Abstract
Objectives: Mindfulness-based stress reduction (MBSR) is a promising intervention for older adults seeking to improve quality of life. More research is needed, however, to determine who is most willing to use the four techniques taught in the program (yoga, sitting meditation, informal meditation, and body scanning). This study evaluated the relationship between the Big Five personality dimensions (neuroticism, extraversion, openness to experience, conscientiousness, and agreeableness) and use of MBSR techniques both during the intervention and at a 6-month follow-up. The hypothesis was that those with higher levels of openness and agreeableness would be more likely to use the techniques.
Methods: Participants were a community sample of 100 older adults who received an 8-week manualized MBSR intervention. Personality was assessed at baseline by using the 60-item NEO Five-Factor Inventory. Use of MBSR techniques was assessed through weekly practice logs during the intervention and a 6-month follow-up survey. Regression analyses were used to examine the association between each personality dimension and each indicator of MBSR use both during and after the intervention.
Results: As hypothesized, openness and agreeableness predicted greater use of MBSR both during and after the intervention, while controlling for demographic differences in age, educational level, and sex. Openness was related to use of a variety of MBSR techniques during and after the intervention, while agreeableness was related to use of meditation techniques during the intervention. Mediation analysis suggested that personality explained postintervention MBSR use, both directly and by fostering initial uptake of MBSR during treatment.
Conclusions: Personality dimensions accounted for individual differences in the use of MBSR techniques during and 6 months after the intervention. Future studies should consider how mental health practitioners would use these findings to target and tailor MBSR interventions to appeal to broader segments of the population.
Introduction
Mindfulness-based stress reduction (MBSR) interventions have shown promise in populations of older adults.1–3 Because individuals differ in their preferences for therapeutic interventions,4–8 more research is needed to determine who is most willing to use the techniques taught in the program. MBSR is an 8-week training program that teaches participants how to use yoga, meditation, and body scanning to increase awareness of thoughts and emotions. The attitudinal foundations fostered by mindfulness practice are nonjudging, patience, beginner's mind (i.e., receptive to new possibilities), trust, nonstriving, acceptance, and letting go.9 These techniques may be particularly helpful for older adults seeking nonpharmacologic approaches to mitigating quality-of-life concerns, including emotional distress,3 loneliness,2 and insomnia.1 Additionally, the yoga component of MBSR can improve balance and coordination for older adults with limited mobility.10
Studies have examined heterogeneity in terms of who benefits most from MBSR interventions (e.g., de Vibe et al., 201311), but there appears to be no research on preferences for use of particular MBSR techniques. Providers could use information about the factors that influence use to target those who are likely to be most interested in the intervention and tailor descriptions to appeal to those who may otherwise be uninterested. The present study examined the relationship between personality and use of specific MBSR techniques (yoga, sitting meditation, informal meditation, and body scan) both during and after an MBSR intervention. To conceptualize individual differences in personality dimensions relevant to MBSR use, this study used the well-validated Five-Factor Model of personality.12 This model describes personality dispositions along five broad dimensions: neuroticism (negative affect, emotional instability), extraversion (sociability, activeness), openness to experience (curiosity, insightfulness), agreeableness (empathy, cooperativeness), and conscientiousness (efficiency, goal-directedness). Observational studies have found a relationship between these personality dimensions and use of complementary and alternative medicine (CAM) techniques in daily life, including methods such as reflexology, homeopathy, osteopathy, and energy healing, in addition to mind–body therapies, such as meditation and yoga.4–8 However, no study has examined longitudinal changes in use of CAM techniques. Understanding how personality shapes use of MBSR could help providers target people who are most interested, as well as tailor their description of MBSR to attract individuals who would otherwise have limited interest.
The present study examined the relationship between personality and use of MBSR techniques among older adults participating in the intervention arm of a broader randomized controlled trial.13 Of the five personality dimensions, it was expected to find that openness and agreeableness would be related to increased use of MBSR techniques. Those with high levels of openness are insightful and introspective12 and have less parasympathetic and affective reactivity to stressful situations,14 which resembles the open curiosity toward both internal and external experiences without reactivity inherent in mindfulness practice.15 Furthermore, openness has been consistently correlated with elements of CAM, including general CAM use,5 breadth of CAM therapies tried,6 and use of mind–body practices.7,8 Those who are agreeable are cooperative and empathetic,12 which parallels critical components of mindfulness practice, including developing a sense of compassion toward others. A positive relationship has been found between agreeableness and willingness to use CAM practices in general6 and CAM mind–body practices, including meditation, visualization, yoga, and t'ai chi.8 Although research has found a relationship between other personality dimensions, particularly conscientiousness,16 and the use of various health services,17 because of the lack of compelling evidence about the relationship between these personality dimensions and use of MBSR specifically, there were no hypotheses concerning neuroticism, conscientiousness, or extraversion.
The study examined use of four MBSR techniques during the 8-week intervention phase and during a 6-month follow-up: (1) yoga, the use of postures and gentle stretching to increase awareness of bodily sensations; (2) sitting meditation, in which participants were told to focus on their breathing while sitting with their eyes closed; (3) informal meditation, in which participants were told to act mindfully while engaging in everyday activities, such as walking or eating; and (4) body scanning, the practice of systematically observing sensations in various parts of the body. The hypothesis was that agreeableness and openness would be associated with increased use of MBSR techniques during and after the intervention.
Materials and Methods
Participants and procedures
The study focused on a community sample of adults aged 60 years and older recruited from the Rochester, New York, area. Participants were recruited using newspaper advertisements and flyers between December 2006 and October 2009. Because of the importance of self-regulation in MBSR practice, exclusion criteria included uncorrected sensory deficits and cognitive impairments (defined as a score of ≤24 on the Mini-Mental Status Examination). Participants also underwent the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition and were excluded if the interview revealed the presence of major depression with psychotic features, psychosis, lifetime history of schizophrenia, bipolar disorder, organic brain syndrome, mental retardation, or alcohol/substance abuse within the last year. All participants were English speaking, and if they were prescribed antidepressant or anxiolytic medications, they must have been receiving a stable regimen for at least 8 weeks before enrolling in the study. Ultimately, 200 participants were enrolled and randomly assigned to the intervention group or control group. The present report concerns participants (n = 100) completing the MBSR intervention.
Personality and demographic data were collected at study entry by one of three masters-level research assistants. Participant characteristics are reported in Table 1. Participants were aged 64–91 years, generally college educated and white, and about evenly split on sex. During the intervention phase, home participation of MBSR techniques was measured using a weekly practice log, in which participants recorded the number of days per week they engaged in yoga, sitting meditation, body scanning, and informal meditation. Most participants (n = 90) additionally completed measures at a follow-up 6 months after the start of the program.
Table 1.
Descriptive Statistics
| Variable | Value | Range |
|---|---|---|
| Demographic characteristics and covariates | ||
| Women (%) | 62 | |
| White race (%) | 97 | |
| College education or greater (%) | 86 | |
| Age (yr) | 72.08 ± 6.74 | 64–91 |
| Mini-Mental Status Examination score | 28.89 ± 1.16 | 25–30 |
| Trail Making Test score (s) | ||
| Trails A | 39.74 ± 18.08 | 17–150 |
| Trails B | 95.11 ± 51.74 | 37–301 |
| Total time | 134.86 ± 63.30 | 54–367 |
| Perceived Stress Scale score | 1.28 ± 0.62 | 0.10–2.80 |
| Personality, 0–4 rating scales | ||
| Neuroticism | 1.37 ± 0.67 | 0.00–3.25 |
| Extraversion | 2.44 ± 0.52 | 1.17–3.58 |
| Openness | 2.66 ± 0.48 | 1.58–3.67 |
| Agreeableness | 2.94 ± 0.49 | 1.58–4.00 |
| Conscientiousness | 2.87 ± 0.55 | 1.50–4.00 |
| MBSR use while in-treatment (d per week) | ||
| Yoga | 2.19 ± 1.31 | 0.00–6.43 |
| Sitting meditation | 3.41 ± 1.47 | 0.29–7.00 |
| Informal meditation | 3.12 ± 1.88 | 0.00–7.00 |
| Body scanning | 3.56 ± 1.54 | 0.00–7.00 |
| Continued use of MBSR after treatment (mo) | ||
| Yoga | 2.62 ± 2.74 | 0.00–6.00 |
| Sitting meditation | 3.54 ± 2.65 | 0.00–6.00 |
| Informal meditation | 4.21 ± 2.72 | 0.00–6.00 |
| Body scanning | 2.80 ± 2.62 | 0.00–6.00 |
Values are expressed as percentage of participants or mean ± standard deviation. n = 100, with 90 supplying complete data at follow-up.
MBSR, mindfulness-based stress reduction.
MBSR intervention
The 8-week MBSR training program was designed to teach participants core techniques of mindfulness practice, including yoga, sitting meditation, body scanning, and informal meditation. These techniques are meant to generate nonjudgmental awareness of sensory and emotional experiences. An experienced and certified MBSR instructor led seven weekly, group-based (15–20 members) 2-hour sessions. A 7-hour intensive session was given in the middle of the program. The techniques were altered to accommodate those with mobility limitations; for example, those in wheelchairs were taught modified sitting yoga postures.
Measures
Personality
The Big Five personality domains were assessed by using the 60-item NEO Five-Factor Inventory, Revised,18 which has been found to be valid in samples of older adults.19,20 The survey measures individual differences in neuroticism (observed Cronbach α = 0.88), extraversion (α = 0.83), openness (α = 0.78), agreeableness (α = 0.82), and conscientiousness (α = 0.87). Participants respond to items, such as “I have a lot of intellectual curiosity” (openness) and “I generally try to be thoughtful and considerate” (agreeableness), using a scale from 0 (strongly disagree) to 4 (strongly agree).
MBSR activities
Beginning with second session, participants completed weekly logs in-session documenting the number of days in the last week they had practiced yoga, sitting meditation, informal meditation, and body scanning. The total attendance rate was high at 93.6%, but if participants were absent in a given week, they were mailed session handouts and the practice log to complete and return. Accordingly, missing data were rare (4.1%). Ratings were averaged across weeks for all completed logs, indicating the average number of days per week engaged in each activity. At 6 months after treatment, participants were asked whether they had used each of the four MBSR techniques in the past month and, if not, how recently (in months) they had last used each technique. These values were reverse-coded to indicate the number of months after treatment that they continued to use each activity (i.e., 0 = no post-treatment use, 1 = continued for 1 month … 6 = still active at 6 months). In support of the psychometrics of the practice logs, reports of use demonstrated excellent internal consistency reliability across the 28 (4 techniques × 7 logs) in-treatment reports (Cronbach α = 0.84) and acceptable internal consistency reliability for the 4-item post-treatment report (Cronbach α = 0.63). As well, in support of convergent validity, in-treatment use correlated with post-treatment use (r = 0.40; p ≤ 0.001). Other studies have also documented the reliability and validity of similar practice logs.21
Covariates for sensitivity analyses
Participants also completed measures of stress and cognitive functioning at study entry that were included in sensitivity analyses. Stress was measured with the 10-item (Cronbach α = 0.87) Perceived Stress Scale.22 Cognitive functioning was assessed with the Trail Making Task,23 a two-part test of cognitive processing speed and executive functioning (Trails A and B); completion times were correlated across the two parts of the test (r = 0.54, p < 0.001), so the total completion time was used as a covariate in sensitivity analyses.
Data analyses
Descriptive statistics were used to summarize patterns of use of MBSR techniques, and correlations examined whether these were associated with demographic variables. All remaining analyses controlled for age, sex, and education level. Regression analyses were used to examine the association between each personality dimension (independent variable) and each indicator of MBSR use (dependent variable), while controlling for demographic covariates. Separate regression analyses were conducted for each personality dimension (e.g., openness), as well as for the sum of the two dimensions with hypothesized effects (i.e., sum of openness + agreeableness); the latter approach provides a simple data reduction strategy useful for explaining the global effect of key personality dimensions on a given outcome.24 For MBSR use, we examined each of the four techniques separately (yoga, sitting meditation, informal meditation, and body scanning) as well as their average, both during the intervention and the post-intervention phases. In sensitivity analyses, these findings were examined and stress and cognitive functioning were controlled for. Finally, mediation analyses examined whether the relationship between personality (independent variable, summated composite of openness and agreeableness) and MBSR use after the intervention (dependent variable) was explained by MBSR use during the intervention (mediator), while controlling for demographic characteristics. Regression was used to determine whether path coefficients were statistically significant, and the bias-corrected bootstrapping method with 10,000 resamples25 was used to determine whether the indirect effect (mediational path) was significant.
Results
Descriptive overview
Use of MBSR techniques varied across activities, individuals, and time. During the MBSR intervention, average weekly participation varied from 2.19 days/wk for yoga to 3.56 days/wk for body scanning (d = 0.82, t[99] = 8.13, p < 0.001) (Table 1). Average use of MBSR activities also varied across individuals, ranging from 0.40 days/wk for the least active participant to 5.86 days/wk for the most active participant. At the follow-up 6 months after the intervention, participants reported discontinuing yoga the earliest, an average of 2.62 months after treatment, and sticking with informal meditation the longest, an average of 4.21 months after treatment (d = 0.47, t[99] = 4.47, p < 0.001) (Table 1). Differential use of MBSR techniques was not associated with demographic variables, with the exception that older participants used sitting meditation more frequently during the intervention (r = 0.25, p = 0.01) and continued informal mediation longer after the intervention (r = 0.25, p = 0.02).
Personality and MBSR practice
As hypothesized, openness and agreeableness predicted greater use of MBSR both during and after the intervention (β up to 0.42) (Table 2). Individuals higher on openness were more likely to use a variety of MBSR techniques than those lower on openness. Findings for agreeableness were less robust, confined to greater use of meditation techniques during the intervention. Neuroticism, extraversion, and conscientiousness were not statistically significantly associated with MBSR use during the intervention or afterward, having only small observed effects (average |β| = 0.08).
Table 2.
Personality Domains of Openness and Agreeableness Predict Greater Use of MBSR Techniques During and After Intervention
| Personality dimension | |||
|---|---|---|---|
| MBSR use | Openness | Agreeableness | Total of openness plus agreeableness |
| Days per week, during the intervention | |||
| Yoga | 0.19 | 0.15 | 0.23* |
| Sitting meditation | 0.21* | 0.20* | 0.28** |
| Informal meditation | 0.23* | 0.29** | 0.36*** |
| Body scanning | 0.23* | 0.01 | 0.16 |
| Average | 0.31** | 0.24* | 0.38*** |
| Months of use after the interventiona | |||
| Yoga | 0.29** | 0.13 | 0.29** |
| Sitting meditation | 0.37*** | 0.11 | 0.34*** |
| Informal meditation | 0.16 | 0.20 | 0.26** |
| Body scanning | 0.31** | 0.15 | 0.33** |
| Average | 0.39*** | 0.20 | 0.42*** |
Table values are standardized β coefficients. Each regression equation involved predicting a single MBSR variable from a single personality dimension, while controlling for age, education level, and sex. Personality was assessed with the NEO Five-Factor Inventory, Revised.
Assessed at 6-month follow-up.
p < 0.05.
p < 0.01.
p < 0.001.
The pattern of findings was similar in sensitivity analyses that, in addition to age, sex, and education level, also controlled for stress and cognitive functioning. All statistically significant findings in Table 2 remained statistically significant, with the exception that loss of degrees of freedom reduced the statistical significance of the association between agreeableness and use of sitting meditation during the intervention (β = 0.20, p = 0.07). Total levels of openness plus agreeableness continued to explain average use during (β = 0.42, p < 0.001) and after the intervention (β = 0.39, p < 0.001).
Mediation analyses
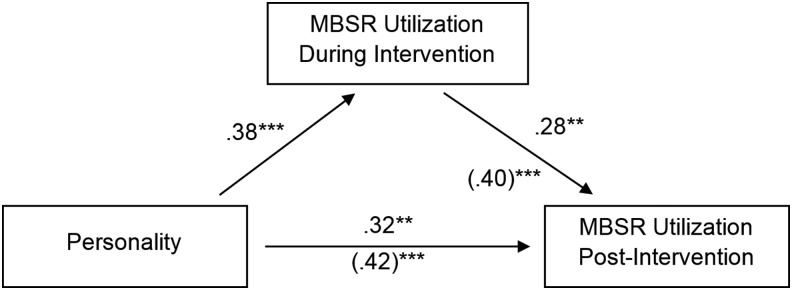
In regression analyses, personality (openness plus agreeableness) and MBSR use during treatment (averaged across techniques) explained 23% of the variance in post-intervention MBSR use (ΔF[2,84] = 13.00, p < 0.001). Analyses supported partial mediation (Fig. 1). Specifically, individual variation in MBSR use during the intervention explained 24% (i.e., the percentage difference between the total effect and the direct effect; [0.42 − 0.32]/0.42 = 0.24; Fig. 1) of the relationship between personality and post-intervention MBSR use (indirect effect p = 0.03). However, personality continued to directly explain post-intervention MBSR use, even while controlling for MBSR use during treatment (β = 0.32, p = 0.003). In summary, personality explained post-intervention MBSR use, both directly and by fostering initial uptake of MBSR during treatment.
FIG. 1.
Personality explains use of mindfulness-based stress reduction (MBSR) after the intervention. In support of partial mediation, different patterns of use during the intervention explained 24% of the relationship between personality and long-term use (indirect effect p = 0.03), with personality continuing to directly explain post-intervention use. Personality = openness + agreeableness. Parenthetical values indicate total effects. **p < 0.01; ***p < 0.001.
Discussion
Consistent with the hypotheses, the personality dimensions of openness and agreeableness were related to increased use of MBSR techniques in an intervention study involving older adults. These results build on previous nonintervention studies that have found a relationship between personality and use of some CAM activities in daily life.4–8 Mediation analysis suggested that post-intervention MBSR use was explained by personality, both directly and by increasing the initial uptake during the intervention.
Together, openness and agreeableness explained moderate variability in total use of MBSR techniques both during and after the intervention (β = 0.38 and 0.42, respectively; Table 2). Whereas agreeableness was related primarily to the use of meditation techniques during the intervention phase, openness was related to the use of a variety of MBSR techniques both during and after the intervention. Findings were similar after adjustment for age, sex, education level, perceived stress, and cognitive functioning, so they cannot be attributed to those potential confounders. Acknowledging some inconsistencies in prior studies, a cross-sectional association has been found between both openness and agreeableness and the use of various CAM therapies, such as reflexology, homeopathy, osteopathy, and energy healing, in addition to mind–body therapies, such as meditation and yoga.4–8 However, the current study appears to be the first prospective study to link higher levels of openness and agreeableness with MBSR use specifically, and the first to do so in the context of intervention research.
The techniques taught in MBSR interventions could be particularly appealing to individuals who score highly in these personality dimensions because they are more curious about their own internal experiences (openness) and are more likely to comply with interventionist instructions (agreeableness). It is also possible that, although those with higher levels of agreeableness were initially compliant with the teacher's instructions, this did not translate into continued use of the techniques. Those with higher levels of openness, however, did continue the practice, which could suggest that the personality dimension of openness is conducive to the teachings of MBSR, so they were able to more easily integrate the techniques into sustained daily use.
The personality dimensions of extraversion, conscientiousness, and neuroticism were not significantly associated with MBSR use. While a relationship between extraversion and the use of certain CAM therapies has been found, this relationship is limited to more interactive CAM components, such as massage therapy.4,8 Conscientiousness has been found elsewhere to relate to treatment adherence,16 but the current findings in this sample of treatment-seeking older adults suggest that this dimension may be less relevant to the use of MBSR.
Because this study found that personality plays a role in the differential use of MBSR activities, future research should examine whether these findings can be used to target and tailor MBSR interventions. Individuals with higher levels of openness and agreeableness spend more time in specific locations (restaurants, bars, and coffee shops26), visit certain types of websites (blogs,27 games,28 social network,29 and shopping28,30), and are more politically liberal.31 Thus, future studies could be directed toward assessing the feasibility of marketing MBSR at relevant locations, websites, and events. Future studies should also address how to market MBSR more effectively toward people lower on openness and agreeableness. Basic personality research shows that individuals who are lower on agreeableness tend to avoid using social support32 and tend to spend more time at home than in public;26 thus, interventionists could target less agreeable individuals by emphasizing that it involves managing stress through self-regulation and can be practiced at home. Although people lower on openness and agreeableness may have ambivalent or antagonistic thoughts about the utility of MBSR, these individuals also tend to experience greater levels of stress,33 so programs could emphasize that MBSR encourages people to accept their thought processes, even skeptical ones, while experimenting with whether the techniques may help. Additionally, while open and agreeable individuals may be more excited about trying new stress-reduction techniques, practitioners might appeal to other individuals by instead emphasizing the scientific evidence base of MBSR.34
This study had several strengths and limitations. The strengths of this study include that it was conducted in the context of an intervention, considered four separate MBSR techniques, was sensitive to the developmental context of older adulthood, and incorporated a 6-month follow-up. One limitation of the study was that the participants were predominantly white and college educated, so future studies could consider a broader sample to increase the generalizability of findings. Second, this study relied on self-reported measures of time spent engaging in home practice of MBSR techniques. Technological advancements, such as ecological momentary assessment,35 could enable future investigations to track use of these techniques more carefully. Third, although the 60-item Revised NEO Personality Inventory has consistently been found reliable and valid across contexts and cultures,18 the current study examined only the five broad personality domains. Future investigations may wish to explore narrow facets of personality, particularly facets of openness and agreeableness, and other constructs, such as creativity,36 trait mindfulness,37 or spirituality.37 Future studies could additionally benefit from incorporating a follow-up measure of personality at the completion of the program phase in order to assess whether learning and using MBSR techniques could affect personality; some research suggests that mindfulness practice may influence aspects of personality over time.38,39
In summary, personality accounted for individual differences in the use of MBSR techniques during and 6 months after intervention in a sample of older adults. Higher levels of openness and agreeableness were predictive of greater use. Because MBSR interventions can provide older adults with effective, nonpharmacologic techniques to help with quality-of-life concerns, future studies should consider how mental health practitioners could use these findings to target and tailor MBSR interventions to appeal to a broader segment of the population.
Acknowledgments
This work was supported in part by the Roadmap Scholars Award of the Louisiana Clinical and Translational Science Center from the National Institute of General Medical Sciences (U54GM104940), the National Institute of Mental Health (R25MH074898, T32MH018911), and the National Institute on Aging (R01AG025474, R24AG031089).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Zhang J, Liu X, Xie X, et al. , Mindfulness-based stress reduction for chronic insomnia in older adults 75+ years of age: a randomized controlled, single-blind clinical trial. Explore 2015;11:180–185 [DOI] [PubMed] [Google Scholar]
- 2.Creswell JD, Irwin MR, Burklund LJ, et al. , Mindfulness-based stress reduction training reduces loneliness and pro-inflammatory gene expression in older adults: a small randomized controlled trial. 2012;26:1095–1101 [DOI] [PMC free article] [PubMed]
- 3.Young LA, Baime MJ. Mindfulness-based stress reduction: effect on emotional distress in older adults. Complement Health Pract Rev 2010;15:59–64 [Google Scholar]
- 4.Sarris J, Goncalves DC, Robins Wahlin TB, Byrne GJ. Complementary medicine use by middle-aged and older women: personality, mood and anxiety factors. J Health Psychol 2011;16:314–321 [DOI] [PubMed] [Google Scholar]
- 5.Thomson P, Jones J, Browne M, Leslie SJ. Psychosocial factors that predict why people use complementary and alternative medicine and continue with its use: a population based study. Complement Ther Clin Pract 2014;20:302–310 [DOI] [PubMed] [Google Scholar]
- 6.Sirois FM, Purc-Stephenson RJ. Personality and consultations with complementary and alternative medicine practitioners: a five-factor model investigation of the degree of use and motives. J Altern Complement Med 2008;14:1151–1158 [DOI] [PubMed] [Google Scholar]
- 7.Honda K, Jacobson JS. Use of complementary and alternative medicine among United States adults: the influences of personality, coping strategies, and social support. Prev Med 2005;40:46–53 [DOI] [PubMed] [Google Scholar]
- 8.Smith BW, Dalen J, Wiggins KT, Christopher PJ, Bernard JF, Shelley BM. Who is willing to use complementary and alternative medicine? Explore 2008;4:359–367 [DOI] [PubMed] [Google Scholar]
- 9.Kabat-Zinn J, Hanh TN. Full Catastrophe Living: using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. Crystal Lake, IL: Delta, 2009 [Google Scholar]
- 10.Tiedemann A, O'Rourke S, Sesto R, Sherrington C. A 12-week Iyengar yoga program improved balance and mobility in older community-dwelling people: a pilot randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2013;68:1068–1075 [DOI] [PubMed] [Google Scholar]
- 11.de Vibe M, Solhaug I, Tyssen R, et al. . Does personality moderate the effects of mindfulness training for medical and psychology students? Mindfulness 2013;6:1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCrae RR, Costa PT., Jr. Introduction to the empirical and theoretical status of the five-factor model of personality traits. In: Widiger TA, Costa PT, Jr., eds. Personality Disorders and the Five-Factor Model of Personality. Washington, DC: American Psychological Association; 2013 [Google Scholar]
- 13.Moynihan JA, Chapman BP, Klorman R, et al. . Mindfulness-based stress reduction for older adults: effects on executive function, frontal alpha asymmetry and immune function. Neuropsychobiology 2013;68:34–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams PG, Rau HK, Cribbet MR, Gunn HE. Openness to experience and stress regulation. J Res Personal 2009;43:777–784 [Google Scholar]
- 15.Klein R, Dubois S, Gibbons C, Ozen L, Marshall S, Cullen N. The Toronto and Philadelphia Mindfulness Scales: associations with satisfaction with life and health-related symptoms. Int J Psychol Psycholog Ther 2015;15:133–142 [Google Scholar]
- 16.Hill PL, Roberts BW. The role of adherence in the relationship between conscientiousness and perceived health. Health Psychol 2011;30:797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Friedman B, Veazie PJ, Chapman BP, Manning WG, Duberstein PR. Is personality associated with health care use by older adults? Milbank Q 2013;91:491–527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCrae RR, Costa PT. A contemplated revision of the NEO Five-Factor Inventory. Personal Individ Diff 2004;36:587–596 [Google Scholar]
- 19.Hayward RD, Taylor WD, Smoski MJ, Steffens DC, Payne ME. Association of five-factor model personality domains and facets with presence, onset, and treatment outcomes of major depression in older adults. Am J Geriatr Psychiatr 2013;21:88–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duberstein PR, Chapman BP, Tindle HA, et al. . Personality and risk for Alzheimer's disease in adults 72 years of age and older: a 6-year follow-up. Psychol Aging 2011;26:351–362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wahbeh H, Lane JB2, Goodrich E1, Miller M1, Oken BS. One-on-one mindfulness meditation trainings in a research setting. Mindfulness 2014;5:88–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24:385–396 [PubMed] [Google Scholar]
- 23.Reitan RM. Trail Making Test: Manual for Administration and Scoring. Mesa, AZ: Reitan Neuropsychology Laboratory, 1992 [Google Scholar]
- 24.Chapman BP, van Wijngaarden E, Seplaki CL, Talbot N, Duberstein P, Moynihan J. Openness and conscientiousness predict 34-week patterns of Interleukin-6 in older persons. Brain Behav Immun 2011;25: 667–673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Meth 2008;40:879–891 [DOI] [PubMed] [Google Scholar]
- 26.Mehl MR, Gosling SD, Pennebaker JW. Personality in its natural habitat: manifestations and implicit folk theories of personality in daily life. J Personal Soc Psychol 2006;90:862. [DOI] [PubMed] [Google Scholar]
- 27.Guadagno RE, Okdie BM, Eno CA. Who blogs? Personality predictors of blogging. Computers Human Behav 2008;24:1993–2004 [Google Scholar]
- 28.McElroy JC, Hendrickson AR, Townsend AM, DeMarie SM. Dispositional factors in internet use: personality versus cognitive style. MIS Q 2007;31:809–820 [Google Scholar]
- 29.Hughes DJ, Rowe M, Batey M, Lee A. A tale of two sites: Twitter vs. Facebook and the personality predictors of social media usage. Computers Human Behav 2012;28:561–569 [Google Scholar]
- 30.Wang CC, Yang HW. Passion for online shopping: the influence of personality and compulsive buying. Social Behav Personal 2008;36:693–706 [Google Scholar]
- 31.Vecchione M, Caprara GV. Personality determinants of political participation: the contribution of traits and self-efficacy beliefs. Personal Individ Diff 2009;46:487–492 [Google Scholar]
- 32.Carver CS, Connor-Smith J. Personality and coping. Annu Rev Psychol 2010;61:679–704 [DOI] [PubMed] [Google Scholar]
- 33.Ebstrup JF, Eplov LF, Pisinger C, Jørgensen T. Association between the Five Factor personality traits and perceived stress: is the effect mediated by general self-efficacy? Anxiety Stress Coping 2011;24:407–419 [DOI] [PubMed] [Google Scholar]
- 34.Furnham A. Are modern health worries, personality and attitudes to science associated with the use of complementary and alternative medicine? Br J Health Psychol 2007;12:229–243 [DOI] [PubMed] [Google Scholar]
- 35.Moore RC, Depp CA, Wetherell JL, Lenze EJ. Ecological momentary assessment versus standard assessment instruments for measuring mindfulness, depressed mood, and anxiety among older adults. J Psychiatr Res 2016;75:116–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ostafin BD, Kassman KT. Stepping out of history: mindfulness improves insight problem solving. Consciousness Cognition 2012;21:1031–1036 [DOI] [PubMed] [Google Scholar]
- 37.Carmody J, Reed G, Kristeller J, Merriam P. Mindfulness, spirituality, and health-related symptoms. J Psychsom Res 2008;64:393–403 [DOI] [PubMed] [Google Scholar]
- 38.van den Hurk PA, Wingens T, Giommi F, et al. , On the relationship between the practice of mindfulness meditation and personality—an exploratory analysis of the mediating role of mindfulness skills. Mindfulness 2011;2:194–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Krasner MS, Epstein RM, Beckman H, et al. . Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA 2009;302:1284–1293 [DOI] [PubMed] [Google Scholar]