Abstract
Purpose
To determine whether conjunctivochalasis (CCh) obliterates the fornix tear reservoir and to discern whether there is concomitant aqueous tear deficiency (ATD) dry eye.
Methods
Retrospective review of 18 eyes of 12 patients with CCh and ATD (CCh+ATD) and 18 eyes of 13 patients with CCh without ATD (CCh-ATD). Changes were compared before and after fornix reconstruction regarding symptoms, basal tear volumes, use of medications, conjunctival inflammation and corneal staining.
Results
Fornix reconstruction with conjunctival recession and amniotic membrane transplantation (AMT) effectively restored the fornix tear reservoir as evidenced by a significant increase of the basal tear volume in both CCh-ATD and CCh+ATD groups. Multivariate regression analysis confirmed that such improvement was significantly correlated with symptomatic resolution (r = 1, p < 0.001), which was also accompanied by significant resolution of corneal staining, conjunctival inflammation, and reduction of topical medications. Intriguingly, the prior diagnosis of ATD was no longer existent in 10 of the 18 eyes (56%) with CCh+ATD suggesting that ATD could be secondary to obliteration of the fornix tear reservoir by CCh.
Conclusion
Obliteration of the fornix tear reservoir is a common pathogenic process regardless of whether CCh is associated with ATD dry eye or not. Restoration of the tear reservoir by fornix reconstruction with conjunctival recession and AMT results in significant resolution of symptoms and signs associated with ATD that is secondary to CCh and helps identify genuine ATD dry eye that is independent of CCh.
Keywords: Amniotic membrane, Aqueous tear deficiency, Conjunctivochalasis, Dry eye, Fornix, Tear
INTRODUCTION
A stable tear film is essential for maintaining ocular surface health thereby providing clear vision and comfort when the eyes are opened. The stability of the tear film requires coordinating effects between both compositional and hydrodynamic elements in the ocular defense system.1 The compositional elements are comprised of the lacrimal glands, the meibomian glands, and the ocular surface epithelium to provide aqueous, lipid and mucins in the tear fluid, respectively, while the hydrodynamic elements include tear evaporation, spread, and drainage, which are controlled by eyelid blinking and closure.2 With each blink, tears spread from the conjunctival cul-de-sac in the fornix (third compartment) to the tear meniscus (second compartment) and finally to the preocular tear film (first compartment).3
Clinically, conjunctivochalasis (CCh) presents as loose and redundant conjunctival folds interspersed between the globe and eyelids4 and may cause a variety of ocular symptoms that mimic dry eye.5 These redundant conjunctival folds disturb the hydrodynamic elements by interfering with the tear outflow by occluding the puncta6,7 and the tear volume in the tear meniscus.8 Recently, we have also reported that CCh interferes with the tear flow from the reservoir in the fornix to the tear meniscus.9 Despite these known interactions, it remains unclear whether CCh actually obliterates the fornix tear reservoir.
The tear volume in the fornix reservoir is traditionally assessed by the Schirmer test, which is known to have a wide range of false positive and negative rates as well as lack of standardization.10–12 The high variability of the Schirmer test is derived from the anesthetic drop size, uneven blotting, and the contact between the paper and eyelashes that elicits reflex tearing overpowering the effect of topical anesthetics.11 This variability is conceivably minimized by using the fluorescein clearance test (FCT), which reduces the contact of lashes from 5 min for Schirmer I test to 1 min. Unlike Schirmer I test, FCT at one setting can help determine basal tearing, reflex tearing, and tear clearance10,13–15 and rather importantly, quantitative measurements by FCT correlate well with those by fluorophotometry.10,13–15 Because the paper strip is bent over the tear meniscus to reach the tear reservoir in the fornix, the measured tear volume conceivably includes both the tear meniscus (the second compartment) and a part of the fornix reservoir (the third compartment). Yet it remains unclear whether the tear volume measured by the Schirmer strip might be affected by CCh that obliterates the fornix tear reservoir.
Because both CCh and ATD dry eye are common in older populations, their coexistence may make it difficult to discern whether a low wetting length is due to ATD or obliteration of the fornix tear reservoir by CCh or both. Additionally, it remains unknown if there is a causative link between CCh and ATD and if there are symptoms that could help discern primary and secondary ATD. To resolve the aforementioned questions, we retrospectively reviewed a total of 25 CCh patients with or without ATD, defined by FCT, and analyzed their clinical outcome following surgery.
METHOD
The study adhered to the tenets of the Declaration of Helsinki. This is a retrospective study approved by the ethics committee of the Ocular Surface Research and Education Foundation (Miami, FL), and included 25 symptomatic CCh patients who had undergone fornix reconstruction with conjunctival recession and amniotic membrane transplantation (AMT) between 2004 and 2014 at Ocular Surface Center (Miami, FL). The diagnosis of CCh was based on the criteria previously summarized by Meller and Tseng4 and graded accordingly. All CCh patients did not have ocular infection, trauma, symblepharon, sunken globe, inadequate blinking and past history of lower lid surgery which complicated the intended measurements described below. All CCh cases remained symptomatic despite maximal conventional medical therapies including topical concomitant medications, bandage contact lens or punctal occulsion. Due to the persistent symptoms, surgery was performed by one surgeon (S.C.G.T) using a previously reported operative technique including excision of mobile and degenerated Tenon’s, fornix deepening reconstruction with conjunctival recession and cryopreserved amniotic membrane (AM) (Bio-Tissue, Miami, FL) transplantation under topical anesthesia.16,17
These 25 patients were divided into 2 groups, i.e., CCh with (+) or without (−) aqueous tear deficiency (ATD) according to FCT. As reported,13 FCT uses the Schirmer paper strip following application of 5 μl of Fluroress® (Akorn Inc, Abita Springs, LA, USA) for one minute every 10 min for a total of 30 min. The diagnosis of ATD was based on the wetting length of less than 3 mm for the first two sets, i.e., 10th and 20th minute in the presence of anesthetics in Fluroess® for measurement of the basal tear volume.
After the surgery, improvement of symptoms was graded into 4 categories: completely/remarkably relief, partial relief, persistent/unchanged, and deteriorated. Superficial punctate keratitis (SPK) measured by fluorescein staining was graded by 0 (none), 1 (mild), 2 (moderate) and 3 (severe). Conjunctival inflammation was graded according to the conjunctival injection in the same manner.
Descriptive statistics for continuous variables are reported as the mean ± SD and analyzed using SPSS software, version 19.0 (SPSS Inc., Chicago, Illinois, USA). Differences between parameters were analyzed by student t-test and Wilcoxon signed ranks test. Correlation among the changes of FCT and variable factors was analyzed by multivariate regression analysis. A p value less than 0.05 was considered statistically significant.
RESULTS
Patient’s medical records including demographics, ocular co-morbidity, previous therapies, clinical presentations and concomitant medications at presentation were retrieved (see Table, Supplemental Digital Content 1, which illustrates the summary of patient’s relevant clinical data.xls). All patients were matched for age, gender, symptomatic CCh severity, interruption of the tear meniscus, prior treatments, fluorescein-stained SPK and conjunctival inflammation. Patients were divided into two groups based on FCT results, i.e., CCh-ATD (18 eyes in 13 patients) and CCh+ATD (18 eyes in 12 patients) with an average basal wetting length of 5.6 ± 2.5 mm and 1.1 ± 0.8 mm, respectively (p < 0.001). Patients with CCh+ATD had more symptoms of dryness, irritation, blurred vision, pain, and photophobia than those with CCh-ATD (p = 0.03) for a mean duration of 5.9 ± 5.6 and 4.7 ± 3.7 years, respectively (p = 0.1). The complaint of watering was more noticeable in CCh-ATD than CCh+ATD (p = 0.04). The follow up period after surgery was 2.2 ± 2.1 and 3 ± 2.7 years for CCh-ATD and CCh+ATD, respectively (p = 0.5).
Changes of Basal Tearing after Fornix Reconstruction with conjunctival recession and AMT
After surgery, the basal wetting length significantly increased in both groups; from 5.6 ± 2.5 to 8.3 ± 2.2 mm in patients without ATD (p<0.001) and from 1.1 ± 0.8 to 3.9 ± 3.1 mm (p<0.001) in patients with ATD. There was no difference in achieving this increase between those eyes receiving prior punctal occlusion and those without in either group (p=0.8, and 0.9, respectively). Interestingly, prior diagnosis of ATD was no longer existent in 10 eyes of CCh+ATD as evidenced by a significant increase of the basal wetting length from 1 ± 0.9 to 6 ± 2.8 mm (p<0.001). The remaining 8 eyes did not exhibit any significant change of the basal wetting length, i.e., from 1.1 ± 0.8 to 1.3 ± 0.7 mm (p = 0.5), suggesting that restoration of the fornix tear reservoir allowed one to identify genuine ATD dry eye that is independent of CCh in eyes with CCh+ATD.
Changes of Symptoms and Signs after Fornix Reconstruction with conjunctival recession and AMT
The aforementioned changes in the basal tear volume was accompanied by an overwhelming symptomatic relief (91.9%), which included complete relief (73.5%) and partial relief (18.4%) of the symptom score, in patients with CCh-ATD, especially regarding irritation (p < 0.001) and photophobia (p = 0.004). There was also an overwhelming symptomatic relief (90.6%), which included complete relief (86.6%) and partial relief (4%) of the symptom score, in patients with CCh+ATD, especially regarding irritation (p = 0.002), photophobia (p = 0.002), blurred vision (p = 0.008), burning (p = 0.03), dryness (p < 0.001), and pain (p = 0.004). Multivariate regression analysis confirmed that such a symptomatic relief was significantly correlated with the improvement of the basal wetting length (r = 1, p < 0.001). There were 8.1% and 9.4% residual symptoms that remained unchanged in CCh-ATD and CCh+ATD, respectively, but none that deteriorated after surgery. The persistent symptoms were significantly correlated with blepharitis (p = 0.02) but not CCh grading (p = 0.5), MGD (p = 0.4), or floppy eyelid syndrome (p = 0.8). The above improvement of symptoms was also accompanied with significant resolution of SPK and reduction of conjunctival inflammation in CCh-ATD (p = 0.03 and <0.001, respectively) and CCh+ATD (p = 0.002 and 0.008, respectively) as well as significant reduction in the use of topical medications in CCh-ATD and CCh+ATD (p = 0.03 and 0.004, respectively).
When compared to those with CCh-ATD, the 10 eyes with CCh+ATD in which ATD was resolved after surgery exhibited similar and significant symptomatic resolution in irritation (p = 0.004) and photophobia (p =0.004). In contrast, the remaining 8 eyes, in which ATD persisted after surgery, exhibited different but significant symptomatic resolution in dryness (p=0.008), blurred vision (p=0.02) and pain (p=0.008). These results suggested that prior diagnosis of ATD may have been misinterpreted because of the obliteration of the fornix tear reservoir by CCh. Intriguingly, SPK, conjunctival inflammation, and the use of topical medications were significantly decreased in the 10 eyes (p = 0.3) of CCh+ATD, in which ATD was resolved after surgery but remained unchanged in the 8 persistent ATD eyes (p =0.1, 0.5, and 0.3, respectively). Collectively, these results further strengthen the notion that restoration of the fornix tear reservoir not only led to resolution of symptoms and signs related to CCh, but also helps discern whether a low wetting length is due to low tear production by ATD or obliteration of the fornix tear reservoir by CCh.
DISCUSSION
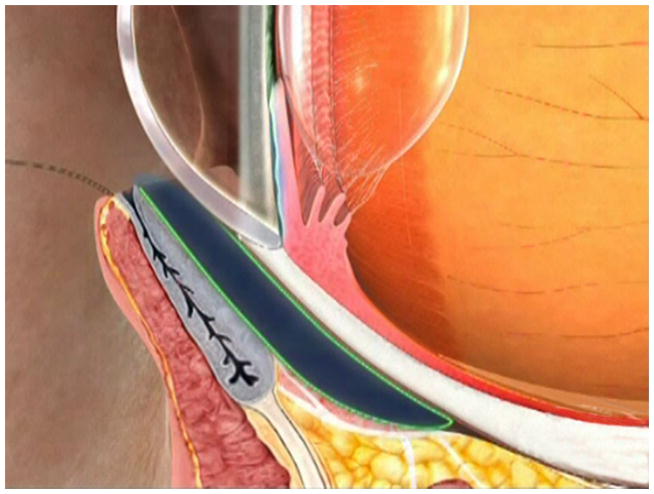
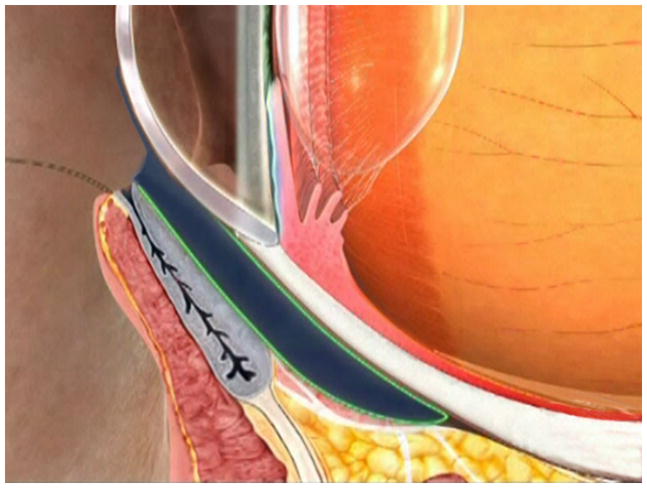
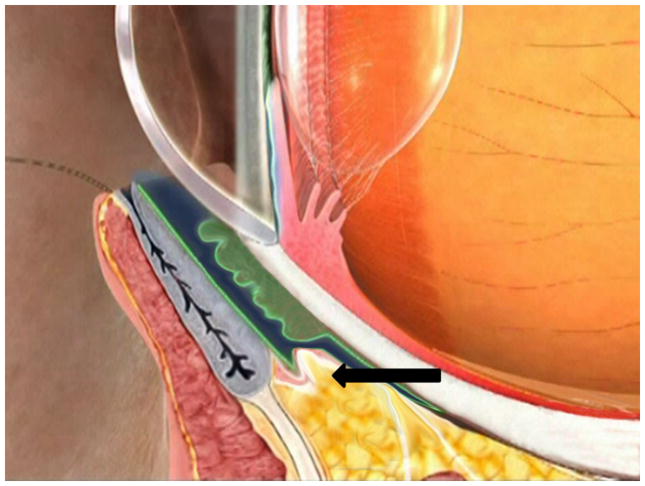
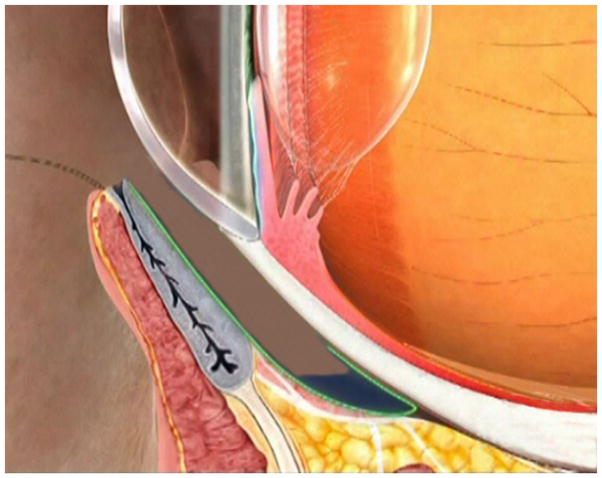
Previous studies have shown that CCh disturbs the preocular tear film by blocking the tear drainage,5,6 disrupting the tear meniscus,5, 8 and interfering with the tear flow from the fornix reservoir to the tear meniscus.9 The present study discloses another pathogenic process, that is, CCh obliterates the fornix tear reservoir (i.e., the third compartment) explaining how CCh may interfere with the tear flow from the fornix reservoir to the tear meniscus. This new understanding is supported by evidence brought to light by the measurement of basal tearing using FCT.10,13 The basal tear volume was significantly increased when the fornix tear reservoir was restored by fornix reconstruction with conjunctival recession and AMT in all 18 eyes with CCh whether there was ATD or not. Our finding differs from Maskin’s18 that did not show any significant change of the basal tear volume in CCh patients, although their patients did experience a significant symptomatic relief after surgery. Such a discrepancy might be attributed to different surgical techniques employed. Conjuntival “resection” but not “recession” was performed by Maskin.18 In contrast, our current surgical procedures include the following key steps: (1) significant rearrangement of conjunctiva by recessing it from the limbus to the fornix following inferior peritomy and anchoring to the fornix, (2) thorough removal of degenerated Tenon’s capsule, and (3) replacement of the Tenon and the conjunctival tissue by two separate layers of cryopreserved AM.16 We strongly suspect that the fornix tear reservoir is not deepened by Maskin, resulting in the lack of significant change in the basal tear volume. We believe that our finding is further strengthened by having a larger sample size and by having the study patients subdivided into CCh-ATD and CCh+ATD. The increase of basal (~ 2.8 mm) tear volumes could not be explained by tear secretion, which has an average rate of 1.2 μl/min with a corresponding increase of 1.5 mm on the Schirmer strip paper.3,19 Based on our results, we theorize that fornix, i.e., conjunctival cul-de-sac, is the predominant compartment serving as the reservoir, which through blinking sustains a steady replenishment for the remaining two compartments, i.e., tear meniscus and preocular tear film (Fig. 1A and 1B). This interpretation is also in agreement with and supported by previous studies using fluorescein3,20 or TC-99m21 to trace the tear flow.
FIGURE 1. Schematic Demonstration of Fornix Tear Reservoir Obliterated by CCh and Restored by Fornix Reconstruction With Conjunctival Recession and AMT.
Under the normal circumstance, the fornix tear reservoir depicted in dark blue is responsible for delivering tear fluids to the tear meniscus by blinking (A, B). In CCh, the fornix tear reservoir is obliterated by loose and wrinkled conjunctiva (C, green) and prolapse fat (C, arrow) due to degenerated Tenon’s capsule. This results in low basal wettings which mimick ATD dry eye. Restoration of the fornix tear reservoir is achieved by fornix deepening reconstruction, resulting in disappearance of ATD dry eye secondary to CCh (i.e., converted to a normal state). Consequently, fornix deepening reconstruction also helps identify ATD dry eye that is independent of CCh (D).
Restoration of the tear reservoir by fornix reconstruction, conjunctival recession and AMT resulted in the disappearance of ATD in 10 of 18 eyes with CCh+ATD. This finding further suggests that the obliteration of the fornix tear reservoir is a primary pathogenic process regardless of whether CCh is associated with ATD dry eye or not. It also sheds new light on our clinical management of patients presenting with both CCh and ATD dry eye. In fact, the close association between CCh and ATD has been described by Rieger in 1990,22 Grene in 199123 and Chhadva in 201524. Hoh et al in 199525 reported that the risk of developing ATD increases with severity of CCh, suggesting that CCh itself may be a cause leading to ATD dry eye. However, because both CCh and ATD dry eye are prevalent in aged populations, it is also challenging to discern ATD that may exist as an independent disease. When compared to those of CCh-ATD, these 10 eyes exhibited similar resolution of symptoms, corneal staining and conjunctival inflammation; further supporting that CCh may mimic or aggravate ATD. This notion clarifies the importance of fornix reconstruction during CCh surgery as a logical step in the clinical management algorithm for dry eye.2 Patients with persistent dry eye symptoms and signs confirmed the diagnosis of primary ATD. This represented the remaining 8 eyes of which the basal tear secretion remained unchanged after CCh surgery with fornix reconstruction. In these patients, ATD can effectively be treated by conventional therapy after eliminating ineffective tear spread by CCh.1,2
In summary, the pathogenesis of CCh involves blockage of tear flow into the nasolacrimal drainage system5,6 and interruption of the continuity of the tear meniscus.5,8 The present study has advanced our understanding of how CCh obliterates fornix tear reservoir so as to interfere with the tears from the fornix tear reservoir to the tear meniscus9 (Fig. 1). Consistent with this concept, we believe that loose and redundant conjunctiva in CCh should extend from the lid margin/meniscus locale (reviewed in6 as well as4) to the fornix. Because the pathology extends deeper into the fornix, we believe that the underlying pathology does not reside in the conjunctiva but rather owes to dissolution of the Tenon’s capsule, which functions as a “carpet pad” to anchor the conjunctiva “carpet” to the underlying sclera “floor”. This notion is also supported by the lack of healthy Tenon’s capsule16,17,26,27 and the presence of prolapsed orbital fat noted during the surgery of CCh (Fig. 1). Furthermore, it is also supported by the experimental data showing excessive degradation of the extracellular matrix by matrix metalloproteinases (MMPs) under pro-inflammatory cytokines.26,27 As of now, a number of surgical procedures have been advocated to treat CCh such as scleral fixation suture,28 crescent bulbar conjunctival excision with direct closure,6,29 resection combined with inferior peritomy and radial relaxing incisions,29 excision with AM transplantation,17,18,30 cauterization/laser coagulation with or without excision31,32 and subconjunctival fibrin sealant followed by excision.33 A majority of these procedures focus on elimination of conjunctival folds close to the tear meniscus. The new understanding of the underlying pathology of CCh presented herein helps us formulate an effective surgical strategy aimed at restoration of the fornix tear reservoir (Fig. 1). Future prospective comparative studies are needed to determine whether the said surgical procedure directed to restoring and deepening the fornix is more effective in treating CCh with or without ATD to ensure a continuous supply of tears from the reservoir to the tear meniscus and the preocular tear film.
Supplementary Material
Table that illustrates the summary of patient’s relevant clinical data.xls
Acknowledgments
Funding/Support: This study was supported in part by an unrestricted grant from Ocular Surface Research Education Foundation, Miami, FL.
The authors thank Szu-Yu Chen for the advice in Schematic drawing.
Footnotes
Financial Disclosure: Dr. Tseng has obtained a patent for the method of preparation and clinical uses of amniotic membrane and has licensed the rights to TissueTech, Inc, which procures and processes, and to Bio-Tissue, Inc., which is a subsidiary of TissueTech, Inc., to distribute cryopreserved amniotic membrane for clinical and research uses.
References
- 1.Tseng SC, Tsubota K. Important concepts for treating ocular surface and tear disorders. Am J Ophthalmol. 1997;124(6):825–835. doi: 10.1016/s0002-9394(14)71700-3. [DOI] [PubMed] [Google Scholar]
- 2.Tseng SC. A practical treatment algorithm for managing ocular surface and tear disorders. Cornea. 2011;30(Suppl 1):S8–S14. doi: 10.1097/ICO.0b013e318228218c. [DOI] [PubMed] [Google Scholar]
- 3.Mishima S, Gasset A, Klyce SD, et al. Determination of tear volume and tear flow. Invest Ophthalmol. 1966;5(3):264–276. [PubMed] [Google Scholar]
- 4.Meller D, Tseng SC. Conjunctivochalasis: literature review and possible pathophysiology. Surv Ophthalmol. 1998;43(3):225–232. doi: 10.1016/s0039-6257(98)00037-x. [DOI] [PubMed] [Google Scholar]
- 5.Di Pascuale MA, Espana EM, Kawakita T, et al. Clinical characteristics of conjunctivochalasis with or without aqueous tear deficiency. Br J Ophthalmol. 2004;88(3):388–392. doi: 10.1136/bjo.2003.025460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu D. Conjunctivochalasis. A cause of tearing and its management. Ophthal Plast & Reconstr Surg. 1986;2:25–28. [PubMed] [Google Scholar]
- 7.Erdogan-Poyraz C, Mocan MC, Irkec M, et al. Delayed tear clearance in patients with conjunctivochalasis is associated with punctal occlusion. Cornea. 2007;26(3):290–293. doi: 10.1097/ICO.0b013e31802e1e24. [DOI] [PubMed] [Google Scholar]
- 8.Pult H, Riede-Pult BH. Impact of conjunctival folds on central tear meniscus height. Invest Ophthalmol Vis Sci. 2015;56(3):1459–1466. doi: 10.1167/iovs.14-15908. [DOI] [PubMed] [Google Scholar]
- 9.Huang Y, Sheha H, Tseng SC. Conjunctivochalasis interferes with tear flow from fornix to tear meniscus. Ophthalmology. 2013;120(8):1681–1687. doi: 10.1016/j.ophtha.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 10.Afonso AA, Monroy D, Stern ME, et al. Correlation of tear fluorescein clearance and Schirmer test scores with ocular irritation symptoms. Ophthalmology. 1999;106:803–810. doi: 10.1016/S0161-6420(99)90170-7. [DOI] [PubMed] [Google Scholar]
- 11.Clinch TE, Benedetto DA, Felberg NT, et al. Schirmer's test. A closer look. Arch Ophthalmol. 1983;101:1383–1386. doi: 10.1001/archopht.1983.01040020385009. [DOI] [PubMed] [Google Scholar]
- 12.Xu KP, Yagi Y, Toda I, et al. Tear function index. A new measure of dry eye. Arch Ophthalmol. 1995;113:84–88. doi: 10.1001/archopht.1995.01100010086025. [DOI] [PubMed] [Google Scholar]
- 13.Prabhasawat P, Tseng SC. Frequent association of delayed tear clearance in ocular irritation. Br J Ophthalmol. 1998;82:666–675. doi: 10.1136/bjo.82.6.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pflugfelder SC, Tseng SC, Sanabria O, et al. Evaluation of subjective assessments and objective diagnostic tests for diagnosing tear-film disorders known to cause ocular irritation. Cornea. 1998;17:38–56. doi: 10.1097/00003226-199801000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Xu KP, Tsubota K. Correlation of tear clearance rate and fluorophotometric assessment of tear turnover. Br J Ophthalmol. 1995;79:1042–1045. doi: 10.1136/bjo.79.11.1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kheirkhah A, Casas V, Blanco G, et al. Amniotic membrane transplantation with fibrin glue for conjunctivochalasis. Am J Ophthalmol. 2007;144(2):311–313. doi: 10.1016/j.ajo.2007.03.044. [DOI] [PubMed] [Google Scholar]
- 17.Meller D, Maskin SL, Pires RT, Tseng SC. Amniotic membrane transplantation for symptomatic conjunctivochalasis refractory to medical treatments. Cornea. 2000;19(6):796–803. doi: 10.1097/00003226-200011000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Maskin SL. Effect of ocular surface reconstruction by using amniotic membrane transplant for symptomatic conjunctivochalasis on fluorescein clearance test results. Cornea. 2008;27(6):644–649. doi: 10.1097/QAI.0b013e31815e723f. [DOI] [PubMed] [Google Scholar]
- 19.Lamberts DW, Foster CS, Perry HD. Schirmer test after topical anesthesis and the tear menius height in normal eyes. Arch Ophthalmol. 1979;97:1082–1085. doi: 10.1001/archopht.1979.01020010536004. [DOI] [PubMed] [Google Scholar]
- 20.MacDonald EA, Maurice DM. The kinetics of tear fluid under the lower lid. Exp Eye Res. 1991;53:421–425. doi: 10.1016/0014-4835(91)90158-b. [DOI] [PubMed] [Google Scholar]
- 21.Fraunfelder FT. Extraocular fluid dynamics: how best to apply topical ocular medication. Trans Am Ophthalmol Soc. 1976;74:457–487. [PMC free article] [PubMed] [Google Scholar]
- 22.Rieger G. Lipid-containing eye drops: a step closer to natural tears. Ophthalmologica. 1990;201:206–212. doi: 10.1159/000310154. [DOI] [PubMed] [Google Scholar]
- 23.Grene RB. Conjunctival pleating and keratoconjunctivitis sicca. Cornea. 1991;10:367–368. doi: 10.1097/00003226-199107000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Chhadva P, Alexander A, McClellan AL, et al. The impact of conjunctivochalasis on dry eye symptoms and signs. Invest Ophthalmol Vis Sci. 2015;56(5):2867–2871. doi: 10.1167/iovs.14-16337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Höh H, Schirra F, Kienecker C, et al. Lidparrallele konjunktivale Falten (LIPCOF) sind ein sicheres diagnostisches Zeichen des trockenen Auges. Ophthalmologe. 1995;92:802–808. [PubMed] [Google Scholar]
- 26.Li DQ, Meller D, Tseng SC. Overexpression of collagenase (MMP-1) and stromelysin (MMP-3) by cultured conjunctivochalasis fibroblasts. Invest Ophthalmol Vis Sci. 2000;41:404–410. [PubMed] [Google Scholar]
- 27.Meller D, Li DQ, Tseng SC. Regulation of collagenase, stromelysin, and gelatinase B in human conjunctival and conjunctivochalasis fibroblasts by interleukin-1b and tumor necrosis factor-a. Invest Ophthalmol Vis Sci. 2000;41:2922–2929. [PubMed] [Google Scholar]
- 28.Otaka I, Kyu N. A new surgical technique for management of conjunctivochalasis. Am J Ophthalmol. 2000;129(3):385–387. doi: 10.1016/s0002-9394(99)00384-0. [DOI] [PubMed] [Google Scholar]
- 29.Yokoi N, Komuro A, Nishii M, et al. Clinical impact of conjunctivochalasis on the ocular surface. Cornea. 2005;24(8 Suppl):S24–S31. doi: 10.1097/01.ico.0000178740.14212.1a. [DOI] [PubMed] [Google Scholar]
- 30.Georgiadis NS, Terzidou CD. Epiphora caused by conjunctivochalasis: treatment with transplantation of preserved amniotic membrane. Cornea. 2001;20:619–621. doi: 10.1097/00003226-200108000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Yang HS, Choi S. New approach for conjunctivochalasis using an argon green laser. Cornea. 2013;32(5):574–578. doi: 10.1097/ICO.0b013e318255eaaa. [DOI] [PubMed] [Google Scholar]
- 32.Nakasato S, Uemoto R, Mizuki N. Thermocautery for inferior conjunctivochalasis. Cornea. 2012;31(5):514–519. doi: 10.1097/ICO.0b013e3181dc81d2. [DOI] [PubMed] [Google Scholar]
- 33.Doss LR, Doss EL, Doss RP. Paste-pinch-cut conjunctivoplasty: subconjunctival fibrin sealant injection in the repair of conjunctivochalasis. Cornea. 2012;31(8):959–962. doi: 10.1097/ICO.0b013e3182400100. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table that illustrates the summary of patient’s relevant clinical data.xls