Background
With wider use of electronic health records (EHRs), physicians increasingly receive notifications via EHR-based inboxes (e.g., Epic’s “In-Basket” and GE Centricity’s “Documents”). Types of notifications include test results, referral responses, medication refill requests, and messages from clinicians, among others.1,2 In our work within the Department of Veterans Affairs (VA), we found providers receive large quantities of EHR-based notifications, making it harder to discern important vs. irrelevant information and increasing their risk of overlooking abnormal test results.3–6 Information overload is of emerging concern because new types of EHR-based notifications and ‘FYI’ messages can be easily created (versus in paper-systems) and this additional workload remains uncompensated1,2,4 despite reimbursement reductions. Moreover, EHRs make it easier to measure information load. We quantified notifications physicians received via inboxes of commercial EHRs to estimate their burden.
Methods
We obtained electronic logs of all notifications received by all physicians during a 6-month period from 1/1/2015-6/30/2015 at three large practices in Texas (two primary care; one multispecialty). We then tabulated notifications that conveyed new information to physicians for the 125 workdays during the study period. Types of notifications were categorized on whether or not they were related to test results. To account for different times each physician spent in the outpatient clinic, we normalized message quantities by percent time worked such that the notification quantity would represent the number of notifications received if the physician was full-time. We excluded physicians working <20% and if they did not work the entire 6 months. We calculated means of normalized notifications each physician would receive each workday, and performed univariate analysis of variance comparisons across sites and between primary care physicians (PCPs, including family medicine, internal medicine, and geriatrics) and specialty physicians at the multispecialty clinic. Additionally, we performed a correlation analysis to determine if an association existed between time worked and normalized number of notifications.
Results
Of 125 physicians, 33 met exclusion criteria, leaving 92 physicians’ EHR inboxes for analysis: 19 PCPs and 46 specialists at Site A using Epic, 12 PCPs at Site B also using Epic, and 15 PCPs at Site C using GE Centricity. We analyzed a total of 276,207 notifications (146,521 Site A, 51,090 Site B, and 78,596 Site C).
Across three sites, PCPs (n=46) received a mean of 76.9 (SD=38.0) total notifications/day (65.2, 113.5, and 62.6 at sites A, B, and C respectively; p<0.001) of which 20.2% (15.5 notifications/day; SD=6.0) were test result-related (15.1, 18.7, and 13.4 at sites A, B, and C respectively; p=0.07; Figure 1). In addition to previously-identified types,2 notifications included messages directly from patients and pharmacies. At site A, we found that specialists received 29.1 total and 10.4 test results notifications/day, significantly fewer than PCPs at the same site (p<0.001 and p=0.03, respectively).
Figure 1. Number and Types of Notifications Received by Physician type.
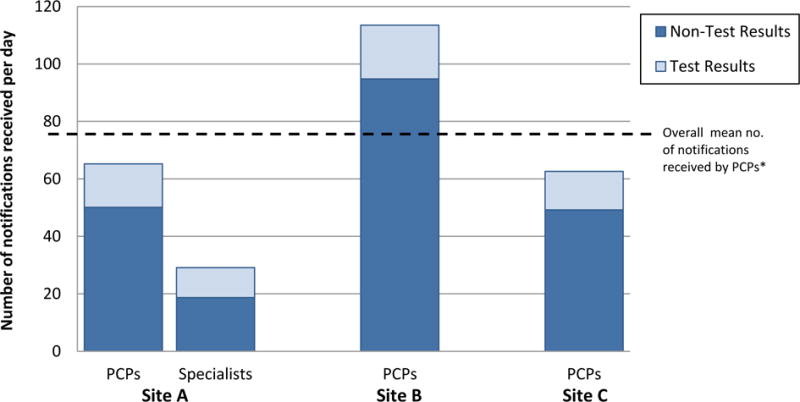
*Primary care providers (PCPs) received a mean of 76.9 notifications/day. Specialists (site A only) received a mean of 29.1 notifications/day (p<.001).
Lastly, there were significant, negative correlations between time worked and normalized daily total notifications received (r=−0.27;p=0.008) suggesting that part-time physicians received more notifications for time spent in clinic than full-time physicians.
Discussion
A large quantity of information is communicated to PCPs each day via commercial EHRs. In our prior VA work, PCPs spent a mean of 49 minutes processing 56.4 notifications of comparable content each day (i.e., mean 52 seconds/notification). Extrapolating this to commercial EHRs suggests clinicians spend an estimated 66.8 minutes/day on processing notifications, which likely adds a substantial burden to their workday. Specialists received less than half this amount, and part-time physicians appeared to receive proportionately more. Because a single notification often contains multiple data points (e.g., metabolic panels contain 7–14 laboratory values), the actual burden and physicians’ required cognitive effort is likely greater. Strategies to help filter messages relevant to high-quality care, EHR designs that support team-based care, and staffing models that assist clinicians in managing this influx of information are needed.
Acknowledgments
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Funding: This project is funded by the Agency for Health Care Research and Quality (R01HS022087), and partially funded by the Houston VA HSR&D Center for Innovations in Quality, Effectiveness and Safety (CIN 13–413). Dr. Murphy is additionally funded by an Agency for Healthcare Research & Quality Mentored Career Development Award (K08-HS022901) and Dr. Singh is additionally supported by the VA Health Services Research and Development Service (CRE 12-033; Presidential Early Career Award for Scientists and Engineers USA 14-274) and the VA National Center for Patient Safety. These funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
There are no conflicts of interest for any authors.
References
- 1.Murphy DR, Reis B, Kadiyala H, et al. Electronic Health Record-Based Messages to Primary Care Providers: Valuable Information or Just Noise? Arch Intern Med. 2012;172(3):283. doi: 10.1001/archinternmed.2011.740. [DOI] [PubMed] [Google Scholar]
- 2.Murphy DR, Reis B, Sittig DF, Singh H. Notifications received by primary care practitioners in electronic health records: a taxonomy and time analysis. Am J Med. 2012;125(2):209.e1–e7. doi: 10.1016/j.amjmed.2011.07.029. [DOI] [PubMed] [Google Scholar]
- 3.Singh H, Spitzmueller C, Petersen NJ, et al. Primary care practitioners’ views on test result management in EHR-enabled health systems: a national survey. J Am Med Inform Assoc. 2012 Dec; doi: 10.1136/amiajnl-2012-001267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McDonald CJ, McDonald MH. Electronic Medical Records and Preserving Primary Care Physicians’ Time: Comment on “Electronic Health Record-Based Messages to Primary Care Providers”. Arch Intern Med. 2012;172(3):285. doi: 10.1001/archinternmed.2011.1678. [DOI] [PubMed] [Google Scholar]
- 5.Wahls TL, Cram PM. The frequency of missed test results and associated treatment delays in a highly computerized health system. BMC Fam Pract. 2007;8:32. doi: 10.1186/1471-2296-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh H, Thomas EJ, Sittig DF, et al. Notification of Abnormal Lab Test Results in an Electronic Medical Record: Do Any Safety Concerns Remain? Am J Med. 2010;123(3):238–244. doi: 10.1016/j.amjmed.2009.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]


