Abstract
Objectives
The aim of this study was to compare the osteogenic effects of demineralized dentin matrix (DDM) combined with recombinant human bone morphogenetic protein-2 (rhBMP-2) in rabbit calvarial defects with DDM and anorganic bovine bone (ABB) combined with rhBMP-2.
Materials and Methods
Four round defects with 8-mm diameters were created in each rabbit calvaria. Each defect was treated with one of the following: 1) DDM, 2) ABB/rhBMP-2, or 3) DDM/rhBMP-2. The rhBMP-2 was combined with DDM and ABB according to a stepwise dry and dip lyophilizing protocol. Histological and microcomputed tomography (µCT) analyses were performed to measure the amount of bone formation and bone volume after 2- and 8-week healing intervals.
Results
Upon histological observation at two weeks, the DDM and ABB/rhBMP-2 groups showed osteoconductive bone formation, while the DDM/rhBMP-2 group showed osteoconductive and osteoinductive bone formation. New bone formation was higher in DDM/rhBMP-2, DDM and ABB decreasing order. The amounts of bone formation were very similar at two weeks; however, at eight weeks, the DDM/rhBMP-2 group showed a two-fold greater amount of bone formation compared to the DDM and ABB/rhBMP-2 groups. The µCT analysis showed markedly increased bone volume in the DDM/rhBMP-2 group at eight weeks compared with that of the DDM group. Notably, there was a slight decrease in bone volume in the ABB/rhBMP-2 group at eight weeks. There were no significant differences among the DDM, ABB/rhBMP-2, and DDM/rhBMP-2 groups at two or eight weeks.
Conclusion
Within the limitations of this study, DDM appears to be a suitable carrier for rhBMP-2 in orthotopic sites.
Keywords: Demineralized dentin matrix, Recombinant human bone morphogenetic protein-2, Microcomputed tomography, Histomorphometric analysis
I. Introduction
Although recombinant human bone morphogenetic protein-2 (rhBMP-2), which is a potent osteoinductor, has long been considered a promising avenue for bone regeneration, and rhBMP-2 has been commercially available for the treatment of oral-maxillofacial defects, the issue of the carrier system is an ongoing topic that has not yet been solved. Like other growth factors, rhBMP-2 requires a delivery system that creates optimal conditions for cellular and vascular growth, cellular attachment, and release kinetics1,2,3,4.
Calcium phosphates, such as hydroxyapatite (HA) and β-tricalcium phosphate (β-TCP), have been deemed to be suitable candidates for rhBMP-2 delivery systems because of their space-providing properties. Biphasic calcium phosphate (BCP) in particular, which is a specific ratio of HA and β-TCP, has well-documented osteoconductive properties5.
However, for the commercially available rhBMP-2 in the maxillofacial region, the only approved carrier is absorbable collagen sponges (ACSs). Several studies have supported this carrier system6,7. Triplett et al.8 reported the results of multicenter randomized clinical trials of rhBMP-2/ACS application for sinus floor elevation and showed that its efficacy and safety were comparable to those of an autogenous bone graft.
On the other hand, a report9 in 1998 suggested that root dentin prepared from extracted teeth could be recycled for use as a carrier of rhBMP-2 because it induces new bone formation in the periodontium, while a later report10 in 2005 showed that the osteoinductive matrices of human demineralized dentin matrix (DDM) particles could be effective as a carrier of rhBMP-2 for bone engineering. Since then, DDM powder has shown great potential as an effective carrier for rhBMP-2 based on in vitro and in vivo studies in 2014 and 201511,12. To date, ectopic bone formation in vivo has demonstrated the possibility of DDM as a suitable carrier for rhBMP-2. Because DDM is composed of mainly type I collagen and HA, it might be more advantageous than ACSs in alveolar bone repair due to its structural integrity11.
The aim of this study is to investigate DDM as a suitable carrier for rhBMP-2 in order to establish efficient and safe approaches for bone regeneration in rabbit calvarial defects. The first objective was to investigate whether the potential bone forming capacity of DDM/rhBMP-2 was greater than that of DDM, as measured using osteoinductivity and osteoconductivity. The second objective was to evaluate whether DDM has greater potential as an rhBMP-2 carrier than does anorganic bovine bone (ABB).
II. Materials and Methods
The rhBMP-2 was provided by the Research and Development Institute of Cowellmedi (Busan, Korea). Two types of scaffolds were selected as carriers of rhBMP-2; AutoBT (human DDM; Korea Tooth Bank, Seoul, Korea) and ABB (Geistlich, Seoul, Korea). DDM and ABB were combined with rhBMP-2 to form DDM/rhBMP-2 (n=12) and ABB/rhBMP-2 (n=12), respectively.
1. Preparations of DDM
An extracted human tooth was soaked in 70% ethyl alcohol and cleaned by removing foreign substances such as restoration materials, root canals, and prosthetics, as well as soft tissues of the periodontium, pulp, and caries. After the cleaned tooth was divided into crown and root, the root portion was collected and prepared for partially DDM as reported previously. Next, 0.3- to 0.8-mm crushed particles were soaked in a distilled water and hydrogen dioxide solution, and the remaining foreign substances were removed by ultrasonic cleaning. The cleaned particles were dehydrated with ethyl alcohol and defatted with an ethyl ether solution. The particles were then decalcified for two hours in 0.6 N HCl11.
2. Preparation of ABB combined with rhBMP-2 and DDM combined with rhBMP-2
ABB and DDM were combined with rhBMP-2 by the dipdry method. Briefly, 0.01 mg of rhBMP-2 (CowellBMP; Cowellmedi) were added to 1 g of ABB particles, frozen in a deep freezer at –70℃ and then fixed in a lyophilizer (ILShin Lab, Seoul, Korea) following the manufacturer's instructions. Alternatively, 2 mg/mL of rhBMP-2 (CowellBMP) were fixed to 0.03 g of DDM by a stepwise dip and dry lyophilizing protocol11,12,13.
3. Surgical procedures
Twelve male rabbits (body weight, 2.50-3.00 kg) were used in this study and were maintained in cages at an ambient room temperature of 21℃ with ad libitum access to water and a standard laboratory pellet diet. Animal selection and management, surgical protocol, and preparation followed routines approved by the Institutional Animal Care and Use Committee (BA1303-124-016-03). The animals were anesthetized with an intramuscular injection (5 mg/kg body weight) of a 4:1 solution of ketamine hydrochloride (Ketalar; Yuhan Co., Seoul, Korea) and xylazine (Rompun; Bayer Korea, Seoul, Korea). The surgical site was shaved and scrubbed with iodine. For the calvarial defect model, an incision was made in the sagittal plane across the cranium, and a full-thickness flap was reflected to expose the calvarial bone. Standardized circular transosseous defects 8 mm in diameter were created on the cranium using a trephine drill (3i Implant Innovations Inc., Palm Beach Gardens, FL, USA) and copious saline irrigation. In total, four round defects with 8 mm diameters were created in each rabbit calvaria. Respective groups received the following treatments: 1) DDM control (0.03 g), 2) ABB/rhBMP-2 (1.0 g), and 3) DDM/rhBMP-2 (0.03 g). All surgical sites underwent primary closure using 4-0 Monosyn (glyconate absorbable monofilament; B. Braun, Aesculap, PA, USA). The animals were sacrificed at two and eight weeks after implantation for radiologic and histologic evaluation. (Fig. 1)
Fig. 1. A. Microcomputed tomography image of an en bloc rabbit calvarial defect. Top left: DDM, top right: DDM, bottom left: ABB/rhBMP-2, bottom right: DDM/rhBMP-2. B. Histologic specimen of DDM at two weeks (H&E staining, ×100). Note the defect border, where DDM particles were grafted. (DDM: demineralized dentin matrix, ABB: anorganic bovine bone, rhBMP-2: recombinant human bone morphogenetic protein-2).
4. Histomorphometric analysis
For histological analysis, the specimens were procured en bloc and fixed in 10% buffered formalin for 10 days, decalcified in 10% formic acid for 14 days, and then embedded in paraffin. From serial sections of 5 µm thickness through the centers of the circular calvarial defects, two sections that contained each central portion were selected and stained with H&E.(Fig. 1. B) For histomorphometric analysis, the specimens were observed though an optical microscope at 100 × magnification. The digital images were obtained using a digital camera attached to the microscope, and the bone ratio of the area of newly formed bone (%) to total calvarial defect area was determined using an image analysis program (Kappa ImageBase Metreo; Kappa Optronics GmbH, Gleichen, Germany).(Fig. 1. B)
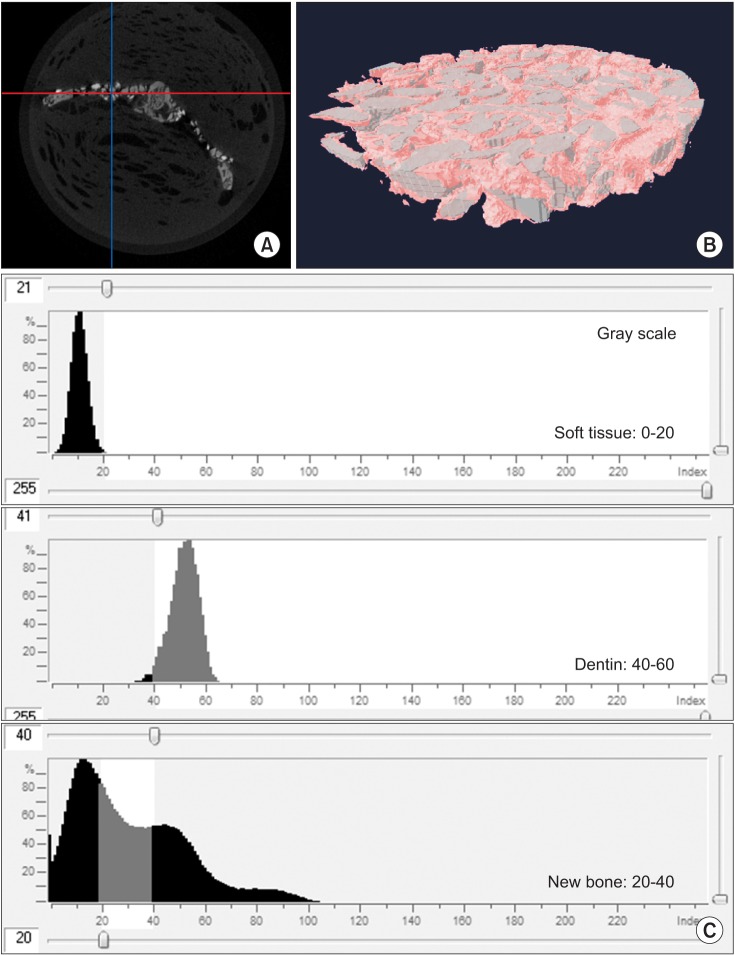
5. Microcomputed tomography (µCT) analysis
Calvarial en bloc specimens were fixed in 10% buffered formalin solution for imaging. The images were produced using a SkyScan 1172 CT system (Bruker microCT, Kontich, Belgium) in a high-resolution scanning mode (pixel matrix, 683×2,000×1,048; pixel size, 10.89 µm). The X-ray source was set at 70 kV and 141 mA for shooting with the aid of a 0.5-mm thick aluminum filter to optimize the contrast. The 360° rotational angle of specimens was set at 0.5° and 590 ms of exposure time.(Fig. 2. A) Three-dimensional images were produced using a CT reconstruction program (NRecon; Bruker microCT), and the bone volume (BV) per tissue volume (TV) was obtained using a reconstructed image analysis program (CTAn, dataviewer; Bruker microCT).
Fig. 2. A. Microcomputed tomography image of calvarial defect, cross section at two weeks after demineralized dentin matrix (DDM) implantation. B. Three-dimensional reconstruction of grafted area as volume of interest (8×1 mm) in the form of a disk from the red line (in Fig. 2. A). C. Quantification of new bone volume at two weeks after DDM implantation using NRecon reconstruction software (NRecon v.1.4.4; SkyScan).
To determine new BV (NBV), the differences in brightness in the images were used. The BV and DDM volume were calculated within the range of the volume of interest (8×1 mm) in the form of a disk inside the skull defect, and this difference was calculated as the NBV ratio.(Fig. 2. B)
To discriminate new bons from graft materials, images of graft materials were produced separately, and Hounsfield units (HU) were calculated to analyze the range of HU values. The HU values considered new bone were set based on a value range of D3 bone of 20-40.(Fig. 2. C) Mean and standard deviation were calculated for all histomorphometric and µCT measurements. Comparative statistics of nonparametric variables were compared using the Mann-Whitney U-test, with P<0.05 used as the threshold of significance. All data analysis was completed using the GraphPad Prism 5.0 (GraphPad Software, San Diego, CA, USA).
III. Results
1. Histological findings
1) DDM at two weeks
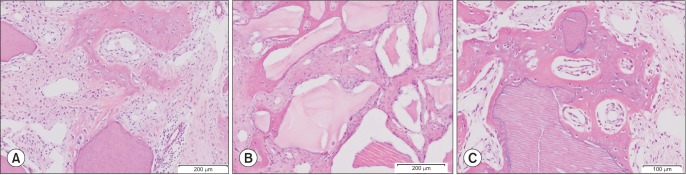
New bone was formed and migrated from the bone defect margin that has abundant osteocytes and blood vessels. All of the fibroblasts around the scaffold and new osteoids were stimulated and transformed phenotypically into osteoblast-like cells. Subsequently, the newly formed bone from the bone defect margin created bridges.(Fig. 3. A)
Fig. 3. A. DDM at two weeks (H&E staining, ×100). New bone was formed and migrated from the bone defect margin that has abundant osteocytes and blood vessels. All of the fibroblasts around the scaffold and new osteoids were stimulated and transformed phenotypically into osteoblast-like cells. B. ABB/rhBMP-2 at two weeks (H&E staining, ×100). New bone was formed and migrated from the bone defect margin to the surface of the ABB scaffold. The cells around the ABB were stabilized, and spaces were filled with dense fibrous connective tissues. C. DDM/rhBMP-2 at two weeks (H&E staining, ×200). Osteoinductive deposits of osteoids are evident, as is the phenotypic transformation of osteoblast-like cells on the surfaces of the osteoids. There was abundant vascular proliferation as evidence of the remodeling capacity in the newly deposited osteoids on the surface of DDM/rhBMP-2. (DDM: demineralized dentin matrix, ABB: anorganic bovine bone, rhBMP-2: recombinant human bone morphogenetic protein-2).
2) ABB/rhBMP-2 at two weeks
New bone was formed and migrated from the bone defect margin to the surface of the ABB scaffold. The cells around the ABB were stabilized, and spaces were filled with dense, fibrous connective tissues.(Fig. 3. B)
3) DDM/rhBMP-2 at two weeks
The newly formed bone around the DDM had very similar cellular and vascular activities to the bone that was formed and migrated from the defect bone margin.(Fig. 3. A) There were osteoinductive deposits of osteoids as well as phenotypic transformation of osteoblast-like cells on the surfaces of the osteoids. There was also abundant vascular proliferation, which provided evidence of the remodeling capacity in the newly deposited osteoids on the surface of DDM/rhBMP-2. (Fig. 3. C)
2. Histomorphometric findings of new bone formation
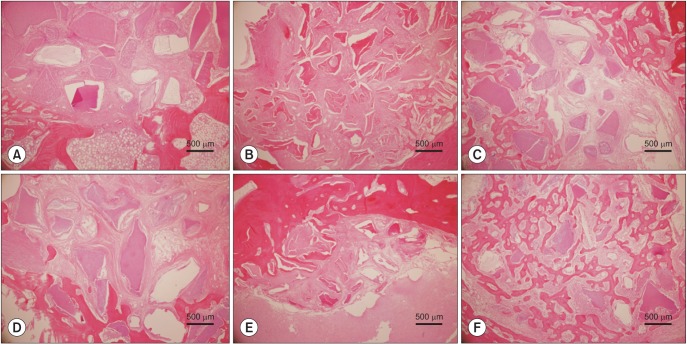
The implantation of the scaffolds combined with rhBMP-2 showed significantly increased bone formation during the period from two weeks to eight weeks. There were no statistically significant differences with P<0.05 using the Mann-Whitney U-test.(Table 1, Fig. 4)
Table 1. Histomorphometric measurements of NBA.
| Healing interval | NBA (%)1 | ||
|---|---|---|---|
| DDM (n=12) |
ABB/rhBMP-2 (n=12) |
DDM/rhBMP-2 (n=12) |
|
| 2 wk (n=6) | 28.38±5.66 | 25.15±5.10 | 35.03±8.93 |
| 8 wk (n=6) | 50.25±7.36 | 52.46±8.69 | 85.12±11.08 |
(NBA: new bone area, DDM: demineralized dentin matrix, ABB: anorganic bovine bone, rhBMP-2: recombinant human bone morphogenetic protein-2, TDA: total defect area)
1NBA (%)=NBA/TDA×100
Values are presented as mean±standard deviation.
Fig. 4. Histomorphometric measurement of new bone formation at two and eight weeks (H&E staining, ×100). A. DDM at two weeks. B. ABB/rhBMP-2 at two weeks. C. DDM/rhBMP-2 at two weeks. D. DDM at eight weeks. E. ABB/rhBMP-2 at eight weeks. F. DDM/rhBMP-2 at eight weeks. The implantation of scaffolds loaded with rhBMP-2 (DDM and ABB) showed significantly increased new bone formation during the period from two to eight weeks. There were no statistically significant differences at P<0.05. (DDM: demineralized dentin matrix, ABB: anorganic bovine bone, rhBMP-2: recombinant human bone morphogenetic protein-2).
1) DDM
After two weeks, minimal amounts of new bone had formed from the bone defect margins toward the central portion. Most of the area in a given defect was filled with fibrous connective tissue. At eight weeks, the bone formation and maturation had increased to a greater extent compared with that in the two-week specimens. New bone growth was observed both from the margins and around the DDM scaffold. (Table 1, Fig. 4)
2) ABB/rhBMP-2
At two weeks, new bone was seen at the periphery of the defect margin and around the ABB particles. The immature bone tissue was not only interconnected between particles, but also partially encircled the ABB particles. At eight weeks, resorption of the ABB was not observed, and bone formation was increased compared with the two-week specimens. The bony tissues around the particles were progressively interconnected.(Table 1, Fig. 4)
3) DDM/rhBMP-2
At two weeks, the amount of new bone formation was very similar to those of the DDM and ABB/rhBMP-2 groups, and it was mainly formed and migrated from the defect margin. The newly formed bone had been deposited directly onto the DDM/rhBMP-2 surface; osteocytes were visible in the lacunae, and osteoblasts were lined up along the bony trabeculae. At eight weeks, new bone was extending remarkably to form an anastomosing network of trabeculae between the DDM/rhBMP-2 particles.(Table 1, Fig. 4)
3. New bone formation measured by µCT
The increased BV was remarkable from two to eight weeks in DDM/rhBMP-2, increasing by 87.14% compared to those of the DDM (+27.5%) and ABB/rhBMP-2 (–17.9%) groups, which showed similar or decreased amounts of BV from two to eight weeks. The results demonstrated that NBV had increased in the DDM and DDM/rhBMP-2 groups by the end of eight weeks, compared with a decrease in NBV in the ABB/rhBMP-2 group. There were no statistically significant differences among the groups with P<0.05 using the Mann-Whitney U-test.(Table 2, Fig. 5)
Table 2. NBV measured by mircocomputed tomography.
| Healing interval | NBA (%)1 | ||
|---|---|---|---|
| DDM (n=12) |
ABB/rhBMP-2 (n=12) |
DDM/rhBMP-2 (n=12) |
|
| 2 wk (n=6) | 25.80±5.01 | 31.50±9.60 | 20.77±11.59 |
| 8 wk (n=6) | 32.90±13.34 | 25.87±12.67 | 38.87±10.21 |
(NBV: new bone volume, DDM: demineralized dentin matrix, ABB: anorganic bovine bone, rhBMP-2: recombinant human bone morphogenetic protein-2, BV: bone volume, TV: tissue volume)
1NBV (%)=BV/TV×100
Values are presented as mean±standard deviation.
Fig. 5. New bone volume measured by microcomputed tomography. New bone volume increased in DDM (27.5%) and DDM/rhBMP-2 (87.14%) from two to eight weeks compared with the decreased new bone volume in ABB/rhBMP-2 (–17.9%). Values are presented as mean±standard deviation. No statistically significant differences were found among the groups. (DDM: demineralized dentin matrix, ABB: anorganic bovine bone, rhBMP-2: recombinant human bone morphogenetic protein-2).
IV. Discussion
The aim of this study was to evaluate the bone forming capacity of DDM loaded with rhBMP-2 in an orthoskeletal site. The first objective was to establish that the potential bone forming capacity of DDM/rhBMP-2 was greater than that of DDM alone, similar to osteoinductivity and osteoconductivity. The second objective was to determine whether DDM has greater potential for application with rhBMP-2 than does ABB. The results of this study demonstrated that the DDM group showed slightly increased BV from two to eight weeks, while the DDM/rhBMP-2 group showed markedly increased BV over the same time. In contrast, the ABB/rhBMP-2 group showed decreased BV at eight weeks compared with the earlier stage. The results of this study imply that, even if the effects of the bone forming capacity at earlier stages were very similar among the DDM, ABB/rhBMP-2, and DDM/rhBMP-2 groups, the effects at later stages demonstrated that DDM was a more suitable rhBMP-2 carrier in terms of bone forming capacity and incorporation compared with DDM/rhBMP-2 and ABB/rhBMP-2.
Although rhBMP-2 was approved by the U.S. Food and Drug Administration in 2007 for use in sinus floor augmentation and extraction socket preservation, further studies including the development of a suitable carrier for BMP are required to generate efficient and safe approaches for bone regeneration using BMPs, and the importance of the carrier for predictable bone formation must not be underestimated4.
Despite numerous materials having been evaluated as rhBMP-2 carriers, including ceramics (HA, TCP, BCP, calcium sulfate), silicate glass, allografts, and demineralized bone matrix, ACS is the only carrier approved for use with rhBMP-2. The reason for the lack of approval is that, while these materials possess some of the required properties for rhBMP-2 carriers, they do not meet all of the necessary performance requirements14. In contrast, ACS has high binding and retention capacities for rhBMP-2 and thus is effective in incorporating and delivering rhBMP-2 to surgical sites15. In addition, ACS gradually releases rhBMP-2 at the implantation site, allowing new bone formation to occur. ACS is fully resorbed over 4 to 10 weeks, and the localized release of rhBMP-2 occurs over two weeks. This slow release and rapid clearance result in minimal systemic exposure, with a half-life of 7 to 16 minutes in the blood stream16 with regard to alternative carriers, many authors have reported that a fibrin matrix is an excellent carrier for BMP-2, and that it provides equivalent results at a seven-fold lower dose of BMP-2 compared with that required with ACS17. However, others have reported that the bone regenerated by collagen with BMP-2 had a higher bone density than the bone regenerated by fibrin with BMP-218. Furthermore, an ABB block with high porosity did not show increased bone formation with the additional use of rhBMP-219. The results of these studies showed that use of the carrier BMP-2 is an important factor affecting the quality of engineered bone.
It was known that collagen is the most documented carrier for rhBMP-2, but it is not osteoconductive and is not well suited for onlay augmentation owing to its poor structural integrity in orthotopic sites. However, DDM has excellent structural integrity and mechanical properties with its HA, type I collagens, and additional dentin matrix proteins20. In addition to the type I collagens present in sponges, the innate dentinal tubules sized 1 to 3 µm in diameter, which can accommodate BMP solution and increase the contact area with proteins, provided microporous spaces to play a major role for the continuous binding of rhBMP-2 to DDM and its release20,21
Before the development and clinical application of human DDM in implant dentistry in 2010, the potential use of DDM as an rhBMP-2 carrier had been reported. Although endogenous BMP has been found in large quantities in dentin in normal young adult mammals, dentin matrix seems not to have been evaluated as a carrier of exogenous BMP until 2 mg of exogenous rhBMP-2 adsorbed to a pulverized root partially DDM was shown to be as osteoinductive as autogeneic bone in 19989,21. Thus, whether or not a large periodontal alveolar bone defect can be repaired using composites of rhBMP-2 and DDM warrants special investigation.
Recent studies have provided evidence that addition of rhBMP-2 to DDM accelerates its osteoinductivity, and that DDM might be effective as a carrier of BMP-2 for bone engineering. These studies showed that DDM/rhBMP-2 induced bone and cartilage, and that the DDM was gradually replaced by new bone, and demonstrated that the DDM/rhBMP-2 showed 79% in the volume of bone marrow, and 21.0% in that of DDM at 32 weeks10,22.
To evaluate DDM (AutoBT; Korea Tooth Bank) as an rhBMP-2 carrier, a time-course kinetic release study of rhBMP-2 from AutoBT in rats has been reported. A statistically significantly large amount of rhBMP-2 was released from AutoBT compared to that released from TCP (P<0.05) up to five weeks after implantation. In addition, the expression of osteonectin and bone formation of AutoBT were superior to those of the TCP. Therefore, the results suggest that DDM is an effective carrier of rhBMP-211,12.
Based on previous studies, the efficacy of DDM/rhBMP-2 in critically sized calvarial defects of rabbit could be interpreted as follows. Through histological evaluation at two weeks, osteoconductive bone formation was observed in the DDM and ABB/rhBMP-2 groups, whereas both osteoinductive and osteoconductive bone formation were observed in the DDM/rhBMP-2 group.(Fig. 3) The areas of increased bone formation as analyzed by histomorphometry from two to eight weeks were 21.87%, 27.31%, and 50.09%, respectively, for the DDM, ABB/rhBMP-2 and DDM/rhBMP-2 groups.(Table 1, Fig. 4) In contrast, µCT measurements revealed markedly increased BV in the DDM/rhBMP-2 group (increased by 87.14%) compared with those of DDM (+27.5%) and ABB/rhBMP-2 (–17.9%), although the differences were not statistically significant.
The remarkable increase in BV in the DDM/rhBMP-2 group compared with that in the DDM group might be due to the binding capacity and slow time-release kinetics related to the collagenous nature and innate microporous structures of the dentinal tubules in DDM. The gradual resorption of DDM, as described in incorporation, also seemed to play a major role in the increased osteoinductive potential of DDM due to addition of rhBMP-210,11,12,22.
In particular, the 17.9% decrease in BV in the ABB/rhBMP-2 group could be explained by the fact that ABB did not meet the requirements such as incorporation rate or cohesiveness, which were closely related at later remodeling stages.
The results demonstrated that NBV had increased in the DDM and DDM/rhBMP-2 groups by the end of eight weeks compared with the decreased NBV in the ABB/rhBMP-2 group. However, there were no significant statistical differences among the groups at that time14.(Table 2, Fig. 5)
V. Conclusion
Within the limitations of this study, it can be suggested that DDM/rhBMP-2 enhances bone formation more than DDM alone or ABB/rhBMP-2. In addition, DDM as a carrier of rhBMP-2 can be used successfully for alveolar bone repair. In the context of the limited dose dependency of rhBMP-2, a study to define the threshold dose is essential for minimizing adverse systemic effects.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Govender S, Csimma C, Genant HK, Valentin-Opran A, Amit Y, Arbel R, et al. Recombinant human bone morphogenetic protein-2 for treatment of open tibial fractures: a prospective, controlled, randomized study of four hundred and fifty patients. J Bone Joint Surg Am. 2002;84:2123–2134. doi: 10.2106/00004623-200212000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Burkus JK, Heim SE, Gornet MF, Zdeblick TA. Is INFUSE bone graft superior to autograft bone? An integrated analysis of clinical trials using the LT-Cage lumbar tapered fusion device. J Spinal Disord Tech. 2003;16:113–122. doi: 10.1097/00024720-200304000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Ripamonti U, Reddi AH. Periodontal regeneration: potential role of bone morphogenetic proteins. J Periodontal Res. 1994;29:225–235. doi: 10.1111/j.1600-0765.1994.tb01216.x. [DOI] [PubMed] [Google Scholar]
- 4.Asahina I. Bone morphogenetic proteins: their history and characteristics. J Hard Tissue Biol. 2014;23:283–286. [Google Scholar]
- 5.Gauthier O, Bouler JM, Aguado E, Pilet P, Daculsi G, Macroporous Biphasic calcium phosphate ceramics: influence of macropore diameter and macroporosity percentage on bone ingrowth. Biomaterials. 1998;19:133–139. doi: 10.1016/s0142-9612(97)00180-4. [DOI] [PubMed] [Google Scholar]
- 6.Kim CS, Kim JI, Kim J, Choi SH, Chai JK, Kim CK, et al. Ectopic bone formation associated with recombinant human bone morphogenetic proteins-2 using absorbable collagen sponge and beta tricalcium phosphate as carriers. Biomaterials. 2005;26:2501–2507. doi: 10.1016/j.biomaterials.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 7.Hyun SJ, Han DK, Choi SH, Chai JK, Cho KS, Kim CK, et al. Effect of recombinant human bone morphogenetic protein-2, -4, and -7 on bone formation in rat calvarial defects. J Periodontol. 2005;76:1667–1674. doi: 10.1902/jop.2005.76.10.1667. [DOI] [PubMed] [Google Scholar]
- 8.Triplett RG, Nevins M, Marx RE, Spagnoli DB, Oates TW, Moy PK, et al. Pivotal randomized, parallel evaluation of recombinant human bone morphogenetic protein-2/absorbable collagen sponge and autogenous bone graft for maxillary sinus floor augmentation. J Oral Maxillofac Surg. 2009;67:1947–1960. doi: 10.1016/j.joms.2009.04.085. [DOI] [PubMed] [Google Scholar]
- 9.Ike M, Urist MR. Recycled dentin root matrix for a carrier of recombinant human bone morphogenetic protein. J Oral Implantol. 1998;24:124–132. doi: 10.1563/1548-1336(1998)024<0124:RDRMFA>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Murata M. Bone engineering using human demineralixed dentin matrix and recombinant human BMP-2. J Hard Tissue Biol. 2005;14:80–81. [Google Scholar]
- 11.Kim YK, Um IW, An HJ, Kim KW, Hong KS, Murata M. Effects of demineralized dentin matrix used as an rhBMP-2 carrier for bone regeneration. J Hard Tissue Biol. 2014;23:415–422. [Google Scholar]
- 12.Kim YK, Kwon KH, Lee ES, Kim CH, Kim MY, Um IW. Experimental study on human demineralized dentin matrix as rhBMP-2 carrier in vivo. J Dent App. 2015;2:269–273. [Google Scholar]
- 13.Jung JH, Yun JH, Um YJ, Jung UW, Kim CS, Choi SH, et al. Bone formation of Escherichia coli expressed rhBMP-2 on absorbable collagen block in rat calvarial defects. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:298–305. doi: 10.1016/j.tripleo.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 14.Geiger M, Li RH, Friess W. Collagen sponges for bone regeneration with rhBMP-2. Adv Drug Deliv Rev. 2003;55:1613–1629. doi: 10.1016/j.addr.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 15.Fiorellini JP, Howell TH, Cochran D, Malmquist J, Lilly LC, Spagnoli D, et al. Randomized study evaluating recombinant human bone morphogenetic protein-2 for extraction socket augmentation. J Periodontol. 2005;76:605–613. doi: 10.1902/jop.2005.76.4.605. [DOI] [PubMed] [Google Scholar]
- 16.McKay WF, Peckham SM, Marotta JS. The science of rhBMP-2. St. Louis: Quality Medical Publishing; 2006. [Google Scholar]
- 17.Schützenberger S, Schultz A, Hausner T, Hopf R, Zanoni G, Morton T, et al. The optimal carrier for BMP-2: a comparison of collagen versus fibrin matrix. Arch Orthop Trauma Surg. 2012;132:1363–1370. doi: 10.1007/s00402-012-1551-2. [DOI] [PubMed] [Google Scholar]
- 18.Jung SY, KO YJ, Jang HS, Kang SW, Park JH. The effect of carrier for BMP-2 delivery on histological aspects of tissue-engineered bone. Tissue Eng Regen Med. 2013;10:341–346. [Google Scholar]
- 19.Schmitt C, Lutz R, Doering H, Lell M, Ratky J, Schlegel KA. Bio-Oss block combined with BMP-2 and VEGF for the regeneration of bony defects and vertical augmentation. Clin Oral Implants Res. 2013;24:450–460. doi: 10.1111/j.1600-0501.2011.02351.x. [DOI] [PubMed] [Google Scholar]
- 20.Kim YK, Um IW, Murata M. Tooth bank system for bone regeneration: safety report. J Hard Tissue Biol. 2014;23:371–376. [Google Scholar]
- 21.Kim YK, Kim SG, Byeon JH, Lee HJ, UM IU, Lim SC, et al. Development of a novel bone grafting material using autogenous teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:496–503. doi: 10.1016/j.tripleo.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 22.Murata M, Kawai T, Kawakami T, Akazawa T, Tazaki J, Ito K, et al. Human acid-insoluble dentin with BMP-2 accelerates bone induction in subcutaneous and intramuscular tissues. J Ceram Soc Jpn. 2010;118:438–441. [Google Scholar]