Abstract
Sexual concerns are prevalent in women with cancer or cancer history and are a factor in patient decision-making about cancer treatment and risk-reduction options. Physical examination of the female cancer patient with sexual concerns, regardless of the type or site of her cancer, is an essential and early component of a comprehensive evaluation and effective treatment plan. Specialized practices are emerging that focus specifically on evaluation and treatment of women with cancer and sexual function problems. As part of a specialized evaluation, oncologists and their patients should expect a thorough physical examination to identify or rule out physical causes of sexual problems or dysfunction. This review provides oncology professionals with a description of the physical examination of the female cancer patient with sexual function concerns. This description aims to inform anticipatory guidance for the patient and to assist in interpreting specialists’ findings and recommendations. In centers or regions where specialized care is not yet available, this review can also be used by oncology practices to educate and support health care providers interested in expanding their practices to treat women with cancer and sexual function concerns.
Key words/phrases: cancer, female, physical examination, sexual dysfunction, survivorship
INTRODUCTION
Sexual function concerns are prevalent in women with cancer or cancer history1–12 and are a factor in patient decision-making about cancer treatment and risk-reduction options.13–15 Several cancer programs in the United States, Canada, Europe and Australia have opened specialized clinical practices that focus specifically on evaluation and treatment of females with cancer and sexual concerns.16–19 With the emergence of new treatment options for female sexual dysfunction,20,21 patients are likely to ask their oncology providers about this aspect of their health.22 As part of a referral for specialized evaluation, oncologists and their patients should expect a thorough physical examination to identify or rule out physical causes of sexual problems or dysfunction.
Female sexual function concerns commonly present with physical, psychological and interpersonal components.23–28 While the majority of women presenting for sexual concerns after cancer have breast or gynecologic cancer types,16,23 reflecting overall cancer prevalence29 and survival rates,30 sexual concerns are common among patients with other cancer types as well.3,6–8,10 Common sexual concerns seen among these patients include those associated with iatrogenic menopause and estrogen deprivation therapy: severe vaginal dryness, painful intercourse, difficulty with arousal and orgasm, and diminished or low libido.31,32 Body image changes and loss of breast or genital erogenous sensation or sexual pleasure are also common,32,33 including among women without, but at elevated risk of, cancer who elect prophylactic mastectomy with immediate reconstruction.34,35 Genital radiation changes, ostomy, diarrhea and stool or flatus incontinence can impair sexual function in women with colorectal cancer.36–39 Pain with kissing,40 dry mouth,41 and loss of smell and taste6 can interfere with sexual function in women with head and neck cancer. Graft-versus-host disease (GVHD) can manifest genitally in women who undergo bone marrow or peripheral blood stem cell transplant for hematologic cancers and cause severe, chronic discomfort in addition to painful intercourse.42,43 Fatigue, disordered sleep, anxiety, depression, relationship strain and partner sexual problems are also common cofactors in women with cancer.44–47
Systematic physical examination of the female cancer patient with sexual concerns, regardless of the type or site of her cancer, is an essential and early component of a comprehensive evaluation and effective treatment plan. Evaluation without physical examination can result in misdiagnosis and failed treatment of sexual function problems. This review provides oncology professionals with a description of the physical examination of the female cancer patient with sexual function concerns. This description aims to inform anticipatory guidance for the patient and to assist in interpreting specialists’ findings and recommendations. In centers or regions where specialized care is not yet available, this review can be used by oncology practices to educate and support health care providers interested in expanding their practices to treat women with cancer and sexual function concerns.
BUILDING THE EVIDENCE BASE FOR THE SYSTEMATIC PHYSICAL EXAMINATION OF FEMALES WITH CANCER AND SEXUAL FUNCTION CONCERNS
Although essential to patient care, no standard practice for physical examination of the female with cancer and sexual function concerns has been established and the literature is sparse on this specific topic. The Scientific Network on Female Sexual Health and Cancer (the Network) was created as an interdisciplinary cooperative group in 2009 that includes behavioral and mental health professionals, educators, nurses, patients, physical therapists, physicians and surgeons (including medical, surgical, gynecologic, and radiation oncologists), and allied professionals working in the field to accelerate the evidence-base and improve the consistency and quality of care for this patient population.48 The Network complements the important work of other groups, with which many Network members are also affiliated (Table 1). Oncologists who refer to or seek to support development of a specialized practice for cancer and female sexuality can find assistance and education from these organizations and should expect specialists in the field to be affiliated with one or more of these or similar professional groups.
Table 1.
Select Professional Group Affiliations of Scientific Network Members: Organizations that Work to Advance Knowledge and Practice to Improve Female Sexual Outcomes
| Organization | Website |
|---|---|
| African Society for Sexual Medicine (ASSM) | http://www.assmweb.org/ |
| American Association of Sex Educators, Counselors and Therapists (AASECT) | http://www.aasect.org/ |
| American Congress of Obstetricians and Gynecologists (ACOG) | http://www.acog.org/ |
| British Society for Sexual Medicine (BSSM) | http://www.bssm.org.uk/ |
| Childhood Gynecologic Cancer Association (CGYNCA) | http://cgynca.org/ |
| European Society for Sexual Medicine (ESSM) | http://www.essm.org/ |
| International Society for Sexual Medicine (ISSM) | http://www.issm.info/ |
| International Society for the Study of Vulvovaginal Disease (ISSVD) | http://issvd.org/ |
| International Society for the Study of Women’s Sexual Health (ISSWSH) | http://www.isswsh.org/ |
| Scientific Network on Female Sexual Health and Cancer | http://cancersexnetwork.org/ |
| Sexual Medicine Society for North America (SMSNA) | http://www.smsna.org/ |
| Society of Gynecologic Oncology (SGO) | https://www.sgo.org/ |
| Society for Sex Therapy and Research (SSTAR) | http://www.sstarnet.org/ |
| World Association for Sexual Health (WAS) | http://www.worldsexology.org/ |
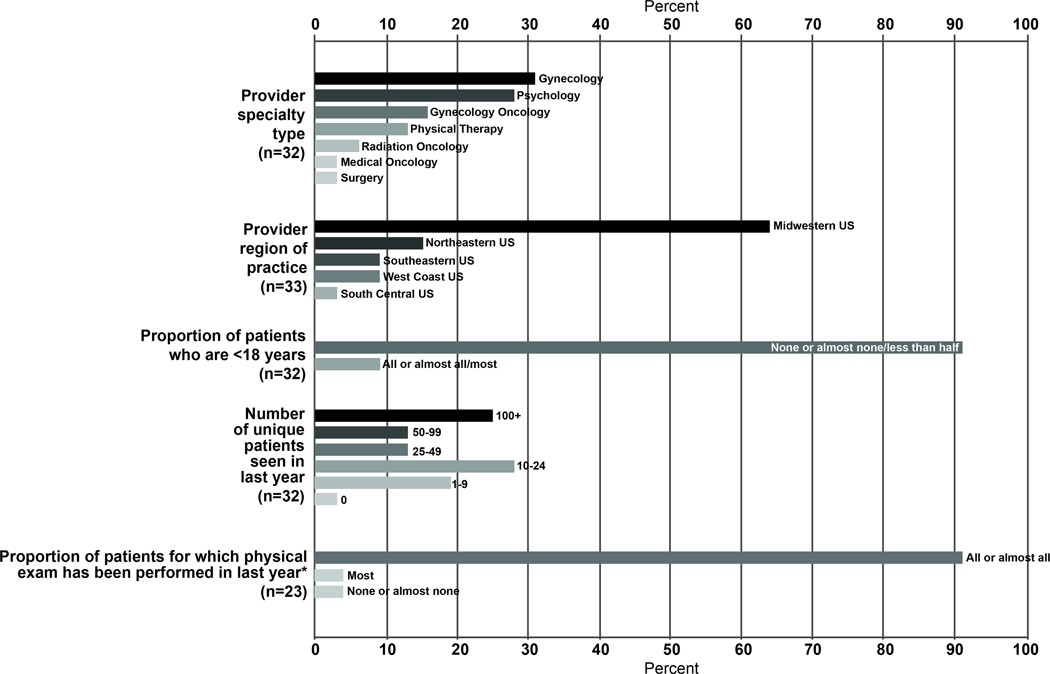
This review by an interdisciplinary subgroup of Network members draws on the best available literature about physical examination of females with cancer and women with sexual function concerns. Review elements, adapted from the Cochrane review framework,49 were operationally defined to guide the literature search by content experts in each area of the physical examination (Table 2). Given the dearth of literature specifically on this topic, expert opinion was solicited from Network members via a brief web-based survey50 (administered and received in advance of the Network’s September 2013 meeting) and a plenary session at the 2013 annual Network meeting. The survey elicited information about physical examination practices across a diversity of providers (N=34) and practices and, to our knowledge, is the only such survey to be fielded on this topic (Figure 1). A plenary session was held to share the web survey results and gain additional input on two key questions: 1) Should a physical examination be performed on all patients with cancer or cancer history who present with sexual concerns? and 2) What are the essential examination elements? Characteristics of respondents generally reflected the disciplinary and geographic diversity of the Network membership at the time of the survey. Data collected from the web-based survey and feedback from the Network conference were used to complement findings from the review of literature. The survey was administered by the Lindau Lab at the University of Chicago and deemed exempt by the University of Chicago Institutional Review Board.
Table 2.
| Review Element | Operational Definition |
|---|---|
| Participants | Females (adult, adolescent, girl) with cancer or women at high risk of cancer who had undergone treatment (surgery, radiation, chemotherapy, hormonal therapy). |
| Interventions | Methods employed for physical examination of females with cancer and sexual problems. |
| Comparisons | Physical examination findings from different systematic physical examination methods that could be used to track individual change over time and to compare outcomes across patient populations seen at different clinical sites. |
| Outcomes | Valid and reliable physical examination findings in the anatomical domains relevant to female sexual function. |
| Search engines | PubMed, MEDLINE and other search engines more specific or relevant to each anatomical domain dating from September 29, 2015 and prior as specific to the engine used. PubMed, which contains all MEDLINE indexed journals, is the preferred search engine and contains publications dating back to 1946. |
Cochrane Review Guidelines‡ were adapted to generate operational definitions for each literature review element and to review the relevant literature using identified search engines. Publications that adhered to the stated operational definition for each review element were included. Relevant literature pertaining to females without cancer was reviewed and considered when no cancer-specific evidence could be found.
49. Cochrane Community. Cochrane Reviews. Available from: http://community.cochrane.org/cochrane-reviews. [Accessed March 25, 2015].
Figure 1.
Scientific Network on Female Sexual Health and Cancer Survey Respondent Provider and Practice Characteristics
WHAT REFERRING ONCOLOGISTS AND PATIENTS SHOULD EXPECT FROM PHYSICAL EVALUATION FOR SEXUAL FUNCTION CONCERNS
Who should have a physical examination?
Attendees of the 2013 Network meeting unanimously agreed that a directed and age-appropriate systematic physical examination is necessary to establish virtually every patient’s treatment plan. No literature was found to counter this opinion. The general exception identified was the rare case in which, in the specialist’s judgment, the risks of examination clearly outweigh the benefits. It is also appropriate for the specialist to forgo or delay the internal gynecologic component of the examination of an adolescent patient (as described in further detail below), or in cases where the patient makes informed refusal, cannot tolerate the examination, or is near the end of life.
Who should perform a physical examination?
Patient-centered oncology51 practice includes brief assessment in the domain of sexual function.52,53 When these issues arise, oncology providers will typically refer to a collaborating provider rather than perform comprehensive evaluation and treatment. In some oncology settings (e.g. MD Anderson radiation oncology practice, University of Wisconsin Carbone Cancer Center) the physical examination component of specialized care for sexual concerns is performed by advanced practice nurses or physician assistants on the oncology team.
Thorough evaluation of the female patient with cancer and sexual function concerns should include a comprehensive physical examination by a provider with expertise in genitopelvic examination skills, knowledge of cancer pathophysiology, and ability to collaborate with the patient’s treating oncologist. Although cancer surveillance is not the primary focus of most sexual medicine specialists, providers performing physical examination in this patient population should be competent to identify and refer for findings suggestive of malignancy. Female patients with cancer and sexual concerns often times self-refer for specialized care rather than raise the issue with the oncology team.54 Depending in part on availability of local services and the timing and nature of her concerns, the patient may present to a physician, advanced practice nurse, or other provider from among a wide diversity of disciplines such as gynecology, physical therapy, primary or survivorship care, psychology or social work, or dermatology. By proactively screening for sexual function concerns,55,56 oncologists can direct their patients in need of specialized care and maintain a high standard of coordination with this aspect of the patient’s care.
COORDINATING THE SPECIALIZED EVALUATION FOR SEXUAL FUNCTION CONCERNS WITH OTHER ASPECTS OF CANCER OR SURVIVORSHIP CARE
Across the continuum of cancer and survivorship care,57,58 chronic medical conditions and routine health maintenance should be addressed prior to initiating specialized care for female sexual concerns. In some settings, the same provider may be responsible for both aspects of the patient’s care. Ideally, the patient and specialist will work collaboratively with both primary care and oncology to effect a treatment plan to align with the patient’s other health needs. Specialists are best-positioned to efficiently evaluate and treat this patient population when the following care coordination elements are in place.
Patients in Active Cancer Care
Female patients with cancer should be informed by the oncology care team about potential short and long-term side effects of cancer treatment, including the possibility of sexual function problems.53,59,60
Female patients with cancer should be in the care of a treating oncology provider, including a hospice or palliative care provider, who is available to the specialist for consultation and care coordination.
Patients undergoing pelvic radiation should be educated by the radiation oncology team before initiating treatment about the possible effects of radiation on vaginal capacity for penetration (e.g. for vaginal speculum or digital examination, or transvaginal ultrasound) and sexual function. A rationale and plan for vaginal dilation should be discussed.60–63 Baseline vaginal capacity and sexual function should be objectively assessed (discussed below) and communicated to the patient before initiating treatment. If not addressed prior to treatment, patients should be seen after the acute vulvar/perineal/perianal inflammatory phase resolves to initiate a vaginal dilation plan and address other sexual function and vaginal capacity concerns.
Patients in Survivorship Care
After cancer treatment is complete, a female with a history of cancer should be in the care of a clinical provider who is attuned to cancer survivorship guidelines53 and available to the specialist for consultation and care coordination.
Untreated chronic medical conditions and late effects of cancer treatment64,65 may be the cause of sexual concerns and should be addressed before specialized evaluation for such concerns.66–68
Gynecologic conditions such as abnormal uterine bleeding or a pelvic mass may be the cause of, and should be addressed before specialized evaluation for, sexual concerns.
General Health Screenings
The patient should be current on appropriate health screenings (e.g. mammogram, pelvic examination, cervical cancer screening, colonoscopy, bone mineral density test) as abnormalities in these areas could influence management of sexual function concerns, especially use of hormone therapies.
OVERVIEW OF THE SPECIALIZED CLINICAL ENCOUNTER FOR EVALUATING FEMALE SEXUAL CONCERNS IN THE CONTEXT OF CANCER OR CANCER HISTORY
Thorough assessment of the female with cancer and sexual concerns typically begins with a clinical intake survey that the patient self-completes. To our knowledge, no standard intake survey has been published; in our own practices, the intake survey for this patient population covers: 1) past medical, reproductive and surgical history, including cancer and treatment history, injuries, menstrual/menopause status, mental health, status of screening and routine health maintenance; 2) medications and allergies; 3) review of systems including sexual concerns and function; 4) partner status, partner health and sexual function; 5) family medical history; 6) history of abuse (physical, emotional, psychological, sexual); 7) nutrition, exercise, sleep, substance use and other health behaviors; 8) screening for anxiety and depression; and 9) referring, primary and oncology provider contact information.
Patient Self-Report of Symptoms
Patient-reported symptoms such as altered mood, disrupted sleep and disturbed thought content are included in review of systems and a comprehensive psychosocial history. Depression and anxiety are prevalent and often go untreated in this patient population.33,44,69,70Mood and anxiety can be further assessed using standardized self-report measures, such as HADS (Hospital Anxiety and Depression Scale), a brief, 14-item self-report questionnaire used with cancer patients as a screening tool.71,72
Baseline Assessment of Sexual Function
Baseline assessment of partnership, gender, identity/orientation, sexual activity, sexual behavior, sexual function and related distress, relationship quality, and sexual abuse and trauma are imperative. The literature offers several self-report tools that are variably used by clinicians for baseline and serial assessment of sexual function in women with cancer.55 Although beyond the scope of this review, these tools have been very capably reviewed by Jeffrey, Flynn, and colleagues in the development of the National Cancer Institute Patient-Reported Outcomes Measurement Information System (PROMIS) Sexual Function and Satisfaction Measures.73–75 Findings from the systematic physical examination should be combined with information elicited from history-taking76–79 and patient self-report56,80–83 to provide a full assessment of sexual functioning and concerns.
THE COMPREHENSIVE PHYSICAL EXAMINATION
The purpose of the physical examination
The routine gynecologic examination performed in the general gynecology or in the gynecology oncology setting typically does not include all of the elements needed to thoroughly assess a patient with sexual function concerns. The purpose of physical examination in female patients with cancer or cancer history and sexual function concerns is to identify and inform the patient of normal and abnormal findings and to determine the salience of these findings to the patient’s presenting symptoms. Patients commonly present with little or no information about sexual side effects of treatment84–87 and with ideas or fears about post-cancer changes to their internal and external genital anatomy.26 In our practices, many female patients report that they have never “looked down there,” or that they have tried, but encountered physical or emotional difficulty.
Elements of the physical examination
The following core elements are performed as part of the routine, age-appropriate systematic physical examination of female patients with cancer or cancer history seeking care for sexual function concerns. An expanded examination may be necessary, depending on the patient’s presentation, cancer type, and clinician judgment. While findings may differ across the cancer care and survivorship continuum, the examination elements are the same. In our experiences, the specialized physical examination for a new patient, using the steps described below, typically takes 10–12 minutes to complete. The order of steps in the physical examination may vary by provider. For example, the physical therapist commonly begins with the general musculoskeletal examination, because this information can be used to inform the specialized assessment of the pelvic floor. With the adult patient, the gynecologist typically begins with the genitopelvic examination. There is no evidence to suggest general benefit of one examination order or another. Table 3 presents detailed, descriptive terms for documenting physical examination findings pertinent to female sexual function by anatomic location.
Table 3.
Key Descriptors for Physical Examination Findings by Anatomical Site in Females with Cancer and Sexual Function Concerns
| Findings and Descriptors | |||||
|---|---|---|---|---|---|
| Anatomical Site | Inspection | Palpation | Specialized Testing | ||
| Normal | Changes | Normal | Changes | ||
| Vulvovaginal examination | |||||
| Inguinal canal |  |
Mass | Small, mobile, non-tender lymph nodes, symmetrical | Firm, enlarged, tender lymph nodes; edema; hernia; lymphocyst |  |
| Mons pubis | Presence of pubic hair covering mons, labia majora. Adolescents: Tanner stage | Decreased, sparse or absent pubic hair due to treatment or personal alteration; radiation changes such as edema (pitting/non-pitting, location); tattoos and/or genital piercing; pigmented lesions, rash or other skin changes | No lesions, tenderness or masses | Presence of lesions, tenderness, or masses |  |
| Labia majora* | Normal size, symmetry | Note abnormal size or symmetry of structures; presence of agglutination, atrophy, edema, erosions, erythema, fissures, granulation, excoriation, laceration, fissures, inflammation, lesions, reticulated leukokeratosis, scars, ulceration, or nodules; urethral caruncle, prolapse, pallor | No lesions, tenderness or masses | Presence of lesions, tenderness, or masses; urethral or peri-urethral glandular discharge | Culture any discharge exuded from palpationof paravaginal glands, peri-urethral glands, urethra |
| Labia minora* Interlabial sulcus folds* | |||||
| Bartholin's glands | Small, ~1–2 mm pink orifice, medial aspect inferior labia minora | Presence and size of Bartholin's gland cyst | No discharge, erythema, swelling or tenderness | Presence of discharge, erythema, swelling or tenderness |  |
| Clitoris* | Size typically 1.5–2cm long by <0.5cm wide; pink color | Agglutination or phimosis, clitoromegaly, pigmented or other lesions | Sensation to pressure | Absence of sensation; tenderness | Hormonal and radiologic testing for clitoromegaly237 |
| Perineum | Normal size, symmetry | Note abnormal size or symmetry of structures; presence of agglutination, atrophy, edema, granulation, excoriation, laceration, fissures, inflammation, lesions, scars, ulceration, or nodules; urethral caruncle, prolapse, pallor | No lesions, tenderness or masses | Presence of lesions, tenderness, or masses; urethral or peri-urethral glandular discharge | Culture any discharge exuded from palpationof paravaginal glands, peri-urethral glands, urethra |
| Vestibule | Pink, glistening | Erythema, pallor, fissures, lesions | No lesions, tenderness or masses | Presence of lesions, tenderness or masses | Cotton swab test - vulvar pain mapping121,123 |
| Vaginal opening (introitus) | Normal size, non-malodorous physiologic discharge, rugae visible | Presence of agglutination, atrophy‡, bleeding, contraction, dehiscence, discharge, dryness, erythema§,‖, pallor, scarring, stenosis or telangiectasia. Note relaxed introitus or bulge from rectocele, cystocele or vaginal vault prolapse. | Easily insert 1–2 fingers without pain | Adhesions, atrophy, dryness, fibrosis, inelasticity, scarring or stenosis | Graduated vaginal dilator examination as described in text |
| Urethral meatus | Normal size, symmetry | Note abnormal size or symmetry of structures; presence of agglutination, atrophy, edema, granulation, excoriation, laceration, fissures, inflammation, lesions, scars, ulceration, or nodules; urethral caruncle, prolapse, pallor | No lesions, tenderness or masses | Presence of lesions, tenderness, or masses; urethral or peri-urethral glandular discharge | Culture any discharge exuded from palpationof paravaginal glands, peri-urethral glands, urethra |
| Skene's glands | Small, ~1 mm pink orifice inferior and lateral to urethral meatus | Presence and size of Skene's gland cyst (rare) | No discharge, erythema, swelling or tenderness | Presence of discharge, erythema, swelling or tenderness |  |
| Urethra | Normal size, symmetry | Note abnormal size or symmetry of structures; presence of agglutination, atrophy, edema, granulation, excoriation, laceration, fissures, inflammation, lesions, scars, ulceration, or nodules; urethral caruncle, prolapse, pallor | No lesions, tenderness or masses | Presence of lesions, tenderness, or masses; urethral or peri-urethral glandular discharge | Culture any discharge exuded from palpation of paravaginal glands, peri-urethral glands, urethra |
| Bladder |  |
 |
Non-tender | Tender, cystocele, full (even after patient voids) |  |
| Vagina | Pink, rugae, physiologic discharge; non-malodorous; 6–7 cm vaginal length; if hysterectomy, cuff intact | Agglutination, ecchymoses, abnormal discharge, decreased or absent ruggae, fibrosis, granulation tissue, hematocolpos, laxity, masses, pallor, scarring, stenosis | Elastic, non-tender, lubricated, rugated | Dry, hematocolpos, inelastic, nodular, tender | Vaginal pH test; KOH and saline wet prep test for BV, yeast, trichomonas. Can also use wet prep to visualize superficial epithelial cells, which will be rare to absent inatrophic vaginitis. Pelvic Organ Prolapse Quantification (POP-Q)to assess pelvic organ prolapse131 |
| Vaginal mucosa | |||||
| Vaginal walls | |||||
| Cervix* | Present or absent; ectropion size; nabothian cyst size, location | Bleeding, discharge, masses, nodules, scarring, ulceration | No cervical motion, tenderness; uniform, "cartilaginous" feel. | Cervical motion tenderness, fibrosis, firmness, tenderness, nodularity | Screening for Gonorrhea/Chlamydia. Screening Pap/HPV if indicated and in sync with primary care |
| Uterus* |  |
 |
6 wk size or smaller, mobile, well-supported | Hematometra, mass, nodule(s), uterine prolapse, uterine or adnexal tenderness, fixed or firm adnexae |  |
| Adnexa* | Small, may not be palpable; mobile | ||||
| Pelvic floor examination | |||||
| Perineum, Vulva | Ability to contract muscles and/or relax after contraction; able to bear down, observed as a slight bulging of the perineum | Vulva drawing in, gaping of the perineum | Presence of muscle tension or laxity at rest; inability to contract muscles and/or relax after contraction; inability to bear down |  |
|
| Bulbocavernous, ischiocavernosus, and transverse perineal muscles |  |
 |
Bilateral muscle strength, length, tone, coordination, and symmetry | Hypertonicity, tenderness (note quality of pain, e.g. burning, stinging, sharp, etc.) or tension | Modified Oxford Scaleused to assess pelvic muscle strength and endurance and assigndegree of muscle contraction around practitioner's finger159 |
| Pelvic floor (levator) muscles |  |
 |
No tension, scarring, or tenderness | Identify faciitis of levator sling, prolapse, scarring, tenderness, tension, or trigger points | Modified Oxford Scaleused to assess pelvic muscle strength and endurance and assigndegree of muscle contraction around practitioner's finger159 |
| Obturator internus muscles | |||||
| Urogenital diaphragm | No tension, non-tender | Hypertonicity, tenderness (note quality of pain, e.g. burning, stinging, sharp, etc.) or tension, and/or urinary urgency triggered by palpation |  |
||
| Rectovaginal examination | |||||
| Anus | Healthy appearing perianal skin | Patulous anus, anal fissure, anal scarring/fibrosis, external/internal hemorrhoid, excoriation, incontinent stool, perianal abscess, radiation changes to the skin such as edema (pitting/non-pitting), erythema, hypo- or hyper-pigmentation or texture (thick/thin, rough/smooth, dry) | Normal anorectal tone; anal wink reflex; grossly heme negative stool | Induration, irregularities or nodules especially along uterosacral ligaments; abnormal anorectal/resting and/or squeeze pressure, palpable lesion, anorectal stenosis, tenderness, changes to skin texture (thick/thin, rough/smooth, dry) | Anoscopy |
| Rectum | |||||
| Rectovaginal septum |  |
 |
No evidence of masses, nodules, swelling, tenderness | Presence of masses, nodules, swelling, tenderness or thickness |  |
| Abdominal examination | |||||
| Abdomen** | Presence of hernias, obesity, ostomies, scars or skin changes, radiation changes to the skin such as edema (pitting/non-pitting), erythema, hypo- or hyper-pigmentation or texture (thick/thin, rough/smooth, dry) | Soft, non-tender | Edema (pitting/non-pitting), changes to skin texture (thick/thin, rough/smooth, dry); hepatomegaly, splenomegaly, scars, tenderness, rebound, guarding; suprapubic tenderness or scarring |  |
|
| Functional breast examination | |||||
| Breast†† | Normal size and symmetry, no dimpling, flattening, masses, changes to the skin such as in color or thickening of the skin or pores. Adolescents: note Tanner stage | Presence of breast asymmetry‡‡, capsular contracture (around expander or implant), discoloration (of skin or donor flap), dry/moist desquamation, edema, erythema, fibrosis, hyperpigmentation, induration, lesions, masses, scarring(including hypertrophic or keloid scars), or telangiectasia | Appropriate fullness, non-tender | Disproportionate or asymmetrical fullness, fibrosis, hyperesthesia, induration, lesions, masses, seroma or tenderness |  |
| Nipples | Normal size and shape | Absence of native nipple***, presence of asymmetry, contraction, flattening or retraction in reconstructed nipple, any discharge, ulceration | Presence of discharge, loss of elasticity |  |
|
| Axilla | Smooth, no scarring or dimpling | Mass, scarring, cording, dimpling, radiation changes to the skin such as edema (pitting/non-pitting), erythema, hypo- or hyper-pigmentation or texture (thick/thin, rough/smooth, dry) | No palpable lymph nodes, no masses, non-tender | Palpable lymph nodes, masses, tender | |
| Lymph nodes (axillary, supraclavicular) | No visibly enlarged lymph nodes | Visibly enlarged lymph nodes, scar from axillary lymph node dissection | Non-palpable or small, mobile, non-tender lymph nodes, symmetrical | Enlarged, tender, fixed, firm lymph node(s) |  |
| Arm | Normal size and shape | Edema | Full range of motion, non-tender | Limited or decreased range of motion, tenderness, lymphedema | Lymphedema can be quantified by measuring the circumference of arm atmidpoint, cubital fossa and midforearm |
These structures may be surgically absent; the clitoris may be diminished in size and the glans may not be visible even with retraction of the clitoral hood in women on aromatase inhibitors.
Auscultation of the abdomen is also recommended to assess for normal bowel sounds.
Includes mastectomy, mastectomy with implant reconstruction, and mastectomy with autologous tissue reconstruction with or without a flap.
Darkly shaded cells indicate where an element is not applicable or specialized testing for sexual function is not needed or available.
To ensure patient safety and comfort, in general, a medical chaperone is present if requested by either the adult patient or the clinician and should be routine for examination of the adolescent.88 The patient may request that her partner be present during the physical examination; her preference should be accommodated, if possible. As a routine practice, the adolescent or adult patient is given the opportunity for private consultation with the clinician during each encounter. In addition, if the examiner and the patient do not speak the same language, a medical interpreter must be engaged to ensure patient consent, bidirectional communication and therapeutic benefit of the encounter.89,90 In some settings, with appropriate planning, medical interpretation can be provided by phone. The benefits to having an interpreter present during the physical examination, including an ad hoc interpreter such as a partner or bilingual staff member, must outweigh risks including patient discomfort and the potential for miscommunication. Referring oncologists can help streamline care by ensuring the specialist is aware in advance of translation or other communication needs.
The following examination elements are performed, always with patient consent and in a private setting. During and after the physical examination, the patient is educated about normal and abnormal findings. These findings should also be communicated back to the referring oncology care provider, with the patient’s permission.
1. Vital Signs
Physical examination of the female patient with cancer and sexuality concerns should include focused constitutional assessment and vital signs to identify risk for or presence of common chronic conditions that can affect overall health and interfere with sexual function.91 Vital signs are taken at the beginning of the medical visit and are briefly reviewed with the patient through the lens of her sexual function concerns. Because these findings sometimes trigger the need for acute medical care or care coordination by the oncology team, we briefly describe common findings and the relevance of these to care for sexual function concerns in females with cancer.
Heart Rate and Blood Pressure
Cardiovascular disease is a leading preventable cause of morbidity and premature mortality in women92 and can affect sexual function. Some chemotherapeutic regimens can cause transient or persistent elevation in blood pressure,93,94 and cardiovascular changes resulting from menopause (natural or iatrogenic) can cause chronic blood pressure elevation.95–97 Situational, or “white coat hypertension” is common in this patient population, especially when presenting for sexual concerns for the first time, and will present as mild to moderate elevation in systolic blood pressure with elevated pulse rate, typically in the range of 85–100 beats per minute.98 Repeating the pulse and blood pressure measurement after establishing rapport with the patient will often times show normalization. A higher pulse rate (>100 bpm) that persists over the course of the visit may indicate dehydration, hyperthyroidism, cardiac arrhythmia or other conditions and warrants further evaluation. Systolic blood pressure higher than 180 and/or diastolic blood pressure higher than 110 that persists during the visit should be referred for immediate treatment to prevent stroke.99 Evidence about the effect of antihypertensive medication on female sexual function is mixed.100 However, several classes of anti-hypertensive medication have been associated with vulvar lichen planus, a treatable cause of dyspareunia.101
Weight
Weight and body mass index (BMI) complement information about patient-reported nutrition and weight changes in relation to cancer or side effects of treatment. Low BMI may indicate poor overall nutrition, decreased appetite, depression, or frailty, all of which can be associated with low libido. Low or high BMI may be associated with impaired body image which is a known risk factor for sexual problems in women. Women with central obesity produce more endogenous estrogen and typically experience less vaginal dryness than thinner women.102–104
2. Mental Status
Anxiety and depression in women with cancer44,69,105–107 and the positive correlation between mental health status and sexual problems44,46,69,70,108 are well documented. Standardized mental status examination (MSE) has been previously described for the oncology and post-treatment settings.109–113 In addition to mood and other mental status information obtained by patient report and history, key elements of the MSE are elicited during physical examination to inform diagnosis and management (Table 4).
Table 4.
Key Mental Status Factors to Observe during the Physical Examination of Women with Cancer and Sexual Concerns110,112
| Mental Status Domains |
Components of Examination | Examples of mental status concerns |
|---|---|---|
| Behavior | Observable assessment of psychomotor activity, gestures, mannerisms, expression, eye contact and ability to follow commands | Slowed physical and emotional reactions; difficulty sitting still, fidgeting |
| Affect | Observable assessment of patient’s emotional state including documenting appropriateness of affect, range (broad or restricted), intensity (blunted, flat normal), fluctuations (labile or even) and quality (i.e. sad, angry, hostile, detached) | Sadness, tearfulness, hopelessness, worry or fearfulness; reluctance to view own genital anatomy with hand mirror; use of deflecting humor or honing in with worry about one specific finding while examining their genitals with a hand mirror |
| Speech | Observable assessment of patient’s speech (quantity, rate, volume/tone, fluency/rhythm and coherence) | Slowed speech with flat tone; short responses; delayed response time when answering questions or following instructions; pressured or non-stop talking, often about unrelated things, rumination, or long/tangential responses |
| Memory | Observable assessment of memory changes or complaints | Difficulty recalling information related to diagnosis, treatment, physical symptoms and other related information discussed during the examination; frequent forgetting; word finding difficulty |
| Thought Process | Observable assessment of patient thought processes by noting their coherence of thought, logic, relevance and flow of ideas | Circumstantial, incoherent, evasive or perseverative thinking |
110. Snyderman et al., 2009. American Family Physician.
112. Goldberg et al., 1992. Southern Medical Journal.
The examiner should be sensitive to behaviors that could be signs of situational or underlying anxiety or depression. Signs of anxiety during the physical examination may include: pressured or non-stop talking, often about unrelated things, which makes communication about the physical examination difficult; long/tangential responses to questions during the examination (e.g. rather than providing a number during the cotton swab test, the patient will qualitatively describe the pain in detail); using deflecting humor; or honing in with worry about one specific finding. Tearfulness during the examination, reluctance when asked if she would like to use a mirror to see her genital anatomy and unusually long response time to questions or instructions may, combined with other indicators, may indicate grief or depression.112 Memory changes are common complaints related to cancer treatment (e.g. chemotherapy) or side effects of treatment (e.g. menopause).114 Repeated uncertainty or confusion in response to questions or instructions during the examination may indicate compromised memory or other cognitive changes.
Evidence of significant mental health concerns suggests the need for further evaluation and treatment by a mental health specialist. Practitioners specializing in the care of women with cancer and sexual concerns should have a competent referral source for psychotherapy, sex and couples therapy, treatment for sexual assault and abuse, and medical management of psychiatric conditions, including suicidality.
3. External Genital Examination
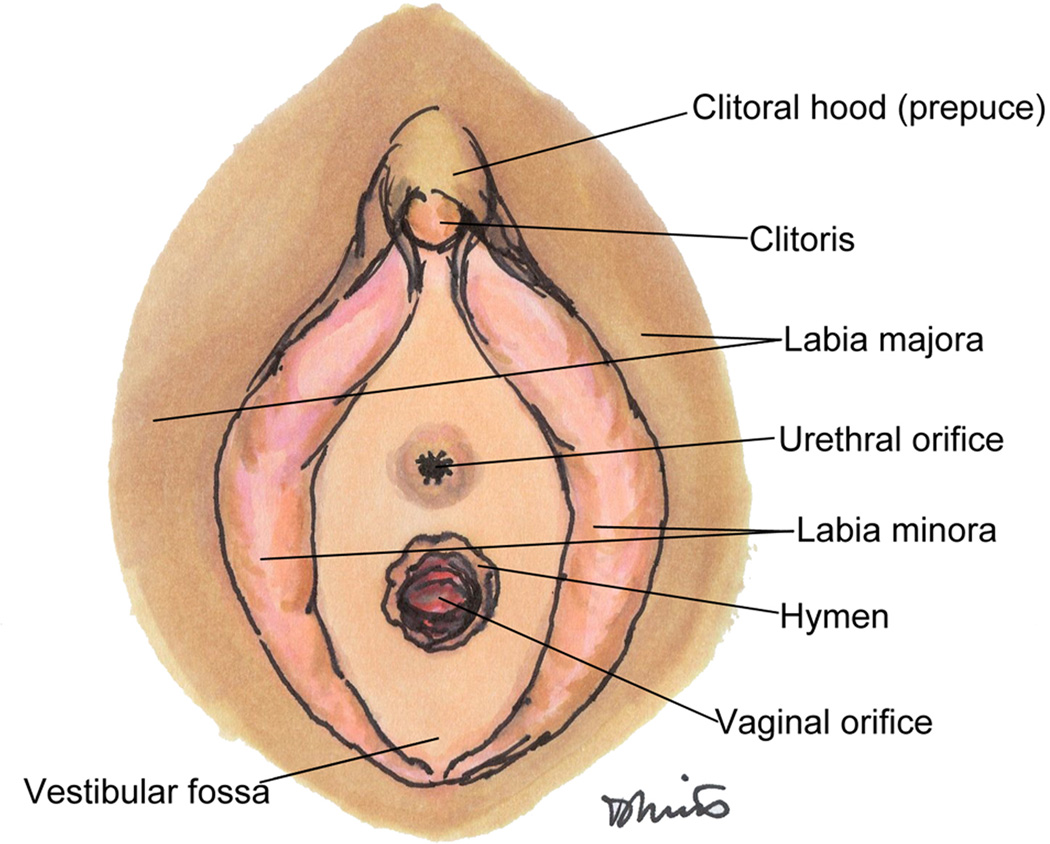
The physical examination includes, at least, the steps of comprehensive internal and external genital examination used in adult and adolescent/pediatric gynecologic practice,115–117 and therefore requires an examiner skilled in genitopelvic examination and procedures. Based on our clinical experience and supporting literature from non-cancer populations, the patient is offered a diagram of the genital anatomy115,118 (Figure 2) and positioned in a slightly upright position with a hand mirror so she can see examination findings and help locate areas of pain.119 In our experience, most patients participate and ask questions during this part of the examination.
Figure 2.
Diagram of genital anatomy to be used with the patient during physical examination
The examination begins with palpation of the inguinal lymph nodes. Close visual inspection of the external genitalia includes the mons pubis, labia majora and minora, clitoris, perineum, vestibule, vaginal introitus, urethral meatus and urethra, noting any new or atypical findings (Table 3). Bilateral oophorectomy and the gonadotoxic effects of chemotherapy and radiation can induce hypoestrogenism, a condition that can cause significant changes in the anatomy and physiology of the genitalia (including atrophy and irritation of the vulva and vagina), and in sexual physiology more generally.120–122 Vulvar edema and lymphedema are documented. Serial photography, with patient or guardian consent, can be used to track benign-appearing lesions of the vulva (such as a well-circumscribed, flat, pigmented lesion or a rash) and to help the patient better visualize vulvar findings.
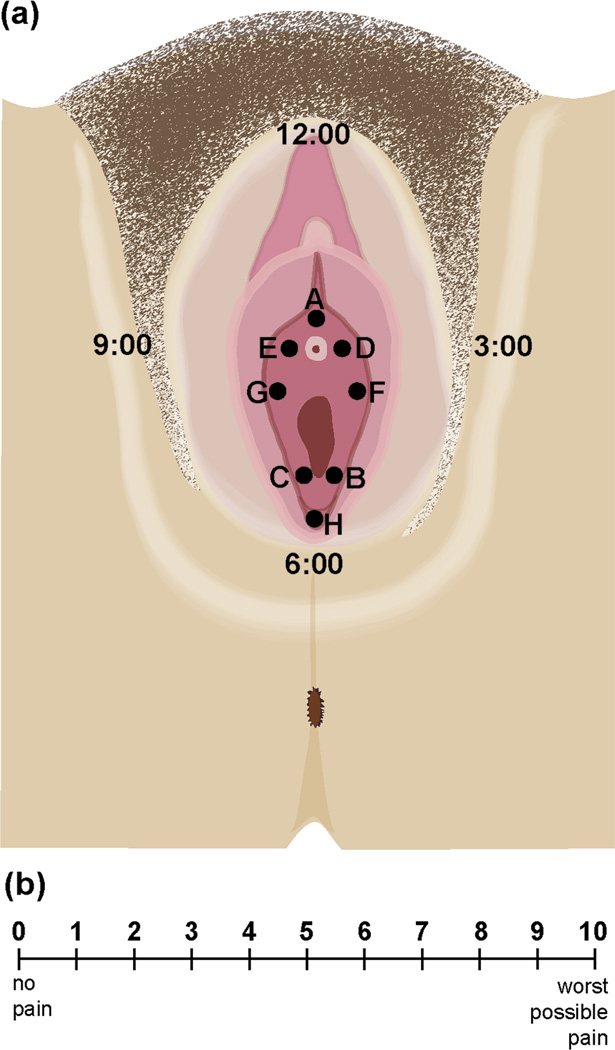
A practical protocol is needed for systematic neurologic examination of the vulvar structures to objectively evaluate genital, including clitoral, sensation.123 Vulvar pain is mapped using the cotton swab test.124 Testing starts with gentle application of a moistened standard-tip cotton swab, beginning laterally on the thighs (mainly to accustom the patient to the sensation) and moving medially to the vestibule. The cotton swab is then applied to standard points A-H on the vulva in alphabetical order (rather than in an expected, such as clockwise, order) (Figure 3a). The patient, using a 0–10 visual analog pain scale (Figure 3b)125 is instructed to describe the sensation as ranging between “zero,” meaning just touch but no pain, and “ten,” or excruciating pain. Using the visual analog scale and a standard approach on serial examinations is useful to objectively quantify, for the provider and patient, change over time126 and also facilitates research. In this patient population, common causes of vulvar pain are contact irritant dermatitis (Figure 4a) in the setting of extreme vulvar atrophy (Figure 4b),127 vestibulodynia, vulvar dystrophies and extreme pelvic floor muscle hypertonicity or vaginismus.128 If vulvar dermatoses are suspected, particularly lichen planus, the oral cavity is examined for apthous ulcers, plaques and erosions.129 A general skin examination documents rash, hives, eczema or more generalized skin conditions that may also affect the vulva. Chronic GVHD (Figure 4c) should be considered in women with a history of allogeneic bone marrow or peripheral stem cell transplantation.42,43 Physical findings in chronic GVHD are graded Minimal (Grade I)/Moderate (Grade 2)/Severe (Grade 3) and can involve vulvar, vaginal and musculoskeletal structures. The physical appearance, especially in Grade I or II cases, can mimic the appearance of vulvar dystrophies.130
Figure 3.
Vulvar Pain Mapping and Visual Analogue Scale
a. Systematic Vulvar Pain Mapping Tool to be used by the provider
b. Adapted Visual Analogue Scale to be used by the patient during assessment
Legend: Figure 3a. is for examiner reference. Figure 3b. is for patient reference during the examination. The patient is provided a laminated copy of the visual analog pain scale. She is instructed that she will feel a light touch with the cotton swab at several different points on the vulva. Each time she feels a touch with the swab, she is instructed to rate the quality of the sensation. “Zero” means touch, but no pain. “Ten” means worst possible pain. If a patient offers a fractional number such as “2.5,” the examiner records the nearest whole number (in this example, 3). Each time vulvar mapping is performed, the examiner refers to the vulvar image to ensure the vulvar sensation points are assessed and recorded in the medical record in the order A–H.
Figure 4.
Photographs of potential physical examination findings
a. Contact Dermatitis
Legend: This image shows vulvar and vestibular erythema, patchy areas of vulvar lichenification, perianal maculopapular erythematous rash, a hemorrhoid, and a flat, pigmented, regular macule of the left lateral vulva.
b. Vulvar Atrophy
Legend: This image shows vulvovaginal atrophy and vaginal introital stenosis in a patient who had completed 5 years of tamoxifen therapy and was taking an aromatase inhibitor.
c. Graft-Versus-Host Disease
Legend: This image shows a scaly, erythematous rash affecting the vulva, perineum and perianal region in a patient with probable graft-versus-host disease. For a full description of potential findings, please see Vogelsang GB, Pavletic SZ. Chronic Graft Versus Host Disease: Interdisciplinary Management. Cambridge University Press; 2009.
d. Breast Reconstruction Post-Mastectomy
Legend: This image shows a reconstructed left breast and nipple with healing scars and a lower abdominal scar resulting from breast reconstruction using the deep inferior epigastric perforator flap.
e. Breast Nipple Scar
Legend: This image shows a right mastectomy scar with absence of the right nipple areolar complex.
4. Vaginal Speculum Examination
As described in Table 3, the speculum examination is used in the adult patient (and in some cases, the adolescent) to assess for vaginal lesions, injury, discharge, atrophy or bleeding. Inspection with a speculum may be facilitated by first inserting a finger into the vagina to assess length131–133 and orientation (e.g. midline, deviated right or left/anterior or posterior). The speculum should be no larger than necessary to fully visualize the vagina; standard speculum blades vary from 2.22 cm to 3.18 cm in width, and 7.62 cm to 12.7cm in length. In most cases, a narrow well-lubricated speculum is sufficient for visualizing the vaginal canal, especially in women with stenosis and/or severe atrophy, with or without a cervix.
Women and adolescents who are sexually active with a new or non-monogamous partner are counseled (before or after the physical examination) about HIV testing134 and offered screening for sexually transmitted infections (STIs)135–137 during the physical examination. Although overall incidence of STIs138 and HIV139 is substantially lower among menopausal women, vulvovaginal atrophy, radiation changes and immune compromise increase susceptibility to infection. Disclosure of cancer history to a new partner is stigmatizing for some women and condoms can be very uncomfortable with severe vaginal dryness. Such factors present a barrier to open communication between partners about safe sex, and few women with cancer, especially women without a current partner, are counseled about STI and HIV prevention.137,140–142 Most women with cancer and sexual function concerns are menopausal and have vaginal atrophy. Candida typically does not grow in a low-estrogen environment.143 Wet prep, vaginal pH testing, and/or vaginal cytology sampling to quantify a maturation value144 are rarely needed, but may be useful modalities, to diagnose and treat sexual problems in this patient population.
5. Vaginal Manual Examination
A careful bimanual pelvic examination144,145 is performed with a single intravaginal examining finger when possible. The purpose of the pelvic examination in this clinical scenario is to assess specifically for conditions that may be contributing to the patient’s sexual function concerns. Thin adhesions due to radiation changes may be appreciated and gently separated or lysed with the examining finger. The patient should be informed (and the referring oncologist aware) that she may, as a result, experience some bleeding and pinkish or watery discharge and that these symptoms can also occur during or after sexual vaginal penetration.
Pain with deep palpation in patients who have undergone vaginal radiation and/or hysterectomy is not uncommon. Tenderness with palpation or contact to the vaginal cuff after hysterectomy, especially if granulation tissue is present, can be avoided during intercourse by sexual positioning that allows the patient to control the depth of penetration. The literature offers very limited insight to the histopathology of vaginal granulation tissue, but there is evidence that macrophages may have a role in recruiting sensory nerves.146 An infectious component could also contribute to sensitivity.147 Further work is needed to understand the variability in and treatment of deep dyspareunia in women with apical vaginal granulation tissue, but biopsy and culture could be useful modalities for evaluation. A vesicovaginal fistula should be considered with persistent granulation tissue and in cases with copious, continuous watery or serosanguinous vaginal discharge.148
A non-malodorous yellow or green vaginal discharge or exudate is common after vaginal radiation149 and/or reconstruction, as fecal pathogens can infect the vaginal tissues. Odorous or fecal-like discharge could be a sign of rectovaginal fistula, particularly in women who have had prior irradiation or pelvic surgery. Signs of STI in a woman at risk, such as cervical mucopurulent discharge and motion tenderness, should prompt culture at the time of the examination. Cervical motion tenderness is not a common radiation effect.
6. Pelvic Floor Function Examination
Many patients with cancer and sexual function concerns present initially to a physical therapist for specialized care. Some oncology care providers will be very familiar with the practice of pelvic physical therapy and have experience referring to these specialists. In other settings, including among general gynecologists, familiarity with the pelvic floor musculoskeletal examination is very limited.150 Given the high prevalence of remediable pelvic and related musculoskeletal disorders among women with dyspareunia and other types of sexual dysfunction,151–153 all specialists caring for women with cancer and sexual concerns should apply a systematic approach to pelvic floor examination that harmonizes with pelvic physical therapy practice described below.
Pelvic muscle examination begins with visual inspection of the perineum and vulva to grossly assess the range of motion of the muscles. In a lithotomy position, the patient is instructed to first contract and then bear down on the pelvic floor.154 Inability to release contraction or to effect bulge with bearing down suggest pelvic floor hypertonicity. Applying a lubricant to the examiner’s gloved index finger, the labia are separated by the thumb and forefinger and the index finger is inserted into the vaginal introitus. Initial depth of insertion is fairly shallow to assess the first layer of muscle, the urogenital triangle (bulbospongiosus, ischiocavernosus, and transverse perineal muscles), which can be assessed via gentle pincer (between the index finger and thumb) palpation. If taut bands are palpated and found to be painful, this may indicate presence of a trigger point, referring an ache to the vaginal or perineal areas. The urogenital triangle, the pelvic floor (levator muscles), obturator internus, the urogenital diaphragm, bladder and urethra should be palpated and assessed. Trigger points are discrete, focal, hyperirritable areas within a taut band of skeletal muscle.155,156 Advancing the examining finger further, the pelvic floor muscles (levator ani) are accessed and palpated for tender or trigger points. Gentle, even pressure is used for palpation of the muscles initially. If well tolerated, this maneuver is repeated with firm pressure.157 Table 3 details descriptors for inspection and palpation of the pelvic floor.
Pelvic muscle strength and endurance should be assessed by asking the patient to contract (“squeeze and lift”) the pelvic floor muscles around the examiner’s finger. A grade (zero to 5, zero being “nil” muscle contraction response and 5 being a “strong” muscle response) should be assigned according to a modified Oxford scale.158,159 Laxity is associated with low tone pelvic floor weakness and, often times, prolapse.160 High tone pelvic floor weakness is prevalent, especially among younger and nulliparous women with post-cancer dyspareunia; muscle tone will feel strong to palpation, but the patient will be unable to generate or release a contraction on command. Palpation of the coccyx and the sacrococcygeal joint can elicit tenderness that contributes to deep dyspareunia and can be addressed with physical therapy and/or sexual positioning. If the vaginal approach is not possible, due to conditions such as pain or stenosis, many of these examination elements can be assessed via a rectal approach.161,162 Decreased sensation in the vulva and or medial thigh may indicate compression or traction injuries affecting the genitofemoral, ilioinguinal and/or iliohypogastric nerves.163
Many patients, particularly those with the following common conditions, benefit from consultation and treatment by a pelvic physical therapist: untreated pelvic or related musculoskeletal injury or inflammation (e.g. arthritis); vaginismus or vaginal stenosis requiring assisted dilation;152 pelvic floor weakness requiring muscle training; pelvic floor trigger points requiring manual therapy;128 comorbid urinary or fecal incontinence requiring exercise for muscle strengthening or control;164 and chronic constipation requiring behavioral interventions and neuromuscular re-education.151,165,166 The pelvic physical therapist specializing in care of this patient population additionally performs an expanded neuromusculoskeletal examination, which typically begins by observing posture and alignment in the standing position.167 In some cases, biofeedback using external sensors may be used to assess muscle tone when digital examination is intolerable. Inspection of posture, habitual sitting and standing positions, and gait pattern provide clues to sources of pain originating outside the genital region.168 External examination includes neuromusculoskeletal, spine, pelvis and hip joints, and soft tissues (connective tissue, muscle and ligaments). Sacroiliac and hip joint dysfunction often refer pain to the pelvic muscles. Scoliosis and pelvic asymmetry such as unlevel iliac crests or leg length discrepancy may create muscle imbalances in the pelvic floor muscles that may manifest as painful, tender trigger points that contribute to dyspareunia. Thorough evaluation and examination are vital for the development, with the patient’s input, of a specific, goal-directed physical therapy treatment plan.
7. Vaginal Capacity Assessment
Well-lubricated vaginal dilators or sounds are used to objectively establish the patient’s baseline (ideally, before treatment), current and desired vaginal capacity (desired capacity may be the size of a male partner’s erect penis, the size of a preferred vibrator or dildo, or the size needed for pain-free internal genital examination) and to track change over time. Medical grade, sterilizable, graduated vaginal dilators for clinical assessment are most widely available in flexible silicone or rigid plastic, white or pink in color, with a variety of head types (e.g. flat, barrel-shaped, conical or ovoid). Although vaginal dilators are widely used in practice and new outcomes research is emerging,60,169 prospective, experimental studies to inform recommendations about the timing and technique for vaginal dilator use are limited.63 Based on our experience, for patients seeking to resume vaginal-penile intercourse, we prefer the flexible silicone model because it more closely mimics the friction and rigidity of the penis; patients are given a choice of head types for the physical examination. In one center where vaginal capacity is routinely assessed with vaginal dilators in this population, patients typically underestimated their vaginal capacity.170 Insertion (by the patient or the clinician, according to patient preference) of graded vaginal dilators, beginning with a dilator size the patient feels she can easily accommodate without pain, provides the patient and the examiner an objective measure of vaginal capacity, helps identify a suitable dilator type and size for self-dilation,171–173 and can be useful for locating pain with penetration (e.g. introital, deep).
The dilator examination also assists in detecting vaginismus. When present, a vaginismus response will typically be elicited when the dilator (or examining finger) is inserted between zero and three centimeters into the vaginal introitus. The patient will express discomfort; she and/or the examiner may feel that the dilator has “hit a wall.” This reflex can often be overcome by instructing the patient to “bear down” or to “push the dilator out of the vagina” while the dilator is being gently advanced. Some patients can learn this technique during the physical examination and effectively translate it to improved vaginal penetration for intercourse, other sexual activities and future internal genital examinations. While the use of vaginal dilators to prevent vaginal stenosis and dyspareunia, particularly after pelvic radiotherapy,174–177 is widely cited in the literature, dilator assessment as part of routine evaluation of women with cancer and sexual concerns has only been reported by one center.170
Findings from the dilator examination can be used to assist the patient in acquiring an appropriately-sized set of medical grade (typically ~$150 U.S. for a graded set of four) or direct-to-consumer (typically $50–100 U.S. for a graded set of four or $40–$55 U.S. for one) dilator devices (U.S. 2012 CPT code for vaginal dilation: 57400).178 An appropriately-sized vibrator or dildo can accomplish the same goal at significantly lower cost ($10–$25 U.S. for one device) and is a more appealing alternative for some women.
A 3-dimensional model of the internal and external genital, reproductive, musculoskeletal and neurovascular pelvic anatomy is used (e.g., the American 3B Scientific Female Pelvis, Atlanta, GA) for explaining physical examination findings to the adult, adolescent or pediatric patient following the physical examination. A printed genital diagram (Figure 2) is useful for explaining examination findings and giving instructions about hygiene techniques and/or the application of topical or intravaginal therapies.
8. Anal and Rectovaginal Examination
Inspection of the anus and perianal skin is important for identifying signs of stool incontinence (patients with diminished perineal sensation and/or chronic vaginal discharge may be unaware of symptoms), hemorrhoids, scarring and skin conditions that may contribute to dyspareunia or otherwise interfere with sexual activity (Table 3). Incontinence (or concern for incontinence) of stool and flatus can prompt a woman to avoid sex and inhibit her sexual response. A rectovaginal examination, using a single, well-lubricated examining finger, assesses: 1) anal tone, scarring and capacity for penetration; 2) constipation; 3) the posterior vaginal wall and cul-de-sac and; 4) if intact, the uterosacral ligaments. Patients with anal fibrosis or stenosis after radiation may benefit from gradual anal dilation to allow normal passage of stool and, if desired, anal intercourse. Anorectal manometry179 may be a useful modality to prevent over-dilation. Care of these patients should be in close collaboration with the colorectal surgeon and patients may benefit from pelvic physical therapy.180,181
9. Abdominal Examination
The abdomen is visually assessed for skin changes, ostomies or scars due to surgery and/or radiation therapy. These conditions can affect body image and/or can cause changes in sensation or pain that interfere with sexual function. Palpation and percussion of the abdomen should evaluate for masses (recurrent disease, hematomas, hernias or lymphocysts), tenderness and hepatosplenomegaly. Suprapubic palpation can elicit tenderness related to bladder conditions and surgical scarring. In some cases, based on expert opinion but not on published experimental evidence, physical therapy and acupuncture may be effective modalities for alleviation of pain related to abdominal wall scarring (Figure 4d). Research is needed to validate these modalities.
10. Breast Examination
Breast or chest wall examination is performed for women who present with sexual function concerns after treatment for breast cancer, breast cancer risk reduction and any breast or chest symptoms that interfere with sexual function. The primary purpose of the breast examination in this context is to document any changes to the breast and to give the patient an opportunity to describe how these changes relate to her sexual function.
Body image, appearance, and aesthetics play an important role in sexual function for many women.182–186 Research and practice focus heavily on preservation of breast cosmesis and function of the ipsilateral lymph nodes and arm.187–192 Much less is known about preservation or systematic assessment of breast function, including sensation, erectile capacity of the nipple,193 feel of the breast to the patient and her partner during intimate and sexual activity,194 range of motion of the breast and arm,195 and psychological perception of the breast as an erogenous zone.196
Although dyspareunia, decreased libido and arousal difficulties are the most common symptoms among women with breast cancer history presenting with sexual function concerns,1,197 the sexual function history and breast examination may also elicit patient report of breast symptoms interfering with sexual function.198 Common symptoms include avoidance of breast contact due to the patient’s or partner’s discomfort with the appearance of the breast,184,199,200 loss of erotic breast and/or nipple sensation,200,201 breast or chest wall pain or unpleasant hypersensitivity especially in radiated or scarred areas.199,202,203 Arm pain,204 discomfort around a chest wall port site and swelling due to lymphedema183 can also interfere. A thoracotomy incision, commonly seen in lung cancer patients, can result in decreased or lost sensation to the breast and nipple;205 women are rarely counseled to expect this change after surgery.
In the specialized female sexual function practice, examination of the breast (Table 3) following surgery with or without radiation therapy for cancer includes visual inspection and palpation of the breast, axilla and lymph nodes, with the patient in both a supine and upright position. Palpation of the reconstructed breast, especially, could reveal masses, nodularity and tenderness related to normal healing that, in the routine breast examination, would raise concern. Pain, tenderness, erythema and edema, especially in the acute recovery phase, may be due to normal healing or the result of serious complications such as infection, necrosis (fat or skin) or tumor recurrence.206 Specialized providers caring for this patient population benefit from training with a breast surgeon to learn how to interpret post-operative breast changes found in physical examination.
Patients who have undergone mastectomy with either autologous tissue reconstruction or implant reconstruction are examined for the presence or absence (Figure 4e) of the native nipple or a reconstructed (Figure 4d) or tattooed nipple. In autologous tissue reconstruction patients, common donor sites include the abdomen (Figure 4d), back, thigh and buttock; pain or scarring in these sites may also interfere with sexual function.207,208 If the donor tissue was from the abdomen, the abdominal wall is evaluated for evidence of hernia, bulge and scar-related discomfort.209–211 If the donor tissue was from the back, any evidence of seroma following latissimus flap reconstruction is noted.212
Breast examination is not necessary in the evaluation of sexual function concerns in patients who have neither breast complaints nor a history of treatment involving the breasts or thorax. Surveillance for breast disease and/or recurrent cancer occurs in the primary and/or oncology care settings according to established guidelines.53,213 In adolescents, inspection of the breasts is necessary for Tanner staging.214
Elements of the physical examination of the pediatric and adolescent girl with concerns about current or future sexual function in the context of cancer or cancer history
Oncology care for girls and adolescents with cancer includes counseling and interventions to preserve future fertility and optimize normal sexual development.215 Although age-specific guidelines for sexual education can be used to inform counseling,216 far less is known about how best to address the topic of future sexual function in the context of cancer care, especially for girls.217 We find no published evidence specific to the physical examination of this patient population in the context of specialized care for current or future sexual function concerns. This section reviews the physical examination components to expect from specialized evaluation for sexual concerns of an adolescent patient with cancer or cancer history.
For adolescents, presence of a family member, in addition to a medical chaperone,88 during the examination and subsequent discussions is at the discretion of the patient.218 A systematic external genital gynecologic examination in an adolescent should include those elements listed above for the adult patient with cancer (Table 3). Adolescents usually do not need any instrumentation of the vagina by speculum or bimanual examination. If necessary, although rarely indicated for assessment of sexual concerns in this population, examination may be done with sedation or under anesthesia.219
Adolescent cancer survivors may have normal or incomplete genital development due to pubertal failure as a result of ovarian surgery, chemotherapy or radiation treatment, or as a result of low endogenous estradiol levels due to malnutrition or chronic illness.215,220 Assessment of the breast and external genitalia is performed to determine if normal pubertal changes have occurred or if they are delayed. Inspection of the breasts and genitals using Tanner staging (Table 3) should lead to reassurance if the findings are normal or to hormonal testing and discussion of treatment options if there is incomplete maturation.218,221 Physiologic estradiol levels in girls are accompanied by findings of estrogen stimulation such as breast maturation and external genital changes such as growth and fullness of labia minora, color change of the vaginal and hymenal mucosa from a dull red to pink, and increased physiologic discharge.222 Prior to puberty, the uterus is a small tubular structure and the ovaries measure about 1 cm3.222 With maturation, ovarian stroma increases in size and ovulatory changes (follicles) can be visualized on ultrasound. Uterine growth can be monitored by the change in the uterus to fundus ratio from 1:1 to 3:1 and increase in endometrial thickness.
In a healthy adolescent who has a normal hormonal milieu, normal vaginal discharge is clear to white, odorless, and of high viscosity. The normal bacterial flora is dominated by lactobacilli, but a variety of other organisms, including some potential pathogens, are also present at lower levels. Lactobacilli convert glycogen to lactic acid. Lactic acid helps to maintain a normal acidic vaginal pH of 3.8 to 4.2. Menstrual abnormalities are common in adolescents, yet the risk of pregnancy and STIs in a sexually active teen should always be considered and, if necessary, evaluated. Preventive measures should be discussed.223 Adolescents who are amenorrheic are counseled that, if sexually active, they should use contraception to prevent unwanted pregnancy; pregnancy can occur in an amenorrheic adolescent.218
Special considerations for interpretation of and counseling about physical examination findings in female childhood cancer survivors and adolescents with cancer
Physical examination findings in adolescents seeking care for current or future sexual function concerns are interpreted with knowledge of common endocrine changes that can affect growth and sexual development.
Endocrine disorders affect up to 60% of childhood cancer survivors following chemotherapy and radiotherapy224–226 and can have implications for female sexual development and function.215,227 Cranial radiation has been associated with central precocious puberty (CPP) at lower doses (18–35 Gy) and higher doses for brain tumor treatment (>35 Gy). The mechanism of CPP following irradiation is hypothesized to involve dysregulation of cortical influences on the hypothalamus and a release of the inhibitory GABAergic tone. Risk factors associated with the development of CPP following hypothalamic irradiation include younger age at treatment, female sex, and increased BMI. Standard treatment of CPP consists of injections of depot parental preparations of GnRH agonists or annual subdermal histrelin acetate implants. The goal of treatment, typically managed by an expert in endocrinology, is to minimize the effect that pubertal levels of estradiol have on advancing skeletal maturation and secondary sexual development. Little is known about the impact of this treatment on sexual function.
Hormone treatment with oral, transdermal or topical estradiol are options for young women with ovarian insufficiency and have been shown to improve current and future sexual function.228 Discussions of current or future sexual concerns, the ability to have sexual intimacy, the possibility of future fertility, the need for contraception and prevention of sexually transmitted infections should be initiated by the oncologist and can be addressed in more depth with a specialized and knowledgeable provider.54,229
CONCLUSION
As part of a referral for specialized care for sexual function concerns, oncologists and their patients should expect a thorough physical examination as an essential component of evaluation, diagnosis and treatment. This review, complemented by multidisciplinary expert opinion where the literature is sparse, describes the elements of a systematic approach to physical examination of this patient population. This information can be used by oncology care providers to help patients understand what to expect from specialized evaluation, to aid in interpretation of specialists’ findings and recommendations, and to recruit and support new professionals to fill gaps in this important, but often overlooked area of female cancer care. In addition, adoption by specialists across sites of a systematic approach to physical examination contributes to overall harmonization efforts needed to advance science in the field.59
The elements of the comprehensive physical examination of this patient population will be iterated and refined over time as new evidence is generated and as the field grows to a broader range of practice settings and patient populations. The field needs low-tech, patient-centered protocols for neurological assessment of vulvar and clitoral sensation and serial assessment of vaginal capacity over time. Additional evidence and infrastructure are needed to establish formal practice guidelines like those produced and vetted by and on behalf of professional organizations (e.g. International Consensus Recommendations for Female Sexual Dysfunction230 or American Heart Association Scientific Statement on Sexual Activity and Cardiovascular Disease231). As the Network matures from a cooperative group to an independent not-for-profit organization, and deepens its interactions with other professional societies in the field, we expect it will develop an infrastructure and consensus process for formalized practice guidelines.
The evidence is particularly sparse for clinical evaluation of sexual function and outcomes in girls and adolescents with cancer, and surprisingly little is known about how to evaluate breast sexual function.232 Research and practice expertise is also needed to better serve particularly marginalized groups, including women with cancer and sexual concerns who are older or widowed, those who identify with a sexual or gender minority group, women with physical and/or cognitive disability, and women receiving palliative or hospice care. Some women do wish to remain sexually active until the end of life; as a matter of compassion and human rights, institutional hospice care settings should ensure patient privacy and support symptom alleviation for comfortable and safe sexual activity. This review and related publications59,233 can be used by oncology care teams to advocate for humane and holistic care for their patients.
The cost to build and sustain an effective female sexual medicine program for women with cancer presents a challenge for patient access to services and limits growth of the field. We advocate special concern for females with cancer and sexual function difficulties who live in poverty or other resource-constrained conditions. A woman’s ability to function sexually, even in the context of cancer, can materially affect her ability to marry, to sustain a marriage or long-term relationship, and to maintain economic security for herself and her children.59,234,235 Many of the physical examination elements we recommend are feasible even in low-resource settings. In our experience, communication of findings from the physical examination helps the patient understand her symptoms and can itself be therapeutic, even if more expensive treatment modalities, such as sex, couples and physical therapy, are not an option. Female sexual medicine providers should learn from and cooperate with international cancer and women’s health aid organizations such as the World Health Organization Department of Reproductive Health and Research236 to broaden access to care that would prevent loss of sexual function and improve sexual outcomes in all females with cancer. We recommend that all specialists in the field contribute in some manner, through direct patient care, education of other providers and education of the public, to improving access to knowledge and care that preserves sexual function in all females with cancer.
The comprehensive physical examination, described in detail here to facilitate a systematic approach across practices, achieves both evaluative and therapeutic goals. Adoption of evidence-based, standard practice for physical examination is needed by specialists across related disciplines to improve sexual outcomes after cancer for patients of all ages and to accelerate patient-centered, multi-site collaborative research.
Acknowledgments
The co-authors gratefully acknowledge, with permission, Yasmin Gosiengfiao, MD, Division of Hematology, Oncology and Stem Cell Transplantation, Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern University Feinberg School of Medicine and Wendy Stock, MD, Department of Medicine, Section of Hematology Oncology, University of Chicago for their generous review and input to the final version of the manuscript. We also acknowledge, with permission, the following individuals for their research support: Ms. Gillian Feldmeth, Ms. Isabella Joslin, Ms. Amber Matthews, and Ms. Chenab Navalkha, all of whom are employees in the Lindau Laboratory. Their effort was supported by the Program in Integrative Sexual Medicine for Women and Girls with Cancer at the University of Chicago. We acknowledge Diane Merritt and Amber Matthews for their creation of the illustrated figures. We would also like to acknowledge Ms. Rachel Barber Jarrett for her research support while employed with the Lindau Laboratory.
Their effort was supported by grants 1K23AG032870-01A1K23 and 5P30 AG 012857 (Chicago Core on Biomeasures in Population-Based Health and Aging Research at the NORC University of Chicago Center on Demography and Economics of Aging) and the Program in Integrative Sexual Medicine for Women and Girls with Cancer (PRISM) at the University of Chicago. Dr. Haefner is on the advisory board of Merck, Co. Inc. Dr. Streicher is on the Speaker’s Bureau of Shionogi (Osphena) and Noven (Brisdelle); PRISM and the Scientific Network on Female Sexual Health and Cancer are supported by the University of Chicago Department of Obstetrics and Gynecology Lindau Laboratory and Section of Gynecology Oncology, and by philanthropic contributions to the Lindau Lab. During this study period, the Scientific Network on Female Sexual Health and Cancer was also supported by Memorial Sloan Kettering Cancer Center’s Breast Cancer Medicine Service and the Female Sexual Medicine and Women’s Health Program, and by the University of Wisconsin-Madison.
Footnotes
Disclosure Statement:
Dr. Lindau and Ms. Abramsohn report no conflicts of interest.
Dr. Haefner reports no other conflicts of interest.
Dr. Streicher reports no conflicts of interest.
The following authors report no disclosures and no conflicts of interest: Baron, Florendo, Jhingran, Kennedy, Krane, Kushner, McComb, Merritt, Park, Siston, Straub.
All report no conflicts of interest.
Contributor Information
Stacy Tessler Lindau, Program in Integrative Sexual Medicine for Women and Girls with Cancer, Department of Obstetrics and Gynecology; Department of Medicine-Geriatrics; MacLean Center on Clinical Medical Ethics; Comprehensive Cancer Center, University of Chicago, Chicago, IL.
Emily M. Abramsohn, Program in Integrative Sexual Medicine for Women and Girls with Cancer, Department of Obstetrics and Gynecology, University of Chicago, Chicago, IL.
Shirley R. Baron, Department of Psychiatry and Behavioral Sciences, Feinberg School of Medicine, Northwestern University, Chicago, IL; Program in Integrative Sexual Medicine for Women and Girls with Cancer, Department of Obstetrics and Gynecology, University of Chicago, Chicago, IL.
Judith Florendo, Florendo Physical Therapy; Program in Integrative Sexual Medicine for Women and Girls with Cancer, Department of Obstetrics and Gynecology, University of Chicago, Chicago, IL.
Hope K. Haefner, Department of Obstetrics and Gynecology, University of Michigan Health System, Ann Arbor, MI.
Anuja Jhingran, Radiation Oncology, University of Texas MD Anderson Cancer Center, Houston, TX.
Vanessa Kennedy, Gynecologic Oncology, Department of Obstetrics and Gynecology, University of California Davis Medical Center, Sacramento, CA.
Mukta K. Krane, Department of Surgery, University of Washington, Seattle, WA.
David M. Kushner, Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, University of Wisconsin School of Medicine and Public Health, Madison, WI.
Jennifer McComb, The Family Institute at Northwestern University, Evanston, IL.
Diane F. Merritt, Pediatric and Adolescent Gynecology, Department of Obstetrics and Gynecology, Washington University School of Medicine, St. Louis, MO.
Julie E. Park, Section of Plastic and Reconstructive Surgery, Department of Surgery, University of Chicago, Chicago, IL.
Amy Siston, Department of Psychiatry and Behavioral Neurosciences, University of Chicago, Chicago, IL.
Margaret Straub, Radiation Oncology, University of Wisconsin Carbone Cancer Center, University of Wisconsin, Madison, WI.
Lauren Streicher, Department of Obstetrics and Gynecology, Feinberg School of Medicine, Northwestern Memorial Hospital, Chicago, IL.
REFERENCES
- 1.Baumgart J, Nilsson K, Evers AS, Kallak TK, Poromaa IS. Sexual dysfunction in women on adjuvant endocrine therapy after breast cancer. Menopause. 2013;20:162–168. doi: 10.1097/gme.0b013e31826560da. [DOI] [PubMed] [Google Scholar]
- 2.Fobair P, Stewart SL, Chang S, D'Onofrio C, Banks PJ, Bloom JR. Body image and sexual problems in young women with breast cancer. Psychooncology. 2006;15:579–594. doi: 10.1002/pon.991. [DOI] [PubMed] [Google Scholar]
- 3.Ford JS, Kawashima T, Whitton J, et al. Psychosexual functioning among adult female survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol. 2014;32:3126–3136. doi: 10.1200/JCO.2013.54.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hill EK, Sandbo S, Abramsohn E, et al. Assessing gynecologic and breast cancer survivors' sexual health care needs. Cancer. 2011;117:2643–2651. doi: 10.1002/cncr.25832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lindau S, Gavrilova N, Andersen D. Sexual morbidity in very long term survivors of vaginal and cervical cancer: a comparison to national norms. Gynecol Oncol. 2007;106:413–418. doi: 10.1016/j.ygyno.2007.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Low C, Fullarton M, Parkinson E, et al. Issues of intimacy and sexual dysfunction following major head and neck cancer treatment. Oral Oncol. 2009;45:898–903. doi: 10.1016/j.oraloncology.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 7.Moreno KF, Khabbaz E, Gaitonde K, Meinzen-Derr J, Wilson KM, Patil YJ. Sexuality after treatment of head and neck cancer: findings based on modification of sexual adjustment questionnaire. Laryngoscope. 2012;122:1526–1531. doi: 10.1002/lary.23347. [DOI] [PubMed] [Google Scholar]
- 8.Reese JB, Shelby RA, Abernethy AP. Sexual concerns in lung cancer patients: an examination of predictors and moderating effects of age and gender. Support Care Cancer. 2011;19:161–165. doi: 10.1007/s00520-010-1000-0. [DOI] [PubMed] [Google Scholar]
- 9.Schover L, Baum G, Fuson L, Brewster A, Melhem-Bertrandt A. Sexual problems during the first 2 years of adjuvant treatment with aromatase inhibitors. J Sex Med. 2014;11:3102–3111. doi: 10.1111/jsm.12684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Syrjala KL, Kurland BF, Abrams JR, Sanders JE, Heiman JR. Sexual function changes during the 5 years after high-dose treatment and hematopoietic cell transplantation for malignancy, with case-matched controls at 5 years. Blood. 2008;111:989–996. doi: 10.1182/blood-2007-06-096594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ye S, Yang J, Cao D, et al. Quality of life and sexual function of patients following radical hysterectomy and vaginal extension. J Sex Med. 2014;11:1334–1342. doi: 10.1111/jsm.12498. [DOI] [PubMed] [Google Scholar]
- 12.Zebrack BJ, Foley S, Wittmann D, Leonard M. Sexual functioning in young adult survivors of childhood cancer. Psychooncology. 2010;19:814–822. doi: 10.1002/pon.1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.ACOG Practice Bulletin No. 89. Elective and risk-reducing salpingo-oophorectomy. Obstet Gynecol. 2008;111:231–241. doi: 10.1097/01.AOG.0000291580.39618.cb. [DOI] [PubMed] [Google Scholar]
- 14.Bober SL, Recklitis CJ, Bakan J, Garber JE, Patenaude AF. Addressing sexual dysfunction after risk-reducing salpingo-oophorectomy: effects of a brief, psychosexual intervention. J Sex Med. 2015;12:189–197. doi: 10.1111/jsm.12713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Finch A, Metcalfe KA, Chiang JK, et al. The impact of prophylactic salpingo-oophorectomy on menopausal symptoms and sexual function in women who carry a BRCA mutation. Gynecol Oncol. 2011;121:163–168. doi: 10.1016/j.ygyno.2010.12.326. [DOI] [PubMed] [Google Scholar]
- 16.Barbera L, Firch M, Adams L, Dasgupta T, Blake J. Improving care for women after gynecological cancer: the development of a sexuality clinic. Menopause. 2011;18:1327–1333. doi: 10.1097/gme.0b013e31821f598c. [DOI] [PubMed] [Google Scholar]
- 17.Cleary V, MCarthy G, Hegarty J. Development of an educational intervention focused on sexuality for women with gynecological cancer. J Psychosoc Oncol. 2012;30:535–555. doi: 10.1080/07347332.2012.703767. [DOI] [PubMed] [Google Scholar]
- 18.Gilbert E, Ussher JM, Perz J. Sexuality after gynaecological cancer: a review of the material, intrapsychic, and discursive aspects of treatment on women's sexual-wellbeing. Maturitas. 2011;70:42–57. doi: 10.1016/j.maturitas.2011.06.013. [DOI] [PubMed] [Google Scholar]
- 19.Krychman M. Sexual rehabilitation medicine in a female oncology setting. Gynecol Oncol. 2006;101:380–384. doi: 10.1016/j.ygyno.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 20.FDA approves first treatment for sexual desire disorder [press release] [Accessed: August 18, 2015]; Available here: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm458734.htm.
- 21.Salvatore S, Nappi RE, Parma M, et al. Sexual function after fractional microablative CO(2) laser in women with vulvovaginal atrophy. Climacteric. 2015;18:219–225. doi: 10.3109/13697137.2014.975197. [DOI] [PubMed] [Google Scholar]
- 22.Schover LR, Fouladi RT, Warneke CL, et al. Seeking help for erectile dysfunction after treatment for prostate cancer. Arch Sex Behav. 2004;33:443–454. doi: 10.1023/B:ASEB.0000037425.31828.06. [DOI] [PubMed] [Google Scholar]
- 23.Carter J, Stabile C, Seidel B, et al. Baseline characteristics and concerns of female cancer patients/survivors seeking treatment at a Female Sexual Medicine Program. Support Care Cancer. 2015;23:2255–2265. doi: 10.1007/s00520-014-2573-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Froeding LP, Ottosen C, Rung-Hansen H, Svane D, Mosgaard BJ, Jensen PT. Sexual functioning and vaginal changes after radical vaginal trachelectomy in early stage cervical cancer patients: a longitudinal study. J Sex Med. 2014;11:595–604. doi: 10.1111/jsm.12399. [DOI] [PubMed] [Google Scholar]
- 25.Juraskova I, Butow P, Bonner C, Robertson R, Sharpe L. Sexual adjustment following early stage cervical and endometrial cancer: prospective controlled multi-centre study. Psychooncology. 2013;22:153–159. doi: 10.1002/pon.2066. [DOI] [PubMed] [Google Scholar]
- 26.Juraskova I, Butow P, Robertson R, Sharpe L, McLeod C, Hacker N. Post-treatment sexual adjustment following cervical and endometrial cancer: a qualitative insight. Psychooncology. 2003;12:267–279. doi: 10.1002/pon.639. [DOI] [PubMed] [Google Scholar]
- 27.Lammerink EA, de Bock GH, Pras E, Reyners AK, Mourits MJ. Sexual functioning of cervical cancer survivors: a review with a female perspective. Maturitas. 2012;72:296–304. doi: 10.1016/j.maturitas.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 28.Rosenberg SM, Tamimi RM, Gelber S, et al. Treatment-related amenorrhea and sexual functioning in young breast cancer survivors. Cancer. 2014;120:2264–2271. doi: 10.1002/cncr.28738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) Program. U.S. Complete Prevalence Counts, Invasive Cancers Only, January 1, 2011. [Accessed: March 2015];1975–2011 Available from: http://seer.cancer.gov/csr/1975_2011/browse_csr.php?sectionSEL=1&pageSEL=sect_01_table.23.html#a.
- 30.National Cancer Institute Surveillance Epidemiology, and End Results (SEER) Program. 5-Year Relative Survival. 2004–2010 Available from: http://seer.cancer.gov/data.
- 31.Amsterdam A, Krychman ML. Sexual dysfunction in patients with gynecologic neoplasms: a retrospective pilot study. J Sex Med. 2006;3:646–649. doi: 10.1111/j.1743-6109.2006.00204.x. [DOI] [PubMed] [Google Scholar]
- 32.Falk SJ, Dizon DS. Sexual dysfunction in women with cancer. Fertil Steril. 2013;100:916–921. doi: 10.1016/j.fertnstert.2013.08.018. [DOI] [PubMed] [Google Scholar]
- 33.Begovic-Juhant A, Chmielewski A, Iwuagwu S, Chapman LA. Impact of body image on depression and quality of life among women with breast cancer. J Psychosoc Oncol. 2012;30:446–460. doi: 10.1080/07347332.2012.684856. [DOI] [PubMed] [Google Scholar]
- 34.Brandberg Y, Sandelin K, Erikson S, et al. Psychological reactions, quality of life, and body image after bilateral prophylactic mastectomy in women at high risk for breast cancer: a prospective 1-year follow-up study. J Clin Oncol. 2008;26:3943–3949. doi: 10.1200/JCO.2007.13.9568. [DOI] [PubMed] [Google Scholar]
- 35.den Heijer M, Seynaeve C, Timman R, et al. Body image and psychological distress after prophylactic mastectomy and breast reconstruction in genetically predisposed women: a prospective long-term follow-up study. Eur J Cancer. 2012;48:1263–1268. doi: 10.1016/j.ejca.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 36.Averyt JC, Nishimoto PW. Addressing sexual dysfunction in colorectal cancer survivorship care. J Gastrointest Oncol. 2014;5:388–394. doi: 10.3978/j.issn.2078-6891.2014.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grant M, McMullen CK, Altschuler A, et al. Gender differences in quality of life among long-term colorectal cancer survivors with ostomies. Oncol Nurs Forum. 2011;38:587–596. doi: 10.1188/11.ONF.587-596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kasparek MS, Hassan I, Cima RR, Larson DR, Gullerud RE, Wolff BG. Long-term quality of life and sexual and urinary function after abdominoperineal resection for distal rectal cancer. Dis Colon Rectum. 2012;55:147–154. doi: 10.1097/DCR.0b013e31823d2606. [DOI] [PubMed] [Google Scholar]
- 39.Milbury K, Cohen L, Jenkins R, Skibber JM, Schover LR. The association between psychosocial and medical factors with long-term sexual dysfunction after treatment for colorectal cancer. Support Care Cancer. 2013;21:793–802. doi: 10.1007/s00520-012-1582-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.O'Brien K, Roe B, Low C, Deyn L, Rogers SN. An exploration of the perceived changes in intimacy of patients' relationships following head and neck cancer. J Clin Nurs. 2012;21:2499–2508. doi: 10.1111/j.1365-2702.2012.04162.x. [DOI] [PubMed] [Google Scholar]
- 41.Monga U, Tan G, Ostermann HJ, Monga TN. Sexuality in head and neck cancer patients. Arch Phys Med Rehab. 1997;78:298–304. doi: 10.1016/s0003-9993(97)90038-1. [DOI] [PubMed] [Google Scholar]
- 42.Spinelli S, Chiodi S, Costantini S, et al. Female genital tract graft-versus-host disease following allogeneic bone marrow transplantation. Haematologica. 2003;88:1163–1168. [PubMed] [Google Scholar]
- 43.Stratton P, Turner ML, Childs R, et al. Vulvovaginal chronic graft-versus-host disease with allogeneic hematopoietic stem cell transplantation. Obstet Gynecol. 2007;110:1041–1049. doi: 10.1097/01.AOG.0000285998.75450.86. [DOI] [PubMed] [Google Scholar]
- 44.Cull A, Cowie VJ, Farquharson DIM, Livingstone JRB. Early stage cervical cancer: Psychological and sexual outcomes of treatment. Br J Cancer. 1993;68:1216–1220. doi: 10.1038/bjc.1993.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pinto AC, de Azambuja E. Improving quality of life after breast cancer: dealing with symptoms. Maturitas. 2011;70:343–348. doi: 10.1016/j.maturitas.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 46.Speer JJ, Hillenberg B, Sugrue DP, et al. Study of sexual functioning determinants in breast cancer survivors. Breast J. 2005;11:440–447. doi: 10.1111/j.1075-122X.2005.00131.x. [DOI] [PubMed] [Google Scholar]
- 47.Stavraka C, Ford A, Ghaem-Maghami S, et al. A study of symptoms described by ovarian cancer survivors. Gynecol Oncol. 2012;125:59–64. doi: 10.1016/j.ygyno.2011.12.421. [DOI] [PubMed] [Google Scholar]
- 48.Goldfarb SB, Abramsohn E, Andersen BL, et al. A national network to advance the field of cancer and female sexuality. J Sex Med. 2013;10:319–325. doi: 10.1111/jsm.12061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cochrane Community. Cochrane Reviews. [Accessed March 25]; Available from: http://community.cochrane.org/cochrane-reviews. [Google Scholar]
- 50.Research Electronic Data Capture (REDCap) [Accessed September 19, 2015]; Available from: https://redcap.uchicago.edu/surveys/?s=LX5WIQXnD2. [Google Scholar]
- 51.Balogh EP, Ganz PA, Murphy SB, Nass SJ, Ferrell BR, Stovall E. Patient-centered cancer treatment planning: improving the quality of oncology care. Summary of an Institute of Medicine workshop. Oncologist. 2011;16:1800–1805. doi: 10.1634/theoncologist.2011-0252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Flynn KE, Lindau ST, Lin L, et al. Development and Validation of a Single-Item Screener for Self-Reporting Sexual Problems in US Adults. J Gen Intern Med. 2015;30:1468–1475. doi: 10.1007/s11606-015-3333-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Breast Cancer V.3.2014. 2014BINV-16. © National Comprehensive Cancer Network, Inc. 2014. All rights reserved. [Accessed January 2, 2015]; [Google Scholar]
- 54.Sporn NJ, Smith KB, Pirl WF, Lennes IT, Hyland KA, Park ER. Sexual health communication between cancer survivors and providers: how frequently does it occur and which providers are preferred? Psychooncology. 2015;24:1167–1173. doi: 10.1002/pon.3736. [DOI] [PubMed] [Google Scholar]
- 55.Flynn KE, Lin L, Cyranowski JM, et al. Development of the NIH PROMIS (R) Sexual Function and Satisfaction measures in patients with cancer. J Sex Med. 2013;10(Suppl 1):43–52. doi: 10.1111/j.1743-6109.2012.02995.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Quirk F, Haughie S, Symonds T. The use of the sexual function questionnaire as a screening tool for women with sexual dysfunction. J Sex Med. 2005;2:469–477. doi: 10.1111/j.1743-6109.2005.00076.x. [DOI] [PubMed] [Google Scholar]
- 57.Miller K, Mehta R, Abraham J, Opneja A, Jain RK. Patterns of long-term cancer survivorship care in a National Cancer Institute-designated Comprehensive Cancer Center. Am J Clin Oncol. 2015 doi: 10.1097/COC.0000000000000217. [DOI] [PubMed] [Google Scholar]
- 58.Salz T, Oeffinger KC, McCabe MS, Layne TM, Bach PB. Survivorship care plans in research and practice. CA Cancer J Clin. 2012;62:101–117. doi: 10.3322/caac.20142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lindau ST, Abramsohn EM, Matthews AC. A manifesto on the preservation of sexual function in women and girls with cancer. Am J Obstet Gynecol. 2015;213:166–174. doi: 10.1016/j.ajog.2015.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shridhar R, Shibata D, Chan E, Thomas CR. Anal cancer: current standards in care and recent changes in practice. CA Cancer J Clin. 2015;65:139–162. doi: 10.3322/caac.21259. [DOI] [PubMed] [Google Scholar]
- 61.Bakker RM, ter Kuile MM, Vermeer WM, et al. Sexual rehabilitation after pelvic radiotherapy and vaginal dilator use: consensus using the Delphi method. Int J Gynecol Cancer. 2014;24:1499–1506. doi: 10.1097/IGC.0000000000000253. [DOI] [PubMed] [Google Scholar]
- 62.Cullen K, Fergus K, DasGupta T, et al. Toward clinical care guidelines for supporting rehabilitative vaginal dilator use with women recovering from cervical cancer. Support Care Cancer. 2013;21:1911–1917. doi: 10.1007/s00520-013-1726-6. [DOI] [PubMed] [Google Scholar]
- 63.Law E, Kelvin JF, Thom B, et al. Prospective study of vaginal dilator use adherence and efficacy following radiotherapy. Radiother Oncol. 2015;116:149–155. doi: 10.1016/j.radonc.2015.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Knowles G, Haigh R, McLean C, Phillips H. Late effects and quality of life after chemo-radiation for the treatment of anal cancer. Eur J Oncol Nurs. 2015;19:479–485. doi: 10.1016/j.ejon.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 65.Schover LR, van der Kaaij M, van Dorst E, Creutzberg C, Huyghe E, Kiserud CE. Sexual dysfunction and infertility as late effects of cancer treatment. EJC Suppl. 2014;12:41–53. doi: 10.1016/j.ejcsup.2014.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Basson R, Rees P, Wang R, Montejo AL, Incrocci L. Sexual function in chronic illness. J Sex Med. 2010;7:374–388. doi: 10.1111/j.1743-6109.2009.01621.x. [DOI] [PubMed] [Google Scholar]
- 67.Owens AF, Tepper MS, editors. Sexual Health, Volume 2: Physical Foundations. Westport, CT: Praeger Publishers; 2007. pp. 391–425. [Google Scholar]
- 68.Perez K, Gadgil M, Dizon DS. Sexual ramifications of medical illness. Clin Obstet Gynecol. 2009;52:691–701. doi: 10.1097/GRF.0b013e3181bf4b4c. [DOI] [PubMed] [Google Scholar]
- 69.Christie KM, Meyerowitz BE, Maly RC. Depression and sexual adjustment following breast cancer in low-income Hispanic and non-Hispanic white women. Psychooncology. 2010;19:1069–1077. doi: 10.1002/pon.1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ganz PA, Desmond KA, Belin TR, Meyerowitz BE, Rowland JH. Predictors of sexual health in women after a breast cancer diagnosis. J Clin Oncol. 1999;17:2371–2380. doi: 10.1200/JCO.1999.17.8.2371. [DOI] [PubMed] [Google Scholar]
- 71.Vodermaier A, Millman RD. Accuracy of the Hospital Anxiety and Depression Scale as a screening tool in cancer patients: a systematic review and meta-analysis. Support Care Cancer. 2011;19:1899–1908. doi: 10.1007/s00520-011-1251-4. [DOI] [PubMed] [Google Scholar]
- 72.Wagner LI, Schink J, Bass M, et al. Bringing PROMIS to practice: Brief and precise symptom screening in ambulatory cancer care. Cancer. 2015;121:927–934. doi: 10.1002/cncr.29104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Flynn KE, Jeffery DD, Keefe FJ, et al. Sexual functioning along the cancer continuum: focus group results from the Patient-Reported Outcomes Measurement Information System (PROMIS(R)) Psychooncology. 2011;20:378–386. doi: 10.1002/pon.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Flynn KE, Reeve BB, Lin L, Cyranowski JM, Bruner DW, Weinfurt KP. Construct validity of the PROMIS(R) sexual function and satisfaction measures in patients with cancer. Health Qual Life Outcomes. 2013;11:40. doi: 10.1186/1477-7525-11-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jeffery DD, Tzeng JP, Keefe FJ, et al. Initial report of the cancer Patient-Reported Outcomes Measurement Information System (PROMIS) sexual function committee: review of sexual function measures and domains used in oncology. Cancer. 2009;115:1142–1153. doi: 10.1002/cncr.24134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Althof SE, Rosen PC, Perelman MA, Rubio-Aurioles E. Standard operating procedures for taking a sexual history. J Sex Med. 2013;10:23–35. doi: 10.1111/j.1743-6109.2012.02823.x. [DOI] [PubMed] [Google Scholar]
- 77.Bober SL, Carter J, Falk S. Addressing female sexual function after cancer by internists and primary care providers. J Sex Med. 2013;10(Suppl 1):112–119. doi: 10.1111/jsm.12027. [DOI] [PubMed] [Google Scholar]
- 78.Kingsberg SA, Parish SJ. The Sexual Health Interview: Female. In: Mulhall JP, et al., editors. Cancer and Sexual Health. New York, NY: Springer Science+Business Media, LLC; 2011. p. 28. [Google Scholar]
- 79.Nusbaum MRHC. The proactive sexual health history. Am Fam Physician. 2002;66:1705–1712. [PubMed] [Google Scholar]
- 80.Derogatis L, Clayton A, Lewis-D'Agostino D, Wunderlich G, Fu Y. Validation of the female sexual distress scale-revised for assessing distress in women with hypoactive sexual desire disorder. J Sex Med. 2008;5:357–364. doi: 10.1111/j.1743-6109.2007.00672.x. [DOI] [PubMed] [Google Scholar]
- 81.Hatzichristou D, Rosen RC, Derogatis LR, et al. Recommendations for the clinical evaluation of men and women with sexual dysfunction. J Sex Med. 2010;7:337–348. doi: 10.1111/j.1743-6109.2009.01619.x. [DOI] [PubMed] [Google Scholar]
- 82.Lamont J. Female sexual health consensus clinical guidelines. J Obstet Gynaecol Can. 2012;34:769–775. doi: 10.1016/S1701-2163(16)35341-5. [DOI] [PubMed] [Google Scholar]
- 83.Wiegel M, Meston C, Rosen R. The female sexual function index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Marital Ther. 2005;31:1–20. doi: 10.1080/00926230590475206. [DOI] [PubMed] [Google Scholar]
- 84.Rekindled: Addressing Sexual Health Concerns After Breast Cancer Treatment. The University of Chicago Medicine 2015. [Accessed September, 2015]; Available from: http://www.uchospitals.edu/specialties/cancer/patient-stories/breast-cancer-tb.html. [Google Scholar]
- 85.Flynn KE, Reese JB, Jeffery DD, et al. Patient experiences with communication about sex during and after treatment for cancer. Psychooncology. 2012;21:594–601. doi: 10.1002/pon.1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Stead ML, Brown JM, Fallowfield L, Selby P. Lack of communication between healthcare professionals and women with ovarian cancer about sexual issues. Br J Cancer. 2003;88:666–671. doi: 10.1038/sj.bjc.6600799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zebrack B. Information and service needs for young adult cancer patients. Support Care Cancer. 2008;16:1353–1360. doi: 10.1007/s00520-008-0435-z. [DOI] [PubMed] [Google Scholar]
- 88.ACOG Committee Opinion No. 373: Sexual misconduct. Obstet Gynecol. 2007;110:441–444. doi: 10.1097/01.AOG.0000263920.00566.72. [DOI] [PubMed] [Google Scholar]
- 89.Gany FM, Gonzalez CJ, Basu G, et al. Reducing clinical errors in cancer education: interpreter training. J Cancer Educ. 2010;25:560–564. doi: 10.1007/s13187-010-0107-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Juckett G, Unger K. Appropriate use of medical interpreters. Am Fam Physician. 2014;90:476–480. [PubMed] [Google Scholar]
- 91.McVary KT. Chapter 48: Sexual Dysfunction. In: Longo ASF Dan L, Kasper Dennis L, Hauser Stephen L, Jameson J Larry, Loscalzo Joseph., editors. Harrison's Principles of Internal Medicine. Eighteenth Edition. Vol. 1. McGraw-Hill Companies, Inc.; 2012. [Google Scholar]
- 92.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics-2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Handler J. Hypertension complicating cancer chemotherapy. J Clin Hypertens. 2007;8:526–529. doi: 10.1111/j.1524-6175.2006.05147.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Monsuez JJ, Charniot JC, Vignat N, Artigou JY. Cardiac side-effects of cancer chemotherapy. Int J Cardiol. 2010;144:3–15. doi: 10.1016/j.ijcard.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 95.Burt VL, Whelton P, Roccella EJ, et al. Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutritional Examination Survey, 1988–1991. Hypertension. 1995;25 doi: 10.1161/01.hyp.25.3.305. [DOI] [PubMed] [Google Scholar]
- 96.Yanes LL, Reckelhoff JF. Postmenopausal hypertension. Am J Hypertens. 2011;24:740–749. doi: 10.1038/ajh.2011.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zanchetti A, Facchetti R, Cesana GC, Modena MG, Pirrelli A, Sega R. Menopause-related blood pressure increase and its relationship to age and body mass index: the SIMONA epidemiological study. J Hypertens. 2005;23:2269–2276. doi: 10.1097/01.hjh.0000194118.35098.43. [DOI] [PubMed] [Google Scholar]
- 98.Mancia G, Bombelli M, Seravalle G, Grassi G. Diagnosis and management of patients with white-coat and masked hypertension. Nat Review Cardiol. 2011;8:686–693. doi: 10.1038/nrcardio.2011.115. [DOI] [PubMed] [Google Scholar]
- 99.Goldstein LB, Bushnell CD, Adams RJ, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:517–584. doi: 10.1161/STR.0b013e3181fcb238. [DOI] [PubMed] [Google Scholar]
- 100.Spatz ES, Canavan ME, Desai MM, Krumholz HM, Lindau ST. Sexual activity and function among middle-aged and older men and women with hypertension. J Hypertens. 2013;31:1096–1105. doi: 10.1097/HJH.0b013e32835fdefa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Clayton R, Chaudhry S, Ali I, Cooper S, Hodgson T, Wojnarowska F. Mucosal (oral and vulval) lichen planus in women: are angiotensin-converting enzyme inhibitors protective, and beta-blockers and non-steroidal anti-inflammatory drugs associated with the condition? Clin Exp Dermatol. 2010;35:384–387. doi: 10.1111/j.1365-2230.2009.03581.x. [DOI] [PubMed] [Google Scholar]
- 102.Cauley JA, Gutai JP, Kuller LH, Ledonne D, Powell JG. The epidemiology of serum sex-hormones in postmenopausal women. Am J Epidemiol. 1989;129:1120–1131. doi: 10.1093/oxfordjournals.aje.a115234. [DOI] [PubMed] [Google Scholar]
- 103.Lukanova A, Lundin E, Zeleniuch-Jacquotte A, et al. Body mass index, circulating levels of sex-steroid hormones, IGF-I and IGF-binding protein-3: a cross-sectional study in healthy women. Eur J of Endocrinol. 2004;150:161–171. doi: 10.1530/eje.0.1500161. [DOI] [PubMed] [Google Scholar]
- 104.McTiernan A, Wu L, Chen C, et al. Relation of BMI and physical activity to sex hormones in postmenopausal women. Obesity. 2006;14:1662–1677. doi: 10.1038/oby.2006.191. [DOI] [PubMed] [Google Scholar]
- 105.Biglia N, Moggio G, Peano E, et al. Effects of surgical and adjuvant therapies for breast cancer on sexuality, cognitive functions, and body weight. J Sex Med. 2010;7:1891–1900. doi: 10.1111/j.1743-6109.2010.01725.x. [DOI] [PubMed] [Google Scholar]
- 106.Linden W, Vodermaier A, Mackenzie R, Greig D. Anxiety and depression after cancer diagnosis: prevalence rates by cancer type, gender, and age. J Affect Disord. 2012;141:343–351. doi: 10.1016/j.jad.2012.03.025. [DOI] [PubMed] [Google Scholar]
- 107.Reich M, Lesur A, Perdrizet-Chevallier C. Depression, quality of life and breast cancer: A review of the literature. Breast Cancer Res Treat. 2008;110:9–17. doi: 10.1007/s10549-007-9706-5. [DOI] [PubMed] [Google Scholar]
- 108.Park H, Yoon HG. Menopausal symptoms, sexual function, depression, and quality of life in Korean patients with breast cancer receiving chemotherapy. Support Care Cancer. 2013;21:2499–2507. doi: 10.1007/s00520-013-1815-6. [DOI] [PubMed] [Google Scholar]
- 109.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 110.Goldberg RJ, Faust D, Novack D. Integrating the cognitive mental status examination into the medical interview. South Med J. 1992;85:491–497. doi: 10.1097/00007611-199205000-00008. [DOI] [PubMed] [Google Scholar]
- 111.Murray KJ, Scott C, Zachariah B, et al. Importance of the mini-mental status examination in the treatment of patients with brain metastases: a report from the Radiation Therapy Oncology Group protocol 91-04. Int J Radiat Oncol Biol Phys. 2000;48:59–64. doi: 10.1016/s0360-3016(00)00600-3. [DOI] [PubMed] [Google Scholar]
- 112.Snyderman D, Rovner BW. Mental status examination in primary care: A review. Am Fam Physician. 2009;80:809–814. [PubMed] [Google Scholar]
- 113.Weinrich S, Sarna L. Delirium in the older person with cancer. Cancer. 1994;74:2079–2091. doi: 10.1002/1097-0142(19941001)74:7+<2079::aid-cncr2820741716>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 114.Bender CM, Sereika SM, Berga SL, et al. Cognitive impairment associated with adjuvant therapy in breast cancer. Psychooncology. 2006;15:422–430. doi: 10.1002/pon.964. [DOI] [PubMed] [Google Scholar]
- 115.ACOG Committee Opinion No. 598: Committee on Adolescent Health Care: The initial reproductive health visit. Obstet Gynecol. 2014;123:1143–1147. doi: 10.1097/01.AOG.0000446826.46833.c0. [DOI] [PubMed] [Google Scholar]
- 116.Guidelines for Women's Health Care: A Resource Manual. 4th ed. Washington, DC: American College of Obstetrics & Gynecology; 2014. [Google Scholar]
- 117.Braverman PK, Breech L, Adolescence Co. American Academy of Pediatrics. Clinical report - gynecologic examination for adolescents in the pediatric office setting. Pediatrics. 2010;126:583–590. doi: 10.1542/peds.2010-1564. [DOI] [PubMed] [Google Scholar]
- 118.Phyliss C, Leppert JFP. Primary Care for Women. 2nd edition. Philadelphia, Pennslyvania: Lippincott Williams & Wilkins; 2004. [Google Scholar]
- 119.Howard FM. Pelvic Pain: Diagnosis and Management. Philadelphia, PA: Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 120.Castelo-Branco C, Cancelo MJ, Villero J, Nohales F, Julia MD. Management of post-menopausal vaginal atrophy and atrophic vaginitis. Maturitas. 2005;52(Suppl 1):S46–S52. doi: 10.1016/j.maturitas.2005.06.014. [DOI] [PubMed] [Google Scholar]
- 121.Kort JD, Eisenberg ML, Millheiser LS, Westphal LM. Fertility issues in cancer survivorship. CA Cancer J Clin. 2014;64:118–134. doi: 10.3322/caac.21205. [DOI] [PubMed] [Google Scholar]
- 122.Van Voorhis BJ. Genitourinary symptoms in the menopausal transition. Am J Med. 2005;118:47–53. doi: 10.1016/j.amjmed.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 123.Vardi Y, Gruenwald I, Sprecher E, Gertman I, Yartnitsky D. Normative values for female genital sensation. Urology. 2000;56:1035–1040. doi: 10.1016/s0090-4295(00)00850-5. [DOI] [PubMed] [Google Scholar]
- 124.Haefner HK. Critique of new gynecologic surgical procedures: surgery for vulvar vestibulitis. Clin Obstet Gynecol. 2000;43:689–700. doi: 10.1097/00003081-200009000-00028. [DOI] [PubMed] [Google Scholar]
- 125.Jacox A, Carr DB, Payne R. Management of Cancer Pain. Rockville, MD: Agency for Health Care Policy and Research; 1994. [Google Scholar]
- 126.ACOG Committee Opinion No. 345: Vulvodynia. Obstet Gynecol. 2006;108:1049–1052. doi: 10.1097/00006250-200610000-00047. [DOI] [PubMed] [Google Scholar]
- 127.Margeson LJ. Vulvar disease pearls. Dermatol Clin. 2006;24:145–155. doi: 10.1016/j.det.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 128.Butrick CW. Pelvic floor hypertonic disorders: identification and management. Obstet Gynecol Clin North Am. 2009;36:707–722. doi: 10.1016/j.ogc.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 129.Edwards L, Lynch PJ. Genital Dermatology Atlas. Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 130.Chronic Graft Versus Host Disease Interdisciplinary Management. New York, NY: Cambrdige University Press; 2009. [Google Scholar]
- 131.Bump RC, Mattiasson A, Bo K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–17. doi: 10.1016/s0002-9378(96)70243-0. [DOI] [PubMed] [Google Scholar]
- 132.Occhino JA, Trabuco EC, Heisler CA, Klingele CJ, Gebhart JB. Changes in vaginal anatomy and sexual function after vaginal surgery. Int Urogynecol J. 2011;22:799–804. doi: 10.1007/s00192-011-1386-3. [DOI] [PubMed] [Google Scholar]
- 133.Weber AM, Walters MD, Schover LR, Mitchinson A. Vaginal anatomy and sexual function. Obstet Gynecol. 1995;86:946–949. doi: 10.1016/0029-7844(95)00291-x. [DOI] [PubMed] [Google Scholar]
- 134.ACOG Committee Opinion No 596: Committee on Gynecologic Practice: Routine human immunodeficiency virus screening. Obstet Gynecol. 2014;123:1137–1139. doi: 10.1097/01.AOG.0000446828.64137.50. [DOI] [PubMed] [Google Scholar]
- 135.ACOG Committee Opinion No. 582: Addressing health risks of noncoital sexual activity. Obstet Gynecol. 2013;122:1378–1382. doi: 10.1097/01.AOG.0000438963.23732.80. [DOI] [PubMed] [Google Scholar]
- 136.U.S. Preventive Services Task Force (USPSTF) USPSTF Recommendations for STI Screening. 2014 Feb; Available from: http://www.uspreventiveservicestaskforce.org/Page/Name/uspstf-recommendations-for-sti-screening#table-of-contents. [Google Scholar]
- 137.LeFevre ML. Screening for chlamydia and gonorrhea: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;161:902–910. doi: 10.7326/M14-1981. [DOI] [PubMed] [Google Scholar]
- 138.Department of Health and Human Services. Sexually Transmitted Disease and Surveillance 2013. Atlanta, GA: 2014. Centers for Disease Control and Prevention. [Google Scholar]
- 139.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2012. [Accessed January 8, 2015];HIV Surveillance Supplemental Report. 2014 19(3) Available from: http://www.cdc.gov/hiv/library/reports/surveillance/. Published November 2014. [Google Scholar]
- 140.Centers for Disease Control and Prevention. Morbidity and Mortality Weekly Report. [Accessed January 8, 2015];Sexually Transmitted Diseases Treatment Guidelines 2010. Available from: http://www.cdc.gov/std/treatment/2010/std-treatment-2010-rr5912.pdf.
- 141.Li J, Thompson TD, Tai E, Zhao G, Oster AM. Testing for human immunodeficiency virus among cancer survivors under age 65 in the United States. Prev Chronic Dis. 2014;11:E200. doi: 10.5888/pcd11.140274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Moyer VA. Screening for HIV: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2013;159:51–60. doi: 10.7326/0003-4819-159-1-201307020-00645. [DOI] [PubMed] [Google Scholar]
- 143.Derzko C, Elliott S, Lam W. Management of sexual dysfunction in postmenopausal breast cancer patients taking adjuvant aromatase inhibitor therapy. Curr Oncol. 2007;14(Suppl 1):S20–S40. doi: 10.3747/co.2007.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Lentz GLR, Gershenson D, Katz V. Comprehensive Gynecology. Sixth Edition. Philadelphia, PA: Elsevier Mosby; 2012. [Google Scholar]
- 145.Charney P, Boynton U, Barad DJH. The Gynecologic Examination. In: Ryden J, Blumenthal PD, editors. Practical Gynecology: A Guide for the Primary Care Physician. 2nd Edition. American College of Physicians Press; 2009. [Google Scholar]
- 146.Miyauchi A, Kanje M, Danielsen N, Dahlin LB. Role of macrophages in the stimulation and regeneration of sensory nerves by transposed granulation tissue and temporal aspects of the response. Scand J Plast Reconstr Surg Hand Surg. 1997;31:17–23. doi: 10.3109/02844319709010501. [DOI] [PubMed] [Google Scholar]
- 147.Wai CY, Nihira MA, Drewes PG, Chang JS, Siddiqui MT, Hemsell DL. Actinomyces associated with persistent vaginal granulation tissue. Infect Dis Obstet Gynecol. 2005;13:53–55. doi: 10.1080/10647440400025637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Berek & Novak's Gynecology. Fourteenth Edition. Philadelphia, PA: Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 149.American Cancer Society. Radiation therapy for endometrial cancer. [Accessed September, 2013];2013 Available from: http://www.cancer.org/cancer/endometrialcancer/detailedguide/endometrial-uterine-cancer-treating-radiation. [Google Scholar]
- 150.Gyang A, Hartman M, Lamvu G. Musculoskeletal causes of chronic pelvic pain: what a gynecologist should know. Obstet Gynecol. 2013;121:645–650. doi: 10.1097/AOG.0b013e318283ffea. [DOI] [PubMed] [Google Scholar]
- 151.Goldfinger C, Pukall CF, Gentilcore-Saulnier E, McLean L, Chamberlain S. A prospective study of pelvic floor physical therapy: pain and psychosexual outcomes in provoked vestibulodynia. J Sex Med. 2009;6:1955–1968. doi: 10.1111/j.1743-6109.2009.01304.x. [DOI] [PubMed] [Google Scholar]
- 152.Reissing ED, Armstrong HL, Allen C. Pelvic floor physical therapy for lifelong vaginismus: a retrospective chart review and interview study. J Sex Marital Ther. 2013;39:306–320. doi: 10.1080/0092623X.2012.697535. [DOI] [PubMed] [Google Scholar]
- 153.Rosenbaum TY, Owens A. The role of pelvic floor physical therapy in the treatment of pelvic and genital pain-related sexual dysfunction (CME) J Sex Med. 2008;5:513–523. doi: 10.1111/j.1743-6109.2007.00761.x. quiz 524-515. [DOI] [PubMed] [Google Scholar]
- 154.Prather H, Spitznagle TM, Dugan SA. Recognizing and treating pelvic pain and pelvic floor dysfunction. Phys Med Rehabil Clin N Am. 2007;18:477–496. doi: 10.1016/j.pmr.2007.06.004. ix. [DOI] [PubMed] [Google Scholar]
- 155.Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Phys. 2002;65:653–662. [PubMed] [Google Scholar]
- 156.Simons DG, Travell JG, Simons LS. Travell & Simons' myofascial pain and dysfunction: upper half of body. Vol. 1. Lippincott Williams & Wilkins; 1999. [Google Scholar]
- 157.Laycock J, Haslam J, editors. Therapeutic Management of Incontinence and Pelvic Pain: Pelvic Organ Disorders. London: Springer - Verlag; 2003. [Google Scholar]
- 158.Frawley HC, Galea MP, Phillips BA, Sherburn M, Bo K. Reliability of pelvic floor muscle strength assessment using different test positions and tools. Neurourol Urodyn. 2006;25:236–242. doi: 10.1002/nau.20201. [DOI] [PubMed] [Google Scholar]
- 159.Laycock J, Jerwood D. Pelvic floor muscle assessment: The PERFECT Scheme. Physiotherapy. 87:631–642. [Google Scholar]
- 160.Braekken IH, Majida M, Ellstrom Engh M, Bo K. Can pelvic floor muscle training improve sexual function in women with pelvic organ prolapse? A randomized controlled trial. J Sex Med. 2015;12:470–480. doi: 10.1111/jsm.12746. [DOI] [PubMed] [Google Scholar]
- 161.Faubion SS, Shuster LT, Bharucha AE. Recognition and management of nonrelaxing pelvic floor dysfunction. Mayo Clinic Proc. 2012;87(2):187–193. doi: 10.1016/j.mayocp.2011.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Reissing ED, Brown C, Lord MJ, Binik YM, Khalife S. Pelvic floor muscle functioning in women with vulvar vestibulitis syndrome. J Psychosom Obstet Gynaecol. 2005;26:107–113. doi: 10.1080/01443610400023106. [DOI] [PubMed] [Google Scholar]
- 163.Nelson P, Apte G, Justiz R, 3rd, Brismee JM, Dedrick G, Sizer PS., Jr Chronic female pelvic pain--part 2: differential diagnosis and management. Pain Pract. 2012;12:111–141. doi: 10.1111/j.1533-2500.2011.00492.x. [DOI] [PubMed] [Google Scholar]
- 164.Bo K. Pelvic floor muscle training in treatment of female stress urinary incontinence, pelvic organ prolapse and sexual dysfunction. World J Urol. 2012;30:437–443. doi: 10.1007/s00345-011-0779-8. [DOI] [PubMed] [Google Scholar]
- 165.Bortolami A, Vanti C, Banchelli F, Guccione AA, Pillastrini P. Relationship between female pelvic floor dysfunction and sexual dysfunction: an observational study. J Sex Med. 2015;12:1233–1241. doi: 10.1111/jsm.12882. [DOI] [PubMed] [Google Scholar]
- 166.Gentilcore-Saulnier E, McLean L, Goldfinger C, Pukall CF, Chamberlain S. Pelvic floor muscle assessment outcomes in women with and without provoked vestibulodynia and the impact of a physical therapy program. J Sex Med. 2010;7:1003–1022. doi: 10.1111/j.1743-6109.2009.01642.x. [DOI] [PubMed] [Google Scholar]
- 167.Prather H, Dugan S, Fitzgerald C, Hunt D. Review of anatomy, evaluation, and treatment of musculoskeletal pelvic floor pain in women. PM R. 2009;1:346–358. doi: 10.1016/j.pmrj.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 168.Montenegro ML, Mateus-Vasconcelos EC, Rosa ESJC, Dos Reis FJ, Nogueira AA, Poli-Neto OB. Postural changes in women with chronic pelvic pain: a case control study. BMC Musculoskelet Disord. 2009;10:82. doi: 10.1186/1471-2474-10-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Denton AS, Maher EJ. Interventions for the physical aspects of sexual dysfunction in women following pelvic radiotherapy. Cochrane Database Syst Rev. 2003;CD003750 doi: 10.1002/14651858.CD003750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Kennedy V, Abramsohn E, Asiedu L, et al. Perceived versus measured functional vaginal capacity in patients with sexual function concerns. J Clin Oncol. 2013;31 abstract 9528. [Google Scholar]
- 171.International Guidelines on Vaginal Dilation after Pelvic Radiotherapy. Oxford: International Clinical Guideline Group; 2012. [Accessed January 8, 2015]. Available from: http://www.owenmumford.com/us/wp-content/uploads/sites/3/2014/11/Dilator-Best-Practice-Guidelines.pdf. [Google Scholar]
- 172.Bonner C, Nattress K, Anderson C, et al. Chore or priority? Barriers and facilitators affecting dilator use after pelvic radiotherapy for gynaecological cancer. Support Care Cancer. 2012;20:2305–2313. doi: 10.1007/s00520-011-1337-z. [DOI] [PubMed] [Google Scholar]
- 173.Carter J, Goldfrank D, Shover LR. Simple strategies for vaginal health promotion in cancer survivors. J Sex Med. 2011;8:549–559. doi: 10.1111/j.1743-6109.2010.01988.x. [DOI] [PubMed] [Google Scholar]
- 174.Bahng AY, Dagan A, Bruner DW, Lin LL. Determination of prognostic factors for vaginal mucosal toxicity associated with intravaginal high-dose rate brachytherapy in patients with endometrial cancer. Int J Radiat Oncol Biol Phys. 2012;82:667–673. doi: 10.1016/j.ijrobp.2010.10.071. [DOI] [PubMed] [Google Scholar]
- 175.Brand AH, Do V, Stenlake A. Can an educational intervention improve compliance with vaginal dilator use in patients treated for a gynecologic malignancy? Int J Gynecol Cancer. 2012;22:897–904. doi: 10.1097/IGC.0b013e31824d7243. [DOI] [PubMed] [Google Scholar]
- 176.Cullen K, Fergus K, Dasgupta T, Fitch M, Doyle C, Adams L. From "sex toy" to intrusive imposition: a qualitative examination of women's experiences with vaginal dilator use following treatment for gynecological cancer. J Sex Med. 2012;9:1162–1173. doi: 10.1111/j.1743-6109.2011.02639.x. [DOI] [PubMed] [Google Scholar]
- 177.Miles T, Johnson N. Vaginal dilator therapy for women receiving pelvic radiotherapy. Cochrane Database Syst Rev. 2014;9:CD007291. doi: 10.1002/14651858.CD007291.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Professional Current Procedural Terminology (CPT) American Medical Association Press; 2012. [Google Scholar]
- 179.Sun WM, Rao SS. Manometric assessment of anorectal function. Gastroenterol Clin North Am. 2001;30:15–32. doi: 10.1016/s0889-8553(05)70165-5. [DOI] [PubMed] [Google Scholar]
- 180.Starr JA, Drobnis EZ, Lenger S, Parrot J, Barrier B, Foster R. Outcomes of a comprehensive nonsurgical approach to pelvic floor rehabilitation for urinary symptoms, defecatory dysfunction, and pelvic pain. Female Pelvic Med Reconstr Surg. 2013;19:260–265. doi: 10.1097/SPV.0b013e31829cbb9b. [DOI] [PubMed] [Google Scholar]
- 181.Visser WS, Te Riele WW, Boerma D, van Ramshorst B, van Westreenen HL. Pelvic floor rehabilitation to improve functional outcome after a low anterior resection: a systematic review. Ann Coloproctol. 2014;30:109–114. doi: 10.3393/ac.2014.30.3.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Al-Ghazal SK, Fallowfield L, Blamey RW. Does cosmetic outcome from treatment of primary breast cancer influence psychosocial morbidity? Eur J Surg Onc. 1999;25:571–573. doi: 10.1053/ejso.1999.0708. [DOI] [PubMed] [Google Scholar]
- 183.Boquiren VM, Esplen MJ, Wong J, Toner B, Warner E, Malik N. Sexual functioning in breast cancer survivors experiencing body image disturbance. Psychooncology. 2015 doi: 10.1002/pon.3819. [DOI] [PubMed] [Google Scholar]
- 184.Fallbjork U, Rasmussen BH, Karlsson S, Salander P. Aspects of body image after mastectomy due to breast cancer - a two-year follow-up study. Eur J Oncol Nurs. 2013;17:340–345. doi: 10.1016/j.ejon.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 185.Hartl K, Schennach R, Muller M, et al. Quality of life, anxiety, and oncological factors: a follow-up study of breast cancer patients. Psychosomatics. 2010;51:112–123. doi: 10.1176/appi.psy.51.2.112. [DOI] [PubMed] [Google Scholar]
- 186.Moreira H, Canavarro MC. A longitudinal study about the body image and psychosocial adjustment of breast cancer patients during the course of the disease. Eur J Oncol Nurs. 2010;14:263–270. doi: 10.1016/j.ejon.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 187.Bajaj AK, Kon PS, Oberg KC, Miles DA. Aesthetic outcomes in patients undergoing breast conservation therapy for the treatment of localized breast cancer. Plast Reconstr Surg. 2004;114:1442–1449. doi: 10.1097/01.prs.0000138813.64478.a7. [DOI] [PubMed] [Google Scholar]
- 188.Fingeret MC, Nipomnick S, Guindani M, Baumann D, Hanasono M, Crosby M. Body image screening for cancer patients undergoing reconstructive surgery. Psychooncology. 2014;23:898–905. doi: 10.1002/pon.3491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Komenaka IK, Winton LM, Bouton ME, et al. Women's Impression of the Expected Breast Appearance and its Association with Breast Cancer Operations. Ann Surg Oncol. 2015;22:2010–2016. doi: 10.1245/s10434-014-4233-1. [DOI] [PubMed] [Google Scholar]
- 190.McCarthy CM, Klassen AF, Cano SJ, et al. Patient satisfaction with postmastectomy breast reconstruction: a comparison of saline and silicone implants. Cancer. 2010;116:5584–5591. doi: 10.1002/cncr.25552. [DOI] [PubMed] [Google Scholar]
- 191.Semprini G, Cattin F, Vaienti L, Brizzolari M, Cedolini C, Parodi PC. Oncoplastic surgery and cancer relapses: cosmetic and oncological results in 489 patients. Breast. 2013;22:946–951. doi: 10.1016/j.breast.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 192.Warrier S, Hwang S, Koh CE, et al. Preservation or division of the intercostobrachial nerve in axillary dissection for breast cancer: meta-analysis of randomised controlled trials. Breast. 2014;23:310–316. doi: 10.1016/j.breast.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 193.Wagner JL, Fearmonti R, Hunt KK, et al. Prospective evaluation of the nipple-areola complex sparing mastectomy for risk reduction and for early-stage breast cancer. Ann Surg Oncol. 2012;19:1137–1144. doi: 10.1245/s10434-011-2099-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Sandham C, Harcourt D. Partner experiences of breast reconstruction post mastectomy. Eur J Oncol Nurs. 2007;11:66–73. doi: 10.1016/j.ejon.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 195.Sclafani LM, Baron RH. Sentinel lymph node biopsy and axillary dissection: added morbidity of the arm, shoulder and chest wall after mastectomy and reconstruction. Cancer J. 2008;14:216–222. doi: 10.1097/PPO.0b013e31817fbe5e. [DOI] [PubMed] [Google Scholar]
- 196.Djohan R, Gage E, Gatherwright J, et al. Patient satisfaction following nipple-sparing mastectomy and immediate breast reconstruction: an 8-year outcome study. Plast Reconstr Surg. 2010;125:818–829. doi: 10.1097/PRS.0b013e3181ccdaa4. [DOI] [PubMed] [Google Scholar]
- 197.Fobair P, Spiegel D. Concerns about sexuality after breast cancer. Cancer J. 2009;15:19–26. doi: 10.1097/PPO.0b013e31819587bb. [DOI] [PubMed] [Google Scholar]
- 198.Gilbert E, Ussher JM, Perz J. Sexuality after breast cancer: a review. Maturitas. 2010;66:397–407. doi: 10.1016/j.maturitas.2010.03.027. [DOI] [PubMed] [Google Scholar]
- 199.Schnur JB, Ouellette SC, Dilorenzo TA, Green S, Montgomery GH. A qualitative analysis of acute skin toxicity among breast cancer radiotherapy patients. Psychooncology. 2011;20:260–268. doi: 10.1002/pon.1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Ussher JM, Perz J, Gilbert E. Changes to sexual well-being and intimacy after breast cancer. Cancer Nurs. 2012;35:456–465. doi: 10.1097/NCC.0b013e3182395401. [DOI] [PubMed] [Google Scholar]
- 201.Wilmoth MC. The aftermath of breast cancer: an altered sexual self. Cancer Nurs. 2001;24:278–286. doi: 10.1097/00002820-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 202.Kanatas A, Lowe D, Velikova G, et al. Issues patients would like to discuss at their review consultation in breast cancer clinics--a cross-sectional survey. Tumori. 2014;100:568–579. doi: 10.1700/1660.18184. [DOI] [PubMed] [Google Scholar]
- 203.Tasmuth T, von Smitten K, Kalso E. Pain and other symptoms during the first year after radical and conservative surgery for breast cancer. Br J Cancer. 1996;74:2024–2031. doi: 10.1038/bjc.1996.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Bosompra K, Ashikaga T, O'Brien PJ, Nelson L, Skelly J. Swelling, numbness, pain, and their relationship to arm function among breast cancer survivors: a disablement process model perspective. Breast J. 2002;8:338–348. doi: 10.1046/j.1524-4741.2002.08603.x. [DOI] [PubMed] [Google Scholar]
- 205.Lindau ST, Surawska H, Paice J, Baron SR. Communication about sexuality and intimacy in couples affected by lung cancer and their clinical-care providers. Psychooncology. 2011;20:179–185. doi: 10.1002/pon.1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Karam AK. Breast cancer posttreatment surveillance: diagnosis and management of recurrent disease. Clin Obstet Gynecol. 2011;54:157–163. doi: 10.1097/GRF.0b013e318208393b. [DOI] [PubMed] [Google Scholar]
- 207.Cordeiro PG. Breast reconstruction after surgery for breast cancer. N Engl J Med. 2008;359:1590–1601. doi: 10.1056/NEJMct0802899. [DOI] [PubMed] [Google Scholar]
- 208.Craggs B, Vanmierlo B, Zeltzer A, Buyl R, Haentjens P, Hamdi M. Donor-site morbidity following harvest of the transverse myocutaneous gracilis flap for breast reconstruction. Plast Reconstr Surg. 2014;134:682e–691e. doi: 10.1097/PRS.0000000000000612. [DOI] [PubMed] [Google Scholar]
- 209.Bajaj AK, Chevray PM, Chang DW. Comparison of donor-site complications and functional outcomes in free muscle-sparing TRAM flap and free DIEP flap breast reconstruction. Plast Reconstr Surg. 2006;117:737–746. doi: 10.1097/01.prs.0000200062.97265.fb. discussion 747–750. [DOI] [PubMed] [Google Scholar]
- 210.Man LX, Selber JC, Serletti JM. Abdominal wall following free TRAM or DIEP flap reconstruction: a meta-analysis and critical review. Plast Reconstr Surg. 2009;124:752–764. doi: 10.1097/PRS.0b013e31818b7533. [DOI] [PubMed] [Google Scholar]
- 211.Wu LC, Bajaj A, Chang DW, Chevray PM. Comparison of donor-site morbidity of SIEA, DIEP, and muscle-sparing TRAM flaps for breast reconstruction. Plast Reconstr Surg. 2008;122:702–709. doi: 10.1097/PRS.0b013e3181823c15. [DOI] [PubMed] [Google Scholar]
- 212.Randolph LC, Barone J, Angelats J, Dado DV, Vandevender DK, Shoup M. Prediction of postoperative seroma after latissimus dorsi breast reconstruction. Plast Reconstr Surg. 2005;116:1287–1290. doi: 10.1097/01.prs.0000181517.20122.36. [DOI] [PubMed] [Google Scholar]
- 213.American Cancer Society. American Cancer Society Guidelines for the Early Detection of Cancer. [Accessed January 8, 2015];2014 doi: 10.3322/canjclin.52.1.8. Availble from: http://www.cancer.org/healthy/findcancerearly/cancerscreeningguidelines/american-cancer-society-guidelines-for-the-early-detection-of-cancer. [DOI] [PubMed] [Google Scholar]
- 214.Bickley L, Szilagyi P. Bates' guide to physical examiniation and history-taking. 11th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 215.ACOG Committee Opinion No. 607: Gynecologic concerns in children and adolescents with cancer. Obstet Gynecol. 2014;124:403–408. doi: 10.1097/01.AOG.0000452746.44206.18. [DOI] [PubMed] [Google Scholar]
- 216.American Academy of Pediatrics: Committee on Psychosocial Aspects of Child and Family Health and Committee on Adolescence. Sexuality education for children and adolescents. Pediatrics. 2001;108:498–502. [PubMed] [Google Scholar]
- 217.Zebrack BJ, Casillas J, Nohr L, Adams H, Zeltzer LK. Fertility issues for young adult survivors of childhood cancer. Psychooncology. 2004;13:689–699. doi: 10.1002/pon.784. [DOI] [PubMed] [Google Scholar]
- 218.Emans SJ, Laufer MR. Emans, Laufer, Goldstein's Pediatric and Adolescent Gynecology. Lippincott Williams & Wilkins; 2012. [Google Scholar]
- 219.Logsdon VK. Common problems in pediatric and adolescent gynecologic surgery. Curr Opin Obstet Gynecol. 2001;13:453–458. doi: 10.1097/00001703-200110000-00002. [DOI] [PubMed] [Google Scholar]
- 220.Bhatia S. Cancer survivorship--pediatric issues. Hematology Am Soc Hematol Educ Program. 2005:507–515. doi: 10.1182/asheducation-2005.1.507. [DOI] [PubMed] [Google Scholar]
- 221.DiVasta AD, Gordon CM. Hormone replacement therapy for the adolescent patient. Ann N Y Acad Sci. 2008;1135:204–211. doi: 10.1196/annals.1429.012. [DOI] [PubMed] [Google Scholar]
- 222.Styne D, Grumbach M. Puberty: Ontogeny, Neuroendocrinology, Physiology, and Disorders. Philadelphia, PA: Elsevier Saunders; 2011. [Google Scholar]
- 223.Kulin HE, Muller J. The biological aspects of puberty. Pediatr Rev. 1996;17:75–86. doi: 10.1542/pir.17-3-75. [DOI] [PubMed] [Google Scholar]
- 224.Brignardello E, Felicetti F, Castiglione A, et al. Endocrine health conditions in adult survivors of childhood cancer: the need for specialized adult-focused follow-up clinics. Eur J Endocrinol. 2013;168:465–472. doi: 10.1530/EJE-12-1043. [DOI] [PubMed] [Google Scholar]
- 225.de Fine Licht S, Winther JF, Gudmundsdottir T, et al. Hospital contacts for endocrine disorders in Adult Life after Childhood Cancer in Scandinavia (ALiCCS): a population-based cohort study. Lancet. 2014;383:1981–1989. doi: 10.1016/S0140-6736(13)62564-7. [DOI] [PubMed] [Google Scholar]
- 226.Patterson BC, Wasilewski-Masker K, Ryerson AB, Mertens A, Meacham L. Endocrine health problems detected in 519 patients evaluated in a pediatric cancer survivor program. J Clin Endocrinol Metab. 2012;97:810–818. doi: 10.1210/jc.2011-2104. [DOI] [PubMed] [Google Scholar]
- 227.Brougham MF, Kelnar CJ, Wallace WH. The late endocrine effects of childhood cancer treatment. Pediatr Rehabil. 2002;5:191–201. doi: 10.1080/1363849021000039407. [DOI] [PubMed] [Google Scholar]
- 228.Hershlag A, Rausch ME, Cohen M. Part 2: Ovarian failure in adolescent cancer survivors should be treated. J Pediatr Adolesc Gynecol. 2011;24:101–103. doi: 10.1016/j.jpag.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 229.Metzger ML, Meacham LR, Patterson B, et al. Female reproductive health after childhood, adolescent, and young adult cancers: guidelines for the assessment and management of female reproductive complications. J CLin Oncol. 2013;31:1239–1247. doi: 10.1200/JCO.2012.43.5511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Basson R, Berman J, Burnett A, et al. Report of the international consensus development conference on female sexual dysfunction: definitions and classifications. J Urol. 2000;163:888–893. [PubMed] [Google Scholar]
- 231.Levine GN, Steinke EE, Bakaeen FG, et al. Sexual activity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2012;125:1058–1072. doi: 10.1161/CIR.0b013e3182447787. [DOI] [PubMed] [Google Scholar]
- 232.Magarakis M, Venkat R, Dellon AL, et al. Pilot study of breast sensation after breast reconstruction: evaluating the effects of radiation therapy and perforator flap neurotization on sensory recovery. Microsurgery. 2013;33:421–431. doi: 10.1002/micr.22124. [DOI] [PubMed] [Google Scholar]
- 233.Krychman M, Millheiser LS. Sexual health issues in women with cancer. J Sex Med. 2013;10(Suppl 1):5–15. doi: 10.1111/jsm.12034. [DOI] [PubMed] [Google Scholar]
- 234.Daly M, Wilson MI. The evolutionary psychology of marriage and divorce. In: Wait L, Bachrach C, editors. The ties that bind: Perspectives on marriage and cohabitation. New York: Aldine de Gruter; 2000. pp. 91–110. [Google Scholar]
- 235.Ratner E, Foran K, Schwartz P, Minkin M. Sexuality and intimacy after gynecological cancer. Maturitas. 2010:23–26. doi: 10.1016/j.maturitas.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 236.World Health Organization. Sexual and reproductive health. [Accessed April 15, 2015]; Available from: http://www.who.int/reproductivehealth/en/.
- 237.Horejsi J. Acquired clitoral enlargement. Diagnosis and treatment. Ann N Y Acad Sci. 1997;816:369–372. doi: 10.1111/j.1749-6632.1997.tb52163.x. [DOI] [PubMed] [Google Scholar]