Abstract
Purpose:
To report a complication pertaining to subconjunctival bevacizumab injection as an adjunct to Ahmed Glaucoma Valve (AGV) implantation.
Case Report:
A 54-year-old woman with history of complicated cataract surgery was referred for advanced intractable glaucoma. AGV implantation with adjunctive subconjunctival bevacizumab (1.25 mg) was performed with satisfactory results during the first postoperative week. However, 10 days after surgery, she developed wound dehiscence and tube exposure. The second case was a 33-year-old man with history of congenital glaucoma and uncontrolled IOP who developed AGV exposure and wound dehiscence after surgery. In both cases, for prevention of endophthalmitis and corneal damage by the unstable tube, the shunt was removed and the conjunctiva was re-sutured.
Conclusion:
The potential adverse effect of subconjunctival bevacizumab injection on wound healing should be considered in AGV surgery.
Keywords: Ahmed Glaucoma Valve, Bevacizumab, Plate Exposure, Tube Exposure, Tube Migration
INTRODUCTION
Glaucoma drainage devices (GDD) have been widely accepted in the management of refractory glaucomas.[1] GDDs have significantly improved the management of glaucoma patients but could be associated with various complications such as tube migration, tube or plate exposure or extrusion, ocular motility disturbance and infection.[2] Erosion of the conjunctiva and exposure of GDDs remains a risk factor for the development of endophthalmitis.[3] Herein, we describe two cases of wound dehiscence and shunt displacement after subconjunctival bevacizumab injection as an adjunct to AGV implantation and report the management of this complication.
CASE REPORT
A 54-year-old woman was referred to Rassoul Akram hospital, Tehran, Iran for uncontrolled glaucoma. She had history of complicated cataract surgery about 20 years ago on the left eye and was aphakic at the time of presentation. Best corrected vision was 20/200, intraocular pressure (IOP) was 45 mmHg, cup-to-disc (C/D) ratio was 0.8, and the superior conjunctiva was scarred from prior surgery. The patient was started on timolol-dorzolamide, brimonidine, and latanoprost and was visited a week later. At that time, IOP was 30 mmHg which was not low enough considering the advanced glaucoma.
The patient underwent an uneventful AGV implantation in the superotemporal quadrant under general anesthesia. After preparing a fornix-based flap, the AGV was primed and secured to the sclera using 7-0 silk sutures. The tube was inserted into the anterior chamber (AC) and secured by 10-0 nylon. At the end of the procedure, a scleral patch graft was sutured over the tube using 10-0 nylon, and the conjunctiva was closed using an 8-0 Vicryl running suture. As an adjunctive measure, 1.25 mg (0.05 ml) bevacizumab was injected subconjunctivally adjacent to the AGV plate.
The day after surgery, IOP was 13, the wound was secure, and the tube was in a good position. The patient was discharged with betamethasone eye drops six times, and ciprofloxacin drops four times a day. Everything remained the same on day 4 after surgery, but on day 10, although IOP was 14 mmHg and visual acuity was stable, the patient complained of pain and copious discharge. On slit lamp examination, the tube was in a good position and the anterior chamber and vitreous were clear; however copious discharge was present around the sutures. The patient was admitted to the hospital with a suspected diagnosis of suture infection. Fortified topical vancomycin and ceftazidime were started every one hour, and betamethasone was discontinued. On day 3 after admission, anterior migration of the tube and complete wound dehiscence was observed [Figures 1 and 2]. For prevention of further complications such as tube-corneal touch, the AGV was explanted and the wound was repaired using 10/0 nylon sutures; the GDD was sent to the laboratory for smears and bacterial culture which were negative. At the time of surgery, the scleral patch graft was found to be necrotic, but no sign of infection around the tube or plate was detected. The eye was quiet with no conjunctival discharge the day after surgery.
Figure 1.

Wound dehiscence and scleral exposure in the first patient, 10 days after Ahmed Glaucoma Valve implantation with adjunctive subconjunctival bevacizumab.
Figure 2.
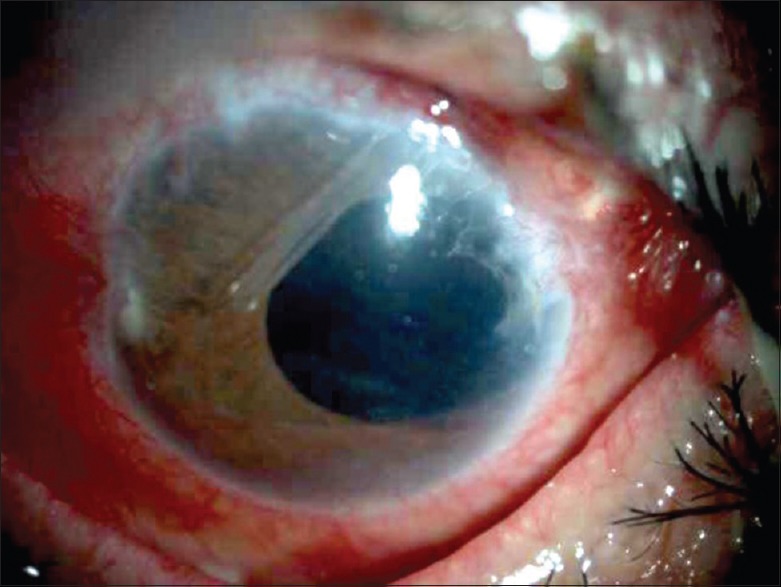
Tube migration after Ahmed Glaucoma Valve implantation with adjunctive subconjunctival bevacizumab in the first patient.
The second case was a 33-year-old man with history of congenital glaucoma. He had undergone trabeculectomy three times before and was pseudophakic at presentation. IOP was 38 mmHg with full medications, and C/D ratio was 0.9. He underwent uneventful AGV implantation and bevacizumab injection using the same technique described above. IOP was 12 mmHg the day after surgery, and the wound was secure. The patient was discharged on betamethasone eye drops six times a day and ciprofloxacin four times a day. The patient did not return for follow-up until 5 months after surgery when was seen complaining of foreign body sensation during this period. Slit lamp examination revealed that the AGV plate was completely exposed and had migrated toward the limbus, but there was no sign of infection or inflammation. During repeat surgery, migration of the AGV and melting of the scleral patch graft were observed [Figure 3]. The device was explanted and the conjunctiva was sutured using 10-0 nylon.
Figure 3.

Plate exposure in the second patient 5 months after Ahmed Glaucoma Valve implantation with adjunctive subconjunctival bevacizumab.
DISCUSSION
AGV implantation is an effective surgical procedure for controlling refractory glaucomas.[1] Although IOP may successfully be controlled, conjunctival complications can occur after surgery. Conjunctival dehiscence is usually a benign complication which does not need repair as long as the tube is well covered. AGV tube or plate exposures are less common, occur later and need urgent repair.[4]
Reasons for conjunctival erosion over patch grafts and the AGV tube are not clear and the condition is probably multifactorial. Mechanical rubbing of the eyelid margin against the patch graft, excessive conjunctival tension over the device, tube malposition, lack of a smooth tapered surface between the patch graft and the host with poor ocular lubrication, and even minute amounts of absolute alcohol retained in the donor sclera might cause these problems.[5] Tube exposure following conjunctival erosion with AGV implants appears to be a major risk factor for development of endophthalmitis.[3]
Black race, diabetes mellitus, use of a high number of glaucoma medications before shunt implantation, history of multiple glaucoma laser procedures, the combination of aqueous shunt implantation with another surgery and inferior location of shunt are risk factors associated with erosion.[6,7]
Herein, we described two patients with conjunctival dehiscence and AGV plate displacement after adjunctive subconjunctival injection of bevacizumab. Both patients had history of chronic use of anti-glaucoma medications and glaucoma surgery. In an evaluation of 158 patients with AGV implantation, Geffen et al reported 8.9% plate or tube exposure 8 months to 4 years after surgery,[4] but we assume that the rapid exposure we observed in our patients may be related to bevacizumab injection.
The function of vascular endothelial growth factor (VEGF) isoforms in pathological angiogenesis and wound healing in the eye still remains unidentified.[6] Wound healing involves a complex interaction between humoral and cellular responses as a consequence of tissue injury and bleeding. VEGF is crucial for angiogenesis and formation of granulation tissue during wound repair and has been proposed to play a role in the healing response principally by promotion of angiogenesis. It has also been shown to be important in epithelialization and collagen deposition.[8,9]
There is mounting evidence on the role of anti-VGEF agents in reducing scar formation after glaucoma surgery, but there is little evidence on the role of VEGF and its complications in shunt surgery.[10] In a prospective study in pediatric glaucoma, Mahdy showed that the adjunctive use of bevacizumab or mitomycin C during AGV implantation significantly enhances shunt survival, while bevacizumab seems to be much safer with no visually devastating complications.[11]
In a pilot study, Chua et al used subconjunctival bevacizumab with 5-fluorouracil and compared it with 5-fluorouracil alone after trabeculectomy augmented with mitomycin. Two eyes from the 5-FU/bevacizumab group experienced a bleb-related complication within 3 months of surgery: One case of blebitis and one case of suture-related abscess with secondary blebitis. They recommended further evaluation of the safety and efficacy of bevacizumab as a modulating agent in glaucoma filtration surgery.[12]
There are reports on the possible role of bevacizumab in delaying corneal wound healing. Kim et al evaluated the effect of bevacizumab on the duration of corneal wound healing and cell growth and showed that application of topical bevacizumab at concentrations of 0, 0.5, 1.0, 1.5, 2.5, or 5 mg/mL, twice daily, to mechanically debrided epithelia of rabbit corneas delayed corneal wound healing.[13] Rojo-Arnao et al reported preliminary findings of adjunctive subconjunctival bevacizumab (SCB) injections in patients undergoing AGV implantation and described less aggressive hypertensive period as measured by post-massage IOP measurements, postoperative glaucoma medications, and cross-sectional bleb area by ultrasound.[14]
We injected 1.25 mg bevacizumab into the subconjunctival space to improve the outcome of implantation, but observed wound dehiscence and loosening of absorbable sutures in both patients. Although wound dehiscence may be related to chronic use of medications or previous surgeries, displacement of the shunt plate and loosening of sutures may be related to bevacizumab. Since any infection at the site of sutures might predispose patient to endophthalmitis, we admitted the first case for close observation, but no sign of AC or vitreous reaction were detected afterward. Moreover, we did not find any sign of infection during explantation of the device and no positive laboratory results suggesting infection. In the second case, the patient complained of foreign body sensation long before admission, but the exact time of wound dehiscence remained undetermined. In both eyes, the conjunctiva had been sutured by Vicryl sutures, and we suspect that the combination of bevacizumab and these sutures could be a predisposing factor for wound dehiscence.
In summary, we have reported two cases of wound dehiscence after subconjunctival injection of bevacizumab.
Since this complication may be attributed to the adjunctive bevacizumab, extra caution and close follow-up in addition to the use of non-absorbable sutures may be advised in such cases.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Wylegala E, Tarnawska D, Lyssek-Boron A, Bilinska B, Jurewicz A, Petela A. A clinical study of the Ahmed glaucoma valve implant in refractory glaucoma. Klin Oczna. 2005;107:221–225. [PubMed] [Google Scholar]
- 2.Bailey AK, Sarkisian SR., Jr Complications of tube implants and their management. Curr Opin Ophthalmol. 2014;25:148–153. doi: 10.1097/ICU.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 3.Al-Torbak AA, Al-Shahwan S, Al-Jadaan I, Al-Hommadi A, Edward DP. Endophthalmitis associated with the Ahmed glaucoma valve implant. Br J Ophthalmol. 2005;89:454–458. doi: 10.1136/bjo.2004.049015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geffen N, Buys YM, Smith M, Anraku A, Alasbali T, Rachmiel R, et al. Conjunctival complications related to Ahmed glaucoma valve insertion. J Glaucoma. 2014;23:109–114. doi: 10.1097/IJG.0b013e31826ab693. [DOI] [PubMed] [Google Scholar]
- 5.Dubey S, Prasanth B, Acharya MC, Narula R. Conjunctival erosion after glaucoma drainage device surgery: A feasible option. Indian J Ophthalmol. 2013;61:355–357. doi: 10.4103/0301-4738.99852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huddleston SM, Feldman RM, Budenz DL, Bell NP, Lee DA, Chuang AZ, et al. Aqueous shunt exposure: A retrospective review of repair outcome. J Glaucoma. 2013;22:433–438. doi: 10.1097/IJG.0b013e3181f3e5b4. [DOI] [PubMed] [Google Scholar]
- 7.Pakravan M, Yazdani S, Shahabi C, Yaseri M. Superior versus inferior Ahmed glaucoma valve implantation. Ophthalmology. 2009;116:208–213. doi: 10.1016/j.ophtha.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Grimm D, Bauer J, Schoenberger J. Blockade of neoangiogenesis, a new and promising technique to control the growth of malignant tumors and their metastases. Curr Vasc Pharmacol. 2009;7:347–357. doi: 10.2174/157016109788340640. [DOI] [PubMed] [Google Scholar]
- 9.Jain L, Vargo CA, Danesi R, Sissung TM, Price DK, Venzon D, et al. The role of vascular endothelial growth factor SNPs as predictive and prognostic markers for major solid tumors. Mol Cancer Ther. 2009;8:2496–2508. doi: 10.1158/1535-7163.MCT-09-0302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li Z, Van Bergen T, Van de Veire S, Van de Vel I, Moreau H, Dewerchin M, et al. Inhibition of vascular endothelial growth factor reduces scar formation after glaucoma filtration surgery. Invest Ophthalmol Vis Sci. 2009;50:5217–5225. doi: 10.1167/iovs.08-2662. [DOI] [PubMed] [Google Scholar]
- 11.Mahdy RA. Adjunctive use of bevacizumab versus mitomycin C with Ahmed valve implantation in treatment of pediatric glaucoma. J Glaucoma. 2011;20:458–463. doi: 10.1097/IJG.0b013e3181efbea5. [DOI] [PubMed] [Google Scholar]
- 12.Chua BE, Nguyen DQ, Qin Q, Ruddle JB, Wells AP, Niyadurupola N, et al. Bleb vascularity following post-trabeculectomy subconjunctival bevacizumab: A pilot study. Clin Experiment Ophthalmol. 2012;40:773–779. doi: 10.1111/j.1442-9071.2012.02798.x. [DOI] [PubMed] [Google Scholar]
- 13.Kim TI, Chung JL, Hong JP, Min K, Seo KY, Kim EK. Bevacizumab application delays epithelial healing in rabbit cornea. Invest Ophthalmol Vis Sci. 2009;50:4653–4659. doi: 10.1167/iovs.08-2805. [DOI] [PubMed] [Google Scholar]
- 14.Rojo-Arnao M, Albis-Donado OD, Lliteras-Cardin M, Kahook MY, Gil-Carrasco F. Adjunctive bevacizumab in patients undergoing Ahmed valve implantation: A pilot study. Ophthalmic Surg Lasers Imaging. 2011;42:132–137. doi: 10.3928/15428877-20110316-02. [DOI] [PubMed] [Google Scholar]


