.50 (1.81) | 1.31 (1.71) | 1.68 (1.88) | 0.029 | 0.090 |
| 2 or More Acute Asthma Visits in Prior Yeara N(%) | 168 (36%) | 72 (32%) | 96 (41%) | 0.042 | 1.3 (0.87–1.93) |
| Inhaled Corticosteroid Use N(%) | 281 (61%) | 138 (61%) | 143 (61%) | 0.924 | 1.0 (0.68–1.56) |
p-value <0.05
p-value <0.05 in regression analyses
Multivariate analyses controlled for child race, child ethnicity, intervention group, caregiver age, and screen time.
Discussion
Our study considers the relationship of overweight/obese status and asthma morbidity among a large community-based sample of urban school-aged children with persistent asthma. In our sample, all children attended school in an underserved, urban school district, and eligibility required them to have persistent asthma symptoms that warranted the use of a daily preventive asthma medication. Among this group, we found that the prevalence of overweight/obese was very high, and while increased prevalence of obesity is well documented in urban areas, the prevalence of overweight and obese status in our sample was even higher than the general population of children living in urban Rochester, NY (Figure 1).(20)
The relationship between asthma and overweight/obesity is complex, and is likely bidirectional. Prior research has found that asthmatic children who are overweight or obese have more ED visits and hospitalizations,(12, 21, 22) have greater activity limitation(13) and miss more school days(22) than their normal weight asthmatic peers. Children with both diagnoses also may experience higher functional morbidity, with studies showing significantly lower quality of life scores,(23) higher rates of emotional difficulties and worse mental health.(13)
We found that overweight/obese children experienced more frequent daytime asthma symptoms than their normal weight peers. They also were more likely to be limited by their asthma when performing even mild activities like walking. These findings are concerning for several reasons. It is likely that children with daytime asthma symptoms and asthma-related activity limitation avoid physical exercise, especially when experiencing difficulty with their breathing, which may exacerbate weight problems. Further, parents, teachers and other care providers may discourage children from participating in physical activity to prevent further difficulty breathing and avoid exercise induced bronchospasm.(24) While there is a potential for uncertainity between asthma symptoms and physical deconditioning related to weight status, this discouragement of physical activity is in contradiction to the 2007 NHLBI Expert Panel guidelines, which clearly indicate that the goal for well controlled asthma includes no limitations on activity.(5) Considering this goal, these reported activity limiations further indicate improper management of asthma in this group. Lastly, physical activity may improve asthma outcomes (25) and has potential for positive benefits on weight status among children with asthma. Children who avoid physical activities may be at a disadvantage in overcoming both health issues.(26)
Overweight/obese children with persistent asthma in this study also reported greater utilization of urgent health care services compared to normal weight children. Specifically, overweight/obese children were significantly more likely to require an ED visit or hospitalization for any reason compared to their normal weight peers. These findings translate to increased cost of healthcare, as well as greater acuity of illness for children who have persistent asthma and are overweight/obese, further emphasizing the need for additional efforts to better understand the morbidity and use of healthcare services that accompanies obesity. Importantly, worse asthma control was observed in these children without the use of more preventive medications. This suggests sub-optimal provision of guideline based asthma care in this population.
Some studies have shown that obese children with asthma are more likely to use asthma medications compared to their normal weight peers.(22) Others have suggested that higher levels of systemic steroid use may contribute to overweight status.(27) In this study we did not observe any differences between groups in the percent of children who were prescribed an inhaled corticosteroid; we were unable to meaningfully evaluate systemic steroid use. Approximately 67% of children in both the normal weight and overweight/obese groups reported the use of any controller asthma medication, and 61% reported using an inhaled corticosteroid. While all children in this sample were experiencing persistent symptoms that warranted the use of a controller medication based on the NHLBI guidelines, the fact that overweight/obese children experienced greater morbidity with equivalent rates of reported preventive medication highlights under-treatment, poor adherence, or reduced physiologic response to these medications among this subgroup.
There were no demographic differences between groups, with the exception that children who were overweight/obese were more likely to have a parent over the age of 30. It is possible that older caregivers are more cautious in allowing physical activity for children with persistent asthma, with the aim of preventing symptoms. Differences in caretaker lifestyle and nutritional habits may also play a role. Additionally, half of the children in this sample were reported to have screen time of >3 hours per day, clearly exceeding the AAP recommendations of no more than 1–2 hours per day of screen time.(28) We initially dichotomized screen time at ≤2 hours/day, per the AAP recommendations, but found that 75% of our total sample exceeded the recommendation, and that this did not differ between groups.(28) When considering previous reports of excessive screen time use, we chose to alter our screen time analysis to look at average screen times of >3 hours/day.(29) While children may be using screen time for relaxation or as an alternative to physical activity due to their asthma symptoms, this likely perpetuates the cycle of poor health habits for these children.
There are a few limitations to this study that should be noted. Asthma symptoms, activity limitation and healthcare utilization were reported by parents at the beginning of the study, and BMI was measured in the last few months of school (approximately 8 months apart). Although weight status is not as likely to change during the school year as it is during the summer,(30, 31) it is possible that some children changed groups (i.e. normal weight to overweight) during the school year. While there was no difference between groups in the percentage of children using preventive inhaled corticosteroid medications, we do not have complete information on the dose of medications used or objective adherence information. We also are unable to account for parent weight status, child atopy, activity time, or dietary habits, all of which may influence childhood weight status. Some studies cite concerns that children with diagnoses of asthma and overweight may have been misdiagnosed with asthma or that assessments of severity level may be inaccurate due to deconditioning or difficulty breathing at night related to obesity.(32) However, all children in this study had physician-diagnosed persistent asthma, making misclassification unlikely. Lastly, our study was conducted among an inner-city sample of school children in Rochester, NY and these findings can only be generalized to similar populations.
This study also has multiple strengths. We include a large community-based sample of urban children, all of whom had persistent asthma symptoms, and thus our findings add to our understanding of the health effects of being overweight or obese among this high-risk group. We obtained objective BMI data as opposed to parent reported height and weight recall, to improve accuracy of classification. Additionally, urban children present a convenient sample to assess the relationships between asthma and weight status as these children are at high risk for both persistent asthma and obesity.(1, 3, 33) We were also able to evaluate many important potentially confounding factors that may influence both asthma and/or weight status such as screen time, premature birth, caregiver education, and smoke exposure.
Conclusions
As the prevalence of overweight/obese status continues to rise in American youth and asthma remains one of the most common chronic illnesses of childhood, understanding how weight status influences the health of children with asthma is increasingly important. Despite the clinically important differences in symptoms, activity limitation, and overall health care utilization that we observed in this study, we did not see differences in use of preventive medications. Reducing asthma morbidity, reducing obesity, and preventing inappropriate weight gain among youth are Healthy People 2020 goals (34, 35). For the children experiencing both asthma and obesity, optimizing asthma therapy and promoting weight management is critical.
Suggestions for providers
Providers should carefully evaluate children who are overweight/obese and also have persistent asthma to consider appropriate preventive asthma treatments and to provide counseling regarding nutrition, physical activity, and limited screen time. Increased attention to weight management in conjunction with asthma control measures may allow for effective treatment of both conditions. Further, optimal management is critical for all children with asthma to ensure the goals of therapy are met and children aren’t experiencing activity limitation that might contribute further to the obesity epidemic.
Acknowledgments
Funding: This work was funded by a grant from the Halcyon Hill Foundation (Jill S. Halterman) and the National Heart, Lung, and Blood Institute (R01 HL079954, Jill S. Halterman).
Clinicaltrials.gov Identifier: NCT00296998
Abbreviations
- BMI
body mass index
- SBAT
School Based Asthma Therapy
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Vital signs: asthma prevalence, disease characteristics, and self-management education: United States, 2001–2009. MMWR Morbidity and mortality weekly report. 2011;60(17):547–52. Epub 2011/05/06. [PubMed] [Google Scholar]
- 2.Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980–2007. Pediatrics. 2009;123(Suppl 3):S131–45. doi: 10.1542/peds.2008-2233C. Epub 2009/04/16. [DOI] [PubMed] [Google Scholar]
- 3.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005–2009. National health statistics reports. 2011;(32):1–14. Epub 2011/03/02. [PubMed] [Google Scholar]
- 4.Schmier JK, Manjunath R, Halpern MT, Jones ML, Thompson K, Diette GB. The impact of inadequately controlled asthma in urban children on quality of life and productivity. Annals of allergy, asthma & immunology: official publication of the American College of Allergy, Asthma, & Immunology. 2007;98(3):245–51. doi: 10.1016/S1081-1206(10)60713-2. Epub 2007/03/24. [DOI] [PubMed] [Google Scholar]
- 5.Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. The Journal of allergy and clinical immunology. 2007;120(5 Suppl):S94–138. doi: 10.1016/j.jaci.2007.09.043. Epub 2007/12/06. [DOI] [PubMed] [Google Scholar]
- 6.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA: the journal of the American Medical Association. 2012;307(5):483–90. doi: 10.1001/jama.2012.40. Epub 2012/01/19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6–e245. doi: 10.1161/CIR.0b013e31828124ad. Epub 2012/12/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saydah S, Bullard KM, Imperatore G, Geiss L, Gregg EW. Cardiometabolic Risk Factors Among US Adolescents and Young Adults and Risk of Early Mortality. Pediatrics. 2013;131(3):e679–86. doi: 10.1542/peds.2012-2583. Epub 2013/02/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trasande L, Liu Y, Fryer G, Weitzman M. Effects of childhood obesity on hospital care and costs, 1999–2005. Health Aff (Millwood) 2009;28(4):w751–60. doi: 10.1377/hlthaff.28.4.w751. Epub 2009/07/11. [DOI] [PubMed] [Google Scholar]
- 10.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. The New England journal of medicine. 2010;362(6):485–93. doi: 10.1056/NEJMoa0904130. Epub 2010/02/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gennuso J, Epstein LH, Paluch RA, Cerny F. The relationship between asthma and obesity in urban minority children and adolescents. Archives of pediatrics & adolescent medicine. 1998;152(12):1197–200. doi: 10.1001/archpedi.152.12.1197. Epub 1998/12/18. [DOI] [PubMed] [Google Scholar]
- 12.von Mutius E, Schwartz J, Neas LM, Dockery D, Weiss ST. Relation of body mass index to asthma and atopy in children: the National Health and Nutrition Examination Study III. Thorax. 2001;56(11):835–8. doi: 10.1136/thorax.56.11.835. Epub 2001/10/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glazebrook C, McPherson AC, Macdonald IA, Swift JA, Ramsay C, Newbould R, et al. Asthma as a barrier to children’s physical activity: implications for body mass index and mental health. Pediatrics. 2006;118(6):2443–9. doi: 10.1542/peds.2006-1846. Epub 2006/12/05. [DOI] [PubMed] [Google Scholar]
- 14.Epstein LH, Wu YW, Paluch RA, Cerny FJ, Dorn JP. Asthma and maternal body mass index are related to pediatric body mass index and obesity: results from the Third National Health and Nutrition Examination Survey. Obesity research. 2000;8(8):575–81. doi: 10.1038/oby.2000.74. Epub 2001/01/13. [DOI] [PubMed] [Google Scholar]
- 15.Tremblay MS, Willms JD. Is the Canadian childhood obesity epidemic related to physical inactivity? International journal of obesity and related metabolic disorders: journal of the International Association for the Study of Obesity. 2003;27(9):1100–5. doi: 10.1038/sj.ijo.0802376. Epub 2003/08/15. [DOI] [PubMed] [Google Scholar]
- 16.Flaherman V, Rutherford GW. A meta-analysis of the effect of high weight on asthma. Archives of disease in childhood. 2006;91(4):334–9. doi: 10.1136/adc.2005.080390. Epub 2006/01/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Halterman JS, Borrelli B, Fisher S, Szilagyi P, Yoos L. Improving care for urban children with asthma: design and methods of the School-Based Asthma Therapy (SBAT) trial. The Journal of asthma: official journal of the Association for the Care of Asthma. 2008;45(4):279–86. doi: 10.1080/02770900701854908. Epub 2008/05/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Halterman JS, Szilagyi PG, Fisher SG, Fagnano M, Tremblay P, Conn KM, et al. Randomized controlled trial to improve care for urban children with asthma: results of the School-Based Asthma Therapy trial. Archives of pediatrics & adolescent medicine. 2011;165(3):262–8. doi: 10.1001/archpediatrics.2011.1. Epub 2011/03/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asmussen L, Olson LM, Grant EN, Fagan J, Weiss KB. Reliability and validity of the Children’s Health Survey for Asthma. Pediatrics. 1999;104(6):e71. doi: 10.1542/peds.104.6.e71. Epub 1999/12/10. [DOI] [PubMed] [Google Scholar]
- 20.Monroe County Department of Public Health. Maternal/Child Health Report Card Update: Executive Summary. 2011 Available from: http://www2.monroecounty.gov/files/health/DataReports/MCH%20Report%20Card%2C%20Executive%20Summary%2C%20FINAL.pdf.
- 21.Carroll CL, Stoltz P, Raykov N, Smith SR, Zucker AR. Childhood overweight increases hospital admission rates for asthma. Pediatrics. 2007;120(4):734–40. doi: 10.1542/peds.2007-0409. [DOI] [PubMed] [Google Scholar]
- 22.Belamarich PF, Luder E, Kattan M, Mitchell H, Islam S, Lynn H, et al. Do obese inner-city children with asthma have more symptoms than nonobese children with asthma? Pediatrics. 2000;106(6):1436–41. doi: 10.1542/peds.106.6.1436. Epub 2000/01/11. [DOI] [PubMed] [Google Scholar]
- 23.van Gent R, van der Ent CK, Rovers MM, Kimpen JL, van Essen-Zandvliet LE, de Meer G. Excessive body weight is associated with additional loss of quality of life in children with asthma. The Journal of allergy and clinical immunology. 2007;119(3):591–6. doi: 10.1016/j.jaci.2006.11.007. Epub 2007/01/09. [DOI] [PubMed] [Google Scholar]
- 24.Lang DM, Butz AM, Duggan AK, Serwint JR. Physical activity in urban school-aged children with asthma. Pediatrics. 2004;113(4):e341–6. doi: 10.1542/peds.113.4.e341. Epub 2004/04/03. [DOI] [PubMed] [Google Scholar]
- 25.Weisgerber M, Webber K, Meurer J, Danduran M, Berger S, Flores G. Moderate and vigorous exercise programs in children with asthma: safety, parental satisfaction, and asthma outcomes. Pediatric pulmonology. 2008;43(12):1175–82. doi: 10.1002/ppul.20895. Epub 2008/11/13. [DOI] [PubMed] [Google Scholar]
- 26.Jago R, Baranowski T, Baranowski JC, Thompson D, Greaves KA. BMI from 3–6 y of age is predicted by TV viewing and physical activity, not diet. Int J Obesity. 2005;29(6):557–64. doi: 10.1038/sj.ijo.0802969. [DOI] [PubMed] [Google Scholar]
- 27.Manaboriboon B, Silverman ED, Homsanit M, Chui H, Kaufman M. Weight change associated with corticosteroid therapy in adolescents with systemic lupus erythematosus. Lupus. 2013;22(2):164–70. doi: 10.1177/0961203312469260. Epub 2012/12/12. [DOI] [PubMed] [Google Scholar]
- 28.American Academy of Pediatrics. Children, adolescents, and television. Pediatrics. 2001;107(2):423–6. doi: 10.1542/peds.107.2.423. Epub 2001/02/07. [DOI] [PubMed] [Google Scholar]
- 29.Foltz JL, Cook SR, Szilagyi PG, Auinger P, Stewart PA, Bucher S, et al. US adolescent nutrition, exercise, and screen time baseline levels prior to national recommendations. Clinical pediatrics. 2011;50(5):424–33. doi: 10.1177/0009922810393499. Epub 2011/02/02. [DOI] [PubMed] [Google Scholar]
- 30.Carrel AL, Clark RR, Peterson S, Eickhoff J, Allen DB. School-based fitness changes are lost during the summer vacation. Archives of pediatrics & adolescent medicine. 2007;161(6):561–4. doi: 10.1001/archpedi.161.6.561. Epub 2007/06/06. [DOI] [PubMed] [Google Scholar]
- 31.von Hippel PT, Powell B, Downey DB, Rowland NJ. The effect of school on overweight in childhood: gain in body mass index during the school year and during summer vacation. American journal of public health. 2007;97(4):696–702. doi: 10.2105/AJPH.2005.080754. Epub 2007/03/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.To T, Vydykhan TN, Dell S, Tassoudji M, Harris JK. Is obesity associated with asthma in young children? The Journal of pediatrics. 2004;144(2):162–8. doi: 10.1016/j.jpeds.2003.09.047. Epub 2004/02/05. [DOI] [PubMed] [Google Scholar]
- 33.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. Epub 2007/12/18. [DOI] [PubMed] [Google Scholar]
- 34.Promotion USDoHaHSOoDPaH. Healthy People 2020: Nutrition and Weight Status Objectives. Washington, DC: [updated 10/30/2012; cited 2013 01/08/2013]. Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=29. [Google Scholar]
- 35.Promotion USDoHaHSOoDPaH. Healthy People 2020: Respiratory Diseases. Washington, DC: [updated 10/30/2012; cited 2013 01/08/2013]. Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=36. [Google Scholar]