Abstract
Focal segmental glomerulosclerosis (FSGS) is a common cause of end-stage renal disease and a common pathologic diagnosis of idiopathic nephrotic syndrome (NS), especially in steroid-resistant cases. FSGS is known to recur after kidney transplantation, frequently followed by graft loss. However, not all patients with FSGS suffer from recurrence after kidney transplantation, and genetic and secondary FSGS have a negligible risk of recurrence. Furthermore, many cases of recurrence achieve remission with the current management of recurrence (intensive plasmapheresis/immunosuppression, including rituximab), and other promising agents are being evaluated. Therefore, a pathologic diagnosis of FSGS itself should not cause postponement of allograft kidney transplantation. For patients with a high risk of recurrence who presented with classical symptoms of NS, that is, severe edema, proteinuria, and hypoalbuminemia, close monitoring of proteinuria is necessary, followed by immediate, intensive treatment for recurrence.
1. Introduction
Focal segmental glomerulosclerosis (FSGS) is a common cause of end-stage renal disease (ESRD). In children, the major causes of ESRD are congenital anomalies of the kidney and urinary tract and hereditary nephropathies, followed by FSGS as the most common form of acquired glomerulopathies causing ESRD [1, 2]. FSGS is the second-most common pathologic diagnosis of idiopathic nephrotic syndrome (NS) [3, 4]. Although the majority of pediatric idiopathic NS patients respond to steroid treatment, some are resistant to treatment and eventually progress to ESRD [5], and their renal pathology often reveals FSGS. Because FSGS is known to recur after kidney transplantation, frequently followed by graft loss in up to 60% of the cases [6–9], the diagnosis of idiopathic FSGS requires a thorough discussion of its prognosis with patients and their families. However, not all patients with FSGS suffer from recurrence after kidney transplantation, and many cases of recurrence achieve remission with the current management of recurrence and enjoy life as a kidney allograft recipient for as long as the average kidney recipient [10–12]. In this paper, the current knowledge of the risk factors for recurrence of FSGS and its treatment in children will be reviewed.
2. Who Is at Risk of Recurrence and Who Is Not?
The reported rates of recurrence are quite variable, from 6 to 58%, depending on the characteristics of the population studied [11–14]. The suggested risk factors for recurrence include the age at onset of disease [14–16], a rapid progression to ESRD (<48–72 months) [17–21], and a history of previous recurrence in an allograft [6, 18, 22]. Pathologic characteristics of the native kidney biopsy, such as mesangial hypercellularity [23] and fewer sclerotic glomeruli [19, 20], and a living donor allograft [24] have also been proposed as risk factors but have not been confirmed [25]. Native kidney nephrectomy prior to kidney transplantation has been suggested by some as a preventive measure of recurrence [21, 26, 27], but it has not been effective and has even shown a higher risk of recurrence in other reports [10, 28, 29]. According to our experiences with 38 children with FSGS, most of those with a later onset (≥6 yrs. old) and a progression to ESRD in the 24–72 months after onset of NS experienced recurrence, whereas those who had an earlier onset (<6 yrs.) of NS with a faster progression (<18 months) did not have recurrence [11]. There has been controversy over the onset age group that is at risk of recurrence; generally younger patients are considered to be at a higher risk than older patients [13], but some studies have reported no differences between adults and children [30] and even higher risks in adults than in children [25]. The main reason for these differences could be the small sample size of the study populations in most of the reports. In addition, two more aspects should be considered.
First, there are several genetic defects that cause FSGS [31–33], and the frequency and distribution of the genetic types of FSGS differ between populations. For example, the NPHS2 mutation is the dominant cause of genetic FSGS in European countries, but it is rare in Koreans and the Japanese [31, 34–36]. Although idiopathic steroid-resistant NS (SRNS) with FSGS pathology is believed to be caused by some circulating factors [37] and is therefore prone to recur after kidney transplantation, most genetic FSGS have defective components of the kidneys, particularly podocytes, and therefore their risk of recurrence is low if not zero [16, 32, 36, 38–40]. Some genetic FSGS are characterized by an early onset of SRNS; some syndromic FSGS are accompanied by extra-renal symptoms that may not be evident at the onset of SRNS, thus mimicking idiopathic SRNS. Because a genetic diagnosis of SRNS-FSGS has not yet been incorporated as a routine component of clinical practice in most parts of the world, we do not know how many of the patients previously categorized as SRNS-FSGS have genetic FSGS. In fact, some of the cases that we previously reported as idiopathic SRNS-FSGS were recently found to have mutations in COQ6 [41] (in patients with progressive hearing loss) or a newly found FSGS-causing gene NUP107 [42] (unpublished data); these patients had an earlier onset (<6 yrs.) of NS with a faster progression (<18 months) and did not have recurrence [11]. A recent report by Ding et al. showed that children with SRNS who initially responded to steroid treatment were at risk of recurrence after kidney transplantation [43]. This finding may also imply that these cases have nongenetic FSGS. In other words, the wide range of risks of recurrence found in the literature seems to have been dependent on whether genetic testing was broadly performed in the studied cohort.
Second, FSGS is a pathologic diagnosis, and there are multiple causes other than idiopathic SRNS that lead to FSGS [44]. Some of the causes are evident, such as chronic infection (e.g., HIV infection) or reflux nephropathy; however, others are not. Therefore, the distinction between “secondary” and primary (idiopathic) FSGS is not always clear. Similar to genetic FSGS, FSGS secondary to other causes does not recur after kidney transplantation if the causes no longer exist after kidney transplantation; some of the reported FSGS cases without recurrence may in fact have been secondary FSGS. In our own clinical experience, patients who presented with proteinuria but without edema did not experience recurrence; although there was no identifiable cause of FSGS and they were therefore categorized as primary FSGS, we speculate that these cases may have had obscure causes leading to FSGS [11]. Therefore, the pathologic diagnosis of FSGS itself does not mean that the disease could recur after kidney transplantation.
3. Are There Biomarkers Predicting Recurrence?
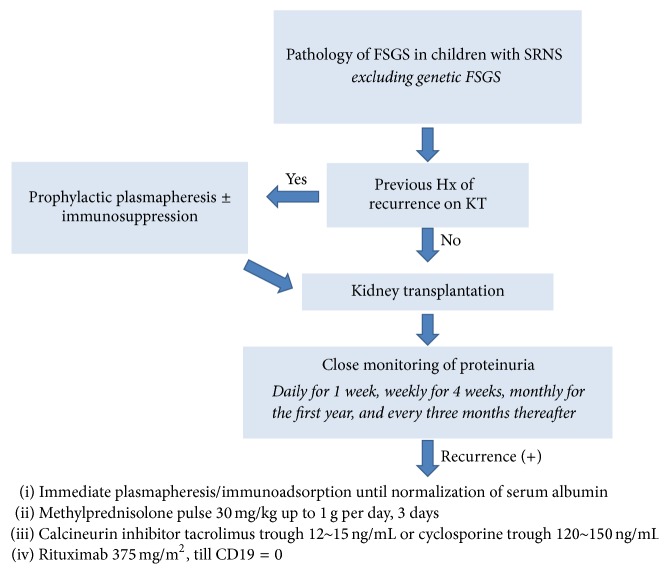
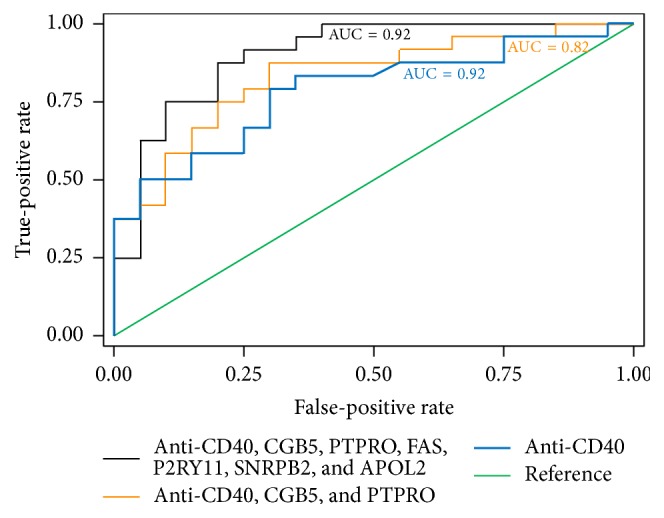
Despite a decades-long search for circulating “permeability factor(s)” causing FSGS [47], these factors remain elusive [37]. When soluble urokinase receptor (suPAR) was reported to be a candidate permeability factor [48], this news was met with excitement. However, contradicting reports followed [49], and therefore the usefulness of suPAR as a biomarker predicting recurrence is currently doubted. Cardiotrophin-like 1 (CLC-1) is another candidate that has been proposed by Savin's group [50] and is awaiting validation. Similar to other circulating factors, autoantibodies including anti-CD40 antibody have been proposed that have shown a good predictive accuracy of recurrence (Figure 1), but these candidates require further validation in clinical trials [45]. Another approach to identifying biomarkers is the assessment of podocyte changes in response to suspicious factor(s). Vasodilator-stimulated phosphoprotein (VASP) in human podocytes has been shown to be phosphorylated in response to plasma from patients with posttransplant recurrence but not to plasma from non-FSGS, and genetic FSGS cases did not show this effect on podocytes (Figure 2). Once these promising biomarkers are validated and incorporated into clinical practice, we will be able to better predict whether recurrence will occur in a certain patient after kidney transplantation [46]. This would enable us to properly evaluate the efficacy of prophylactic management such as prophylactic plasmapheresis/immunoadsorption or immunosuppression and to possibly conduct preventive measures before transplantation [9].
Figure 1.
Validation of the FAST Ab panel in rFSGS and the predictive accuracy of the subsets of this panel. ROC analysis for three fitted logistic regression models. The outcome was recurrence versus nonrecurrence of FSGS, and the independent predictors were the log-transformed relative fluorescent signal values of seven Abs: CD40, PTPRO, FAS, CGB5, SNRPB2, APOL2, and P2RY11. The three logistic regression models fitted are shown. Model 1 used the FAST (FSGS antibody serological test) panel with all seven Abs, resulting in an AUC = 0.9. Model 2 used three Abs (CD40, PTPRO, and CGB5), and its ROC curve had an AUC of 0.82. Model 3 used only CD40 Ab data for the ROC analysis, resulting in an AUC of 0.77. Reproduced with permission from The American Association for the Advancement of Science © 2014 (AAAS), Delville et al. [45].
Figure 2.
Scatter plot of VASP phosphorylation levels by patient group. Phosphorylation for each individual sample was assigned a densitometry value relative to the control (normal) plasma sample from the same gel, which was normalized to 1. Reproduced with permission from Wiley © 2012 Pathological Society of Great Britain and Ireland, Harris et al. [46].
4. How to Treat Recurrence
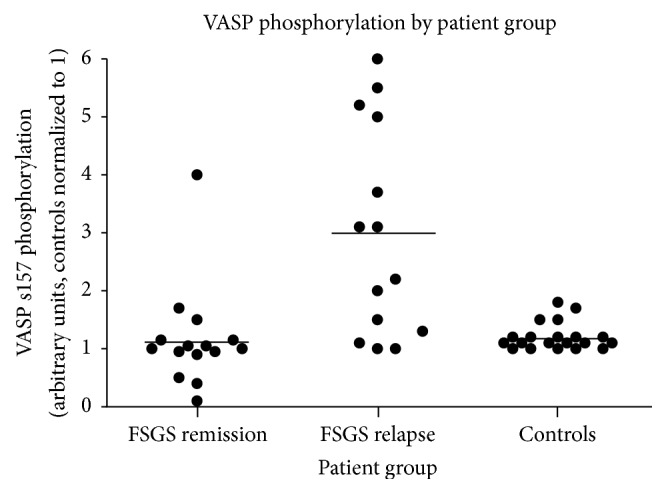
Although the recurrence of FSGS is a significant risk factor of graft loss [24, 29, 30, 51, 52], the outcomes of recurrent FSGS have so much improved that primary FSGS is no longer considered a contraindication of transplantation. The remission rate of pediatric recurrent FSGS has been reported to be as high as 70% [11, 12]. The mainstay of treatment for recurrent FSGS is plasmapheresis (removing 1.5 plasma volumes with 5% albumin replacement)/immunoadsorption because recurrence is believed to be caused by circulating factor(s) [53–55]. There have been no prospective randomized clinical trials to compare the efficacies of plasmapheresis and immunoadsorption, and the outcomes of studies using either method seem similar; therefore, the choice between these two methods depends on their availability and the preference of the treating physician [55–57]. It is important to begin treatment as soon as possible because removal or replacement of the FSGS-causing circulating factor(s) should be instituted before irreversible damage can be inflicted to the glomeruli [58]. While there is no evidence that anuric status at the time of transplantation prevents recurrence, recurrence can be detected more promptly if the patient had been anuric, and therefore native kidney nephrectomy can be considered in patients with residual urine output. Once the factors are removed, maintenance immunosuppression against graft rejection would also suppress the resurgence of the source of FSGS. It seems that, for some patients, plasmapheresis/immunoadsorption is sufficient to induce remission of recurrent FSGS [55, 59]. For others, intense immunosuppression with high-dose methylprednisolone, cyclosporine [12], cyclophosphamide [9], or rituximab [60] at various combinations is necessary. Although high-dose cyclosporine has been advocated as necessary by some [9, 12] and tacrolimus as a replacement for cyclosporine has been questioned [9], in our own clinical experience, tacrolimus trough levels of 12 to 15 ng/mL in combination with high-dose methylprednisolone and rituximab in addition to immediate and intense plasmapheresis have worked well, achieving remission in more than 80% of recent recurrent cases (unpublished data). The addition of rituximab to the current strategy against recurrent FSGS seems beneficial, demonstrating a response rate of up to 79% in recurrent FSGS [60, 61]. Although the optimal dosage (375 mg/m2 up to 6 doses or a single dose of 100 mg [62]) and mechanism of action (eradication of B lymphocytes or binding to sphingomyelin phosphodiesterase acid-like 3b [SMPDL-3b] on podocytes [63]) of this medication remain elusive, a single dose or two of 375 mg/m2 rituximab have been satisfactory in achieving sustained complete remission in our practice (Figure 3).
Figure 3.
Approach for patients with SRNS-FSGS, authors' suggestion.
There are several promising therapeutic agents that are awaiting validation. Cytotoxic T-lymphocyte-associated antigen 4-immunoglobulin fusion protein (CTLD4-Ig, abatacept) has been tested on the basis that B7-1 (CD80) induction on podocytes plays an important role in the pathogenesis of proteinuria [64] and could eradicate proteinuria in recurrent FSGS [65]; however, the long-term efficacy of this agent has not been confirmed [66]. Of note, another form of CTLA4-Ig, belatacept, is being evaluated as a long-acting maintenance immunosuppressant against kidney allograft rejection [67]. CTLA4-Ig, a costimulatory inhibitor that competes with B7-1, could be indicated in the suppression of both allograft rejection and proteinuria. However, belatacept has been shown to increase the risk of posttransplant lymphoproliferative disease in Epstein-Barr virus- (EBV-) naïve patients [68]. Because the majority of pediatric recipients are naïve to EBV infection, caution is warranted when considering CTLA4-Ig as a therapeutic agent against recurrent FSGS in children. Another agent of interest is galactose. In the search for a “permeability factor” causing FSGS, galactose was found to bind to the factor(s) and eliminate their proteinuric effect [69, 70]. In addition to the clinical trials of this agent in pediatric SRNS [71, 72], anecdotal cases of significant improvement have been reported in recurrent FSGS [73, 74]. Successful treatment of recurrent FSGS has also been reported with anti-TNF-α treatment [75] (based on the upregulation of TNF-α mRNA in patients with FSGS [76]), adrenocorticotrophic hormone gel [77], and allogeneic mesenchymal stem cells [78, 79].
An important point is that treatment failure on native kidneys does not predict treatment failure for posttransplantation recurrence of FSGS. Why? For recurrent FSGS after transplantation, we start treatment almost immediately, before the formation of sclerosis. This implies that delays in treating the native kidney lead to treatment failure, resulting in progressive renal damage. Therefore, if we are equipped with reliable biomarkers that indicate which medications will be effective in specific patients at the time of NS diagnosis, we will be able to tailor the treatment of pediatric NS, thus applying “precision medicine” to these patients.
5. How to Prevent Recurrence
While any discussion of preventive treatments efficacy is futile because we do not know whether subjects will experience recurrence after transplantation, patients who had lost their previous allograft to recurrence of FSGS have particularly high risk of recurrence [6, 18, 22]. For these patients, to eliminate circulating factors, preemptive plasmapheresis/immunoadsorption is considered, three to five sessions prior to the transplantation followed by immediate posttransplant sessions of three to five [80–85]. Additional single dose of rituximab (375 mg/m2) along with immunosuppression of corticosteroid, calcineurin inhibitor, and mycophenolate mofetil for two weeks prior to kidney transplantation was shown to prevent recurrence [81, 84].
6. Conclusion
Recurrence after kidney transplantation is devastating for patients and families. However, the outcomes of recurrent FSGS are quite good with the current management strategy; therefore, the pathologic diagnosis of FSGS itself should not be a cause for postponing allograft kidney transplantation. For patients with a high risk of recurrence, close monitoring of proteinuria as suggested by the Kidney Disease: Improving Global Outcomes guidelines for the management of kidney transplant recipients [86] is necessary, followed by immediate, intensive treatment for recurrence, as suggested in Figure 3.
Acknowledgments
This study was supported by a grant (HI12C0014) from the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea.
Competing Interests
The authors declare that there are no competing interests regarding the publication of this paper.
References
- 1.Kari J. Epidemiology of chronic kidney disease in children. Journal of Nephropathology. 2012;1(3):162–163. doi: 10.5812/nephropathol.8113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harambat J., van Stralen K. J., Kim J. J., Tizard E. J. Epidemiology of chronic kidney disease in children. Pediatric Nephrology. 2012;27(3):363–373. doi: 10.1007/s00467-011-1939-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mubarak M., Kazi J. I., Lanewala A., Hashmi S., Akhter F. Pathology of idiopathic nephrotic syndrome in children: are the adolescents different from young children? Nephrology Dialysis Transplantation. 2012;27(2):722–726. doi: 10.1093/ndt/gfr221. [DOI] [PubMed] [Google Scholar]
- 4.Gipson D. S., Troost J. P., Lafayette R. A., et al. Complete remission in the nephrotic syndrome study network. Clinical Journal of the American Society of Nephrology. 2016;11(1):81–89. doi: 10.2215/CJN.02560315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mekahli D., Liutkus A., Ranchin B., et al. Long-term outcome of idiopathic steroid-resistant nephrotic syndrome: a multicenter study. Pediatric Nephrology. 2009;24(8):1525–1532. doi: 10.1007/s00467-009-1138-5. [DOI] [PubMed] [Google Scholar]
- 6.Cochat P., Fargue S., Mestrallet G., et al. Disease recurrence in paediatric renal transplantation. Pediatric Nephrology. 2009;24(11):2097–2108. doi: 10.1007/s00467-009-1137-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Stralen K. J., Verrina E., Belingheri M., et al. Impact of graft loss among kidney diseases with a high risk of post-transplant recurrence in the paediatric population. Nephrology Dialysis Transplantation. 2013;28(4):1031–1038. doi: 10.1093/ndt/gfs549. [DOI] [PubMed] [Google Scholar]
- 8.Canaud G., Delville M., Legendre C. Recurrence of focal and segmental glomerulosclerosis after transplantation. Transplantation. 2016;100(2):284–287. doi: 10.1097/TP.0000000000000902. [DOI] [PubMed] [Google Scholar]
- 9.Bacchetta J., Cochat P. Primary disease recurrence—effects on paediatric renal transplantation outcomes. Nature Reviews Nephrology. 2015;11(6):371–384. doi: 10.1038/nrneph.2015.54. [DOI] [PubMed] [Google Scholar]
- 10.Sener A., Bella A. J., Nguan C., Luke P. P. W., House A. A. Focal segmental glomerular sclerosis in renal transplant recipients: predicting early disease recurrence may prolong allograft function. Clinical Transplantation. 2009;23(1):96–100. doi: 10.1111/j.1399-0012.2008.00908.x. [DOI] [PubMed] [Google Scholar]
- 11.Lee S. E., Min S. I., Kim Y. S., et al. Recurrence of idiopathic focal segmental glomerulosclerosis after kidney transplantation: experience of a Korean tertiary center. Pediatric Transplantation. 2014;18(4):369–376. doi: 10.1111/petr.12257. [DOI] [PubMed] [Google Scholar]
- 12.Shishido S., Satou H., Muramatsu M., et al. Combination of pulse methylprednisolone infusions with cyclosporine-based immunosuppression is safe and effective to treat recurrent focal segmental glomerulosclerosis after pediatric kidney transplantation. Clinical Transplantation. 2013;27(2):E143–E150. doi: 10.1111/ctr.12079. [DOI] [PubMed] [Google Scholar]
- 13.Huang K., Ferris M. E., Andreoni K. A., Gipson D. S. The differential effect of race among pediatric kidney transplant recipients with focal segmental glomerulosclerosis. American Journal of Kidney Diseases. 2004;43(6):1082–1090. doi: 10.1053/j.ajkd.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 14.Hickson L. J., Gera M., Amer H., et al. Kidney transplantation for primary focal segmental glomerulosclerosis: outcomes and response to therapy for recurrence. Transplantation. 2009;87(8):1232–1239. doi: 10.1097/tp.0b013e31819f12be. [DOI] [PubMed] [Google Scholar]
- 15.Ingulli E., Tejani A. Incidence, treatment, and outcome of recurrent focal segmental glomerulosclerosis posttransplantation in 42 allografts in children—a single-center experience. Transplantation. 1991;51(2):401–405. doi: 10.1097/00007890-199102000-00025. [DOI] [PubMed] [Google Scholar]
- 16.Maas R. J. H., Deegens J. K. J., van den Brand J. A. J. G., Cornelissen E. A. M., Wetzels J. F. M. A retrospective study of focal segmental glomerulosclerosis: clinical criteria can identify patients at high risk for recurrent disease after first renal transplantation. BMC Nephrology. 2013;14, article 47 doi: 10.1186/1471-2369-14-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tejani A., Stablein D. H. Recurrence of focal segmental glomerulosclerosis posttransplantation: a special report of the North American pediatric renal transplant cooperative study. Journal of the American Society of Nephrology. 1992;2(12) supplement:S258–S263. doi: 10.1681/ASN.V212s258. [DOI] [PubMed] [Google Scholar]
- 18.Dall'Amico R., Ghiggeri G., Carraro M., et al. Prediction and treatment of recurrent focal segmental glomerulosclerosis after renal transplantation in children. American Journal of Kidney Diseases. 1999;34(6):1048–1055. doi: 10.1016/S0272-6386(99)70010-7. [DOI] [PubMed] [Google Scholar]
- 19.Cheong H., II, Han H. W., Park H. W., et al. Early recurrent nephrotic syndrome after renal transplantation in children with focal segmental glomerulosclerosis. Nephrology Dialysis Transplantation. 2000;15(1):78–81. doi: 10.1093/ndt/15.1.78. [DOI] [PubMed] [Google Scholar]
- 20.Kim S. J., Ha J., Jung I. M., et al. Recurrent focal segmental glomerulosclerosis following renal transplantation in Korean pediatric patients. Pediatric Transplantation. 2001;5(2):105–111. doi: 10.1034/j.1399-3046.2001.005002105.x. [DOI] [PubMed] [Google Scholar]
- 21.Fujisawa M., Iijima K., Ishimura T., et al. Long-term outcome of focal segmental glomerulosclerosis after Japanese pediatric renal transplantation. Pediatric Nephrology. 2002;17(3):165–168. doi: 10.1007/s00467-001-0759-0. [DOI] [PubMed] [Google Scholar]
- 22.Crosson J. T. Focal segmental glomerulosclerosis and renal transplantation. Transplantation Proceedings. 2007;39(3):737–743. doi: 10.1016/j.transproceed.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 23.Dantal J., Baatard R., Hourmant M., Cantarovich D., Buzelin F., Soulillou J. P. Recurrent nephrotic syndrome following renal transplantation in patients with focal glomerulosclerosis: a one-center study of plasma exchange effects. Transplantation. 1991;52(5):827–831. doi: 10.1097/00007890-199111000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Baum M. A. Outcomes after renal transplantation for FSGS in children. Pediatric Transplantation. 2004;8(4):329–333. doi: 10.1111/j.1399-3046.2004.00181.x. [DOI] [PubMed] [Google Scholar]
- 25.Nehus E. J., Goebel J. W., Succop P. S., Abraham E. C. Focal segmental glomerulosclerosis in children: multivariate analysis indicates that donor type does not alter recurrence risk. Transplantation. 2013;96(6):550–554. doi: 10.1097/tp.0b013e31829c2431. [DOI] [PubMed] [Google Scholar]
- 26.Stuart F. P. Selection, preparation, and management of kidney transplant recipients. Medical Clinics of North America. 1978;62(6):1381–1397. doi: 10.1016/s0025-7125(16)31742-4. [DOI] [PubMed] [Google Scholar]
- 27.The 13th report of the human renal transplant registry. Transplantation Proceedings. 1977;9(1):9–26. [PubMed] [Google Scholar]
- 28.Odorico J. S., Knechtle S. J., Rayhill S. C., et al. The influence of native nephrectomy on the incidence of recurrent disease following renal transplantation for primary glomerulonephritis. Transplantation. 1996;61(2):228–234. doi: 10.1097/00007890-199601270-00012. [DOI] [PubMed] [Google Scholar]
- 29.Cara Fuentes G. M., Garcia Meseguer C., Pena Carrion A., et al. Long-term outcome of focal segmental glomerulosclerosis after pediatric renal transplantation. Pediatric Nephrology. 2010;25(3):529–534. doi: 10.1007/s00467-009-1361-0. [DOI] [PubMed] [Google Scholar]
- 30.Hwang J. H., Han S. S., Huh W., et al. Outcome of kidney allograft in patients with adulthood-onset focal segmental glomerulosclerosis: comparison with childhood-onset FSGS. Nephrology Dialysis Transplantation. 2012;27(6):2559–2565. doi: 10.1093/ndt/gfr699. [DOI] [PubMed] [Google Scholar]
- 31.Sadowski C. E., Lovric S., Ashraf S., et al. A single-gene cause in 29.5% of cases of steroid-resistant nephrotic syndrome. Journal of the American Society of Nephrology. 2015;26(6):1279–1289. doi: 10.1681/asn.2014050489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Giglio S., Provenzano A., Mazzinghi B., et al. Heterogeneous genetic alterations in sporadic nephrotic syndrome associate with resistance to immunosuppression. Journal of the American Society of Nephrology. 2015;26(1):230–236. doi: 10.1681/ASN.2013111155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Trautmann A., Bodria M., Ozaltin F., et al. Spectrum of steroid-resistant and congenital nephrotic syndrome in children: the podoNet registry cohort. Clinical Journal of the American Society of Nephrology. 2015;10(4):592–600. doi: 10.2215/cjn.06260614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kitamura A., Tsukaguchi H., Iijima K., et al. Genetics and clinical features of 15 Asian families with steroid-resistant nephrotic syndrome. Nephrology Dialysis Transplantation. 2006;21(11):3133–3138. doi: 10.1093/ndt/gfl347. [DOI] [PubMed] [Google Scholar]
- 35.Lee J. H., Han K. H., Lee H., et al. Genetic basis of congenital and infantile nephrotic syndromes. American Journal of Kidney Diseases. 2011;58(6):1042–1043. doi: 10.1053/j.ajkd.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 36.Santín S., Tazón-Vega B., Silva I., et al. Clinical value of NPHS2 analysis in early- and adult-onset steroid-resistant nephrotic syndrome. Clinical Journal of the American Society of Nephrology. 2011;6(2):344–354. doi: 10.2215/cjn.03770410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wada T., Nangaku M. A circulating permeability factor in focal segmental glomerulosclerosis: the hunt continues. Clinical Kidney Journal. 2015;8(6):708–715. doi: 10.1093/ckj/sfv090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weber S., Gribouval O., Esquivel E. L., et al. NPHS2 mutation analysis shows genetic heterogeneity of steroid-resistant nephrotic syndrome and low post-transplant recurrence. Kidney International. 2004;66(2):571–579. doi: 10.1111/j.1523-1755.2004.00776.x. [DOI] [PubMed] [Google Scholar]
- 39.Ulinski T. Recurrence of focal segmental glomerulosclerosis after kidney transplantation: strategies and outcome. Current Opinion in Organ Transplantation. 2010;15(5):628–632. doi: 10.1097/mot.0b013e32833dee3a. [DOI] [PubMed] [Google Scholar]
- 40.Weber S., Tönshoff B. Recurrence of focal-segmental glomerulosclerosis in children after renal transplantation: clinical and genetic aspects. Transplantation. 2005;80(1) supplement:S128–S134. doi: 10.1097/01.tp.0000187110.25512.82. [DOI] [PubMed] [Google Scholar]
- 41.Heeringa S. F., Chernin G., Chaki M., et al. COQ6 mutations in human patients produce nephrotic syndrome with sensorineural deafness. The Journal of Clinical Investigation. 2011;121(5):2013–2024. doi: 10.1172/jci45693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Miyake N., Tsukaguchi H., Koshimizu E., et al. Biallelic mutations in nuclear pore complex subunit NUP107 cause early-childhood-onset steroid-resistant nephrotic syndrome. The American Journal of Human Genetics. 2015;97(4):555–566. doi: 10.1016/j.ajhg.2015.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ding W. Y., Koziell A., McCarthy H. J., et al. Initial steroid sensitivity in children with steroid-resistant nephrotic syndrome predicts post-transplant recurrence. Journal of the American Society of Nephrology. 2015;25(6):1342–1348. doi: 10.1681/ASN.2013080852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fogo A. B. Causes and pathogenesis of focal segmental glomerulosclerosis. Nature Reviews Nephrology. 2015;11(2):76–87. doi: 10.1038/nrneph.2014.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Delville M., Sigdel T. K., Wei C., et al. A circulating antibody panel for pretransplant prediction of FSGS recurrence after kidney transplantation. Science Translational Medicine. 2014;6(256) doi: 10.1126/scitranslmed.3008538.256ra136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Harris J. J., McCarthy H. J., Ni L., et al. Active proteases in nephrotic plasma lead to a podocin-dependent phosphorylation of VASP in podocytes via protease activated receptor-1. The Journal of Pathology. 2013;229(5):660–671. doi: 10.1002/path.4149. [DOI] [PubMed] [Google Scholar]
- 47.Maas R. J., Deegens J. K., Wetzels J. F. Permeability factors in idiopathic nephrotic syndrome: historical perspectives and lessons for the future. Nephrology Dialysis Transplantation. 2014;29(12):2207–2216. doi: 10.1093/ndt/gfu355. [DOI] [PubMed] [Google Scholar]
- 48.Wei C., El Hindi S., Li J., et al. Circulating urokinase receptor as a cause of focal segmental glomerulosclerosis. Nature Medicine. 2011;17(8):952–960. doi: 10.1038/nm.2411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Spinale J. M., Mariani L. H., Kapoor S., et al. A reassessment of soluble urokinase-type plasminogen activator receptor in glomerular disease. Kidney International. 2015;87(3):564–574. doi: 10.1038/ki.2014.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sharma M., Zhou J., Gauchat J.-F., et al. Janus kinase 2/signal transducer and activator of transcription 3 inhibitors attenuate the effect of cardiotrophin-like cytokine factor 1 and human focal segmental glomerulosclerosis serum on glomerular filtration barrier. Translational Research. 2015;166(4):384–398. doi: 10.1016/j.trsl.2015.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Baum M. A., Stablein D. M., Panzarino V. M., Tejani A., Harmon W. E., Alexander S. R. Loss of living donor renal allograft survival advantage in children with focal segmental glomerulosclerosis. Kidney International. 2001;59(1):328–333. doi: 10.1046/j.1523-1755.2001.00494.x. [DOI] [PubMed] [Google Scholar]
- 52.Vinai M., Waber P., Seikaly M. G. Recurrence of focal segmental glomerulosclerosis in renal allograft: an in-depth review. Pediatric Transplantation. 2010;14(3):314–325. doi: 10.1111/j.1399-3046.2009.01261.x. [DOI] [PubMed] [Google Scholar]
- 53.Savin V. J., Sharma R., Sharma M., et al. Circulating factor associated with increased glomerular permeability to albumin in recurrent focal segmental glomerulosclerosis. The New England Journal of Medicine. 1996;334(14):878–883. doi: 10.1056/nejm199604043341402. [DOI] [PubMed] [Google Scholar]
- 54.McCarthy E. T., Sharma M., Savin V. J. Circulating permeability factors in idiopathic nephrotic syndrome and focal segmental glomerulosclerosis. Clinical Journal of the American Society of Nephrology. 2010;5(11):2115–2121. doi: 10.2215/CJN.03800609. [DOI] [PubMed] [Google Scholar]
- 55.Straatmann C., Kallash M., Killackey M., et al. Success with plasmapheresis treatment for recurrent focal segmental glomerulosclerosis in pediatric renal transplant recipients. Pediatric Transplantation. 2014;18(1):29–34. doi: 10.1111/petr.12185. [DOI] [PubMed] [Google Scholar]
- 56.Fencl F., Šimková E., Vondrák K., et al. Recurrence of nephrotic proteinuria in children with focal segmental glomerulosclerosis after renal transplantation treated with plasmapheresis and immunoadsorption: case reports. Transplantation Proceedings. 2007;39(10):3488–3490. doi: 10.1016/j.transproceed.2007.09.045. [DOI] [PubMed] [Google Scholar]
- 57.Fencl F., Vondrak K., Rosik T., et al. Recurrence of nephrotic proteinuria in children with focal segmental glomerulosclerosis—early treatment with plasmapheresis and immunoadsorption should be associated with better prognosis. Minerva Pediatrica. In press. [PubMed] [Google Scholar]
- 58.Canaud G., Dion D., Zuber J., et al. Recurrence of nephrotic syndrome after transplantation in a mixed population of children and adults: course of glomerular lesions and value of the columbia classification of histological variants of focal and segmental glomerulosclerosis (FSGS) Nephrology Dialysis Transplantation. 2010;25(4):1321–1328. doi: 10.1093/ndt/gfp500. [DOI] [PubMed] [Google Scholar]
- 59.Ponticelli C. Recurrence of focal segmental glomerular sclerosis (FSGS) after renal transplantation. Nephrology Dialysis Transplantation. 2010;25(1):25–31. doi: 10.1093/ndt/gfp538. [DOI] [PubMed] [Google Scholar]
- 60.Trachtman R., Sran S. S., Trachtman H. Recurrent focal segmental glomerulosclerosis after kidney transplantation. Pediatric Nephrology. 2015;30(10):1793–1802. doi: 10.1007/s00467-015-3062-1. [DOI] [PubMed] [Google Scholar]
- 61.Araya C. E., Dharnidharka V. R. The factors that may predict response to rituximab therapy in recurrent focal segmental glomerulosclerosis: a systematic review. Journal of Transplantation. 2011;2011:7. doi: 10.1155/2011/374213.374213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cho J.-H., Lee J.-H., Park G.-Y., et al. Successful treatment of recurrent focal segmental glomerulosclerosis with a low dose rituximab in a kidney transplant recipient. Renal Failure. 2014;36(4):623–626. doi: 10.3109/0886022X.2014.882238. [DOI] [PubMed] [Google Scholar]
- 63.Fornoni A., Sageshima J., Wei C., et al. Rituximab targets podocytes in recurrent focal segmental glomerulosclerosis. Science Translational Medicine. 2011;3(85) doi: 10.1126/scitranslmed.3002231.85ra46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mundel P., Reiser J. Proteinuria: an enzymatic disease of the podocyte. Kidney International. 2010;77(7):571–580. doi: 10.1038/ki.2009.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yu C.-C., Fornoni A., Weins A., et al. Abatacept in B7-1-positive proteinuric kidney disease. The New England Journal of Medicine. 2013;369(25):2416–2423. doi: 10.1056/nejmoa1304572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Garin E. H., Reiser J., Cara-Fuentes G., et al. Case series: CTLA4-IgG1 therapy in minimal change disease and focal segmental glomerulosclerosis. Pediatric Nephrology. 2014;30(3):469–477. doi: 10.1007/s00467-014-2957-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rostaing L., Massari P., Garcia V. D., et al. Switching from calcineurin inhibitor-based regimens to a belatacept-based regimen in renal transplant recipients: a randomized phase II study. Clinical Journal of the American Society of Nephrology. 2011;6(2):430–439. doi: 10.2215/cjn.05840710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wéclawiak H., Kamar N., Ould-Mohamed A., Cardeau-Desangles I., Rostaing L. Biological agents in kidney transplantation: belatacept is entering the field. Expert Opinion on Biological Therapy. 2010;10(10):1501–1508. doi: 10.1517/14712598.2010.514901. [DOI] [PubMed] [Google Scholar]
- 69.De Smet E., Rioux J.-P., Ammann H., Déziel C., Quérin S. FSGS permeability factor-associated nephrotic syndrome: remission after oral galactose therapy. Nephrology Dialysis Transplantation. 2009;24(9):2938–2940. doi: 10.1093/ndt/gfp278. [DOI] [PubMed] [Google Scholar]
- 70.Savin V. J., McCarthy E. T., Sharma R., Charba D., Sharma M. Galactose binds to focal segmental glomerulosclerosis permeability factor and inhibits its activity. Translational Research. 2008;151(6):288–292. doi: 10.1016/j.trsl.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 71.Sgambat K., Banks M., Moudgil A. Effect of galactose on glomerular permeability and proteinuria in steroid-resistant nephrotic syndrome. Pediatric Nephrology. 2013;28(11):2131–2135. doi: 10.1007/s00467-013-2539-z. [DOI] [PubMed] [Google Scholar]
- 72.Trachtman H., Savin V. J. Galactose treatment in focal segmental glomerulosclerosis. Pediatric Nephrology. 2014;29(5):p. 931. doi: 10.1007/s00467-013-2700-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Robson K., Hill P., Langsford D., Dwyer K., Goodman D., Langham R. Galactose therapy reduces proteinuria in patients with recurrent focal segmental glomerulosclerosis after kidney transplantation. Nephrology. 2015;20(supplement 1):13–16. doi: 10.1111/nep.12422. [DOI] [PubMed] [Google Scholar]
- 74.Jhaveri K. D., Naber T. H., Wang X., et al. Treatment of recurrent focal segmental glomerular sclerosis posttransplant with a multimodal approach including high-galactose diet and oral galactose supplementation. Transplantation. 2011;91(6):e35–e36. doi: 10.1097/TP.0b013e3182088b67. [DOI] [PubMed] [Google Scholar]
- 75.Leroy S., Guigonis V., Bruckner D., et al. Successful anti-TNFα treatment in a child with posttransplant recurrent focal segmental glomerulosclerosis. American Journal of Transplantation. 2009;9(4):858–861. doi: 10.1111/j.1600-6143.2009.02550.x. [DOI] [PubMed] [Google Scholar]
- 76.Bakr A., Shokeir M., El-Chenawi F., El-Husseni F., Abdel-Rahman A., El-Ashry R. Tumor necrosis factor-alpha production from mononuclear cells in nephrotic syndrome. Pediatric Nephrology. 2003;18(6):516–520. doi: 10.1007/s00467-003-1122-4. [DOI] [PubMed] [Google Scholar]
- 77.Mittal T., Dedhia P., Roy-Chaudhury P., et al. Complete remission of post-transplantation recurrence of focal segmental glomerulosclerosis with the use of adrenocorticotrophic hormone gel: case report. Transplantation Proceedings. 2015;47(7):2219–2222. doi: 10.1016/j.transproceed.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 78.Belingheri M., Lazzari L., Parazzi V., et al. Allogeneic mesenchymal stem cell infusion for the stabilization of focal segmental glomerulosclerosis. Biologicals. 2013;41(6):439–445. doi: 10.1016/j.biologicals.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 79.Vanikar A. V., Trivedi H. L., Shah P. R., et al. Single-center experience on renal transplantation in primary focal and segmental glomerulosclerosis using hematopoietic stem cell transplantation in thymus, bone marrow, portal and peripheral circulation. Saudi Journal of Kidney Diseases and Transplantation. 2013;24(1):15–21. doi: 10.4103/1319-2442.106232. [DOI] [PubMed] [Google Scholar]
- 80.Chikamoto H., Hattori M., Kuroda N., et al. Pretransplantation combined therapy with plasmapheresis and rituximab in a second living-related kidney transplant pediatric recipient with a very high risk for focal segmental glomerulosclerosis recurrence. Pediatric Transplantation. 2012;16(7):E286–E290. doi: 10.1111/j.1399-3046.2011.01610.x. [DOI] [PubMed] [Google Scholar]
- 81.Audard V., Kamar N., Sahali D., et al. Rituximab therapy prevents focal and segmental glomerulosclerosis recurrence after a second renal transplantation. Transplant International. 2012;25(5):e62–e66. doi: 10.1111/j.1432-2277.2012.01462.x. [DOI] [PubMed] [Google Scholar]
- 82.Couloures K., Pepkowitz S. H., Goldfinger D., Kamil E. S., Puliyanda D. P. Preventing recurrence of focal segmental glomerulosclerosis following renal transplantation: a case report. Pediatric Transplantation. 2006;10(8):962–965. doi: 10.1111/j.1399-3046.2006.00571.x. [DOI] [PubMed] [Google Scholar]
- 83.Gohh R. Y., Yango A. F., Morrissey P. E., et al. Preemptive plasmapheresis and recurrence of FSGS in high-risk renal transplant recipients. American Journal of Transplantation. 2005;5(12):2907–2912. doi: 10.1111/j.1600-6143.2005.01112.x. [DOI] [PubMed] [Google Scholar]
- 84.Meyer T. N., Thaiss F., Stahl R. A. K. Immunoadsorbtion and rituximab therapy in a second living-related kidney transplant patient with recurrent focal segmental glomerulosclerosis. Transplant International. 2007;20(12):1066–1071. doi: 10.1111/j.1432-2277.2007.00562.x. [DOI] [PubMed] [Google Scholar]
- 85.Ohta T., Kawaguchi H., Hattori M., et al. Effect of pre- and postoperative plasmapheresis on posttransplant recurrence of focal segmental glomerulosclerosis in children. Transplantation. 2001;71(5):628–633. doi: 10.1097/00007890-200103150-00008. [DOI] [PubMed] [Google Scholar]
- 86.Kasiske B. L., Zeier M. G., Chapman J. R., et al. KDIGO clinical practice guideline for the care of kidney transplant recipients: a summary. Kidney International. 2010;77(4):299–311. doi: 10.1038/ki.2009.377. [DOI] [PubMed] [Google Scholar]