Abstract
The status of the macula is a significant factor in determining final visual outcomes in rhegmatogenous retinal detachment (RRD) and should be considered in the timing of surgical repair. Several studies have shown that macula-involving RRDs attain similar visual and anatomic outcomes when surgery is performed within seven days as compared to emergent surgery (within 24 hours). In contrast, surgery prior to macular detachment in macula-sparing RRDs generally yields the best visual outcomes. In the case of macula-sparing RRDs, it is not clear how long the macula may remain attached, therefore, standard practice dictates emergent surgery. Timing of presentation, examination findings, case complexity, co-existing medical conditions, surgeon expertise, and timing and quality of access to operating facilities and staff, however, should all be considered in determining whether a macula-sparing RRD requires immediate intervention or if equivalent visual and possibly better overall outcomes can be achieved with scheduled surgery within an appropriate time frame.
Keywords: Macula-Sparing Rhegmatogenous Retinal Detachment, Emergency Surgery, Time-to-Surgery, Macula-on, Fovea-Sparing, Rhegmatogenous Retinal Detachment
INTRODUCTION
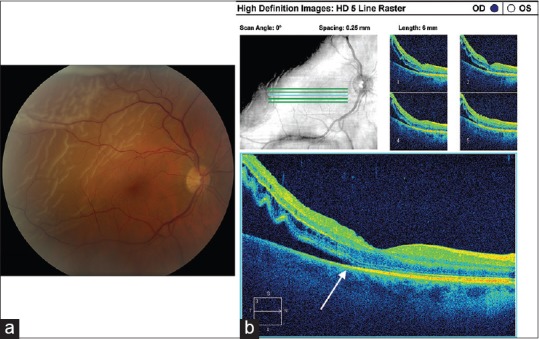
Historically, all rhegmatogenous retinal detachments (RRDs) were considered surgical emergencies; therefore, the patient was taken for immediate surgical repair at the time of presentation. The prevalent thought at the time was that emergent surgery would lead to better visual and anatomic outcomes. More recent studies, however, have shown that the status of the macula is a significant factor in determining final visual outcomes and should be considered in the timing of surgical repair.[1,2,3,4,5,6,7,8,9] Macula-off or macula-involving RRD refers to cases in which the liquefied vitreous has already entered the subfoveal space resulting in potentially permanent damage to the patient's visual acuity via photoreceptor cell death and retinal anoxia [Figure 1].[10,11] In these cases, surgical repair is typically scheduled within seven to ten days of detachment [Table 1].[2,3,4,5] In contrast, macula- or fovea-sparing (also dubbed macula-on) RRD indicates that subretinal fluid has not affected central vision and that visual acuity remains at baseline [Figure 2a–c]. The timing of surgical repair is vital in preventing progression of fluid into the subfoveal space and reducing the potential for subsequent vision loss.[12] The goal of RRD repair is to reattach the retina and to improve (macula-involving RRD) or stabilize (macula-sparing RRD) vision.
Figure 1.
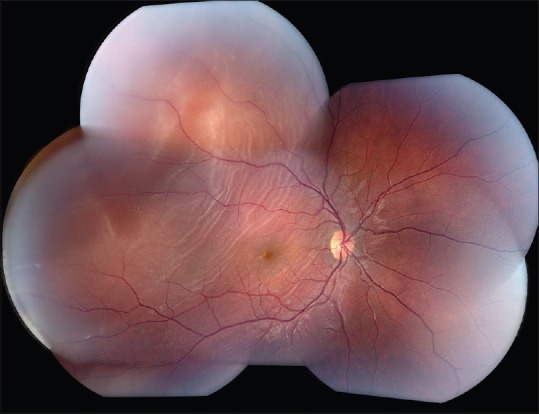
Fundus photograph of macula-involving rhegmatogenous retinal detachment. Subretinal fluid can be seen extending into the macula. The retinal tear, noted superotemporally on examination, is outside the field of view.
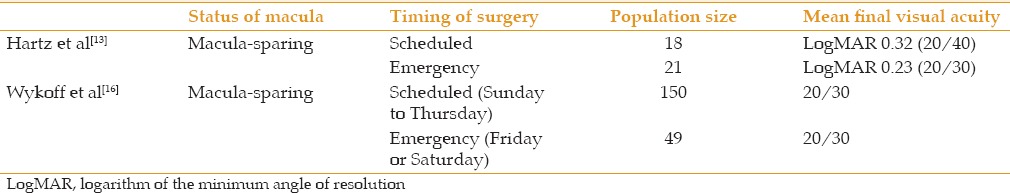
Table 1.
Final visual acuity and anatomic success after surgical repair of macula-involving rhegmatogenous retinal detachment
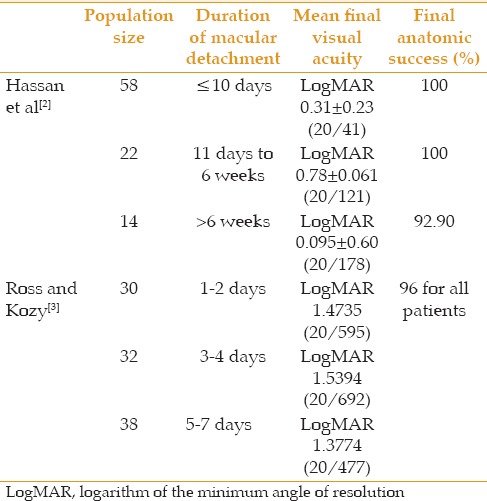
Figure 2.
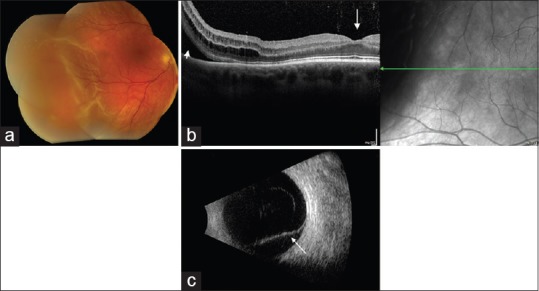
Macula-sparing rhegmatogenous retinal detachment (RRD). (a) Fundus photograph of macula-sparing RRD. The subretinal fluid does not extend to involve the fovea. (b) Heidelberg optical coherence tomography (OCT) of macula-sparing RRD shows subretinal fluid (short arrow) and overlying detached retina. The fovea (long arrow) remains attached. (c) B-scan ultrasound shows macula-sparing RRD (arrow).
MACULA-SPARING RHEGMATOGENOUS RETINAL DETACHMENT
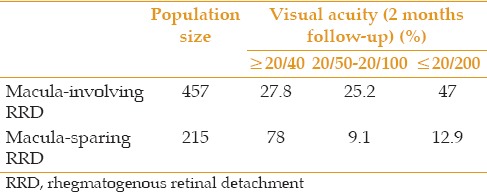
Macula-sparing RRDs have a higher probability of achieving better visual outcomes.[9,13] Williamson et al compared 330 patients with macula-sparing RRD and 325 patients with macula-involving RRD. Visual acuities were compared to the duration of RRD (1, 2, 3, 4, 5, 6, 7-13, 14-20, and ≥21 days). Patients with macula-sparing RRD achieved better vision (median 6/6) than subjects with macula-involving RRD (median 6/9).[14] Salicone et al showed similar visual outcomes for macula-sparing versus macula-involving RRDs [Table 2].[9]
Table 2.
Visual acuity of macula-sparing and macula involving rhegmatogenous retinal detachment
Repair of macula-sparing RRDs generally leads to excellent anatomic and visual outcomes. Wilkinson found that 97% of macula-sparing RRDs were successfully repaired with a single operation and 90% achieved visual acuity of 20/40 or better following surgical repair. In the same study, 24% of eyes with normal (20/20) or near-normal (20/25) preoperative visual acuity suffered from partial vision loss (≥20/30) post-operatively despite anatomically successful reattachment.[15]
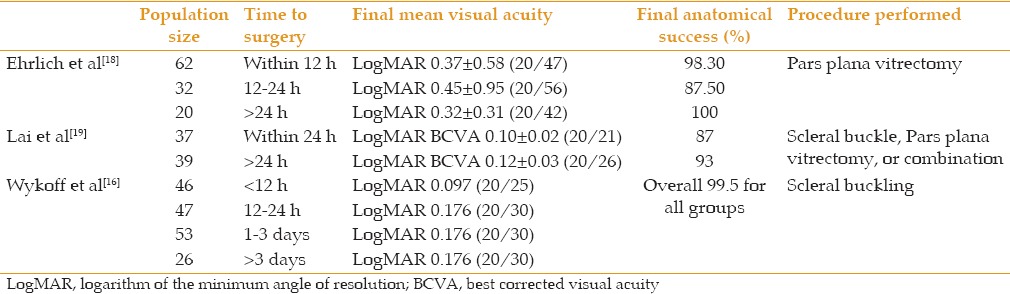
Hartz et al compared macula-sparing and macula-involving RRDs in scheduled and emergency settings and sought to determine whether there was a statistically significant difference in visual acuity outcomes [Table 3]. A 15% random sample was extracted from 884 cases of primary scleral buckling procedures performed from 1983 to 1987. Medical records of the 137 randomly selected patients were analyzed and all relevant patient characteristics were compared. Of the 18 patients with macula-sparing RRD scheduled for surgery, none progressed to involve the fovea prior to surgery. Final visual acuity outcomes for scheduled and emergent surgery were similar after taking into account presenting patient characteristics.[13] Wykoff et al similarly showed equivalent visual acuity outcomes in emergent versus scheduled surgery for macula-sparing RRDs [Table 3].[16]
Table 3.
Visual acuity outcomes in scheduled versus emergency macula-sparing rhegmatogenous retinal detachment repair with scleral buckling procedure
Ho et al reviewed 82 patients with macula-sparing RRD with average time-to-surgery of 2.33 days and found that most did not progress within the first few days after presentation. Eleven (13%) patients demonstrated progression of fluid with an average rate of 1.88 disc diameters/day. Ho et al concluded that the distance of subretinal fluid from the fovea at presentation was the only significant risk factor for progression to foveal detachment.[17]
Three separate studies have looked at the correlation between time-to-surgery in macula-sparing RRD and anatomic and visual outcomes [Table 4].[16,18,19] These studies concluded that delaying the repair of macula-sparing RRD does not necessarily result in worse anatomic or visual outcomes.
Table 4.
Visual and anatomic outcomes of macular-sparing rhegmatogenous retinal detachment
Of the 114 patients in Elrich's study, six subjects had delayed surgery (two to five days) based on institutional policies that retinal reattachment surgery must start before hour 20:00 or wait until the next available day and time. Two of 32 patients in the 12-24 hour time-to-surgery cohort progressed to involve the macula before the scheduled surgical repair. In both cases, the patients had bullous superior RRDs encroaching on the macula at presentation [Figure 3a and b]. Despite progression of the RRD, both patients had successful reattachment of the retina and maintained their excellent preoperative visual acuity. The authors did not find a correlation between time-to-surgery and final anatomic or visual outcomes but advocated undertaking RRD repair as soon as reasonably possible, especially in superior detachments and those involving the temporal arcades.[18]
Figure 3.
(a) Fundus photograph of macula-threatening RRD with subretinal fluid encroaching on the fovea; (b) Cirrus optical coherence tomography (OCT) of macula-threatening RRD. The subretinal fluid extends to the edge of the fovea (arrow) but visual acuity remains 20/20.
In Lai's analysis, the median time to surgery for the ≤24-hour group was 0.8 ± 0.4 days. Median time to surgery for the >24-hour group was 3.7 ± 2.2 days. Variables such as timing of surgery, lens status, location of detachment, and type of surgery did not lead to a statistically significant higher risk of retinal redetachment. Lai et al, however, did find that patients who presented with pseudophakic macula-sparing RRDs were more likely to undergo early (<24 hours) surgical repair. There is a possibility that pseudophakic macula-sparing RRDs present with findings that prompt the surgeon to intervene sooner.[19]
Wykoff observed the greatest range of time-to-surgery and concluded that many macula-sparing RRDs can be safely deferred for a short period of time. This study included 187 macula-sparing RRDs of which 12 (6%) were operated on during a weekend or holiday. There were 55 (29%) patients who went to the operating room between 24 and 72 hours after initial evaluation and eight (4%) patients who were operated on more than one week after presentation. In the group operated on after one week, surgery was delayed due to RRDs diagnosed bilaterally, medical problems, personal reasons, and in one patient, hurricane constraint. This patient was the only case in whom the RRD progressed to involve the macula but only after four days, and final visual acuity was 20/40. The observed trend was that superior and temporal RRDs and patients with superior retinal breaks received surgery sooner.[16]
These studies found no statistically significant differences between patients with macula-sparing RRD who were operated on the day of presentation versus days later in terms of final anatomic and visual outcomes. The studies accounted for variable factors including age, gender, lens status, duration of symptoms, location of RRD, location or number of retinal breaks, intraoperative drainage of subretinal fluid, intraoperative complications and the need for reoperation, and still found no correlation with final visual acuity or anatomic success. Limitations of these studies are their retrospective design and relatively small population size. Although a prospective study would give us useful information and have more control over variables, it would be unethical to extend a patient's time-to-surgery for macula-sparing RRD.
DISADVANTAGES OF EMERGENCY SURGERY
Conventionally, all retinal detachment surgeries were considered emergent in nature. Recent studies have shown different requirements for time-to-surgical repair in macula-sparing versus macula-involving RRDs. In macula-involving RRDs, a seven to ten day window to surgical repair is considered as standard practice based on clinical, post-mortem, and animal studies showing similar anatomic and functional outcomes whether the patient is scheduled for surgery or operated on emergently within 24 hours. In macula-sparing RRDs, little has been published regarding whether surgery should be performed emergently, scheduled within one to three days, or scheduled within seven days. It is standard practice to operate within 24 hours to reduce the possibility of macular detachment; however there are no studies which have specifically shown that operating so quickly achieves better outcomes.[12] The general thought is simply to perform surgery emergently in an effort to significantly reduce the possibility of macular detachment. Since there is no known definitive time period until macular detachment, and since visual outcomes are significantly better if macular detachment does not occur preoperatively, why not operate on an emergent basis? Emergent surgeries performed in a wide spectrum of medical subspecialties have been shown to have additional risks and costs that must be considered.[13,20,21,22,23,24] This is dubbed the “weekend effect” and studies regarding this phenomenon in the operative literature consistently demonstrate sub-standard outcomes for emergent and elective surgeries performed during the weekend.[24] While causes of the “weekend effect” remain largely unknown, factors may include lack of access to operating facilities and trained staff, surgeon fatigue, surgeon inexperience, and greater risks related to co-morbid medical conditions when surgery is performed out of normal hours.
ACCESS TO FACILITIES AND TRAINED STAFF IN EMERGENCY SURGERY
In the 2015 Preferences and Trends (PAT) Survey, vitreoretinal surgeons were asked to state the percentage of surgical procedures performed in an ambulatory surgery center (ASC). Out of 814 respondents, 504 (62%) performed some or all of their cases in an ASC.[25] The 38% of respondents who did not use an ASC most likely performed surgery at a private, teaching, or Veterans Affairs (VA) medical center hospital. For vitreoretinal surgeons that perform surgery solely at an ASC, access to ASC facilities for emergent surgery may be extremely limited or completely unavailable during evenings and weekends. These same surgeons may have hospital privileges at a nearby hospital; however, the operating room in these situations may have inadequate instrumentation and/or staffing due to the limited number of vitreoretinal surgical cases performed.
In situations which the vitreoretinal surgeon performs an adequate number of cases at the hospital, allowing access to proper instrumentation and trained staff, still other concerns arise. Heng correctly noted that scheduling emergency surgery cases among elective cases often results in prolonged waits for emergency surgery and delay or cancellation of elective cases.[26] Frimpong-Ansah and Kirkby reported on data collected from a questionnaire that was sent to all members of the British and Eire Association of Vitreo-Retinal Surgeons (BEAVRS). Of the 78 respondents, 66 (84.6%) had access to operating room and staff on weekends, but as the authors noted, this did not necessarily mean that surgery could be easily arranged. It is ease of access to and functionality of facilities that are crucial, not just the availability of facilities and staff. In some instances, non-ophthalmology operating rooms were shared and there was sporadic availability of ophthalmic-trained staff. In other instances, generally trained nurses obtained phone advice from ophthalmic-trained staff. This is hardly an ideal situation to operate on a macula-sparing RRD. It is also important to note that even in the best situation, ophthalmic-trained staff do not always equate to vitreoretinal-trained staff.
In the same study, 22 of 78 (28.3%) vitreoretinal surgeons that responded to the survey provided continuous retina call. This led the authors to conclude that most likely, the majority of vitreoretinal surgeons covered call informally when they were not strictly on call.[27] A similar study was conducted in Spain in which a questionnaire was given to the heads of ophthalmology departments to obtain information on the management of urgent RRDs. Eighty percent (80%) of respondents admitted to difficulties in management of urgent RRDs during weekends including availability of operating rooms, anesthesiology staff and trained ophthalmic nurses. Seventy-four percent (74%) of respondents admitted to having no vitreoretinal specialist and referred patients to other hospitals.[28] The authors note that the limited number of presenting macula-sparing RRDs makes it difficult to justify allocating resources for emergent RRD surgery in all hospitals. Rojas suggests concentrating emergent surgery at specific centers. Unfortunately, this would make access difficult for patients not living nearby these centers. In addition, referral to these centers would increase the time from diagnosis to surgery, possibly leading to an increase in the number of cases in which the macula is detached by the time of surgery.[24,29,30]
SURGEON FATIGUE
Surgery performed in an emergent setting is typically outside normal work hours and may lead to a higher risk of complications and adverse effects based on physician and staff fatigue. It is believed that muscular and mental fatigue can develop during prolonged operating leading to a reduction in a surgeon's fine motor control and reduced precision of instrument movement.[31,32] One study showed intraoperative complications in 5.1% of RRD operations.[33] Future studies comparing these complication rates in emergency versus scheduled surgery would be instructive in showing whether surgeon fatigue should be considered as a factor in determining the best time to perform surgery for a macula-sparing RRD.
SURGEON EXPERIENCE
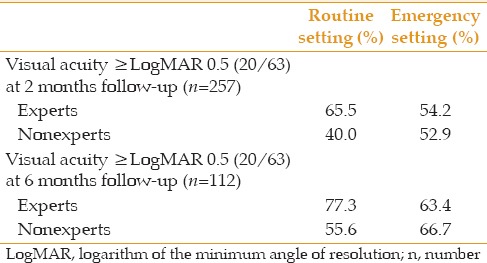
Another consideration for the success of retinal detachment repair is surgeon experience. This is especially important in emergency cases. On-call surgeons for evening and weekend procedures may include vitreoretinal fellows-in-training as well as surgeons who operate infrequently. Mazinani et al showed that the learning effect was reduced by half after 500 vitreoretinal procedures which corresponded to approximately 60 retinal detachment procedures.[34] Koch et al analyzed 1,810 cases of RRD and found that non-experts who had performed fewer than 30 pars plana vitrectomies (PPV) and 30 scleral buckling procedures (SBP) for RRD as primary surgeons, achieved inferior anatomic results when performing surgery in the emergency setting [Table 5].[35] In the routine setting, experts and non-experts achieved comparable results; however, Koch specifically analyzed the final outcomes of patients with visual acuity ≥0.5 LogMAR (20/63) [Table 6]. In this group, there was a trend for better visual outcomes when surgery was performed by an expert surgeon in a routine setting. One reason for this trend may have been that scheduled surgery allowed for assistance by expert surgeons and thus, overall better outcomes.
Table 5.
Primary anatomical success rates of retinal reattachment for experts versus nonexperts performing repair of rhegmatogenous retinal detachment in routine and emergency settings
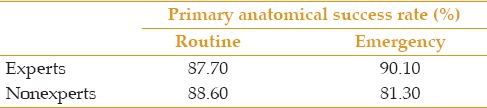
Table 6.
2 and 6 months visual acuity in rhegmatogenous retinal detachment surgeries performed by experts and nonexperts
SYSTEMIC RISKS ASSOCIATED WITH EMERGENCY SURGERY
Emergency surgery has potential disadvantages that must be considered in the context of co-existing systemic illness and anesthesia risk. While this has not been specifically studied in the context of emergency retinal detachment surgery, data from related analyses can be beneficial. Henderson et al reviewed ophthalmic surgery cancellations in an ambulatory surgical center over a two-year period. Medical reasons accounted for 40% of all late cancellations, with the majority denied anesthesia clearance related to cardiovascular problems (uncontrolled high blood pressure, new arrhythmia, etc.)[36] Another study by Maa and Sullivan looked at late ophthalmic cancellations at a Veterans Affairs (VA) medical center and found that nearly 30% were due to medical reasons. Of the patients cancelled for medical reasons, approximately 36% were due to vascular causes including myocardial infarction, arrhythmia, high blood pressure, stroke symptoms and chest pain. Another 10% of these cancellations were due to pulmonary causes including hypoxia. The remaining medical reasons for cancellation included anemia, polycythemia, continuing anticoagulants and elevated blood glucose levels greater than 300 mg/dL.[37] It is interesting to note that Maa's analysis took into account the 13.3% of patients who were felt to be high-risk for ophthalmic surgery at the time of clinical evaluation and were referred for medical clearance in advance of elective surgery. Despite this clearance, nearly one-third of patients were cancelled on presentation for surgery due to concerning medical reasons. Elevated blood pressure and glucose levels, arrhythmia, anemia and hypoxia are significant medical concerns that can lead to intraoperative and post-operative complications.[38,39] In the emergent setting of macula-sparing RRD, some of the medical reasons for cancellation in the above studies may be tolerated in favor of better visual outcomes. In these instances, there may be little or no effort to delay surgery in order to evaluate patients with systemic pathology because of the concern for impending macular detachment.[13] Cardiovascular or internal medicine clearance prior to surgery, within an appropriate time frame, may allow for improved systemic outcomes while maintaining visual outcomes. Short-term positioning, bed rest and/or bilateral patching to reduce the height and progression of retinal detachment may be a consideration during this time period if necessary.[40,41,42,43,44,45]
COST ANALYSIS OF EMERGENCY SURGERY
Several studies have outlined cost-analysis for treatment of retinal disease such as age-related macular degeneration and macular edema, but this same analysis is mostly lacking in retinal detachment repair.[46,47,48] Chang reported a total cost ranging from $2,763 to $7,940 for repair of primary RRD depending on treatment modality (pneumatic retinopexy, scleral buckle, or pars plana vitrectomy), and practice and surgical setting.[49]
Hartz et al found a 25% greater cost incurred for patients undergoing emergency retinal detachment surgery due to the difference in pay scales to support personnel.[13] It is noteworthy that none of the 18 patients with macula-sparing RRD progressed to involve the macula while awaiting scheduled surgery in Hartz's study. Hartz also found no evidence that delaying surgery contributed to a worse visual outcome regardless of the status of the macula. Aside from the cost-analysis findings, the most important observation in this study was that patient characteristics greatly influenced how surgery was scheduled. Patients thought to have a more acute detachment, no pre-existing optic nerve or macular pathology (greater visual potential) and little subretinal fluid, more often had surgery on an emergent basis. These and other prognostic indicators at presentation may prove to be the most important factors in determining the rate at which a macula-sparing RRD will progress to involve the macula. It is possible that individual genetic and anatomic differences may render the retina-RPE adhesion more or less susceptible to progression of an RRD.[50] Further analysis of these indicators is imperative so that emergent or scheduled surgery can be performed in the best interest of the patient's co-existing systemic conditions, psychosocial issues and personal needs, while taking into account the additional risks and costs of unnecessary emergency surgery.
Another factor which will likely matter in the United States in the near future has to do with the Patient Protection and Affordable Care Act which directs the Centers for Medicare and Medicaid Services to provide information about each surgeon's use of resources and the quality of care provided to patients.[51] The increased use of resources in emergent surgery will need to be justified by the quality of care and final visual, anatomic and possibly even systemic outcomes.
DISCUSSION
Without question, every reasonable effort should be made to perform surgery on macula-sparing RRDs prior to detachment of the macula, thereby allowing for the best possible functional outcomes. The critical query, however, remains: How long before the macula will detach? A controlled, prospective trial to answer this question is impractical and unethical. In certain instances, scheduled surgery for macula-sparing RRD can benefit the patient and decrease unnecessary costs to the health care system, while still allowing excellent final visual results. Further analysis of high-risk indicators leading to progression of macula-sparing RRD would prove useful in determining those patients that can safely wait for scheduled surgery. Factors such as the timing of presentation, examination findings (location of detachment, vitreous syneresis, operculated versus tractional retinal defects, signs of chronicity), case complexity, patient's co-existing medical conditions, surgeon expertise, and timing and quality of access to operating facilities and staff should all be considered in determining whether a macula-sparing RRD requires immediate intervention or, in fact, the patient would do better with scheduled surgery within an appropriate time frame.
REFERENCES
- 1.Burton TC. Recovery of visual acuity after retinal detachment involving the macula. Trans Am Ophthalmol Soc. 1982;80:475–497. [PMC free article] [PubMed] [Google Scholar]
- 2.Hassan TS, Sarrafizadeh R, Ruby AJ, Garretson BR, Kuczynski B, Williams GA. The effect of duration of macular detachment on results after the scleral buckle repair of primary, macula-off retinal detachments. Ophthalmology. 2002;109:146–152. doi: 10.1016/s0161-6420(01)00886-7. [DOI] [PubMed] [Google Scholar]
- 3.Ross WH, Kozy DW. Visual recovery in macula-off rhegmatogenous retinal detachments. Ophthalmology. 1998;105:2149–2153. doi: 10.1016/S0161-6420(98)91142-3. [DOI] [PubMed] [Google Scholar]
- 4.Ross WH. Visual recovery after macula-off retinal detachment. Eye (Lond) 2002;16:440–446. doi: 10.1038/sj.eye.6700192. [DOI] [PubMed] [Google Scholar]
- 5.Mowatt L, Shun-Shin GA, Arora S, Price N. Macula off retinal detachments. How long can they wait before it is too late? Eur J Ophthalmol. 2005;15:109–117. [PubMed] [Google Scholar]
- 6.Mitry D, Awan MA, Borooah S, Syrogiannis A, Lim-Fat C, Campbell H, et al. Long-term visual acuity and the duration of macular detachment: Findings from a prospective population-based study. Br J Ophthalmol. 2013;97:149–152. doi: 10.1136/bjophthalmol-2012-302330. [DOI] [PubMed] [Google Scholar]
- 7.Diederen RM, La Heij EC, Kessels AG, Goezinne F, Liem AT, Hendrikse F. Scleral buckling surgery after macula-off retinal detachment: Worse visual outcome after more than 6 days. Ophthalmology. 2007;114:705–709. doi: 10.1016/j.ophtha.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Lo WR, Kim SJ, Srivastava SK. Timing of detachment surgery. Ophthalmology. 2008;115:586–587. doi: 10.1016/j.ophtha.2007.08.040. [DOI] [PubMed] [Google Scholar]
- 9.Salicone A, Smiddy WE, Venkatraman A, Feuer W. Visual recovery after scleral buckling procedure for retinal detachment. Ophthalmology. 2006;113:1734–1742. doi: 10.1016/j.ophtha.2006.03.064. [DOI] [PubMed] [Google Scholar]
- 10.Kubay OV, Charteris DG, Newland HS, Raymond GL. Retinal detachment neuropathology and potential strategies for neuroprotection. Surv Ophthalmol. 2005;50:463–475. doi: 10.1016/j.survophthal.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Chang CJ, Lai WW, Edward DP, Tso MO. Apoptotic photoreceptor cell death after traumatic retinal detachment in humans. Arch Ophthalmol. 1995;113:880–886. doi: 10.1001/archopht.1995.01100070054025. [DOI] [PubMed] [Google Scholar]
- 12.The repair of rhegmatogenous retinal detachments. American Academy of Ophthalmology. Ophthalmology. 1996;103:1313–1324. doi: 10.1016/s0161-6420(96)30505-8. [DOI] [PubMed] [Google Scholar]
- 13.Hartz AJ, Burton TC, Gottlieb MS, McCarty DJ, Williams DF, Prescott A, et al. Outcome and cost analysis of scheduled versus emergency scleral buckling surgery. Ophthalmology. 1992;99:1358–1363. [PubMed] [Google Scholar]
- 14.Williamson TH, Shunmugam M, Rodrigues I, Dogramaci M, Lee E. Characteristics of rhegmatogenous retinal detachment and their relationship to visual outcome. Eye (Lond) 2013;27:1063–1069. doi: 10.1038/eye.2013.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilkinson CP. Visual results following scleral buckling for retinal detachments sparing the macula. Retina. 1981;1:113–116. doi: 10.1097/00006982-198101020-00007. [DOI] [PubMed] [Google Scholar]
- 16.Wykoff CC, Smiddy WE, Mathen T, Schwartz SG, Flynn HW, Jr, Shi W. Fovea-sparing retinal detachments: Time to surgery and visual outcomes. Am J Ophthalmol. 2010;150:205–210.e2. doi: 10.1016/j.ajo.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 17.Ho SF, Fitt A, Frimpong-Ansah K, Benson MT. The management of primary rhegmatogenous retinal detachment not involving the fovea. Eye (Lond) 2006;20:1049–1053. doi: 10.1038/sj.eye.6702083. [DOI] [PubMed] [Google Scholar]
- 18.Ehrlich R, Niederer RL, Ahmad N, Polkinghorne P. Timing of acute macula-on rhegmatogenous retinal detachment repair. Retina. 2013;33:105–110. doi: 10.1097/IAE.0b013e318263ceca. [DOI] [PubMed] [Google Scholar]
- 19.Lai MM, Khan N, Weichel ED, Berinstein DM. Anatomic and visual outcomes in early versus late macula-on primary retinal detachment repair. Retina. 2011;31:93–98. doi: 10.1097/IAE.0b013e3181de55f0. [DOI] [PubMed] [Google Scholar]
- 20.Desai VR, Jea A, Gonda DD, Lam S, Luerssen TG. The effect of weekend and after-hours surgery on morbidity and mortality rates in pediatric neurosurgery. Neurosurgery. 2015;62:231. doi: 10.3171/2015.6.PEDS15184. [DOI] [PubMed] [Google Scholar]
- 21.Moghadamyeghaneh Z, Carmichael JC, Smith BR, Mills S, Pigazzi A, Nguyen NT, et al. A comparison of outcomes of emergent, urgent, and elective surgical treatment of diverticulitis. Am J Surg. 2015;210:838–845. doi: 10.1016/j.amjsurg.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 22.Kukreja S, Ambekar S, Ahmed OI, Menger RP, Sin AH, Nanda A. Impact of elective versus emergent admission on perioperative complications and resource utilization in lumbar fusion. Clin Neurol Neurosurg. 2015;136:52–60. doi: 10.1016/j.clineuro.2015.05.015. [DOI] [PubMed] [Google Scholar]
- 23.Tadisina KK, Chopra K, Singh DP. The “weekend effect” in plastic surgery: Analyzing weekday versus weekend admissions in body contouring procedures from 2000 to 2010. Aesthet Surg J. 2015;35:995–998. doi: 10.1093/asj/sjv088. [DOI] [PubMed] [Google Scholar]
- 24.Zapf MA, Kothari AN, Markossian T, Gupta GN, Blackwell RH, Wai PY, et al. The “weekend effect” in urgent general operative procedures. Surgery. 2015;158:508–514. doi: 10.1016/j.surg.2015.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stone TW, editor. ASRS 2015 Preferences and Trends Membership Survey. Chicago, IL: American Society of Retina Specialists; 2015. [Google Scholar]
- 26.Heng M, Wright JG. Dedicated operating room for emergency surgery improves access and efficiency. Can J Surg. 2013;56:167–174. doi: 10.1503/cjs.019711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frimpong-Ansah K, Kirkby GR. Arrangements for the management of urgent retinal detachments in the United Kingdom and Eire in the year 2000: Results of a survey. Eye (Lond) 2002;16:754–760. doi: 10.1038/sj.eye.6700326. [DOI] [PubMed] [Google Scholar]
- 28.Rojas J, Fernández I, Pastor JC, Gómez-Ulla F, Piñero A. Urgent retinal detachment management by the National Health System of Spain. Project retina 2. Arch Soc Esp Oftalmol. 2007;82:279–284. doi: 10.4321/s0365-66912007000500006. [DOI] [PubMed] [Google Scholar]
- 29.Leaver PK. Trends in vitreoretinal surgery – Time to stop and think. Br J Ophthalmol. 1999;83:385–386. doi: 10.1136/bjo.83.4.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mitry D, Charteris DG, Yorston D, Siddiqui MA, Campbell H, Murphy AL, et al. The epidemiology and socioeconomic associations of retinal detachment in Scotland: A two-year prospective population-based study. Invest Ophthalmol Vis Sci. 2010;51:4963–4968. doi: 10.1167/iovs.10-5400. [DOI] [PubMed] [Google Scholar]
- 31.Slack PS, Coulson CJ, Ma X, Webster K, Proops DW. The effect of operating time on surgeons' muscular fatigue. Ann R Coll Surg Engl. 2008;90:651–657. doi: 10.1308/003588408X321710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Waqar S, Park J, Kersey TL, Modi N, Ong C, Sleep TJ. Assessment of fatigue in intraocular surgery: Analysis using a virtual reality simulator. Graefes Arch Clin Exp Ophthalmol. 2011;249:77–81. doi: 10.1007/s00417-010-1531-6. [DOI] [PubMed] [Google Scholar]
- 33.Jackson TL, Donachie PH, Sallam A, Sparrow JM, Johnston RL. United Kingdom national ophthalmology database study of vitreoretinal surgery: Report 3, retinal detachment. Ophthalmology. 2014;121:643–648. doi: 10.1016/j.ophtha.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 34.Mazinani BA, Rajendram A, Walter P, Roessler GF. Does surgical experience have an effect on the success of retinal detachment surgery? Retina. 2012;32:32–37. doi: 10.1097/IAE.0B013E3182411CD2. [DOI] [PubMed] [Google Scholar]
- 35.Koch KR, Hermann MM, Kirchhof B, Fauser S. Success rates of retinal detachment surgery: Routine versus emergency setting. Graefes Arch Clin Exp Ophthalmol. 2012;250:1731–1736. doi: 10.1007/s00417-012-2007-7. [DOI] [PubMed] [Google Scholar]
- 36.Henderson BA, Naveiras M, Butler N, Hertzmark E, Ferrufino-Ponce Z. Incidence and causes of ocular surgery cancellations in an ambulatory surgical center. J Cataract Refract Surg. 2006;32:95–102. doi: 10.1016/j.jcrs.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 37.Maa A, Sullivan BR. Medical reasons for same-day cancellations in ophthalmic surgery at a VA hospital. Fed Pract. 2010;27:17–21. [Google Scholar]
- 38.Aguirre-Córdova JF, Chávez-Vázquez G, Huitrón-Aguilar GA, Cortés-Jiménez N. Why is surgery cancelled. Causes, implications, and bibliographic antecedents? Gac Med Mex. 2003;139:545–551. [PubMed] [Google Scholar]
- 39.Hand R, Levin P, Stanziola A. The causes of cancelled elective surgery. Qual Assur Util Rev. 1990;5:2–6. doi: 10.1177/0885713x9000500102. [DOI] [PubMed] [Google Scholar]
- 40.Tewari A, Shah GK. Management of primary retinal detachments. Rev Ophthalmol. 2006;13:62–68. [Google Scholar]
- 41.Lin T, Mieler WF. Management of primary rhegmatogenous RD. Rev Ophthalmol. 2008;15:57–65. [Google Scholar]
- 42.Foster WJ. Bilateral patching in retinal detachment: Fluid mechanics and retinal “settling”. Invest Ophthalmol Vis Sci. 2011;52:5437–5440. doi: 10.1167/iovs.11-7249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Algvere P, Rosengren B. Immobilization of the eye. Evaluation of a new method in retinal detachment surgery. Acta Ophthalmol (Copenh) 1977;55:303–316. doi: 10.1111/j.1755-3768.1977.tb01312.x. [DOI] [PubMed] [Google Scholar]
- 44.Lincoff H, Stopa M, Kreissig I. Ambulatory binocular occlusion. Retina. 2004;24:246–253. doi: 10.1097/00006982-200404000-00010. [DOI] [PubMed] [Google Scholar]
- 45.Hofmann H, Hanselmayer H. Retinal detachment: Extent and occurrence of reattachment using preoperative immobilization. Klin Monbl Augenheilkd. 1973;162:178–185. [PubMed] [Google Scholar]
- 46.Smiddy WE. Relative cost of a line of vision in age-related macular degeneration. Ophthalmology. 2007;114:847–854. doi: 10.1016/j.ophtha.2006.10.038. [DOI] [PubMed] [Google Scholar]
- 47.Smiddy WE. Economic considerations of macular edema therapies. Ophthalmology. 2011;118:1827–1833. doi: 10.1016/j.ophtha.2010.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Smiddy WE. Clinical applications of cost analysis of diabetic macular edema treatments. Ophthalmology. 2012;119:2558–2562. doi: 10.1016/j.ophtha.2012.09.015. [DOI] [PubMed] [Google Scholar]
- 49.Chang JS, Smiddy WE. Cost-effectiveness of retinal detachment repair. Ophthalmology. 2014;121:946–951. doi: 10.1016/j.ophtha.2013.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vrabec TR, Baumal CR. Demarcation laser photocoagulation of selected macula-sparing rhegmatogenous retinal detachments. Ophthalmology. 2000;107:1063–1067. doi: 10.1016/s0161-6420(00)00091-9. [DOI] [PubMed] [Google Scholar]
- 51.Tornambe P. Reply: Does surgical experience have an effect on the success of retinal detachment surgery? Retina. 2012;32:1693–1694. doi: 10.1097/IAE.0b013e318260af0f. [DOI] [PubMed] [Google Scholar]


