Abstract
The proliferation of vaporization (‘vaping’) as a method for administering cannabis raises many of the same public health issues being debated and investigated in relation to e-cigarettes (e-cigs). Good epidemiological data on the prevalence of vaping cannabis are not yet available, but with current trends towards societal approval of medicinal and recreational use of cannabis, the pros and cons of vaping cannabis warrant study. As with e-cigs, vaping cannabis portends putative health benefits by reducing harm from ingesting toxic smoke. Indeed, vaping is perceived and being sold as a safer way to use cannabis, despite the lack of data on the health effects of chronic vaping. Other perceived benefits include better taste, more efficient and intense effects and greater discretion which allows for use in more places. Unfortunately, these aspects of vaping could prompt an increased likelihood of trying cannabis, earlier age of onset, more positive initial experiences, and more frequent use, thereby increasing the probability of problematic use or addiction. Sales and marketing of vaping devices with no regulatory guidelines, especially related to advertising or product development targeting youth, parallels concerns under debate related to e-cigs and youth. Thus, the quandary of whether or not to promote vaping as a safer method of cannabis administration for those wishing to use cannabis, and how to regulate vaping and vaping devices, necessitates substantial investigation and discussion. Addressing these issues in concert with efforts directed towards e-cigs may save time and energy and result in a more comprehensive and effective public health policy on vaping.
Keywords: Cannabis, vaporization, e-cigarettes, vaping, marijuana, policy
INTRODUCTION
A quick PubMed search reveals multiple editorials and many studies highlighting the controversies and concerns related to electronic cigarette (e-cig) use, particularly in the context of tobacco regulation policy and impact on youth [1–6]. The crux of the dilemma pits potential harm reduction benefits of e-cigs (i.e. vaporizing nicotine can reduce smoking-related respiratory illnesses and mortality, and potential for use as a quit smoking aid) against unknown potential harms (i.e. health impact of long-term inhalation of aerosol, inadvertent impact on increasing or maintaining use of nicotine or tobacco and intentional or unintentional promotion of a pathway to tobacco smoking for youth). For those attending to the changing landscape of marijuana (cannabis) use, strikingly similar apprehensions related to the proliferation of the vaporization (vaping) of cannabis products jump off the page. The scientific and regulatory communities, however, have been slow to connect these issues; the mention of vaping devices designed for cannabis or the potential to use cannabis products in an e-cig device rarely receives more than a sentence or two in the discussion of e-cigs.
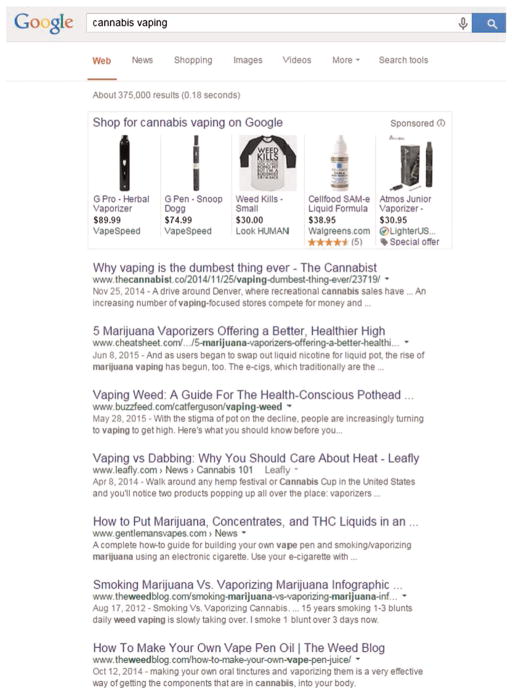
For those less familiar, ‘vaping’ is the slang term for the vaporization of substances (e.g. flavors, nicotine or cannabis products) whereby liquid, oil or plant material is heated to a temperature that releases an aerosolized mixture of water vapor and active ingredients [e.g. nicotine in e-cigs and tetrahydrocannabinol (THC) or cannabidol for cannabis], which is then inhaled. This method of administration avoids combustion of the substance and the inhaling of smoke, which contains carbon monoxide and other by-products of combustion. Vaping, whether of nicotine, cannabis or other substances, has risen in popularity, such that the Oxford Dictionary designated ‘vape’ the word of the year in 2014. One can glean a sense of the emergence and magnitude of vaping cannabis products in current-day culture by typing ‘cannabis vape’ or ‘cannabis vaping’ into an internet search engine and viewing a plethora of information, promotional advertisements and instructional videos (Fig. 1). Good epidemiological data on the prevalence of vaping cannabis are not yet available, but concerns about cannabis vaping would surely be warranted if its proliferation parallels what has been observed with e-cigs among youth and adults globally [7]. More than 450 brands of e-cigs are available world-wide, and an estimated 3 billion dollars were spent on e-cigs globally in 2013. Among US high school students, from 2011 to 2014 a ninefold increase in e-cig use (1.5–13.4%) was reported, with a similar increase observed in middle school students, and e-cigs emerged as the most common method for using ‘tobacco’ in both age groups [8].
Figure 1.
Screenshot of a search for cannabis vape on Google. Available at: https://www.google.com/?gws_rd=ssl#q=cannabis+vape (accessed 23 June 2015)
With current legislation and regulatory shifts trending towards societal approval of recreational and medicinal use of cannabis in the United States and other countries [9,10], the pros and cons of vaping cannabis warrant careful investigation. Here we seek to heighten awareness, understanding and discussion that might prompt scientific, regulatory and public examination of this emerging method of using cannabis.
THEORETICAL BENEFITS OF VAPING
Little enough is known about the health benefits of e-cig use, but almost nothing is known about health benefits that might accrue from vaping cannabis. As with e-cigs, vaping cannabis may reduce negative health effects associated with inhalation of cannabis smoke by delivering desired cannabinoid compounds more efficiently and with fewer carcinogenic by-products. Vaping cannabis reduces the ingestion of smoke-related toxins and carcinogens such as carbon monoxide, tar, ammonia and hydrogen cyanide that are typically inhaled when smoking cannabis [11–13], and cannabis users perceive vaping to be safer or less harmful to their health compared to combustible smoking methods [14,15]. Indeed, cannabis users report having more respiratory problems than non-users [16], and replacing smoking with vaping is likely to reduce this known harm. Vaping cannabis has been associated with fewer reports of respiratory symptoms [17], but there have been no clinical trials that experimentally assigned vaping to a sample of cannabis smokers.
Another theoretical advantage of vaping is limiting the exposure of others to cannabis smoke. Even less is known about the health impact of second-hand cannabis smoke, but this will become an issue in countries and US states where use is legal and becomes common in public places. Limiting the exposure of others to second-hand smoke may be particularly salient to those seeking to use cannabis for medical conditions, where delivering a desired dose more efficiently and with less exposure to non-using family members is desired [18]. Just as governing bodies currently have to examine how smoke-free laws apply to e-cig users, they will now have to examine how these laws apply to those who smoke or vape cannabis.
Those who vape cannabis identify non-health benefits of this practice as well [14,15], indicating that it tastes better than smoking, is more discreet (no smell), with some feeling that they gain more of the desired positive effects from using less cannabis (increased delivery efficiency). This suggests that vaping may afford a more pleasurable experience that can be enjoyed in more places without disturbing others, and for lower cost. The question is how these attributes, along with the perception of vaping as a safe or healthy method for using cannabis, will impact upon frequency and quantity of cannabis use and the likelihood of trying it among non-users—especially adolescents. For us, these queries raise important concerns.
POTENTIAL DOWNSIDE OF VAPING
When discussing e-cigs, the term ‘double-edged sword’ frequently appears when weighing the benefits and risks. Vaping cannabis affords a similar quandary and trepidations. Multiple studies indicate that reductions in perceived risk of harm may lead to earlier initiation of use of many types of substances (including cannabis), increased frequency or quantity of use and decreased motivation to quit or reduce use [19,20]. All these issues are being played out in the e-cig literature, which is indicating that e-cigs are recruiting adolescents with lower-risk profiles than tobacco smokers [21]. It is not yet known whether experimentation with e-cigs puts these intermediate-risk youths at risk for transition to combustible use, although one longitudinal study points to increased risk [22]. Additionally, because it takes 2–3 years for adolescent experimenters to transition to regular smoking, it is too early to take solace in the fact that regular cigarette smoking among adolescents continues to decline in most countries. Finally, several studies suggest that e-cigs may also be failing to deliver on initial hopes that these products would greatly reduce or eliminate the use of combusted products among addicted smokers [23,24], although smokers are clearly hearing mixed messages on the harms and benefits of e-cigs from the public health community.
The decrease in perceived risk and potential concomitant increase in cannabis use associated with vaping cannabis may become even more consequential than that for e-cig and tobacco or nicotine use. With regular tobacco use, the primary and arguably sole harm is the adverse effects of smoke inhalation on physical health (e.g. cancers, cardiovascular and pulmonary disorders); if used exclusively, e-cigs could eliminate most of this risk. Typically, regular users of cannabis use cannabis less frequently than regular cigarette users use tobacco, which results in comparatively fewer harm concerns for lung cancer and chronic lung disease among cannabis smokers. The harms generally of most concern with cannabis—especially among youth—are those associated with misuse and addiction. These are the behavioral, psychological and neurocognitive consequences of repeated or chronic intoxication (e.g. increased risk behaviors, poor school or job performance, family and interpersonal problems, accidents, memory and motivational problems, development of addiction [25]). Vaping of cannabis has no foreseeable positive impact on these harms. Instead, the aforementioned positive attributes of vaping will probably contribute to increases in the frequency of use and misuse and have an adverse impact on public health by increasing the risk of these well-documented consequences of cannabis misuse.
Epidemiological, clinical and laboratory research demonstrates that risk factors for and characteristics of cannabis use disorders are comparable to other substance use disorders, and that its addictive potential is slightly lower, but certainly not negligible [25–29]. As discussed above, vaping, through its safer label, better taste and elimination of ingestion of harsh smoke, could prompt earlier age of onset and provide a more positive first experience with cannabis, both of which are associated with escalation and development of substance use problems [30–32]. Secondly, to the extent that vaping devices provide more efficient and perhaps more intense effects for less effort and cost, the use of these devices will probably impact frequency of use and thereby contribute to the development of problematic use or addiction. Most certainly, such ‘positive’ features of vaping devices will become part of promotional marketing strategies, and this could further drive greater use. Signs of such marketing practices already appear on the internet, and many such advertisements clearly target youth (if you have not yet performed the suggested internet search, we suggest you do; see Fig. 1).
Vaping devices are being promoted not just to accommodate cannabis plant material, but also for use of new, high-potency cannabis concentrates (e.g. honey oil, wax, shatter). Concentrates are created by extracting active cannabinoids from cannabis plant material using one of several solvents, most frequently butane. This extraction process can take place almost anywhere and, due to the highly volatile nature of the solvent, has led to reports of burns and explosions [33]. Moreover, because the extraction process is not regulated, the purity and potency of these concentrates is frequently unknown. Currently we have no empirical data on the effects of administering high-potency cannabis products with a device that potentially maximizes intensity of cannabis effects, although some recent data have linked frequent use of high-potency cannabis to risk of earlier-onset psychosis [34]. Generally, experience from other substances suggests that increases in potency and delivery efficiency enhance misuse and addiction. Also, mixing cannabis with tobacco is already one of the more common methods of using cannabis in many parts of the world [35]. To the extent that vaping devices promote smoking a tobacco–cannabis mixture, they may result in more frequent cannabis and tobacco administration.
Anxieties about the rapidly growing vaping industry’s product development and marketing practices that parallel the historic concerns with big tobacco companies cannot, and should not, be dismissed [36,37]. The US market for legal cannabis showed an estimated growth from 1.5 billion in 2013 to 2.7 billion in 2014 alone, and this was with only a limited number of states having operational dispensaries for medical or recreational cannabis. The vaping industry is developing rapidly alongside the legalized cannabis market (and e-cig market), and a growing lobby is already petitioning against regulation of these devices. As is the case with other recreational and medicinal substances, the goal of those who make and sell these products is to encourage as many people as possible to use cannabis products, and to use a great deal of the product. That is, their aim is to design products and marketing strategies that have the best chance of creating a market of addicted regular users. We have already observed the nascent e-cig industry develop third- and fourth-generation devices that capitalize on more effective and efficient delivery of nicotine, and an explosion in the availability of flavor choices and competitive marketing.
Another concern raised about e-cigs is the implications of the development of a cool ‘vaping culture’ that could lead to escalation of the repeated and chronic use of devices with unknown health effects [1]. Vaping of substances in addition to nicotine (flavors, cannabis) could certainly contribute to escalation of this cultural trend and probably result in the interchange or combining of materials used in vaping devices. Adding flavors to make more palatable products is a long-standing practice of the alcohol, tobacco, and now the vaping industry. Finally, e-cig use and cannabis vaping, along with legalization of cannabis products, are likely to make the depiction of vaping behaviors more public, which could reverse the progress that has been made in the de-normalization of smoking through smoke-free ordinances that have eliminated smoking in the work-place, restaurants and bars in many communities. One can imagine a future where e-cigarette, vape shop and hookah venues merge with some equivalent of the Amsterdam coffee shop and the traditional bar scene, promoting the use of all three drugs (alcohol, nicotine/tobacco and cannabis) in one venue.
Regular and frequent vaping of any substance not only incurs the risks associated with misuse of the substances, it also creates uneasiness about the unknown effects of repeated and long-term use of vaping devices. Vaping liquids typically include carrier compounds such as propylene glycol and glycerol, and devices can vary in their levels of delivery of toxicants into the lungs and into the air, depending on the material from which they are constructed (e.g. plastic, metal, glass) and their heating capacity. With cannabis, for example, vaping devices such as the Volcano have superior temperature control but are expensive (>$600). More economical units suffer from poor temperature control, resulting in a wide range of cannabinoid to by-product ratios [13] and perhaps mitigation of the purported harm reduction aspects of vaping. The proliferation of sales of diverse types of vaping devices from many manufacturers, with no regulatory guidelines in place, would seem to increase the probability of experiencing adverse effects, which will vary across devices and patterns of use.
Current knowledge suggests that, in the short term, inhaling vapors (aerosol) portends substantially less harm to the lungs than inhaling smoke; but it would seem wise to consider the history of tobacco as a harbinger of things to come. It took many years to recognize the harm inherent in tobacco smoke, in part because industry used its profits to conduct public relations campaigns that undermined the science implicating their products as harmful and found ways to engage health-conscious smokers with seemingly healthy products, such as filters and low tar cigarettes. These cigarette modifications seemed like a good idea on first inspection but resulted in harming the health-conscious smokers who adopted their use. The same caution applies to potential health consequences of vaping.
Our comments here are not intended as a diatribe against vaping or the legalization of cannabis. Instead, we wish to enhance awareness and generate discourse and studies regarding the rapidly growing phenomenon of vaping of cannabis. Rapid industry growth urgently necessitates addressing whether or not to promote vaping as a ‘safer’ method of cannabis administration, and how to regulate these products. We suggest that such considerations be contemplated and investigated in conjunction with current activities to understand the impact of vaping nicotine and the regulation of e-cigs. Most regulatory issues related to manufacturing, sales and use of vaping devices are relevant to both substances. Moreover, the common phenomena of concurrent or simultaneous use of tobacco and cannabis will probably impact upon consumer choices of vaping devices and how they are used. Finally, policymakers need to consider the risks and benefits of policies designed to maintain vaping as a small business versus allowing large corporate interests to acquire vaping companies. For example, one advantage of small businesses is that they are less likely to undertake massive national marketing campaigns that drive consumption—and one advantage of large corporations is that they have the resources to address regulatory constraints around testing and quality control of the product. Addressing these issues simultaneously with all vaping products would save time and money, and result in a more comprehensive and effective public health policy, as well as consistency in messages to the public regarding the health implications of vaping.
Acknowledgments
Drs. Budney and Lee, receive research and training support from the National Institute on Drug Abuse (T32DA037202 and R01DA032243).
Footnotes
Declaration of interests
None.
References
- 1.Gostin LO, Glasner AY. E-cigarettes, vaping, and youth. JAMA. 2014;312:595–6. doi: 10.1001/jama.2014.7883. [DOI] [PubMed] [Google Scholar]
- 2.West R, Brown J. Electronic cigarettes: fact and faction. Br J Gen Pract. 2014;64:442–3. doi: 10.3399/bjgp14X681253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Britton J. Electronic cigarettes: pro. Thorax. 2015;70:309–10. doi: 10.1136/thoraxjnl-2015-206935. [DOI] [PubMed] [Google Scholar]
- 4.Furber A. Electronic cigarettes: reasons to be cautious. Thorax. 2015;70:307–8. doi: 10.1136/thoraxjnl-2014-206735. [DOI] [PubMed] [Google Scholar]
- 5.Galandiuk S. E-cigarettes: an asset or liability in efforts to lessen tobacco smoking and its consequences. Mayo Clin Proc. 2015;90:1–3. doi: 10.1016/j.mayocp.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 6.Pisinger C, Dossing M. A systematic review of health effects of electronic cigarettes. Prev Med. 2014;69:248–60. doi: 10.1016/j.ypmed.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization (WHO) Electronic Nicotine Delivery Systems. Geneva: WHO; 2014. Contract no.: FCTC/COP/6/10 Rev.1. [Google Scholar]
- 8.Arrazola RA, Singh T, Corey CG, Husten CG, Neff LJ, Apelberg BJ, et al. Tobacco use among middle and high school students—United States, 2011–2014. Morb Mortal Wkly Rep. 2015;64:381–5. [PMC free article] [PubMed] [Google Scholar]
- 9.Room R. Legalizing a market for cannabis for pleasure: Colorado, Washington, Uruguay and beyond. Addiction. 2014;109:345–51. doi: 10.1111/add.12355. [DOI] [PubMed] [Google Scholar]
- 10.Pew Research Center. Six facts about marijuana. [accessed 14 April 2015];Facttank: News in the Numbers (internet) Available at: http://www.pewresearch.org/fact-tank/2015/04/14/6-facts-about-marijuana/
- 11.Abrams DI, Vizoso HP, Shade SB, Jay C, Kelly ME, Benowitz NL. Vaporization as a smokeless cannabis delivery system: a pilot study. Clin Pharmacol Ther. 2007;82:572–8. doi: 10.1038/sj.clpt.6100200. [DOI] [PubMed] [Google Scholar]
- 12.Moir D, Rickert WS, Levasseur G, Larose Y, Maertens R, White P, et al. A comparison of mainstream and sidestream marijuana and tobacco cigarette smoke produced under two machine smoking conditions. Chem Res Toxicol. 2008;21:494–502. doi: 10.1021/tx700275p. [DOI] [PubMed] [Google Scholar]
- 13.Pomahacova B, Van der Kooy F, Verpoorte R. Cannabis smoke condensate III: the cannabinoid content of vaporised Cannabis sativa. Inhal Toxicol. 2009;21:1108–12. doi: 10.3109/08958370902748559. [DOI] [PubMed] [Google Scholar]
- 14.Malouff JM, Rooke SE, Copeland J. Experiences of marijuana-vaporizer users. Subst Abuse. 2014;35:127–8. doi: 10.1080/08897077.2013.823902. [DOI] [PubMed] [Google Scholar]
- 15.Etter JF. Electronic cigarettes and cannabis: an exploratory study. Eur Addict Res. 2015;21:124–30. doi: 10.1159/000369791. [DOI] [PubMed] [Google Scholar]
- 16.Tetrault JM, Crothers K, Moore BA, Mehra R, Concato J, Fiellin DA. Effects of marijuana smoking on pulmonary function and respiratory complications: a systematic review. Arch Intern Med. 2007;167:221–8. doi: 10.1001/archinte.167.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Earleywine M, Barnwell SS. Decreased respiratory symptoms in cannabis users who vaporize. Harm Reduct J. 2007;4:11. doi: 10.1186/1477-7517-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herrmann ES, Cone EJ, Mitchell JM, Bigelow GE, LoDico C, Flegel R, et al. Non-smoker exposure to secondhand cannabis smoke II: effect of room ventilation on the physiological, subjective, and behavioral/cognitive effects. Drug Alcohol Depend. 2015;151:194–202. doi: 10.1016/j.drugalcdep.2015.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Okaneku J, Vearrier D, McKeever RG, LaSala GS, Greenberg MI. Change in perceived risk associated with marijuana use in the United States from 2002 to 2012. Clin Toxicol (Phila) 2015;53:151–5. doi: 10.3109/15563650.2015.1004581. Epub 2015/02/04. [DOI] [PubMed] [Google Scholar]
- 20.Pacek LR, Mauro PM, Martins SS. Perceived risk of regular cannabis use in the United States from 2002 to 2012: differences by sex, age, and race/ethnicity. Drug Alcohol Depend. 2015;149:232–44. doi: 10.1016/j.drugalcdep.2015.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wills TA, Knight R, Williams RJ, Pagano I, Sargent JD. Risk factors for exclusive e-cigarette use and dual e-cigarette use and tobacco use in adolescents. Pediatrics. 2015;135:e43–51. doi: 10.1542/peds.2014-0760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sutfin EL, Reboussin BA, Debinski B, Wagoner KG, Spangler J, Wolfson M. The impact of trying electronic cigarettes on cigarette smoking by college students: a prospective analysis. Am J Public Health. 2015;105:e83–9. doi: 10.2105/AJPH.2015.302707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hitchman SC, Brose LS, Brown J, Robson D, McNeill A. Associations between e-cigarette type, frequency of use, and quitting smoking: findings from a longitudinal online panel survey in Great Britain. Nicotine Tob Res. 2015 doi: 10.1093/ntr/ntv078. Epub 2015/04/22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al-Delaimy WK, Myers MG, Leas EC, Strong DR, Hofstetter CR. E-cigarette use in the past and quitting behavior in the future: a population-based study. Am J Public Health. 2015;105:1213–9. doi: 10.2105/AJPH.2014.302482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370:2219–27. doi: 10.1056/NEJMra1402309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Budney AJ, Vandrey RG, Fearer SA. Cannabis (marijuana) In: Ruiz P, Strain E, editors. Lowinson & Ruiz’s Substance Abuse: A Comprehensive Textbook. Baltimore, MD: Lippincott, Williams & Wilkins; 2011. pp. 214–36. [Google Scholar]
- 27.Cooper ZD, Haney M. Cannabis reinforcement and dependence: role of the cannabinoid CB1 receptor. Addict Biol. 2008;13:188–95. doi: 10.1111/j.1369-1600.2007.00095.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.von Sydow K, Lieb R, Pfister H, Hofler M, Wittchen HU. What predicts incident use of cannabis and progression to abuse and dependence? A 4-year prospective examination of risk factors in a community sample of adolescents and young adults. Drug Alcohol Depend. 2002;68:49–64. doi: 10.1016/s0376-8716(02)00102-3. [DOI] [PubMed] [Google Scholar]
- 29.Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. JAMA. 2004;291:2114–21. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- 30.Fergusson DM, Horwood LJ, Lynskey MT, Madden PA. Early reactions to cannabis predict later dependence. Arch Gen Psychiatry. 2003;60:1033–9. doi: 10.1001/archpsyc.60.10.1033. [DOI] [PubMed] [Google Scholar]
- 31.Scherrer JF, Grant JD, Duncan AE, Sartor CE, Haber JR, Jacob T, et al. Subjective effects to cannabis are associated with use, abuse and dependence after adjusting for genetic and environmental influences. Drug Alcohol Depend. 2009;105:76–82. doi: 10.1016/j.drugalcdep.2009.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gfroerer JC, Wu L-T, Penne MA. Initiation of Marijuana Use: Trends, Patterns, and Implications. SAMHSA; Rockville, MD: 2002. [Google Scholar]
- 33.Jensen G, Bertelotti R, Greenhalgh D, Palmieri T, Maguina P. Honey oil burns: a growing problem. J Burn Care Res. 2014;36:e34–7. doi: 10.1097/BCR.0000000000000067. [DOI] [PubMed] [Google Scholar]
- 34.Di Forti M, Sallis H, Allegri F, Trotta A, Ferraro L, Stilo SA, et al. Daily use, especially of high-potency cannabis, drives the earlier onset of psychosis in cannabis users. Schizophr Bull. 2014;40:1509–17. doi: 10.1093/schbul/sbt181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Agrawal A, Budney AJ, Lynskey MT. The co-occurring use and misuse of cannabis and tobacco: a review. Addiction. 2012;107(7):1221–33. doi: 10.1111/j.1360-0443.2012.03837.x. Epub 2012/02/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barry RA, Hiilamo H, Glantz SA. Waiting for the opportune moment: the tobacco industry and marijuana legalization. Milbank Q. 2014;92:207–42. doi: 10.1111/1468-0009.12055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grana RA, Ling PM. Smoking revolution’: a content analysis of electronic cigarette retail websites. Am J Prev Med. 2014;46:395–403. doi: 10.1016/j.amepre.2013.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]