Abstract
Objectives. To confirm the effectiveness of community health workers’ involvement as counselors or case managers in a self-help diabetes management program in 2009 to 2014.
Methods. Our open-label, randomized controlled trial determined the effectiveness of a self-help intervention among Korean Americans aged 35 to 80 years in the Baltimore-Washington metropolitan area with uncontrolled type 2 diabetes. We measured and analyzed physiological and psychobehavioral health outcomes of the community health worker–counseled (n = 54) and registered nurse (RN)–counseled (n = 51) intervention groups in comparison with the control group (n = 104).
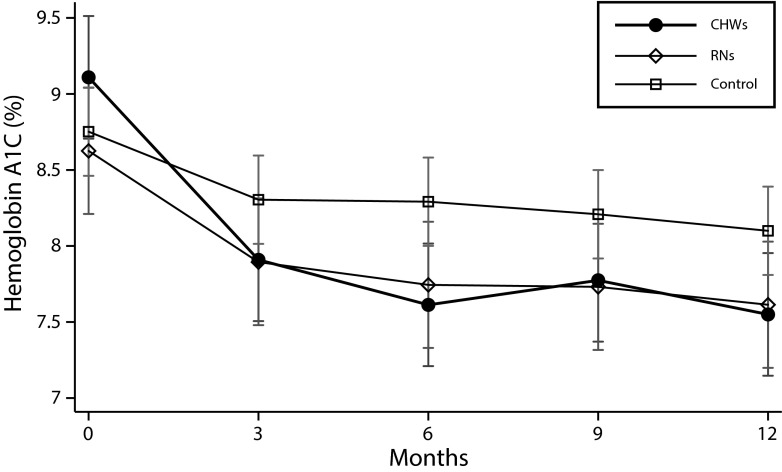
Results. The community health workers’ performance was comparable to that of the RNs for both psychobehavioral outcomes (e.g., self-efficacy, quality of life) and physiological outcomes. The community health worker–counseled group showed hemoglobin A1C reductions from baseline (–1.2%, −1.5%, −1.3%, and −1.6%, at months 3, 6, 9, and 12, respectively), all of which were greater than reductions in the RN-counseled (−0.7%, −0.9%, −0.9%, and −1.0%) or the control (−0.5%, −0.5%, −0.6%, and −0.7%) groups.
Conclusions. Community health workers performed as well as or better than nurses as counselors or case managers in a self-help diabetes management program in a Korean American community.
Community-based participatory research has been recognized as effective in addressing health disparities, especially in ethnic/linguistic minority groups.1,2 When it is combined with other theoretical frameworks that are designed to explain human behaviors, including the self-help model,3 social learning theory,4 and diffusion theory,5,6 community-based participatory research has proved especially effective in the management and control of chronic conditions, including smoking cessation,7 hypertension,8 diabetes,9,10 and depression.11
The day-to-day management and control of these chronic conditions within the naturally occurring environment is as important as, or perhaps more important than, the treatment received at the hospital, because these chronic conditions are manageable, and the related morbidities can be prevented with a level of daily attention and care that is attainable in the community. Also, for example, people with diabetes spend, on average, less than one tenth of a day per year in institutions, including hospitals, for diabetes-related treatment (International Classification of Diseases, Ninth Revision,12 codes: 250.00–250.93).13
Community-based participatory research has greatly advanced our knowledge of health promotion in the community, and it has provided best-practice models for the management of chronic conditions.14 Its contributions are most noteworthy when ethnic/linguistic minorities and underserved populations are involved9,10,15: community-based participatory research is now recognized for its potential as a mover and changer of community health.1,16,17
Despite the contributions of community-based participatory research, the question remains as to whether the potential and promise of community-based participatory research in the management of chronic conditions have been fully realized, because community-based participatory research is a process of working with the community and not ministering to the community18; it is based on an equitable partnership between the academic partner and the community partner.1,19
We report our findings from a community-based behavioral intervention clinical trial, which show the importance and centrality of the community partner and community health workers in doing community-based participatory research, not only in the recruitment and enrollment of study participants but also in the intervention. We implemented the study, Self-Help Intervention Program for Diabetes Management (SHIP-DM), in 2009 to 2014. The objective was to test the effectiveness of a community-based multimodal self-help intervention among Korean Americans with type 2 diabetes.
KOREAN AMERICAN COMMUNITY-ACADEMIC PARTNERSHIP
The community partner of the SHIP-DM was an ongoing community-based research center, the Korean Resource Center, which was established in 2001 by several Korean American community leaders and health care researchers in the Baltimore-Washington metropolitan area, with the mission of reducing health disparities and improving the quality of life in the Korean American community through scientific research.
The Korean American Community-Academic Partnership (KA-CAP) used a 1999 epidemiological survey of Korean Americans in the Baltimore-Washington region20 to identify 5 priority areas (smoking, hypertension, diabetes, depression, and cancer screening) that warranted immediate attention. Little scientific research related to Korean Americans was then available in these areas because (1) Korean Americans represented a numerically small group, constituting fewer than 0.8% of all Americans; (2) Korean Americans were scattered all over the United States in their own enclaves with a unique culture and language, and they were invisible and inaccessible to mainstream academic researchers; and, consequently, (3) studies on Korean American health consisted of only a few cross-sectional surveys and no clinical trials or intervention studies.
Underpinning the Korean Resource Center were the Community Advisory Board and community health workers. The Community Advisory Board members were Korean American community leaders of faith-based organizations, civic and social clubs, and health care providers. The Korean Resource Center was, and still is, financially and programmatically independent of the Community Advisory Board organizations, the academic partner, or other collaborators. The center negotiated its equal share with the academic partner, which usually has been set at 50% of total direct costs of publicly funded research projects. In return, the community partner actively engaged in research, from planning and administration to evaluation and dissemination, resulting in an equal partnership (Table A, available as a supplement to the online version of this article at http://www.ajph.org).
Community health workers have always played pivotal roles in our program, because they come from the same community and share the same culture and language with the study participants, and, above all, they are trusted by the members of the community. In addition to their conventional roles, including recruitment, enrollment, and retention of study participants, they were actively engaged in the intervention as counselors or case managers in our program. Only a few studies have reported employing community health workers for health coaches, counselors, or case managers, with varying degrees of fidelity.9,11,21–24
METHODS
This study was an open-label, randomized controlled trial to determine the effectiveness of a self-help intervention among Korean Americans aged 35 to 80 years with type 2 diabetes.
Theoretical Framework
Along with theoretical premises from the self-help model,3 we used a modified Predisposing, Reinforcing, and Enabling Constructs in Education/Environmental Diagnosis and Evaluation (PRECEDE)–Policy, Regulatory, and Organizational Constructs in Educational and Environmental Development (PROCEED) model.25 It enables researchers to easily connect the predisposing, enabling, and reinforcing factors to measurable health outcomes or action items. In addition, we used the RE-AIM (reach, efficacy and effectiveness, adoption, implementation, and maintenance) model to establish and refine the parameters of community health worker training on the management of chronic conditions in the community.26 The 5 components of the RE-AIM model were integrated into the community health workers’ training manual. The model also has provided a strategic frame of reference for outreach, recruitment, intervention, and dissemination; they were discussed at weekly research meetings, where attendance was mandatory for all research staff (including community health workers).
Study Participants
Details of the intervention and their effects on the primary and secondary outcomes have been reported elsewhere.27 In short, we enrolled community-dwelling Korean Americans with uncontrolled type 2 diabetes, as measured by a hemoglobin A1C level of 7.0% (53 mmol/mol) or higher, who were able to speak and read Korean. The intervention groups received didactic education or training for 12 hours focusing on the etiology of diabetes, diet, exercise, medications, stress management, and diabetes-related health literacy; this educational component was followed by monthly telephone counseling by a team of registered nurses (RNs) and community health workers.
Measurements
In addition to demographic information at baseline, we measured both physiological and psychobehavioral health outcomes; physiological data were obtained at baseline and at months 3, 6, 9, and 12 and included hemoglobin A1C and blood glucose, triglyceride, cholesterol, high-density lipoprotein, and low-density lipoprotein levels. Psychobehavioral outcomes included self-efficacy for diabetes, quality of life, diabetes knowledge, attitudes toward diabetes, and depression were measured at the same time as the physiological outcomes, except not at 9 months. Details of the outcome measures were reported elsewhere.27
RESULTS
Our KA-CAP has resulted in several benchmarks in community capacity building in the Korean American community. Through the diabetes awareness campaign and outreach efforts, we exposed the Korean American community, organizations, and individuals to our program. These efforts included printed information at least once a week in the local Korean print media (24 advertisements, 4 contributing articles, 9 feature stories), together with 25 presentations to members of Korean congregations, the distribution of 3380 brochures and handouts at 20 physicians’ offices and 15 Korean restaurants, and 63 posters. Community health workers contacted and met with Korean American organizations, newspaper managers, physicians, and owners or operators of other establishments frequented by Korean Americans.
In addition, the KA-CAP has engaged in other community-based participatory research programs in which community health workers were trained for cognitive impairment screening,28 depression screening, and breast and cervical cancer screening. Furthermore, community health workers assisted Korean Americans in enrolling in health insurance plans, including Medicaid, under the Affordable Care Act (ACA; Pub L No. 111–148) by obtaining the state-endorsed certification. The KA-CAP also provided education and training on community-based participatory research to more than 20 students, including 5 postdoctoral fellows, during this program.
Training Community Health Workers
In addition to the standard Health Insurance Portability and Accountability Act, training for health research, and Occupational Safety and Health Administration training for a safe workplace, the community health workers’ training manual covers
the principles of community-based participatory research,
the roles of community health workers,
outreach techniques (e.g., expanding the circle of friends),
communication skills with patients, and
data collection and reports.
Community health workers received an initial training of 12 hours, and they honed their skills through on-the-job training thereafter. In addition, community health workers received diabetes-specific training for 12 hours, with principal investigators and coinvestigators as the instructors. In this training, various techniques were used, including audiovisual presentations, show-and-tell, role-play, and teach-back. Instructors reviewed the community health worker trainees’ performance and fidelity to the material through a pass/fail test. Only those who passed were assigned to the functions for which they were trained. The details of community health worker training have been reported elsewhere.29
The counseling team of 4 RNs and 3 community health workers were trained in conducting motivational interviews to assist the participants in setting monthly behavioral goals and in figuring out how they could achieve their goals in the areas of diet, exercise, medication, and stress management. Once they had passed a fidelity review by the principal investigators and coinvestigators, these RNs and community health workers were assigned to counseling. All counseling sessions were recorded for quality control, and every 10th (about 10%) counseling record was cross-reviewed by another counseling team member. At the initial stage of the program, the participants assigned to the community health workers were relatively stable and had lower acuity. However, at the later stages, community health workers were able to take patients with higher counseling demands because their content knowledge about disease management and counseling capabilities had improved.
All 3 community health workers were in their early 40s and married, with 1 or 2 children. They had resided in the Korean American community for 6 to 12 years and attended church there regularly. All had received their education in Korea: 1 had completed high school, another had completed college, and the third received a master’s degree. They had no working experience in health care before joining the KA-CAP.
Recruitment and Enrollment
Challenges in recruitment and enrollment.
The KA-CAP had to overcome several challenges: (1) the target population (Korean Americans in the Baltimore-Washington metropolitan area) was spread over 3 states, (2) face-to-face screening for enrollment was mandatory, (3) only 24 months were available for screening and enrollment, and (4) the enrollment had to be aligned with the intervention schedule, in part because the intervention had to begin within a reasonable timeframe (i.e., within 4 weeks of enrollment). Logistical issues also had to be addressed because the partnership had only a limited number of personnel to deploy for both recruitment and intervention, which happened at the same time.
The confirmation of participants’ eligibility for a program such as ours tended to be time-intensive and expensive, and that presented a barrier to the recruitment of eligible participants. Because of substantial cost and time to send potential participants to the Johns Hopkins Institute for Clinical and Translational Research (Baltimore, MD) for screening laboratory tests, we devised a 3-stage screening process.
Prescreening with random blood glucose tests.
The first stage of the screening process was the use of random blood glucose tests. When a result of greater than 120 milligrams per deciliter was obtained after a fast of more than 12 hours, or 200 milligrams per deciliter after a meal, and the screened individual self-reported taking diabetes medication, we scheduled a visit to the Korean Resource Center for a further test: the A1CNow+ (Bayer Diabetes Care, Whippany, NJ). During the 24-month enrollment period, we reached out 121 times (to 32 churches, 2 trade meetings, 1 Korean festival, and 86 screening booths at Korean supermarkets), prescreening a total of 4457 subjects (with some duplications) with random blood glucose tests. The outreach team typically consisted of a nurse and 2 or 3 community health workers. Excluding travel, the outreach took an average of 3 hours for a church, 2 hours for a trade meeting, 8 hours for the festival, and 5 hours each time for the booth at the supermarket.
Screening with point of care testing.
A visit to the Korean Resource Center for the point of care testing took less than 10 minutes, and each point of care test kit cost about $10. Subjects whose result was lower than 6.8% were not eligible for the project, but they might have been diabetic; we gave a booklet in Korean on how to manage diabetes to each individual in this category. Of the 597 subjects who received the point of care testing, 334 (55.9%) subjects with test results of 6.8% or higher were scheduled for the third and final confirmatory test at the Institute for Clinical and Translational Research.
Testing hemoglobin A1C using blood serum.
The Institute for Clinical and Translational Research test confirmed that a total of 254 Korean Americans were eligible to participate in the project; 47 individuals were not eligible because their A1C level was lower than 7.0%, and an additional 2 individuals had abnormal laboratory reports. Furthermore, 4 individuals refused to participate because of scheduling conflicts. Therefore, a total of 250 subjects were finally enrolled the project and randomly assigned to the intervention (n = 120) or the control group (n = 130).
Retention.
The program was very intense, because it demanded a major commitment on the participant’s part to building adequate skills in self-help diabetes management, such as health literacy and lifestyle management, including diet, exercise, and communication skills. In addition to the initial 2 visits to the center, all participants were required to come back to the center for blood tests and questionnaire completion at 3, 6, 9, and 12 months. Interviews at each visit, including a 24-hour recall using Korean food models and a thorough medication inventory, took about 2 hours.
In particular, those in the intervention groups were asked to attend 6 education and training sessions (2 hours each) within 4 weeks of eligibility determination, to respond to monthly telephone counseling (10−50 minutes), to obtain random blood glucose measurements twice a day at home, and to keep a written diabetes diary during the project period. We provided this group with a glucose meter, strips, and lancets; none of the study participants received any monetary compensation for their participation. The control group received a shortened education and training session after program completion. When the program concluded with the last (11th) cohort, a total of 105 patients in the intervention group (54 in the community health worker−counseled and 51 in the RN-counseled) and 104 in the control group had completed the program, resulting in a retention rate of 83.6%.
Comparison of Physiological and Psychobehavioral Outcomes
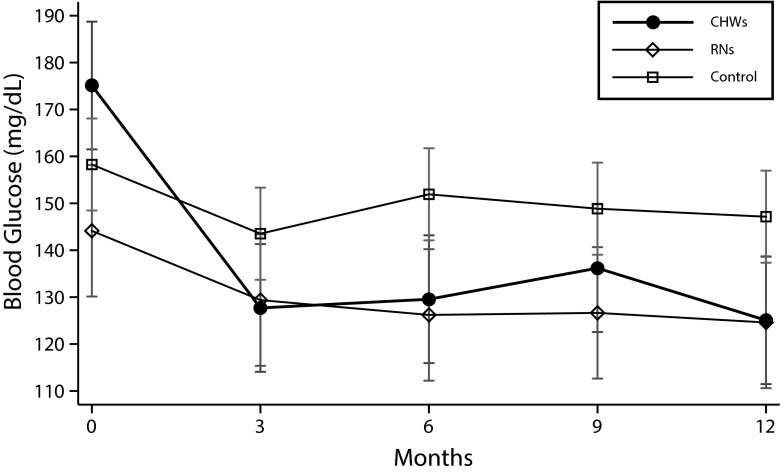
The demographic characteristics of the 3 groups (community health worker−counseled, RN-counseled, and control) at baseline were identical with regard to age, gender, marital status, educational achievement (in years), number of years in the United States, and number of years of having diabetes. Fewer participants in the community health worker−counseled group were working full or part time (42.6%) than in the RN-counseled (64.7%) or the control (65.4%) groups, and the differences were statistically significant (χ22 = 8.5; P = .015). The 3 groups were not different in physiological and behavioral indicators at baseline, except for the blood glucose level: the community health worker−counseled group showed the highest level (175.1 mg/dL), followed by the control (158.3 mg/dL) and the RN-counseled groups (144.1 mg/dL). The differences were statistically significant (F2 = 3.7; P = .027).
All 3 groups started the program with similar levels of hemoglobin A1C at baseline, although those in the community health worker−counseled group had the highest mean level. It was notable that the reductions in the community health worker−counseled group were much greater than those in the RN-counseled or the control groups. The trend toward a reduction in the community health worker−counseled group (b = −0.11; SE = 0.01; P < .001) was steeper than that in the RN-counseled (b = −0.07; SE = 0.01; P < .001) or the control (b = −0.05; SE = 0.01; P < .001) groups. As expected, these reduction trends were statistically different between the community health worker−counseled and control groups (χ21 = 13.25; P < .001) but not between the community health worker−counseled and the RN-counseled groups (χ21 = 3.24; P < .07) (Figure 1). At the end of the project, 72.2% of the individuals in the community health worker−counseled group had attained a reduction in hemoglobin A1C of more than 0.5%; this figure was higher than that in the RN-counseled (58.8%) or the control (48.1%) groups (Table B, available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 1—
Comparison of Hemoglobin A1C Changes From Baseline to 12 Months Among the Community Health Worker–Counseled, Registered Nurse–Counseled, and Control Groups of Korean Americans Aged 35–80 Years in the Baltimore-Washington Metropolitan Area With Type 2 Diabetes: 2009–2014
Note. CHW = community health worker; RN = registered nurse. Whiskers indicate 95% confidence intervals.
A similar pattern of reduction was observed in the blood glucose levels among the 3 groups: changes from baseline were statistically significant in the community health worker–counseled and RN-counseled groups from 3 months to 12 months, but only the reductions at 3 and 12 months were statistically significant in the control group. Note that the reduction trends were greatest in the community health worker–counseled group (b = −3.05; SE = 0.53; P < .001), higher than in the RN-counseled group (b = −1.39; SE = 0.55; P = .011) or in the control group (b = −0.56; SE = 0.38; P = .14; Figure 2).
FIGURE 2—
Comparison of Blood Glucose Changes From Baseline to 12 Months Among the Community Health Worker–Counseled, Registered Nurse–Counseled, and Control Groups of Korean Americans Aged 35–80 Years in the Baltimore-Washington Metropolitan Area With Type 2 Diabetes: 2009–2014
Note. CHW = community health worker; RN = registered nurse. Whiskers indicate 95% confidence intervals.
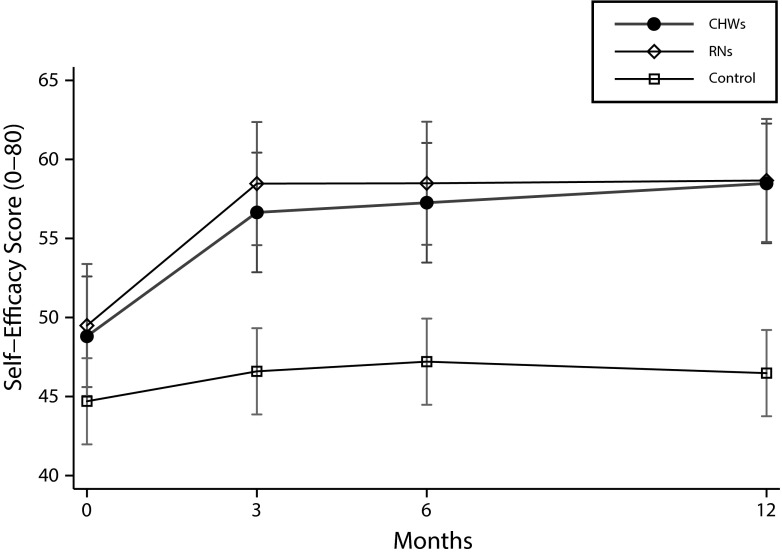
The levels of self-efficacy for diabetes changes in the community health worker–counseled and RN-counseled groups were similar at baseline, and they improved over time at almost identical rates, with the improvements being statistically significant in the community health worker–counseled group (b = 0.69; SE = 0.14; P < .001) and the RN-counseled group (b = 0.62; SE = 0.14; P < .001). However, the improvements in the control group (b = 0.12; SE = 0.10; P = .23) were not statistically significant (Figure 3).
FIGURE 3—
Comparison of Self-Efficacy for Diabetes Changes From Baseline to 12 Months Among the Community Health Worker–Counseled, Registered Nurse–Counseled, and Control Groups of Korean Americans Aged 35–80 Years in the Baltimore-Washington Metropolitan Area With Type 2 Diabetes: 2009–2014
Note. CHW = community health worker; RN = registered nurse. Whiskers indicate 95% confidence intervals.
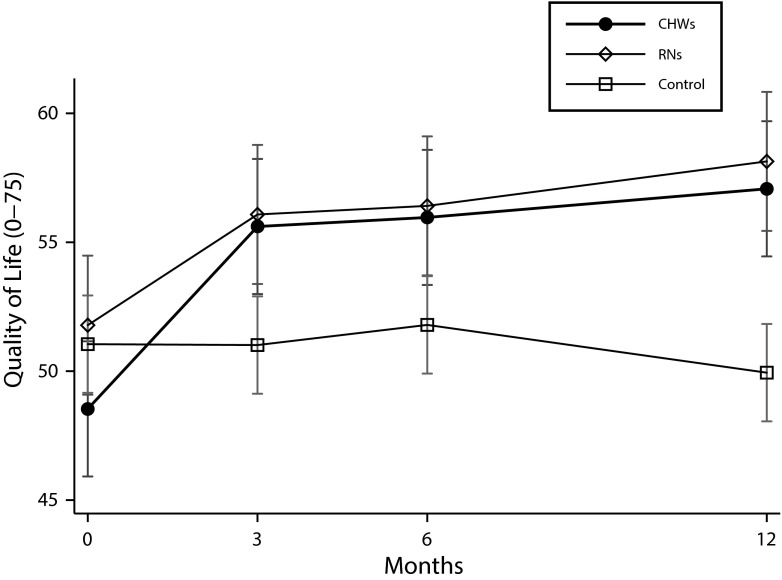
The community health worker–counseled group started the program with a lower quality of life score than did the RN-counseled group, but the community health worker–counseled group improved at a much greater rate (b = 0.60; SE = 0.10; P < .001) than did either the RN-counseled (b = 0.47; SE = 0.10; P < .001) or the control group (b = −0.09; SE = 0.07; P = .24), and at 12 months, the 2 counseled groups had almost identical quality of life scores (Figure 4).
FIGURE 4—
Comparison of Quality-of-Life Changes From Baseline to 12 Months Among the Community Health Worker–Counseled, Registered Nurse–Counseled, and Control Groups of Korean Americans Aged 35–80 Years in the Baltimore-Washington Metropolitan Area With Type 2 Diabetes: 2009–2014
Note. CHW = community health worker; RN = registered nurse. Whiskers indicate 95% confidence intervals.
DISCUSSION
Our study found that community-based participatory research is effective for the management and control of chronic conditions such as type 2 diabetes in a naturally occurring environment, especially in an ethnic/linguistic minority community. Furthermore, our findings indicate that community health workers are the most important asset and resource in the community-based participatory research process because they are the primary contact with study participants and are the motivators, coaches, and, most importantly, trusted friends of the patients. For example, in our clinical trials, health outcomes were improved in both of the intervention groups and the control group, although the improvements in the intervention groups were statistically higher than those in the control group.8 This result can be explained by the fact that participation in our clinical trial by itself constituted an intervention, with those in the control group receiving less attention.
The beneficial effects can be further amplified by community health workers’ active engagement with participants in the community because of their proximity to patients, without language or cultural barriers. Community health workers were flexible in scheduling telephone calls and site visits, sometimes in the evenings and on weekends, so that they were convenient for the participants. Furthermore, trust was built by the frequent contacts between community health workers and study participants: a community health worker met with each assigned individual 3 times during enrollment and 6 times during the education intervention; they then had 5 more meetings with each participant for data collection and counseled each participant in the intervention group up to 11 times via telephone. The community health workers contacted the control group less frequently, omitting the 6 meetings for education and the 11 telephone calls for counseling, but they contacted both groups via telephone numerous times to schedule appointments for follow-up.
The findings provide valuable insight into the effectiveness of community health workers as interventionists. Given the scarcity of bilingual health care providers in certain linguistically isolated communities, having community health workers as counselors or case managers is a viable option or strategy for extending the capacity of community-based participatory research and to fill the gap in the community-based management of chronic conditions. Their new role as a case manager is feasible because of structured training based on the community health workers’ training manual and because of constant assessment and refinement of community health workers’ capacity and fidelity.
Our KA-CAP was effective in community-based participatory research because we were able to overcome what is probably the biggest challenge in the academic-community partnership, although a delicate and often invisible one: discussion, negotiation, and agreement about the sharing of power, control, and resources by the 2 partners.30–32 The process may not always be smooth, partly because those representing the academic partner can be reluctant to yield control over the research process. The voice of the academic partner often dominates community-based participatory research studies, whereas the voice of the community partner has tended to be treated as a backdrop. For example, the community partners are often included as coauthors in published articles that report planning or capacity-building processes, but they are rarely included as coauthors in articles reporting the results of intervention studies, let alone made the first or corresponding author on the relevant articles. The disappearance of the community partner in the dissemination process may reflect the reality of community-based participatory research, with the community partner generally fading away after the completion of the data collection. However, our KA-CAP chose to share resources and control equally, resulting in a win-win outcome for all stakeholders, including the community and academic partners, the community and its members, and the sponsored institutions.
PUBLIC HEALTH IMPLICATIONS
The prevalence of diabetes is expected to rise in the nation33 and in the world34 in the future, indicating that a gap exists in the current diabetes management and control system. Our study confirmed the usefulness of a community-based “bottom-up” approach as “a local solution to a global problem”35 of managing and controlling diabetes in a naturally occurring community setting.
The KA-CAP is in line with national health care reform, which is emphasizing the importance of prevention and patient engagement in treatment36 and creating healthier communities (ACA, Title IV, Subtitles A, B, & C; Title V). The act also requires the transformation of health care workforces, and our study provides strong empirical evidence that with proper training and collaboration, community health workers can be effective frontline primary and secondary prevention workers, especially in linguistic/ethnic minority communities.
ACKNOWLEDGMENTS
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (grant R18DK083936), with material support from LifeScan (Milpitas, CA), including devices (OneTouch glucometer, OneTouch UltraSoft test strips, and OneTouch UltraSoft lancets) for study participants. In addition, the Johns Hopkins Institute for Clinical and Translational Research supported the cost of the blood serum laboratory tests.
We are grateful for the substantial editorial assistance provided by Deborah McClellan, PhD. We thank our current and former community health workers, especially Lily Chin, Jung-Ah Ahn, and Hyun-Joo Kim, for their hard work.
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or other sources of support.
HUMAN PARTICIPANT PROTECTION
The research protocol was approved by the Johns Hopkins Medical Institutions institutional review board, and written consent was obtained from all study participants.
REFERENCES
- 1.Israel BA, Coombe CM, Cheezum RR et al. Community-based participatory research: a capacity-building approach for policy advocacy aimed at eliminating health disparities. Am J Public Health. 2010;100:2094–2102. doi: 10.2105/AJPH.2009.170506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferreira MP, Gendron F. Community-based participatory research with traditional and indigenous communities of the Americas: historical context and future directions. Int J Crit Pedagogy. 2011;3:153–168. [Google Scholar]
- 3.Braden CJ. Learned self-help response to chronic illness experience: a test of three alternative learning theories. Sch Inq Nurs Pract. 1990;4(1):23–41. [PubMed] [Google Scholar]
- 4.Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice Hall; 1977. [Google Scholar]
- 5.Tandon SD, Phillips K, Bordeaux BC et al. A vision for progress in community health partnerships. Prog Community Health Partnersh. 2007;1(1):11–30. doi: 10.1353/cpr.0.0007. [DOI] [PubMed] [Google Scholar]
- 6.Green LW, Ottoson JM, Garcıa C, Hiatt RA. Diffusion theory and knowledge dissemination, utilization, and integration in public health. Annu Rev Public Health. 2009;30:151–174. doi: 10.1146/annurev.publhealth.031308.100049. [DOI] [PubMed] [Google Scholar]
- 7.Andrews JO, Newman SD, Heath J, Williams LB, Tingen M. Community-based participatory research and smoking cessation interventions: a review of the evidence. Nurs Clin North Am. 2012;47:81–96. doi: 10.1016/j.cnur.2011.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim KB, Han HR, Huh BY, Nguyen T, Lee HB, Kim MT. The effect of a community-based self-help multimodal behavioral intervention in Korean American seniors with high blood pressure. Am J Hypertens. 2014;27:1199–1208. doi: 10.1093/ajh/hpu041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gary TL, Batts-Turner M, Yeh HC et al. The effects of a nurse case manager and a community health worker team on diabetic control, emergency department visits, and hospitalizations among urban African Americans with type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2009;169:1788–1794. doi: 10.1001/archinternmed.2009.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim MT, Han HR, Song HJ et al. A community-based, culturally tailored behavioral intervention for Korean Americans with type 2 diabetes. Diabetes Educ. 2009;35:986–994. doi: 10.1177/0145721709345774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim MT, Kim KB, Han HR, Huh B, Nguyen T, Lee HB. Prevalence and predictors of depression in Korean American elderly: findings from the Memory and Aging Study of Koreans (MASK) Am J Geriatr Psychiatry. 2015;23(7):671–683. doi: 10.1016/j.jagp.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980. [Google Scholar]
- 13.Agency for Healthcare Research and Quality. National Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP) Available at: http://hcupnet.ahrq.gov/HCUPnet.jsp. Accessed January 21, 2015. [PubMed]
- 14.Lorig K, Ritter PL, Villa FJ, Armas J. Community-based peer-led diabetes self-management: a randomized trial. Diabetes Educ. 2009;35:641–651. doi: 10.1177/0145721709335006. [DOI] [PubMed] [Google Scholar]
- 15.Hill-Briggs F, Lazo M, Peyrot M et al. Effect of problem-solving-based diabetes self-management training on diabetes control in a low income patient sample. J Gen Intern Med. 2011;26:972–978. doi: 10.1007/s11606-011-1689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010;100(suppl 1):S40–S46. doi: 10.2105/AJPH.2009.184036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Israel BA, Schulz AJ, Parker EA, Becker AB. Community-based participatory research: policy recommendations for promoting a partnership approach in health research. Educ Health (Abingdon) 2001;14(2):182–197. doi: 10.1080/13576280110051055. [DOI] [PubMed] [Google Scholar]
- 18.Peterson JC. CBPR in Indian Country: tensions and implications for health communication. Health Commun. 2010;25:50–60. doi: 10.1080/10410230903473524. [DOI] [PubMed] [Google Scholar]
- 19.Black KZ, Hardy CY, De Marco M et al. Beyond incentives for involvement to compensation for consultants: increasing equity in CBPR approaches. Prog Community Health Partnersh. 2013;7:263–270. doi: 10.1353/cpr.2013.0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim MT, Kim KB, Juon HS, Hill MN. Prevalence and factors associated with high blood pressure in Korean Americans. Ethn Dis. 2000;10:364–374. [PubMed] [Google Scholar]
- 21.DePue JD, Dunsiger S, Seiden AD et al. Nurse-community health worker team improves diabetes care in American Samoa: results of a randomized controlled trial. Diabetes Care. 2013;36:1947–1953. doi: 10.2337/dc12-1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Henderson VA, Barr KLC, An LC et al. Community-based participatory research and user-centered design in a diabetes medication information and decision tool. Prog Community Health Partnersh. 2013;7:171–184. doi: 10.1353/cpr.2013.0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gerber BS, Rapacki L, Castillo A et al. Design of a trial to evaluate the impact of clinical pharmacists and community health promoters working with African-Americans and Latinos with diabetes. BMC Public Health. 2012;12:891. doi: 10.1186/1471-2458-12-891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kahn LS, Tumiel-Berhalter L, D’Aniello R et al. The impacts of “Growing Our Own”: a pilot project to address health disparities by training health professionals to become certified diabetes educators in safety net practices. Diabetes Educ. 2012;38(1):86–93. doi: 10.1177/0145721711427455. [DOI] [PubMed] [Google Scholar]
- 25.Green LW, Kreuter MW. Health Promotion Planning: An Educational and Environmental Approach. 2nd ed. Mountainview, CA: Mayfield Publishing; 1991. [Google Scholar]
- 26.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim MT, Kim KB, Huh B et al. The effect of a community-based self-help intervention: Korean Americans with type 2 diabetes. Am J Prev Med. 2015;49:726–737. doi: 10.1016/j.amepre.2015.04.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Han HR, Park SY, Song H, Kim M, Kim KB, Lee HB. Feasibility and validity of dementia assessment by trained community health workers based on Clinical Dementia Rating. J Am Geriatr Soc. 2013;61(7):1141–1145. doi: 10.1111/jgs.12309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Han HR, Kim KB, Kim MT. Evaluation of the training of Korean community health workers for chronic disease management. Health Educ Res. 2007;22(4):513–521. doi: 10.1093/her/cyl112. [DOI] [PubMed] [Google Scholar]
- 30.Lowry KW, Ford-Paz R. Early career academic researchers and community-based participatory research: wrestling match or dancing partners? Clin Transl Sci. 2013;6:490–492. doi: 10.1111/cts.12045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.May M, Law J. CBPR as community health intervention: institutionalizing CBPR within community based organizations. Prog Community Health Partnersh. 2008;2(2):145–155. doi: 10.1353/cpr.0.0019. [DOI] [PubMed] [Google Scholar]
- 32.Weiss ES, Stevenson AJ, Erb-Downward J et al. Sustaining CBPR partnerships to address health disparities in times of economic instability. J Health Care Poor Underserved. 2012;23:1527–1535. doi: 10.1353/hpu.2012.0170. [DOI] [PubMed] [Google Scholar]
- 33.Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr. 2010;8:29. doi: 10.1186/1478-7954-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103(2):137–149. doi: 10.1016/j.diabres.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 35.Singh P, Chokshi DA. Community health workers-a local solution to a global problem. N Engl J Med. 2013;369:894–896. doi: 10.1056/NEJMp1305636. [DOI] [PubMed] [Google Scholar]
- 36.Patient-Centered Outcomes Research Institute. National Priorities for Research and Research Agenda. 2012. Available at: http://www.pcori.org/assets/PCORI-National-Priorities-and-Research-Agenda-2012-05-21-FINAL1.pdf. Accessed February 15, 2015.