Abstract
Background
Evidence suggests obesity-related social stigma and impairment in work function may be the two most detrimental quality of life (QOL) factors to overall well-being among patients seeking weight loss surgery (WLS); whether the relative importance of QOL factors varies across patient sex and race/ethnicity is unclear.
Methods
We interviewed 574 patients seeking WLS at two centers. We measured patient’s health utility (preference-based well-being measure) as determined via standard gamble scenarios assessing patients’ willingness to risk death to achieve weight loss or perfect health. Multivariable models assessed associations between patients’ utility and five weight-related QOL domains stratified by gender and race: social stigma, self-esteem, physical function, public distress (weight stigma), and work life.
Results
Depending on patients’ sex and race/ethnicity, mean utilities ranged from 0.85 to 0.91, reflecting an average willingness to assume a 9–15 % risk of death to achieve their most desired health/weight state. After adjustment, African Americans (AAs) reported higher utility than Caucasians (+ 0.054, p=0.03), but utilities did not vary significantly by sex. Among Caucasian and AA men, impairment in physical functioning was the most important factor associated with diminished utility; social stigma was also a leading factor for Caucasian men. Among Caucasian women, self-esteem and work function appeared equally important. Social stigma was the leading contributor to utility among AA women; QOL factors did not appear as important among Hispanic patients.
Conclusion
AAs reported higher utilities than Caucasian patients. Individual QOL domains that drive diminished well-being varied across race/ethnicity and sex.
Keywords: Race, Quality of life, Health utility, Bariatric surgery, Obesity
Introduction
Obesity affects more than a third of U.S. adults and has far-reaching adverse consequences, [1–4] including substantial negative physical, social, and economic effects that impair quality of life (QOL) [5, 6]. While health providers tend to focus on the medical complications of obesity, evidence suggests that QOL factors may be of greater importance to patients in terms of contributing to their overall well-being and in terms of whether patients consider potentially risky weight treatments, such as bariatric surgery [7].
Unlike in many health conditions, the adverse social consequences of obesity can be extremely profound and for many patients, the social stigma associated with their obesity may be more disturbing to patients than even the physical limitations. Most studies on the QOL consequences of obesity use health status survey measures such as the Short-Form-36 (SF-36) and the Impact of Weight on QOL (IWQOL) to assign scores to the physical and psychological impairments patients report as a result of obesity; however, the scores on the different domains are not directly comparable, such that a lower score on one domain does not necessarily mean a less desirable outcome for the patient than a higher score in another domain.
Measuring health utility is an approach to assigning a quantifiable value to the health-related QOL that represents the subjective preferences of individuals [8]. This is usually accomplished using a universal metric, such as the willingness to assume a risk of dying to achieve a desired outcome, so that an individual’s willingness to assume risk reflects the level of undesirability of their current health state and the desirability of the more desired state. By using a common metric, the impact of diseases and treatment outcomes can be compared across conditions [9]. In a survey study of over 650 patients seeking bariatric surgery [10], we measured the health utility or the quantifiable value patients placed on their current weight and health. In that study, we identified the two strongest correlates of patients’ utility among the QOL domains measured by the SF-36 and IWQOL-lite were social stigma and obesity’s adverse impact on role or work functioning, suggesting that these were the two most important QOL domains that drove diminished overall well-being or how much patients devalued their current state of being (disutility). These two factors were more important than other QOL domains studied including low self-esteem, sexual dysfunction, and impaired overall mental functioning. As is true of patients seeking bariatric surgery, generally, Caucasian women comprised the majority of our study sample. Hence, whether these earlier findings reflect those of other demographics subgroups, particularly men and racial and ethnic minorities, are not clear. Health status QOL studies consistently demonstrate that Caucasian women with obesity tend to report lower QOL scores overall and in the domain of social stigma than their male or African American counterparts [6].
In this context, our current analysis extends our earlier analysis on the same study cohort by examining the QOL domains most strongly associated with overall well-being among different sex, and racial and ethnic subgroups of patients seeking bariatric surgery. A better understanding of the QOL domains most important to different subgroups of patients will help us identify QOL outcomes most relevant to evaluating the value and effectiveness of different weight treatments that incorporate patients’ values.
Methods
Study Sample, Recruitment, and Data Collection
Participants were patients enrolled in the Assessment of Bariatric Surgery Study (ABS), a longitudinal cohort study of patients seeking bariatric surgery to understand their preferences and decision-making around bariatric surgery and the long-term health and QOL outcomes associated with surgery. Recruited patients were being evaluated for bariatric surgery at two academic medical centers in Boston, one of which served a large racial minority and socially disadvantaged urban population. To be eligible, patients had to speak English, be aged 18 to 65 years, and have a valid address and phone number. Patients were excluded if they had undergone bariatric surgery or were excluded by their health providers. Of those eligible, 654 enrolled, representing a 70 % response rate. Details on recruitment and data collection have been described elsewhere and include an hour-long baseline telephone interview [10]. The study was approved by the institutional review boards at Beth Israel Deaconess Medical Center, Boston Medical Center, and University of Massachusetts. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. A trained research nurse abstracted clinical information from the medical record.
Health Utility
To quantify the value patients placed on their current weight and health, we used a modified version of the standard gamble method (gold standard approach) to assess patients’ preference or “utility” for their current weight and health, which we described previously [9, 11]. We first asked patients to consider the classic hypothetical choice of either (1) continuing in their current health and weight without any improvement or (2) taking a gamble. The gamble had two possible outcomes: (1) “perfect health” or (2) immediate death. In the traditional health utility conceptual model, perfect health or excellent health is considered the most desired health state by individuals and utilities can be viewed as a way of estimating the value of another health state (including their current health state or well-being) as a percentage of “perfect health” [8]. Because we have found in earlier work that some patients value being at a lower body weight more than being at perfect health, [12] we administered a series of additional scenarios where we substituted perfect health with achieving a pre-specified level of weight loss as the desired outcome in order to be able to anchor utilities to the patients’ most desired health state. This approach allowed us to anchor utilities on each patient’s actual most valued state rather than assuming that all patients would place the greatest value on “perfect health”. We then specified that the treatment was associated with a small risk of dying and asked patients to estimate the highest acceptable risk of death they were willing to assume to achieve each weight or health outcome; the highest risk was confirmed through an iterative process. The specified weight loss levels expressed in pounds (in order of presentation) were patients’ self-reported “ideal” weight, weight loss associated with a BMI of 25 kg/m2 (framed as their “highest healthy weight”), 20 % weight loss, and 10 % weight loss.
Based on responses to these scenarios, we calculated patients’ health/weight utility relative to their most valued state, whether it was perfect health or one of the lower weight states; the most valued state served as the reference state with an assigned utility of 1.00. For example, if a patient responds that he/she is willing to assume the highest risk of death to achieve their ideal weight, and the risk is 20 %, then his/her current health utility is calculated to be 0.80. Therefore, the valuation of a patient’s current health and weight is expressed as a function of the individual’s most valued health state.
Health Status Measure of Qualify of Life
We measured patients’ QOL via the Impact of Weight on Quality of Life-lite (IWQOL-lite), which is comprised of 31 items that capture five QOL domains specific to obesity, [13] i.e., physical function, self-esteem, sexual life, public distress, and work. The measure has excellent psychometric properties and test-retest reliability [13]. Patients were administered a series of statements that begin with “Because of my weight…” and then asked to rate whether the statements are “always true, usually true, sometimes true, rarely true, or never true.” The Public Distress subscale has been shown to have construct validity for capturing “weight stigma”; [13, 14] items ask whether respondents experience ridicule, teasing, or unwanted attention because of their weight, whether they worry about fitting into seats in public places, fitting into aisles, finding chairs that are strong enough, etc., and whether they experience discrimination. Each subscale is scored on a 0–100 scale, [6] where higher scores reflect better QOL.
Body Mass Index and Sociodemographic Factors
We calculated patients’ BMI by multiplying self-reported weight in lbs by 703 and dividing by the square of their height in inches. We also elicited patients’ sex, race, and ethnicity and determined their age based on date of birth information abstracted from the medical record.
Data Analysis
We used descriptive statistics to characterize health utility and QOL scores by patient sex and race and ethnicity. We then conducted multivariable linear modeling to examine the association between different demographic factors including sex and race ethnicity and utility. We next developed sequential multivariable models to examine the relative impact of the following on the outcome of health utility stratified by sex and then by race and ethnicity: demographic factors (age, education), BMI, overall QOL via summary of QOL scores, and individual subscale scores of each QOL domain measured by the IWQOL-lite. To determine the relative importance of each of these factors, we examined the change in model R2 with the addition each of subsequent variable relative to the previous model. The model R2 ranges up to 1.00 and can be interpreted as the proportion of the variability in outcome measured by variables in the model. Individual QOL sub-scales leading to the largest change in model R2 are deemed to be more important than other subscales that result in smaller changes in model R2.
Results
Of 654 participants in the ABS study, 574 had complete health utility and QOL data to be included in our present analysis. Table 1 characterizes our analytic sample by sex and race and ethnicity. There were only 15 African American and 19 Hispanic men in our study sample. Women and minorities were generally significantly younger and less educated, and reported lower income. Health utilities across different subgroups ranged from 0.85 to 0.91, indicating that patients were willing to accept a 9–15 % risk of mortality to achieve their most optimal weight and health state. Differences were not statistically significant across sex or race/ethnicity prior to adjustment; however, after adjustment for other demographic factors, African American patients and those with higher educational levels were significantly more likely to report higher health utilities.
Table 1.
Sample characteristics of patients seeking bariatric surgery
| Men | Overall (n=163) | Caucasian (n=118) | African American (n=15) | Hispanic (n=19) |
|---|---|---|---|---|
| Mean age (sd) | 46.1 (11.2) | 47.7 (11.1) | 43.2 (8.6) | 39.6 (11.0)* |
| Mean BMI (kg/m2) (sd) | 49.1 (9.3) | 47.9 (8.9) | 54.3 (9.8)* | 53.0 (10.5)* |
| Mean Health Utility (sd) | 0.85 (0.2) | 0.84 (0.2) | 0.87 (0.2) | 0.87 (0.2) |
| Mean Quality of Life (Total) (sd) | 57.8 (19.0) | 59.6 (18.1) | 53.6 (19.8) | 50.3 (23.2) |
| Education, % | ||||
| High school or less | 26 | 22 | 27 | 42 |
| Some college or 2-year | 30 | 28 | 53 | 26 |
| 4 year college diploma or more | 44 | 50 | 20 | 32 |
| Income, % | ||||
| $20,000 or less | 17 | 13 | 40* | 21* |
| Over $80,000 | 48 | 57 | 27* | 21* |
| Women | Overall (n=491) | Caucasian (n=315) | African American (n=100) | Hispanic (n=57) |
| Mean age (sd) | 43.3 (11.7) | 44.8 (11.7) | 42.2 (11.4) | 36.4 (9.8)* |
| Mean BMI (kg/m2) (sd) | 46.4 (7.6) | 46.0 (7.3) | 48.4 (8.8)* | 45.3 (5.6) |
| Mean Health Utility (sd) | 0.88 (0.2) | 0.87 (0.2) | 0.91 (0.2) | 0.87 (0.3) |
| Mean Quality of Life (Total) (sd) | 52.1 (20.2) | 51.1 (19.5) | 57.7 (20.5)* | 49.8 (21.3) |
| Education, % | ||||
| High school or less | 27 | 23 | 29* | 47* |
| Some college or 2-year | 39 | 37 | 49* | 33* |
| 4 year college diploma or more | 33 | 40 | 21* | 19* |
| Income, % | ||||
| $20,000 or less | 20 | 12 | 31* | 45* |
| Over $80,000 | 32 | 44 | 9* | 11* |
Weighted samples were used to account for oversampling of nonwhites during recruitment
Results in bold indicate statistically significant differences across the variable by race/ethnicity at p<0.05. We used an ANOVA and Kruskal-Wallis one-way ANOVA for continuous and categorical variables respectively to determine if the specified variable was significant across all race/ethnicity groups. If the ANOVA or Kruskal-Wallis ANOVA tests are significant, a Dunnett’s pairwise comparison or Wilcoxon pairwise comparison test was used for continuous and categorical variables respectively to see if there were significant differences between Caucasian and African American patients or between Caucasian and Hispanic patients
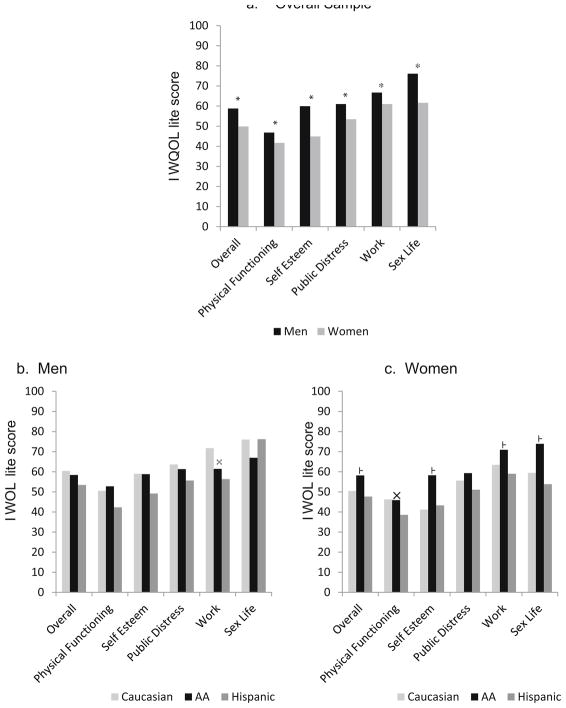
Figure 1 presents QOL scores by sex and race after adjusting for age and BMI. Men reported higher QOL scores than women overall and in all of the following domains: physical functioning, self-esteem, public distress or weight stigma, sex life, and work. Among men, QOL scores were not significantly different across race and ethnicity except that Hispanic men reported significantly lower scores on the work life sub-scale than Caucasians. Among women, African Americans reported significantly higher scores on all domains relative to Caucasians except for public distress or weight stigma; QOL scores were similar between Hispanic and Caucasian women except for physical functioning.
Fig. 1.
Quality of life scores by sex and race among patients seeking bariatric surgery after adjustment +
*P<0.05 for a Wald test difference of means by sex
P<0.05 for a Wald test difference of means by race/ethnicity African American compared to Caucasian
× P<0.05 for a Wald test difference of means by race/ethnicity Hispanic compared to Caucasian
+ Adjusted for age, BMI, race/ethnicity, and education
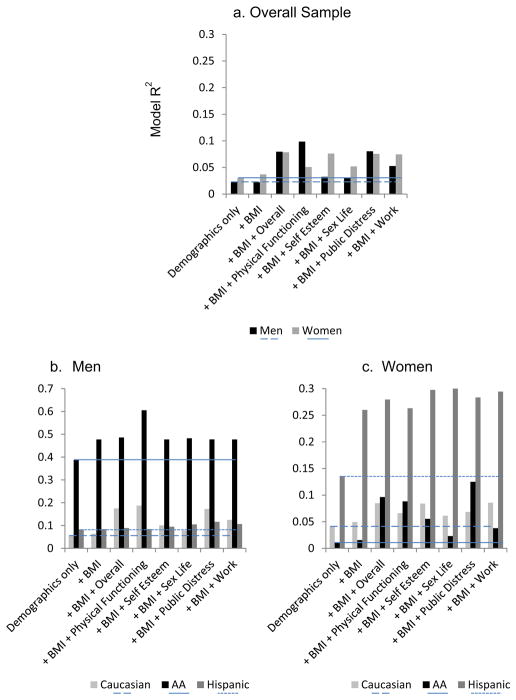
When we examined the importance of various factors associated with utility among patients seeking bariatric surgery (Fig. 2a), we found that physical functioning was the most important contributor to men’s utility, explaining an additional 8 % of the variation above the 2 % attributable to demographic factors alone; for every 10 point higher score in the physical functioning domain, utility increased by 0.03 (β=0.03± 0.008, p<0.001) (Table 2). Among men, physical functioning was followed closely by weight stigma (β=0.02±0.008, p= 0.003), which explained 6 % of the variation beyond demographic factors. Among women seeking surgery, self-esteem (β=0.02±0.004, p<0.001), weight stigma (β=0.02±0.004, p <0.0001), and work functioning (β=0.02±0.004, p<0.0001) appeared to be equal contributors to utility, each explaining an additional 4 % of the variation in disutility beyond the 3.5 % explained by demographic factors and BMI.
Fig. 2.
Marginal contribution of individual quality of life domains in explaining the variation in patient’s health utility above and beyond demographic factors and BMI by sex and race/ethnicity for patients seeking bariatric surgery+
+ Adjusted for age, BMI, race/ethnicity, and education
Table 2.
Association between demographics factors and health utility
| Demographic Factors | Health Utility |
|---|---|
| Age, decade higher | −0.002±0.0080, p=0.82 |
| BMI, per unit increase | −0.002±0.0012, p=0.11 |
| Race | Reference |
| Caucasian | |
| African American | 0.054±0.0246, p=0.03 |
| Hispanic | 0.039±0.0293, p=0.18 |
| Sex | |
| Male | −0.028±0.0211, p=0.18 |
| Female | Reference |
| Education | |
| High school or less | Reference |
| Some college or 2-year | −0.012±0.0228, p=0.59 |
| 4 year college diploma or more | 0.059±0.0232, p=0.01 |
Results are adjusted for all factors in the table. Statistically significant results are bolded
Figure 2b, c also presents that the relative contributions of different QOL domains stratified further by race and ethnicity among men and women separately (Table 3). Among men, physical functioning appeared to be very important to both Caucasians and African Americans, explaining more than 10 % and 20 % of the variation in utility, respectively, above and beyond age, education, and BMI; for every 10-point increase in physical functioning score, utilities increased by 0.040 among Caucasian men and 0.052 among the 15 African American men in our study; only the result for Caucasian men was statistically significant (Table 2). Weight stigma was also an important and significant correlate of utility among Caucasian men and explained 10 % of the marginal variation in their utility (Fig. 2 b, Table 2). Quality of life did not seem to contribute much to explaining utility among the 19 Hispanic men in our study.
Table 3.
Association between quality of life domains and health utility
| Men
|
||||
|---|---|---|---|---|
| Overall | Caucasian | AA | Hispanic | |
| Overall Score | 0.030±0.0098 | 0.046±0.0119 | 0.011±0.0274 | 0.007±0.0273 |
| p<0.01 | p<0.001 | p=0.71 | p=0.80 | |
| Physical Function | 0.030±0.0084 | 0.040±0.0099 | 0.052±0.0302 | 0.002±0.0218 |
| p<0.001 | p<0.0001 | p=0.12 | p=0.93 | |
| Self- Esteem | 0.009±0.0076 | 0.020±0.0093 | 0.000±0.0179 | −0.008±0.0207 |
| p=0.21 | p=0.04 | p=0.99 | p=0.71 | |
| Sex Life | 0.009±0.0076 | 0.013±0.0098 | −0.006±0.0195 | 0.010±0.0183 |
| p=0.26 | p=0.20 | p=0.77 | p=0.61 | |
| Public Distress | 0.023±0.0076 | 0.034±0.0091 | 0.002±0.0190 | 0.014±0.0206 |
| p<0.01 | p<0.001 | p=0.93 | p=0.52 | |
| Work Life | 0.018±0.0082 | 0.029±0.0103 | −0.000±0.0209 | 0.011±0.0206 |
| p=0.03 | p<0.01 | p=0.96 | p=0.59 | |
| Women | ||||
| Overall Score | 0.024±0.0053 | 0.024±0.0071 | 0.028±0.0101 | 0.016±0.0140 |
| p<0.0001 | p<0.001 | p<0.01 | p=0.26 | |
| Physical Function | 0.013±0.0049 | 0.015±0.0065 | 0.023±0.0088 | −0.006±0.0125 |
| p=0.01 | p=0.02 | p<0.01 | p=0.66 | |
| Self- Esteem | 0.018±0.0040 | 0.018±0.0053 | 0.015±0.0078 | 0.017±0.0102 |
| p<0.0001 | p=0.001 | p=0.06 | p=0.11 | |
| Sex Life | 0.009±0.0034 | 0.009±0.0044 | 0.006±0.0070 | 0.015±0.0086 |
| p<0.01 | p=0.06 | p=0.41 | p=0.09 | |
| Public Distress | 0.018±0.0042 | 0.014±0.0057 | 0.025±0.0074 | 0.014±0.0114 |
| p<0.0001 | p=0.02 | p=0.001 | p=0.21 | |
| Work Life | 0.018±0.0043 | 0.019±0.0056 | 0.012±0.0084 | 0.018±0.0115 |
| p<0.0001 | p<0.001 | p=0.16 | p=0.13 | |
Quality of life was measured on a scale of 0 to 100 and utility on a scale of 0 to 1. The parameter estimates represent a 10-unit increase in the quality of life domains after adjustment for age, education, and BMI on the weighted sample. There were only 15 African American men and 19 Hispanic men in the study; results pertaining to this group must be interpreted with extreme caution Statistically significant results are bolded
In contrast, among Caucasian women, self-esteem level and work life were the most important correlates of utility (Fig. 2c, Table 2), each explaining about 5 % of the marginal variation. For African American women, weight stigma explained approximately 12 % of the marginal variation (Fig. 2c); a 10-point increase in subscale score was significantly associated with a 0.014 increase in utility. Among Hispanic women, BMI alone contributed 20 % of the marginal variation in utility beyond age and education; self-esteem, sex life, and work life contributed modestly beyond age, education, and BMI.
Interestingly, scores on individual QOL domains were not a good indicator of whether the QOL domain was an important contributor to utility. For example, while self-esteem and work life were the two most important contributors to utility among Caucasian women, Caucasian women, on average, scored the highest on work life and the lowest on self-esteem subscales (Fig. 1 c).
Comment
In our study of over 570 patients seeking bariatric surgery, we found that at baseline, health utility, or the value that patients associate with their current weight and health, was significantly higher among African American relative to Caucasian patients and among those who were highly educated. In contrast, utilities did not vary significantly by sex. However, the relative importance of different domains in contributing to patients’ disutility or diminished QOL did vary depending on both patients’ sex and race. Among Caucasian and African American men, weight-related impairment in physical functioning was an important factor associated with their utility; for Caucasian men, weight stigma was also important. In contrast, among Caucasian women, self-esteem and work function were most important, whereas among African American women, weight stigma was most important. Interestingly, QOL scores were not important determinants of utility among either Hispanic men or women independent of age, sex, education, and BMI. Of note, absolute QOL scores did not necessarily indicate the relative importance of the QOL domain in explaining patient utility.
Consistent with our study’s findings, previous research suggests that women, Caucasian patients, and those seeking weight treatments tend to report lower QOL scores than their respective counterparts [6]. However, few studies have examined whether specific QOL domains play a disproportionate role in contributing to diminished overall well-being [15]. The mean health utility ranges we observed are comparable to health utilities associated with living with diabetes on the low end of the scale and mild clinical depression on the higher end of the scale estimated in other studies [16]. Understanding how patients prioritize some QOL outcomes more than others is important as weight treatments may have differential effects on different QOL domains, and the extent to which treatments are or are not successful from the patients’ perspective may depend on the treatment’s effect on specific QOL domains. In an earlier analysis, we found that physical functioning and weight stigma were the two most important QOL domains associated with patients’ utility among those seeking bariatric surgery [15]. However, whether these earlier findings reflect the perspectives of different gender and racial and ethnic subgroups were unclear. Our current analysis extends our previous work on the same cohort and demonstrates that the relative importance of different QOL factors do differ across different demographic subgroups.
Recently, we published a similar survey study of primary care patients with moderate to severe obesity [17]. In that study, we also found that the relative importance of different QOL domains varied by sex and race; however, how they varied was quite different from our present findings. Among male primary care patients, QOL appeared relatively unimportant with all domains contributing only 1 % of the variation in patients’ utility. Among women, 10 % of the marginal contribution beyond demographic factors was attributable to overall QOL scores; this was especially the case for Caucasian women. Weight stigma and sex life were leading contributors to utility among Caucasian women seen in primary care. Sex life was the leading contributor among African American women, whereas work life was the major contributor among Hispanic men and women. What is particularly striking in that study was that work life alone explained approximately 20 % of the marginal variation in disutility among Hispanic women, whereas QOL factors contributed less than 10 % of the marginal contribution among the other subgroups of patients.
The disparate findings among the various sex and racial and ethnic subgroups in our current study as compared to our primary care study [17] may provide some insight into the potential role QOL plays in understanding what might drive some patients to seek bariatric surgery [18, 19]. This hypothesis is supported by another analysis of our primary care study, [7] which demonstrated that African American primary care patients were less likely to have seriously considered surgery than Caucasian patients, but this difference largely dissipated once overall QOL scores were accounted for. Our finding that social stigma is a leading contributor to diminished utility in Caucasian men and African American women seeking bariatric surgery in our study but not in their respective primary care counterparts suggests that social stigma may be important in decisions to seek bariatric surgery among these two groups. These same two groups have traditionally been under-represented among those seeking obesity treatment and this is consistent with our finding that social stigma is not particularly salient in unselected obese Caucasian men and African American women patients in primary care; however, our present findings suggest that among those for whom social stigma does adversely affect well-being, it may be an important motivator to seek treatment. One study of obese Caucasian and African American women seeking bariatric surgery [20] found that the frequency of weight stigmatizing experiences was associated with depressed mood regardless of race. Two strategies used by Caucasian women to cope with weight stigma appear to improve depression scores including positive self-talk and self-love suggesting that these could be effective strategies to apply clinically to help reduce stigma. Unfortunately, Fettich’s study did not identify similar strategies for African American women. As with our study, Fettich’s study also had small samples of men especially ethnic and racial minorities, making it difficult to draw conclusions on these subgroups from our respective data. Future research is needed to examine the perspectives of these two populations.
In contrast, while weight stigma is important among unselected women primary care patients with obesity, obesity’s effect on self-esteem and work function may be the critical factor that motivates some Caucasian women to seek bariatric surgery. The striking difference in the role work function plays among Hispanic primary care patients relative to Hispanic patients seeking surgery may reflect the fact that we included Spanish-speaking patients in our primary care study (25 % of all Hispanic patients) but not in our current study. We speculate that Spanish-speaking patients in our primary care study may have had more limited occupational opportunities whereby their obesity may play a greater adverse impact; furthermore, these patients may face unique additional barriers that prevent them from seeking bariatric surgery, as we estimate only about 1 % of otherwise study-eligible patients were excluded in the present study based on language alone.
Our findings also have important implications on how we interpret QOL measures and on how we can deliver patient-centered, preference-based, obesity-related care more effectively. Absolute QOL scores do not necessarily predict the relative importance of specific QOL factors to patients. Moreover, our study also shows how little of the variation in a patients’ utility traditional QOL scores actually measure. This finding is not unique to the IWQOL-lite instrument. In earlier work, our group found that the widely used Short-form or SF-36 made similarly modest contributions in explaining the disutility experienced by patients with moderate to severe obesity [15].
Our results must be interpreted in the context of the study’s limitations. Given the cross-sectional nature of our current study, we cannot necessarily infer a causal link between specific QOL domains and low health utility, nor can we conclude that improvements in these domains would necessarily improve patients’ health utility; this link will need to be established when longitudinal data from ABS, which prospectively measures changes in these domains and changes in health utility as a result of weight loss, becomes available. Study subjects were recruited from bariatric surgery centers in Greater Boston; therefore, results may not generalize to patients seeking bariatric surgery elsewhere. Furthermore, we had very few African American and Hispanic men in our study sample and results pertaining to these two subgroups must be considered preliminary and interpreted with extreme caution. Finally, our results are influenced by how QOL domains were measured. One domain can appear to be more important than a second domain if the second domain is not as well-measured as the first.
In summary, the relative importance of different obesity-related QOL factors in adversely affected patients varies by sex and race among patients who are actively seeking surgical treatment to address their obesity. Scores on traditional health status measures may be misleading in that lower scores on one domain do not always translate into a greater adverse impact to patients. Whether additional measures that capture the value patients associate with their weight need to be incorporated clinically or in future research is unclear and warrants further study.
Acknowledgments
The study was funded by a grant from the National Institutes of Health (R01DK073302, PI Wee). Dr. Wee is also supported by a NIH Midcareer Mentorship Award (K24DK087932). The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Ms. Huskey had full access to the data and takes responsibility for the integrity and accuracy of the data.
Funding
The study was funded by a grant from the National Institutes of Health (R01DK073302, PI Wee). Dr. Wee is also supported by a NIH Midcareer Mentorship Award (K24DK087932).
Footnotes
Compliance with Ethical Standards
Conflict of Interest
Dr. Apovian reports grants from National Institutes of Health, from Myos, from Aspire Bariatrics, and from GI Dynamics; grants and personal fees from Amylin, from Sanofi-Aventis, from Orexigen, and from Takeda; personal fees from Merck, from Johnson & Johnson, from Arena, from Nutrisystem, from Zafgen, from EnteroMedics, and from NovoNordisk for work unrelated to the current project. All other authors declare they have no conflict of interest.
References
- 1.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 2.Calle EE, Rodriguez C, Walker-Thurmond K, et al. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348(17):1625–38. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 3.Resnick HE, Valsania P, Halter JB, et al. Differential effects of BMI on diabetes risk among black and white Americans. Diabetes Care. 1998;21(11):1828–35. doi: 10.2337/diacare.21.11.1828. [DOI] [PubMed] [Google Scholar]
- 4.Stevens J. Impact of age on associations between weight and mortality. Nutr Rev. 2000;58(5):129–37. doi: 10.1111/j.1753-4887.2000.tb01847.x. [DOI] [PubMed] [Google Scholar]
- 5.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9(12):788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 6.White MA, O’Neil PM, Kolotkin RL, et al. Gender, race, and obesity-related quality of life at extreme levels of obesity. Obes Res. 2004;12(6):949–55. doi: 10.1038/oby.2004.116. [DOI] [PubMed] [Google Scholar]
- 7.Gerland P, Masquelier B, Helleringer S, et al. Maternal mortality estimates. Lancet. 2014;384(9961):2211. doi: 10.1016/S0140-6736(14)62424-7. [DOI] [PubMed] [Google Scholar]
- 8.The medium and the message of Ebola. Lancet. 2014;384(9955):1641. doi: 10.1016/S0140-6736(14)62016-X. [DOI] [PubMed] [Google Scholar]
- 9.Shepard DS. In: Cost-effectiveness in health and medicine. Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. New York: Oxford University Press; 1996. [Google Scholar]; J Ment Health Policy Econ. 1999;2(2):91–2. [Google Scholar]
- 10.Wee CC, Hamel MB, Apovian CM, et al. Expectations for weight loss and willingness to accept risk among patients seeking weight loss surgery. JAMA Surg. 2013;148(3):264–71. doi: 10.1001/jamasurg.2013.1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wee CC, Davis RB, Huskey KW, et al. Quality of life among obese patients seeking weight loss surgery: the importance of obesity-related social stigma and functional status. J Gen Intern Med. 2013;28(2):231–8. doi: 10.1007/s11606-012-2188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wee CC, Jones DB, Davis RB, et al. Understanding patients’ value of weight loss and expectations for bariatric surgery. Obes Surg. 2006;16(4):496–500. doi: 10.1381/096089206776327260. [DOI] [PubMed] [Google Scholar]
- 13.Kolotkin RL, Crosby RD, Kosloski KD, et al. Development of a brief measure to assess quality of life in obesity. Obes Res. 2001;9(2):102–11. doi: 10.1038/oby.2001.13. [DOI] [PubMed] [Google Scholar]
- 14.Kolotkin RL, Head S, Hamilton M, et al. Assessing impact of weight on quality of life. Obes Res. 1995;3(1):49–56. doi: 10.1002/j.1550-8528.1995.tb00120.x. [DOI] [PubMed] [Google Scholar]
- 15.Wee CC, Davis RB, Huskey KW, Jones DB, Hamel MB. Quality of life among obese patients seeking weight loss surgery: the role of obesity-related social stigma and functional status. J Gen Intern Med. 2012 doi: 10.1007/s11606-012-2188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tengs TO, Wallace A. One thousand health-related quality-of-life estimates. Med Care. 2000;38(6):583–637. doi: 10.1097/00005650-200006000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Consequences of a competitive research culture. Lancet. 2014;384(9960):2084. doi: 10.1016/S0140-6736(14)62357-6. [DOI] [PubMed] [Google Scholar]
- 18.Nguyen NT, Paya M, Stevens CM, et al. The relationship between hospital volume and outcome in bariatric surgery at academic medical centers. Ann Surg. 2004;240(4):586–93. doi: 10.1097/01.sla.0000140752.74893.24. discussion 93–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Santry HP, Gillen DL, Lauderdale DS. Trends in bariatric surgical procedures. JAMA. 2005;294(15):1909–17. doi: 10.1001/jama.294.15.1909. [DOI] [PubMed] [Google Scholar]
- 20.Fettich KC, Chen EY. Coping with obesity stigma affects depressed mood in African-American and white candidates for bariatric surgery. Obesity. 2012;20(5):1118–21. doi: 10.1038/oby.2012.12. [DOI] [PMC free article] [PubMed] [Google Scholar]