Abstract
Objective
To determine if coronary artery calcium (CAC) is associated with incident non-cardiovascular disease (CVD).
Background
CAC is considered a measure of vascular aging, associated with increased risk of cardiovascular and all-cause mortality. The relationship with non-CVD is not well defined.
Methods
6,814 participants from 6 MESA (Multi-ethnic Study of Atherosclerosis) field centers, followed for a median of 10.2 years. Modified Cox proportional hazard ratios accounting for the competing risk of fatal coronary heart disease (CHD) were calculated for new diagnoses of cancer, pneumonia, chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD), deep vein thrombosis (DVT)/pulmonary embolism (PE), hip fracture and dementia. Analyses were adjusted for age, gender, race, socioeconomic status, health insurance status, body mass index, physical activity, diet, tobacco use, number of medications used, systolic and diastolic blood pressure, total and HDL-C cholesterol, antihypertensive, aspirin and cholesterol medication and diabetes. The outcome was first incident non-CVD diagnosis.
Results
Compared to those with CAC=0, those with CAC >400 had an increased hazard of cancer (1.53, 1.18-1.99), CKD (1.70, 1.21-2.39), pneumonia (1.97, 1.37-2.82), COPD (2.71, 1.60-4.57) and hip fracture (4.29, 1.47-12.50). CAC>400 was not associated with dementia or DVT/PE. Those with CAC=0 had decreased risk of cancer (0.76, 0.63-0.92), CKD (0.77, 0.60-0.98), COPD (0.61, 0.40- 0.91) and hip fracture (0.31, 0.14 - 0.70) compared to those with CAC>0. CAC=0 was not associated with less pneumonia, dementia or DVT/PE. The results were attenuated, but remained significant, after removing participants with non-fatal CHD.
Conclusion
Participants with elevated CAC were at increased risk of cancer, CKD, COPD and hip fractures. Those with CAC=0 are less likely to develop common age related comorbid conditions, and represent a unique population of “healthy agers”.
Keywords: coronary artery calcium, aging, biologic aging, coronary artery disease, cancer
Introduction
Over the last four decades, there has been a substantial decline in cardiovascular disease (CVD) mortality, partly from improved identification and modification of risk factors (1). The rate of non-CVD deaths has not declined as rapidly (2), resulting in CVD decreasing to the second leading cause of death in certain populations (3).
Coronary artery calcium (CAC) scoring is a non-invasive, direct measure of coronary atherosclerosis and powerful predictor of incident CVD and all-cause mortality (4). CAC scores increase with chronologic age (5). However, there is considerable heterogeneity within age groups (6) translating into an “equivalent” chronologic age varying up to 30 years (7). This potentially permits CAC scores to reclassify risk independent of age (8). Indeed, CAC retains a strong predictive value for all-cause mortality beyond age (9), raising the idea that CAC scores may provide a superior estimate of “arterial age” (10).
CAC scores have been associated with the presence of traditional risk factors and likely partially represent the cumulative burden of risk factor exposure. However, even those with no traditional CV risk factors can have elevated CAC scores and increased risk of CVD (11). Higher levels of CAC are also associated with an increased risk of death from non-CVD causes (12). This may be from higher incidences of other age-related diseases, like cancer, which has been associated with very high CAC scores (13). There have been mixed results when examining the relationship between CAC and other non-CVD such as kidney disease (14, 15) and decreased bone density (16, 17).
To our knowledge, there have been no studies examining the relationship between CAC and other age-related diseases associated with significant morbidity and mortality like osteoporotic fractures, pneumonia, dementia, deep vein thrombosis (DVT) or pulmonary embolism (PE). We sought to evaluate whether CAC, as a marker of arterial age, is an independent predictor of non-CVD diagnoses. We hypothesized that having CAC = 0 would be associated with a low risk of disease and having elevated CAC would be associated with a higher burden of non-CVD.
Methods
Study Population
Participants were from the Multi-Ethnic Study of Atherosclerosis (MESA) (18). MESA is a prospective, observational cohort of 6,814 people, from 6 U.S. cities, between 45 and 84 years old and of diverse backgrounds, who were free of CVD and not under active cancer treatment. Baseline, lifestyle characteristics and anthropometric measurements were measured at the initial exam. All participants with CAC scanning at baseline and follow up data were eligible for inclusion. Institutional Review Board approval was obtained at each site. Each participant gave written informed consent (http://www.mesa-nhlbi.org).
Coronary artery calcium score measurements
Detailed methods for computed tomography (CT) scan technique and interpretation were previously described (19). Chicago, Los Angeles and New York used cardiac-gated electron-beam CT scanning. The other sites used multidetector CT scanning. At the baseline exam, each participant was scanned two consecutive times with mean Agatston score used for the analysis. All images were interpreted at a single center, with good intra- and inter-reader agreement (kappa=0.92).
Follow up
Follow up occurred every 9-12 months for a median of 10.2 years (mean=9.5 years, interquartile range 9.7-10.7 years). New diagnoses were verified by review of hospital records and death certificates. Coronary heart disease (CHD) related endpoints were adjudicated and classified by two physicians from the MESA mortality and morbidity review committee. Non-CVD diagnoses were abstracted from inpatient records by ICD-9 codes. ICD-9 codes related to the following broader groups were included - chronic kidney disease (CKD) and indicators of end stage renal failure, any malignant neoplasm, dementia, hip fracture, DVT or PE, pneumonia, and COPD. A full list of codes used is in Supplementary Table 1.
Statistical Analysis
We modeled CAC as a continuous and binary variable (present/absent and zero or >400). In accordance with prior reports, CAC was analyzed as a continuous variable using base-2 logarithm of coronary calcium score plus 1 (log2 [CAC+1]) to determine how the doubling of calcium score affects risk and to include those with CAC=0(20). There were no deviations from the linear assumption when modeling continuous CAC.
Baseline characteristics are presented by CAC stratum. Continuous variables are presented as mean (standard deviation), while categorical variables as the number with the attribute (percentage of total). Analysis of variance (ANOVA) was used to test means across groups for normally distributed variables and Kruskal-Wallis for not normally distributed variables. Chi-square analysis was used to test differences in distributions for categorical variables.
The risk of each non-CVD diagnosis was analyzed individually and with a composite measure of the first occurrence of any one of the diagnoses. Raw proportions experiencing each diagnosis were calculated by CAC stratum and compared using chi square analysis. Kaplan Meier curves for non-CVD free survival were constructed. Hazard ratios (HRs) and 95% confidence intervals (CI) for non-CVD and CVD free survival were then calculated for each CAC definition with sequentially adjusted modified Cox proportional hazards regression models. To account for the competing risk of a fatal coronary heart disease (CHD) event, regression models were modified which creates informative censoring due to the strong relationship between CAC and CHD. Other non-CVD diagnoses were not considered as competing risks.
Model 1 was unadjusted. In model 2, analyses were adjusted for age, gender, race, health insurance status and socioeconomic status (SES), using education and income level. Because age varied between CAC groups, additional strategies were employed to limit residual confounding. For each outcome, sequential fractional polynomial terms for age were fit (using the flexible “fp” command in STATA), and retained throughout all outcome-specific models if their inclusion resulted in significant improvement in model variance. An age2 term was also empirically tested for each outcome, however this did not further improve model fit beyond the best fit fractional polynomial age term. Additionally, age × CAC interaction terms were tested and retained for outcomes in which they were statistically significant.
Model 3 added adjustments for body mass index (BMI), physical activity, diet and smoking status, including never, former and current use and pack years of smoking. Descriptions of physical activity and diet are included in supplementary information. Model 4 added the total number of medications used as a surrogate for burden of co-morbid illness and access to care. Model 5 added adjustments for traditional cardiovascular risk factors including systolic (SBP) and diastolic blood pressure (DBP), use of anti-hypertensive and lipid lowering medications, total and high density lipoprotein (HDL) cholesterol, use of aspirin, and presence of diabetes. Model 6 added a sensitivity analysis where participants with any non-fatal CHD event at or before the time of the non-CVD diagnosis were removed from the sample (supplementary table 2). This accounted for the potential identification bias of a co-morbid illness during an admission for CHD. Additional sensitivity analyses were performed stratifying by age category (< and ≥ 65). Statistical analysis was done using Stata 13 (College Station, TX, USA). A p value <0.05 was considered statistically significant.
Results
Baseline characteristics
Baseline characteristics are presented in Table 1. Among the 6,814 participants, 50.1% (N=3,416) had CAC =0, 39.9% (N=2,721) had CAC scores 1 - 400 and 9.9% (N=677) had CAC > 400. The mean age was 62 years with 52.9% female, 38.5% Caucasian, 27.8% African American, 22% Hispanic and 11.8% Chinese. Those with CAC = 0 were more likely to be younger, female and more physically active.
Table 1.
Baseline characteristics of participants by CAC stratum.
| All Participants (N=6814) | CAC=0 (N=3416) | CAC 1-400 (N=2721) | CAC >400 (N=677) | P-value | |
|---|---|---|---|---|---|
| Age, years | 62.15 (10.2) | 57.97 (9.1) | 65.32 (9.6) | 70.50 (7.8) | <0.001 |
| Female | 3601 (52.9%) | 2167 (63.4%) | 1232 (45.3%) | 202 (29.8%) | <0.001 |
| Race/Ethnicity | <0.001 | ||||
| Caucasian | 2622 (38.5%) | 1127 (33%) | 1144 (42.0%) | 351 (51.9%) | |
| Chinese | 803(11.8%) | 399 (11.7%) | 352 (12.9%) | 52 (7.7%) | |
| African American | 1893 (27.8%) | 1072 (31.4%) | 669 (24.6%) | 152 (22.5%) | |
| Hispanic | 1496 (22%) | 818 (24%) | 556 (20.4%) | 122 (18.0%) | |
| Socioeconomic status | |||||
| Completed High school | 5566 (82%) | 2808 (82.6%) | 2206 (81.3%) | 552 (81.7%) | 0.42 |
| Income level | 3232 (49.4%) | 1723 (52.3%) | 1215 (46.6%) | 294 (45.9%) | <0.001 |
| % with no health insurance | 609 (8.97%) | 379 (11.14%) | 204 (7.51%) | 26 (3.85%) | <0.001 |
| BMI (kg/m2) | 28 (5.5) | 28 (5.7) | 28 (5.4) | 29 (5.0) | 0.49 |
| Moderate & Vigorous Physical Activity (MET-min/week) | 5749 (5896) | 6013 (5822) | 5596 (6136) | 5036 (5166) | <0.001 |
| Healthy Diet | 2824 (45.3%) | 1340 (43.2%) | 1176 (47.1%) | 308 (48.5%) | 0.004 |
| Smoking Status | <0.001 | ||||
| Never | 3418 (50.3%) | 1905 (56.0%) | 1248 (46%) | 265 (39.2%) | |
| Former | 2487 (36.6%) | 1045 (30.7%) | 1113 (41%) | 329 (48.7%) | |
| Current | 887 (13.1%) | 451 (13.3%) | 354 (13.0%) | 82 (12.1%) | |
| Pack years of smoking | 11.3 ( 20.9) | 7.94 (16.5) | 13.42 (22.58) | 19.84 (28.64) | <0.001 |
| Systolic Blood Pressure (mmHg) | 127 (21) | 122 (21) | 130 (22) | 135 (22) | <0.001 |
| Diastolic Blood Pressure (mmHg) | 72 (10) | 71 (10) | 72 (10) | 73 (10) | <0.001 |
| Total Cholesterol (mg/dL) | 194 (35.7) | 194 (35.0) | 195 (36.2) | 192 (37.3) | 0.051 |
| HDL-C (mg/dL) | 51 (14.8) | 53 (15.0) | 50 (14.4) | 49 (14.6) | <0.001 |
| Anti-hypertensive therapy | 2536 (37%) | 984 (29%) | 1161 (43%) | 391 (58%) | <0.001 |
| Lipid Lowering therapy | 1100 (16%) | 360 (11%) | 543 (20%) | 197 (29%) | <0.001 |
| Average Total Number of Medications | 3.25 (2.9) | 2.90 (2.7) | 3.43 (2.9) | 4.26 (3.2) | <0.001 |
| Presence of Diabetes | 859 (12.7%) | 318 (9.4%) | 387 (14.3%) | 154 (22.9%) | <0.001 |
| Aspirin Use | 1298 (19.9%) | 462 (14.2%) | 607 (23.1%) | 229 (35.5%) | <0.001 |
Cancer
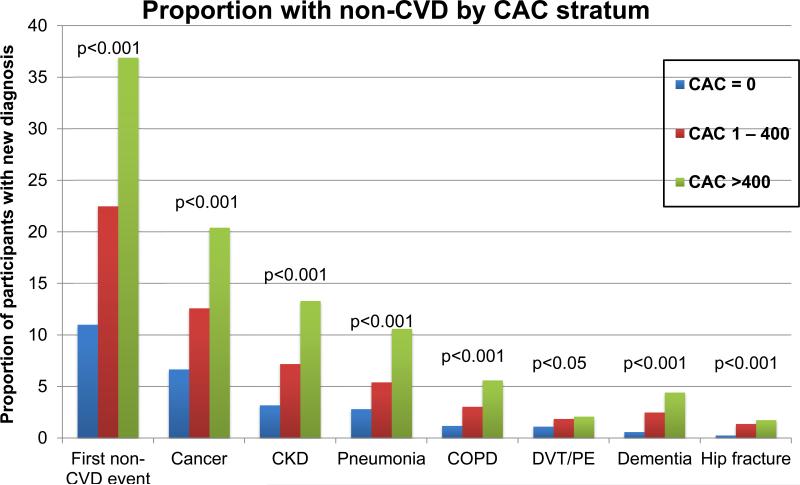
There were 710 new cancer diagnoses. The proportions of participants with cancer by CAC stratum were 6.67%, 12.6% and 20.4% for CAC=0, CAC 1 – 400 and CAC >400, respectively (p<0.001) (Figure 1). Those with CAC>0 accounted for 67.9% of cancer cases. Unadjusted and adjusted hazard ratios are in Table 2 and 3. In multivariable-adjusted models (Model 5), a doubling of CAC score was associated with a 4% increased risk of cancer (HR 1.04, 95%CI 1.02 – 1.07)(Table 2). Those with CAC >400 had a 53% greater hazard of cancer compared to those with CAC=0 (HR 1.53, 1.18-1.99)(Table 3). Those with CAC=0 had a lower hazard of being diagnosed when compared to those with CAC>0 (HR 0.76, 0.63- 0.92) (Table 4). Prostate cancer was the most common cancer diagnosed (21% of cancer cases), followed by lung cancer (14% of cancer cases), gastrointestinal/colon cancer (13% of cancer cases), breast cancer (10% of cancer cases), skin cancer (9% of cancer cases), hematologic malignancies (6% of cancer cases) and uterine/ovarian cancer (5% of cancer cases). After accounting for gender differences, there was no strong association between CAC score stratum and overall cancer type.
Figure 1.
Proportion of participants within each coronary artery calcium (CAC) score stratum with any new non-cardiovascular disease (CVD) diagnosis and by each specific diagnosis. Blue bars represent CAC scores=0, the red bars represent CAC scores of 1 – 400, and green bars represent CAC scores >400. (CKD = chronic kidney disease; COPD=chronic obstructive pulmonary disease; DVT=deep vein thrombosis; PE=pulmonary embolism)
Table 2.
Hazard of new non-cardiovascular disease (CVD) and CVD diagnosis with doubling of coronary artery calcium (CAC) score.
| Log2[CAC +1] | |||||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| Cancer | 1.13 (1.11, 1.15) | 1.05 (1.02, 1.07) | 1.04 (1.01, 1.06) | 1.03 (1.01, 1.06) | 1.04 (1.02, 1.07) |
| CKD | 1.18 (1.15, 1.20) | 1.08 (1.05, 1.12) | 1.08 (1.04, 1.11) | 1.07 (1.04, 1.10) | 1.07 (1.03, 1.10) |
| Pneumonia | 1.17 (1.13, 1.20) | 1.08 (1.04, 1.12) | 1.07 (1.03, 1.10) | 1.06 (1.02, 1.09) | 1.07 (1.03, 1.11) |
| DVT/PE | 1.10 (1.06, 1.13) | 1.04 (0.99, 1.08) | 1.01 (0.97, 1.06) | 1.01 (0.96, 1.05) | 1.03 (0.98, 1.08) |
| COPD | 1.19 (1.14, 1.24) | 1.11 (1.05, 1.16) | 1.09 (1.04, 1.15) | 1.08 (1.03, 1.14) | 1.10 (1.05, 1.16) |
| Dementia | 1.23 (1.18, 1.28) | 1.05 (1.00, 1.10) | 1.06 (1.003, 1.11) | 1.06 (1.002, 1.11) | 1.06 (1.01, 1.12) |
| Hip Fracture | 1.22 (1.14, 1.29) | 1.09 (1.003, 1.18) | 1.11 (1.02, 1.20) | 1.10 (1.01, 1.20) | 1.10 (1.01, 1.21) |
| Any non-CVD | 1.15 (1.14, 1.17) | 1.06 (1.04, 1.08) | 1.06 (1.04, 1.08) | 1.05 (1.03, 1.07) | 1.06 (1.04, 1.08) |
| CVD | 1.26 (1.23, 1.28) | 1.20 (1.17, 1.23) | 1.19 (1.16, 1.22) | 1.19 (1.16, 1.22) | 1.17 (1.14, 1.20) |
Cox proportional hazard ratios and 95% confidence intervals for non-CVD diagnoses comparing doubling of CAC score and comparing those with CAC >400 to those with CAC =0. Model 1: Unadjusted. Model 2: Age (best fit model – see methods section), Gender, Race, Health Insurance status, and socioeconomic status (SES) (completed high school and income level). Model 3: Model 2 + body mass index (BMI), Physical Activity, Diet, Smoking Status and pack years. Model 4: Model 3 + Total Medications Used. Model 5: Model 4 + Systolic blood pressure (SBP), Diastolic blood pressure (DBP), Anti-Hypertensive Medications, Total Cholesterol, High density lipoprotein (HDL) Cholesterol, Lipid Lowering Medications, Diabetes, Aspirin use.
Statistically significant values are in black and bold for model 5. Non-significant values are in gray. CKD = chronic kidney disease; COPD=chronic obstructive pulmonary disease; DVT=deep vein thrombosis; PE=pulmonary embolism.
Table 3.
Hazard of new non-cardiovascular disease (CVD) and CVD diagnosis with coronary artery calcium score greater than 400 (CAC >400) compared to those with CAC = 0.
| CAC >400 v CAC =0 | |||||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| Cancer | 3.60 (2.95, 4.41) | 1.64 (1.29, 2.07) | 1.49 (1.16, 1.92) | 1.45 (1.13, 1.86) | 1.53 (1.18, 1.99) |
| CKD | 4.57 (3.55, 5.89) | 2.00 (1.47, 2.74) | 1.93 (1.39, 2.70) | 1.75 (1.27, 2.43) | 1.70 (1.21, 2.39) |
| Pneumonia | 4.72 (3.53, 6.30) | 2.16 (1.54, 3.02) | 1.88 (1.33, 2.68) | 1.71 (1.21, 2.41) | 1.97 (1.37, 2.82) |
| DVT/PE | 2.24 (1.50, 3.35) | 1.26 (0.80, 2.00) | 0.89 (0.54, 1.47) | 0.86 (0.52, 1.41) | 1.07 (0.64, 1.78) |
| COPD | 5.50 (3.64, 8.32) | 2.69 (1.61, 4.50) | 2.45 (1.44, 4.18) | 2.17 (1.30, 3.64) | 2.71 (1.60, 4.57) |
| Dementia | 6.45 (4.14, 10.05) | 1.33 (0.81, 2.19) | 1.47 (0.88, 2.47) | 1.48 (0.87, 2.50) | 1.61 (0.93, 2.79) |
| Hip Fracture | 8.74 (3.93, 19.45) | 3.18 (1.19, 8.50) | 4.16 (1.48, 11.73) | 3.91 (1.39, 10.97) | 4.29 (1.47, 12.50) |
| Any non-CVD | 4.16 (3.58, 4.84) | 1.88 (1.57, 2.24) | 1.78 (1.47, 2.15) | 1.69 (1.40, 2.04) | 1.80 (1.48, 2.18) |
| CVD | 9.52 (7.65, 11.86) | 6.01 (4.65, 7.77) | 5.44 (4.16, 7.10) | 5.11 (3.91, 6.67) | 4.45 (3.36, 5.88) |
Cox proportional hazard ratios and 95% confidence intervals for non-CVD diagnoses comparing doubling of CAC score and comparing those with CAC >400 to those with CAC =0. Model 1: Unadjusted. Model 2: Age (best fit model – see methods section), Gender, Race, Health Insurance status, and socioeconomic status (SES) (completed high school and income level). Model 3: Model 2 + body mass index (BMI), Physical Activity, Diet, Smoking Status and pack years. Model 4: Model 3 + Total Medications Used. Model 5: Model 4 + Systolic blood pressure (SBP), Diastolic blood pressure (DBP), Anti-Hypertensive Medications, Total Cholesterol, High density lipoprotein (HDL) Cholesterol, Lipid Lowering Medications, Diabetes, Aspirin use.
Statistically significant values are in black and bold for model 5. Non-significant values are in gray. CKD = chronic kidney disease; COPD=chronic obstructive pulmonary disease; DVT=deep vein thrombosis; PE=pulmonary embolism.
Table 4.
Hazard of new non-cardiovascular disease (CVD) diagnosis for those with CAC=0 compared to those with CAC >0.
| CAC =0 vs CAC >0 | |||||
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| Cancer | 0.44 (0.38, 0.51) | 0.75 (0.64, 0.89) | 0.77 (0.64, 0.92) | 0.79 (0.66, 0.94) | 0.76 (0.63, 0.92) |
| CKD | 0.38 (0.31, 0.46) | 0.69 (0.55, 0.86) | 0.71 (0.56, 0.90) | 0.74 (0.58, 0.94) | 0.77 (0.60, 0.98) |
| Pneumonia | 0.40 (0.32, 0.50) | 0.71 (0.55, 0.92) | 0.78 (0.60, 1.02) | 0.82 (0.62, 1.06) | 0.77 (0.58, 1.01) |
| DVT/PE | 0.57 (0.44, 0.75) | 0.85 (0.62, 1.17) | 1.01 (0.73, 1.41) | 1.04 (0.75, 1.45) | 0.94 (0.66, 1.33) |
| COPD | 0.32 (0.23, 0.45) | 0.56 (0.38, 0.81) | 0.64 (0.43, 0.96) | 0.69 (0.46, 1.03) | 0.61 (0.40, 0.91) |
| Dementia | 0.26 (0.18, 0.38) | 0.87 (0.59,1.30) | 0.81 (0.54, 1.21) | 0.80 (0.53, 1.21) | 0.76 (0.49, 1.17) |
| Hip Fracture | 0.17 (0.09, 0.33) | 0.37 (0.17, 0.78) | 0.30 (0.14, 0.67) | 0.31 (0.14, 0.69) | 0.31 (0.14, 0.70) |
| Any non-CVD | 0.41 (0.36, 0.45) | 0.71 (0.63,0.81) | 0.74 (0.65, 0.85) | 0.76 (0.66, 0.87) | 0.75 (0.65, 0.86) |
| CVD | 0.21 (0.17, 0.25) | 0.31 (0.26, 0.39) | 0.34 (0.27, 0.42) | 0.35 (0.28, 0.43) | 0.38 (0.30, 0.47) |
Cox proportional hazard ratios and 95% confidence intervals for non-CVD diagnoses comparing doubling of CAC score and comparing those with CAC >400 to those with CAC =0. Model 1: Unadjusted. Model 2: Age (best fit model – see methods section), Gender, Race, Health Insurance status, and socioeconomic status (SES) (completed high school and income level). Model 3: Model 2 + body mass index (BMI), Physical Activity, Diet, Smoking Status and pack years. Model 4: Model 3 + Total Medications Used. Model 5: Model 4 + Systolic blood pressure (SBP), Diastolic blood pressure (DBP), Anti-Hypertensive Medications, Total Cholesterol, High density lipoprotein (HDL) Cholesterol, Lipid Lowering Medications, Diabetes, Aspirin use.
Statistically significant values are in black and bold for model 5. Non-significant values are in gray. CKD = chronic kidney disease; COPD=chronic obstructive pulmonary disease; DVT=deep vein thrombosis; PE=pulmonary embolism.
Chronic Kidney Disease (CKD)
CKD was diagnosed in 395 participants. The proportion increased with increasing CAC stratum from 3.2% in participants with CAC=0 to 13.3% in participants with CAC >400 (p<0.001) (Figure 1). With adjustment for CVD risk factors, a doubling of CAC score remained significantly associated with an increased hazard of being diagnosed (HR 1.07, 1.03- 1.10)(Table 2). Those with CAC >400 were 70% more likely to develop CKD compared to those with CAC = 0 (HR 1.70, 1.21- 2.39) (Table 3) and those with CAC=0 had a lower hazard of being diagnosed with CKD (HR 0.77, 0.60-0.98) (Table 4).
Pneumonia
There were 315 cases of pneumonia. Proportions ranged from 2.8% when CAC=0 to 10.6% in those with CAC >400 (p<0.001) (Figure 1). In multivariable-adjusted models (model 5), there was a 7% increased hazard of being diagnosed with pneumonia with doubling of the CAC score (HR 1.07, 1.03 - 1.11)(Table 2). Those with CAC>400 had two times the hazard of developing pneumonia compared to those with CAC=0 (HR 1.97, 1.37- 2.82) (Table 3). Those with CAC=0 did not have a significantly decreased risk of pneumonia (HR 0.77, 0.58 – 1.01) when compared to those with CAC>0 (Table 4). This was associated in unadjusted models but lost after controlling for demographic and lifestyle factors (model 3, Table 4).
Deep Vein Thrombosis (DVT) or Pulmonary Embolism (PE)
DVT or PE was documented in 205 participants. Among those with CAC=0, 1.1% were diagnosed, 1.9% in those with CAC= 1-400 and 2.1% in those with CAC >400 (p<0.05) (Figure 1). In unadjusted models, doubling of CAC score and CAC >400 were associated with increased hazard of DVT or PE (1.10, 1.06-1.13 and 2.24, 1.50-3.35, respectively) (Table 2 and 3, respectively). Having CAC=0 was protective in unadjusted models (0.57, 0.44-0.75) (Table 4).
These relationships were lost after controlling for age, gender, race, SES and health insurance status (Tables 2, 3 and 4). In multivariable adjusted models (model 5), there was no association with a new diagnosis of DVT/PE and doubling of the CAC score (HR 1.03, 0.98 – 1.08) (Table 2), having CAC>400 (1.07, 0.64 – 1.78) (Table 3) or having CAC =0 (0.94, 0.66 – 1.33) (Table 4).
Chronic Obstructive Pulmonary Disease (COPD)
During follow up, 161 participants were diagnosed with COPD. Proportions increased with increasing CAC score stratum from 1.2% in those with CAC=0 to 5.6% in those with CAC >400 (p<0.001) (Figure 1). In model 5, doubling of CAC score was associated with a 10% increased hazard of COPD (1.10, 1.05 – 1.16)(Table 2). Those with CAC >400 were 2.7 times more likely than those with CAC=0 (2.71, 1.60 – 4.57) to have a new diagnosis of COPD (Table 3). Those with CAC=0 were approximately half as likely to be diagnosed compared to those with any CAC (0.61, 0.40 – 0.91) (Table 4).
Dementia
Dementia was diagnosed in 119 participants and had increasing proportions with higher CAC stratum from 0.61% to 4.43% (p<0.001) (Figure 1). After multivariable adjustment, doubling of the CAC score was associated with a 6% increased risk (HR 1.06, 1.01 - 1.12) (Table 2). Comparing those with CAC >400, to those with CAC=0, unadjusted models showed an increased hazard ratio of 6.45 (4.14, 10.05) (Table 3). This relationship was lost when controlling for age, gender, race, SES and health insurance status (model 2, Table 3). Similarly, those with CAC=0 compared to those with CAC>0 had a significant association in unadjusted models (0.26, 0.18-0.38) but this was lost when controlling for age, gender, race, SES and health insurance status (model 2, Table 4).
Hip Fractures
Hip fractures were the least common with 59 cases. Proportions diagnosed by CAC category ranged from 0.26% when CAC=0 to 1.77% in those with CAC >400 (p<0.001) (Figure 1). In multivariable adjusted models, doubling of CAC was associated with a 10% increased risk of events (1.01 - 1.21) (Table 2). Participants with CAC >400 had a higher risk of hip fracture in multivariable adjusted modeling (model 5) (4.29, 1.47 - 12.5) (Table 3). Participants with CAC=0 had a 69% lower risk of hip fracture in multivariable adjusted modeling (0.31, 0.14 – 0.70) (Table 4).
Aggregate outcome of first any non-CVD diagnosis
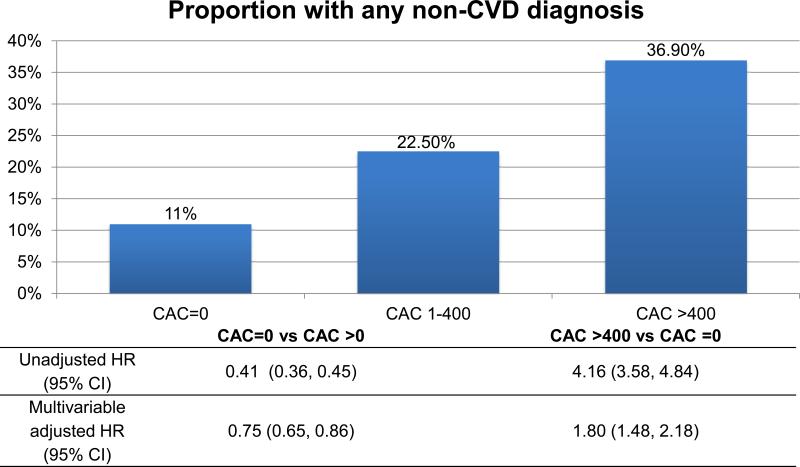
There were 1,238 first non-CVD diagnoses. The proportion of the first occurrence of any one of these was 11.0% for CAC =0, 22.5% for CAC=1 – 400 and 36.9% for CAC >400 (p<0.001) (Figure 2). In multivariable adjusted models, doubling of the CAC score was associated with a 6% increased risk of any non-CVD diagnosis (HR 1.06, 1.04-1.08) (Table 2). Those with CAC score >400 were 1.80 times more likely to be diagnosed with any non-CVD compared to those with CAC = 0 (HR 1.80, 1.48 -2.18) (Table 3). Participants with CAC=0 had a lower rate of non-CV disease compared to those with CAC>0 (HR 0.75, 0.65-0.86) (Table 4). Kaplan Meier curves for the composite and individual outcomes are shown in supplementary materials.
Figure 2.
Proportion of participants with any non-cardiovascular disease (CVD) diagnosis along with unadjusted (model 1) and multivariable adjusted (model 5) Cox proportional hazard ratios, adjusted for the competing risk of fatal coronary heart disease (95% confidence intervals). Multivariable model was adjusted for age (best fit, see methods), gender, race, socioeconomic status (SES), health insurance status, smoking status and pack years of smoking, body mass index (BMI), physical activity, diet, total number of medications used, systolic and diastolic blood pressure, anti-hypertensive medication use, total and HDL (high density lipoprotein) cholesterol, lipid lowering medication and aspirin use and presence of diabetes.
Sensitivity analysis
The results of the sensitivity analysis are in supplementary table 2. Results were attenuated, with similar overall conclusions after removing participants with an interim or concurrent non-fatal CHD event at the time of diagnosis of the non-CV disease. New diagnoses of cancer, CKD, COPD and any-non CVD event remained associated with doubling of CAC score (Supplementary Table 2).
Age stratification
Results of age stratified analysis are presented in Table 5. In participants ≥65, doubling of the CAC score was associated with an increased hazard of cancer (1.04, 1.01 – 1.07), CKD (1.07, 1.03 – 1.11), pneumonia (1.08, 1.03 – 1.13), COPD (1.09, 1.03 – 1.16) and the composite outcome (1.06, 1.04 – 1.08). Limited power prevented detailed analysis of modeling in those <65, although point estimates were similar with non-significant interaction with the age < or ≥ 65 term.
Table 5.
Age stratified analysis of the doubling of coronary artery calcium (CAC) score.
| Log2[CAC+1] | ||
|---|---|---|
| Age <65 | Age ≥65 | |
| Cancer | 1.04 (1.00 – 1.09) | 1.04 (1.01 – 1.07) |
| CKD | 1.05 (0.98 – 1.12) | 1.07 (1.03 – 1.11) |
| Pneumonia | 1.04 (0.97 – 1.11) | 1.08 (1.03 – 1.13) |
| DVT/PE | 1.03 (0.95 – 1.11) | 1.02 (0.96 – 1.08) |
| COPD | 1.12 (1.00 – 1.25) | 1.09 (1.03 – 1.16) |
| Dementia | -- | 1.06 (1.00 – 1.12) |
| Hip Fracture | 1.15 (0.94 – 1.41) | 1.09 (0.99 – 1.20) |
| Any non-CVD event | 1.04 (1.00 – 1.07) | 1.06 (1.04 – 1.08) |
| CVD | 1.19 (1.14, 1.24) | 1.16 (1.12, 1.20) |
Cox proportional hazard ratios (and 95% confidence intervals) for those <65 and those ≥65 years of age. Model is adjusted for age (best fit – see methods section), gender, race, health insurance status, SES (completed high school and income level), body mass index (BMI), physical activity, diet, smoking status and pack years, total number of medications used, systolic blood pressure (SBP), diastolic blood pressure (DBP), anti-hypertensive medications, total cholesterol, high density lipoprotein (HDL) cholesterol, lipid lowering medications, diabetes and aspirin use. The interaction of CAC with age < or ≥ 65 was not significant.
Statistically significant values are in black and bold. Non-significant values are in gray. CKD = chronic kidney disease; COPD=chronic obstructive pulmonary disease; DVT=deep vein thrombosis; PE=pulmonary embolism; CVD = cardiovascular disease.
Discussion
Our results demonstrate that CAC scores are associated with non-CVD diagnoses, notably cancer, CKD, COPD and hip fractures. Participants with CAC scores >400 had a 53% adjusted increased hazard of cancer diagnosis, 70% increased hazard of CKD diagnosis, 197% increased hazard of developing pneumonia, 271% increased hazard of COPD diagnosis, and 429% increased hazard of hip fracture. Participants with CAC = 0 (50% of the population) appeared at reduced risk of non-CVD, independent of known CVD risk factors. While these results were attenuated when excluding patients with interim non-fatal CHD events, overall conclusions remained unchanged. Taken together, higher CAC scores were highly associated with the initial development of any first non-CVD diagnosis. From a public health perspective, it is notable that 20% of the first occurrences of a non-CVD event occurred in the 10% of patients with CAC >400 and 70% of the events were in those with CAC >0.
Strengths of our analysis include the large sample, multi-ethnic makeup, detailed baseline risk factor assessment, and the use of a competing risk model, which is important given the known association of CAC with fatal CHD. In addition, rather than assuming a linear association, we allowed flexible modeling of age to achieve the best fit and thus limit residual confounding from age.
It is important to consider the possible mechanisms underlying these results. CAC per se is unlikely to be causally associated with non-CVD. In general, CAC is considered to be a risk integrator, and may reflect lifetime exposure to both measured and unmeasured risk factors shared in common between CVD and non-CVD outcomes (21). It may also represent a common underlying vulnerability to the development of tissue injury at sites with varying relationships to the cardiovascular system. As such, the CAC score may be one marker of an individual's risk of future disease burden.
Pneumonia was not associated with CAC scores in models removing individuals with an interim non-fatal CHD event, suggesting it may be a more acute event that is more likely to be an incidental co-diagnosis during the inpatient care for, or related to complications of, a CHD event. Furthermore, DVT/PE were weakly associated with CAC and are well known to have a variety of more acute-onset risk factors, including trauma and surgery(22) which could be less related to CVD and arterial aging. Dementia, likely had too few cases to confirm an association with CAC given the large confidence interval.
Implications
We hypothesized that CAC scores could be a surrogate measure of arterial aging and identify those at increased risk of age related, non-CV disease. CAC has been described as a measure of so-called “biologic age” (7), supported by studies showing absolute CAC scores as better predictors of CVD events than age alone (10). Our results support CAC as a marker for other age related diseases and support limited prior findings showing an association between elevated CAC scores and non-CV diseases including cancer (13) and COPD (23). While CAC has been shown to be associated with all-cause mortality (24-26), this association may be driven by both cardiovascular and select non-cardiovascular causes. The risk ratio of cardiovascular versus non-CVD diagnoses likely varies as a function of the CAC score and future mortality studies may benefit from ascertainment of cause of death and modeling the risk of both cardiovascular and non-cardiovascular causes.
An important finding is that people with CAC=0 appear to be protected from CVD and other chronic diseases. These “healthy agers” are at very low risk of CVD and non-CVD morbidity and mortality (24, 27, 28). There are broad implications to identifying and studying such people in the population. These people are extremely unlikely to be high utilizers of health care services because of the decreased risk of comorbidities. In contrast, those with elevated CAC are at high risk of developing multiple chronic conditions and are likely to require increased services. These findings, which mirror the observation that individuals with multiple chronic conditions utilize a disproportionate share of healthcare resources (29), have marked implications for patient centered medical homes, accountable care organizations, insurers, public health officials, and other stakeholders in the distribution of healthcare resource expenditures.
Limitations
New non-CVD diagnoses in MESA were obtained via ICD hospital coding and therefore must be interpreted as time-to-diagnosis, not necessarily time-to-disease onset. This would mostly affect the diagnoses of cancer, COPD and CKD, which could be detected prior to hospitalization. Furthermore, by using inpatient codes, there may be bias towards capturing severe cases and missing milder cases that are exclusively managed in the outpatient setting. Additionally, outcome ascertainment was administrative and does not represent systematically adjudicated events as is the case for CVD-related outcomes in MESA.
The number of participants with hip fractures, DVT/PE and dementia were small and our study may not be powered to firmly establish the relationship. Further studies of these outcomes are needed, perhaps leveraging electronic medical record (EMR) and claims files databases that would allow examination of a larger sample of patients. In addition, follow up time in MESA may not be sufficient for detecting risk in participants with the lowest CAC scores. At this time, our data are not powered for stratifying results based on gender or race.
Conclusion
Elevated CAC scores are associated with age-related diseases including cancer, COPD, CKD, and hip fractures. Those with CAC=0 are less likely to develop common age related comorbid conditions, and represent a unique population of “healthy agers”.
Supplementary Material
Perspectives.
Competency in Medical Knowledge:
Coronary artery calcium (CAC) scoring is a non-invasive, direct measure of coronary atherosclerosis
Competency in Patient Care and Procedural Skills:
CAC retains a strong predictive value for all-cause mortality beyond age
Translational Outlook:
People with CAC=0 appear to be protected from multiple chronic non cardiovascular diseases.
Acknowledgements
The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Financial support – This research was supported by contracts N01-HC-95159, N01-HC-95160, N01-HC-95161, N01-HC-95162, N01-HC-95163, N01-HC-95164, N01-HC-95165, N01-HC-95166, N01-HC-95167, N01-HC-95168 and N01-HC-95169 from the National Heart, Lung, and Blood Institute and by grants UL1-TR-000040 and UL1-TR-001079 from NCRR.
There are no relationships with industry.
Abbreviations
- CAC
coronary artery calcium
- CVD
cardiovascular disease
- CHD
coronary heart disease
- COPD
chronic obstructive pulmonary disease
- PE
pulmonary embolism
- DVT
deep vein thrombosis
- SBP
systolic blood pressure
- DBP
diastolic blood pressure
- CT
computed tomography
- SES
socioeconomic status
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med. 2007;356:2388–98. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 2.Araujo F, Gouvinhas C, Fontes F, La Vecchia C, Azevedo A, Lunet N. Trends in cardiovascular diseases and cancer mortality in 45 countries from five continents (1980-2010). Eur J Prev Cardiol. 2013 doi: 10.1177/2047487313497864. [DOI] [PubMed] [Google Scholar]
- 3.Siegel R, Naishadham D, Jemal A. Cancer statistics for hispanics/latinos, 2012. CA Cancer J Clin. 2012;62:283–98. doi: 10.3322/caac.21153. [DOI] [PubMed] [Google Scholar]
- 4.Shaw LJ, Raggi P, Schisterman E, Berman DS, Callister TQ. Prognostic value of cardiac risk factors and coronary artery calcium screening for all-cause mortality. Radiology. 2003;228:826–33. doi: 10.1148/radiol.2283021006. [DOI] [PubMed] [Google Scholar]
- 5.McClelland RL, Chung H, Detrano R, Post W, Kronmal RA. Distribution of coronary artery calcium by race, gender, and age: Results from the multi-ethnic study of atherosclerosis (MESA). Circulation. 2006;113:30–7. doi: 10.1161/CIRCULATIONAHA.105.580696. [DOI] [PubMed] [Google Scholar]
- 6.Tota-Maharaj R, Blaha MJ, McEvoy JW, et al. Coronary artery calcium for the prediction of mortality in young adults 75 years old. Eur Heart J. 2012;33:2955–62. doi: 10.1093/eurheartj/ehs230. [DOI] [PubMed] [Google Scholar]
- 7.Shaw LJ, Raggi P, Berman DS, Callister TQ. Coronary artery calcium as a measure of biologic age. Atherosclerosis. 2006;188:112–9. doi: 10.1016/j.atherosclerosis.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 8.Grundy SM. Coronary plaque as a replacement for age as a risk factor in global risk assessment. Am J Cardiol. 2001;88:8E–11E. doi: 10.1016/s0002-9149(01)01712-x. [DOI] [PubMed] [Google Scholar]
- 9.Tota-Maharaj R, Blaha MJ, Blankstein R, et al. Association of coroary artery calcium and coronary heart disease events in young and elderly participants in the multi-ethnic study of atherosclerosis: A secondary analysis of a prospective, population-based cohort. Mayo Clin Proc. 2014;89:1350–9. doi: 10.1016/j.mayocp.2014.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McClelland RL, Nasir K, Budoff M, Blumenthal RS, Kronmal RA. Arterial age as a function of coronary artery calcium (from the multi-ethnic study of atherosclerosis [MESA]). Am J Cardiol. 2009;103:59–63. doi: 10.1016/j.amjcard.2008.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.LaMonte MJ, FitzGerald SJ, Church TS, et al. Coronary artery calcium score and coronary heart disease events in a large cohort of asymptomatic men and women. Am J Epidemiol. 2005;162:421–9. doi: 10.1093/aje/kwi228. [DOI] [PubMed] [Google Scholar]
- 12.Desai CS, Ning H, Kang J, et al. Competing cardiovascular outcomes associated with subclinical atherosclerosis (from the multi-ethnic study of atherosclerosis). Am J Cardiol. 2013;111:1541–6. doi: 10.1016/j.amjcard.2013.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen WT, Huang JH, Hsieh MH, Chen YJ. Extremely high coronary artery calcium score is associated with a high cancer incidence. Int J Cardiol. 2012;155:474–5. doi: 10.1016/j.ijcard.2011.12.077. [DOI] [PubMed] [Google Scholar]
- 14.Fox CS, Larson MG, Keyes MJ, et al. Kidney function is inversely associated with coronary artery calcification in men and women free of cardiovascular disease: The framingham heart study. Kidney Int. 2004;66:2017–21. doi: 10.1111/j.1523-1755.2004.00973.x. [DOI] [PubMed] [Google Scholar]
- 15.Parikh NI, Hwang SJ, Larson MG, et al. Indexes of kidney function and coronary artery and abdominal aortic calcium (from the framingham offspring study). Am J Cardiol. 2008;102:440–3. doi: 10.1016/j.amjcard.2008.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bakhireva LN, Barrett-Connor EL, Laughlin GA, Kritz-Silverstein D. Differences in association of bone mineral density with coronary artery calcification in men and women: The rancho bernardo study. Menopause. 2005;12:691–8. doi: 10.1097/01.gme.0000184422.50696.ef. [DOI] [PubMed] [Google Scholar]
- 17.Hyder JA, Allison MA, Wong N, et al. Association of coronary artery and aortic calcium with lumbar bone density: The MESA abdominal aortic calcium study. Am J Epidemiol. 2009;169:186–94. doi: 10.1093/aje/kwn303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bild DE, Bluemke DA, Burke GL, et al. Multi-ethnic study of atherosclerosis: Objectives and design. Am J Epidemiol. 2002;156:871–81. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 19.Carr JJ, Nelson JC, Wong ND, et al. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: Standardized protocol of multi-ethnic study of atherosclerosis (MESA) and coronary artery risk development in young adults (CARDIA) study. Radiology. 2005;234:35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- 20.Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–45. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 21.Blaha MJ, Silverman MG, Budoff MJ. Is there a role for coronary artery calcium scoring for management of asymptomatic patients at risk for coronary artery disease?: Clinical risk scores are not sufficient to define primary prevention treatment strategies among asymptomatic patients. Circ Cardiovasc Imaging. 2014;7:398, 408. doi: 10.1161/CIRCIMAGING.113.000341. discussion 408. [DOI] [PubMed] [Google Scholar]
- 22.Anderson FA, Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003;107:I9–16. doi: 10.1161/01.CIR.0000078469.07362.E6. [DOI] [PubMed] [Google Scholar]
- 23.Park HY, Lim SY, Hwang JH, et al. Lung function, coronary artery calcification, and metabolic syndrome in 4905 korean males. Respir Med. 2010;104:1326–35. doi: 10.1016/j.rmed.2010.02.024. [DOI] [PubMed] [Google Scholar]
- 24.Budoff MJ, Shaw LJ, Liu ST, et al. Long-term prognosis associated with coronary calcification: Observations from a registry of 25,253 patients. J Am Coll Cardiol. 2007;49:1860–70. doi: 10.1016/j.jacc.2006.10.079. [DOI] [PubMed] [Google Scholar]
- 25.Shaw LJ, Giambrone AE, Blaha MJ, et al. Long-term prognosis after coronary artery calcification testing in asymptomatic patients: A cohort study. Ann Intern Med. 2015;163:14–21. doi: 10.7326/M14-0612. [DOI] [PubMed] [Google Scholar]
- 26.Raggi P, Gongora MC, Gopal A, Callister TQ, Budoff M, Shaw LJ. Coronary artery calcium to predict all-cause mortality in elderly men and women. J Am Coll Cardiol. 2008;52:17–23. doi: 10.1016/j.jacc.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 27.Blaha M, Budoff MJ, Shaw LJ, et al. Absence of coronary artery calcification and all-cause mortality. JACC Cardiovasc Imaging. 2009;2:692–700. doi: 10.1016/j.jcmg.2009.03.009. [DOI] [PubMed] [Google Scholar]
- 28.Budoff MJ, McClelland RL, Nasir K, et al. Cardiovascular events with absent or minimal coronary calcification: The multi-ethnic study of atherosclerosis (MESA). Am Heart J. 2009;158:554–61. doi: 10.1016/j.ahj.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vogeli C, Shields AE, Lee TA, et al. Multiple chronic conditions: Prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med. 2007;22(Suppl 3):391–5. doi: 10.1007/s11606-007-0322-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.