Abstract
Purpose:
To evaluate long-term follow-up data on implantation of a full-ring intra-corneal implant (MyoRing) for management of keratoconus.
Methods:
A total of 40 keratoconic eyes of 37 consecutive patients who had undergone MyoRing implantation using the Pocket Maker microkeratome (Dioptex, GmbH, Linz, Austria) and completed 3 years of follow-up appointments were included in this retrospective study. Uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), refraction and keratometry (K) readings were measured and evaluated preoperatively, and 3 years, postoperatively.
Results:
No intraoperative complications were observed in this case series. Three years postoperatively, there was a significant improvement in UDVA, CDVA, K readings, spherical equivalent (SE), and manifest sphere and cylinder (P < 0.05 for all comparisons). UDVA was significantly improved from 1.14 ± 0.27 to 0.30 ± 0.21 LogMAR (P = 0.001), CDVA was also improved from 0.52 ± 0.23 to 0.18 ± 0.12 LogMAR (P = 0.001), SE was decreased by 4.35 diopters (D) and average keratometric values were reduced by 2.34 D (P = 0.001). Overall, 81% of subjects were moderately to highly satisfied 3 years after surgery and 64.90% agreed to have the fellow eye implanted with MyoRing.
Conclusion:
MyoRing implantation using the Pocket Maker microkeratome was found to be a minimally invasive procedure for improving visual acuity and refraction in the majority of the patients with keratoconus.
Keywords: Cornea, Intrastromal Corneal Ring, Keratoconus, MyoRing
INTRODUCTION
Keratoconus is a bilateral, progressive, non-inflammatory ectatic corneal disease of unknown etiology which impairs visual function due to corneal thinning and protrusion.[1,2,3] Management of keratoconus includes spectacles,[1,4] contact lenses,[5] collagen crosslinking (CXL),[6] intracorneal ring segments (ICRSs),[7,8,9,10,11] deep anterior lamellar keratoplasty, and penetrating keratoplasty (PK).[12,13,14]
ICRSs play a pivotal role in the management of keratoconus by flattening the central cornea via an “arc-shortening” effect on the corneal lamellae.[15] However several complications, including non-concentric tunnels and segment extrusion, as well as the presence of perplexing nomograms limit the advantages of ICRSs.[16,17] Corneal intrastromal implantation system (CISIS) using the Pocket Maker microkeratome (Dioptex, GmbH, Linz, Austria) and the MyoRing intracorneal implant (Dioptex, GmbH, Linz, Austria) are a surgical option whereby a flexible full-ring implant is inserted into a corneal pocket for treatment of keratoconus,[18,19] post-LASIK keratectasia,[20] as well as moderate and high myopia.[21] MyoRing is a flexible, full-ring polymethylmetacrylate (PMMA) intracorneal implant, available in diameters ranging from 5 to 6 mm and thickness ranging from 200 to 400 μm in 20 μm increments. The anterior surface is convex, and the posterior surface is concave, with a radius of curvature of 8.00 mm.[21]
Reports on long-term outcomes and late complications of implantation of this type of intrastromal implants are scarce. The present study evaluates the visual and refractive outcomes of MyoRing implantation in eyes with keratoconus using the mechanical Pocket Maker microkeratome technology. We included keratoconic patients who had completed at least three years of follow-up examinations.
METHODS
Of 65 patients (69 eyes) who had been operated during the study period, twenty patients (21 eyes) were unable to attend follow-up appointments and were thus excluded from the study. Of the 44 patients (48 eyes) with complete follow-up, seven patients (eight eyes) were excluded because of additional interventions including MyoRing removal or exchange, or DALK. A total of 37 patients (40 eyes) with moderate and severe keratoconus, aged 18 and 45 years remained in this retrospective study.
All eyes had undergone (Dioptex, GmbH, Linz, Austria) implantation using the Pocket Maker microkeratome (Dioptex, GmbH, Linz, Austria) from October 2010 to June 2011 at Bina Eye Hospital, Tehran, Iran. The Institutional Review Board of the Eye Research Center approved this study, and the tenets of the Declaration of Helsinki were followed.
Keratoconus diagnosis was based on corneal topography and slit lamp examination.[1] Inclusion criteria were keratoconic patients with no corneal scar, minimum corneal thickness of 360 microns, contact lens intolerance and uncorrected distance visual acuity (UDVA) worse than 20/50. Exclusion criteria for surgery were pregnancy, breast-feeding, history of vernal and atopic keratoconjunctivitis, history of keratorefractive surgery in the scheduled eye, presence of dry eye, history of corneal stromal disorders, hyperopia and patients with other ocular and systemic comorbidities.
A comprehensive ophthalmic examination was performed pre- and postoperatively in all cases which included measurement of unorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), manifest refraction (sphere and cylinder), ultrasonic pachymetry, fundus examination, slit lamp biomicroscopy and corneal topography.
The MyoRing dimensions were selected according to the MyoRing nomogram based on theoretical calculation derived from an experimental biomechanical corneal model.[22,23,24,25] This nomogram takes into account mean central keratometry and corneal thickness at the thinnest point.[18] Orbscan II topography system (Bausch and Lomb) was used to evaluate the anterior and posterior corneal surfaces. Visual acuity was measured using the Snellen chart and then converted to logarithm of minimum angle of resolution (LogMAR) notations for statistical analysis.
All surgical procedures were performed by the same experienced surgeon (K.J.) under topical anesthesia. The central point of the site of intrastromal corneal ring implantation was marked under the operation microscope (OMS-800 Standard, TOPCON Corporation, Japan). All procedures were performed with a temporal approach using self-sealing incisions. A pocket was created in the 9-mm central corneal at a depth of 300 microns using a Pocket Maker microkeratome. Then, the Myoring was implanted into the corneal pocket.[19,20,21] The position of the implant was adjusted intraoperatively using a handheld keratoscope [Figure 1]. At the conclusion of the operation, a bandage contact lens was placed on the cornea.
Figure 1.
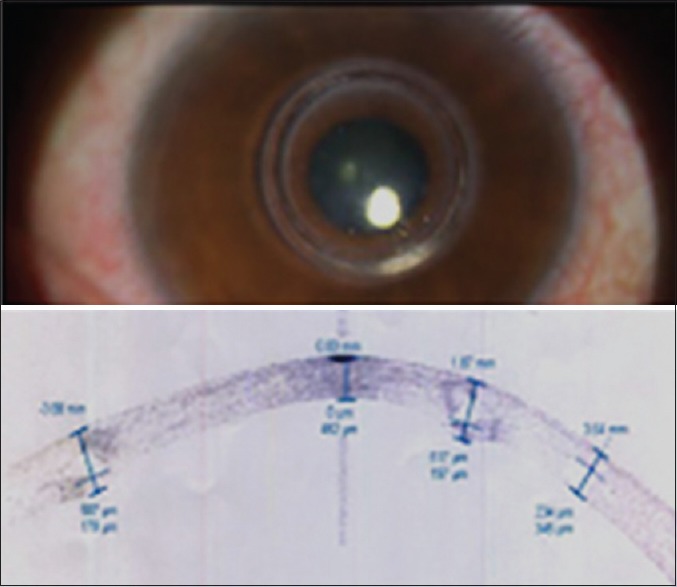
MyoRing implant in a keratoconic eye.
Postoperatively, all eyes were medicated with bethamethasone 0.1% eye drops (Sina Darou, Tehran, Iran) 4 times a day, chloramphenicol 0.5% eye drops (Sina Darou, Tehran, Iran) 4 times a day, and non-preserved artificial tear (Artelac) (Baush and Lomb, France, SAS) 4 times a day. Chloramphenicol eye drops were discontinued 1 week postoperatively, and betamethasone eye drops were tapered off over 4-6 weeks. Bandage contact lenses were removed on the first postoperative day.
Safety of the procedure was assessed using a refractive surgery safety index given below:
Safety index = (postoperative CDVA)/(preoperative CDVA)
Efficacy of the procedure was assessed using a refractive surgery efficacy index given below:
Efficacy index = (postoperative UDVA)/(preoperative CDVA).[26,27]
Overall satisfaction was assessed using a 6-point Likert scale: 0 - no satisfaction, 1 - very little satisfaction, 2 - little satisfaction, 3 - moderate satisfaction, 4 - much satisfaction, 5 - very much satisfaction.
Statistical analysis was performed with SPSS software (IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp). Continuous variables are presented in mean and standard deviations while qualitative variables are reported in frequencies (percentages). The paired t-test was used to compare pre-and postoperative values including UDVA, CDVA, SE, maximum keratometry, minimum keratometry, and average keratometry. P values less than 0.05 were considered as statistically significant.
RESULTS
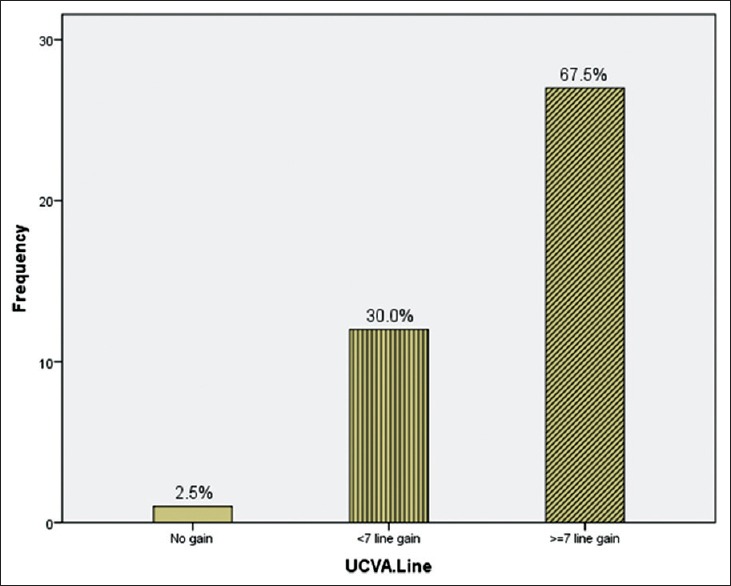
A total of 40 eyes of 37 patients with mean age of 28.2 ± 12 (range 18 to 45) years, including 19 male (51.3%) and 18 female (48.7%) subjects, were analyzed. UDVA and CDVA were improved significantly in all patients as compared to preoperative values [Table 1]. Mean UDVA was improved from 1.14 LogMAR preoperatively to 0.30 LogMAR postoperatively (P< 0.001), and mean CDVA was improved from 0.52 to 0.18 LogMAR (P< 0.001). UDVA and CDVA were improved by 8 and 4 Snellen lines, respectively [Figures 2 and 3]. The efficacy and safety indexes were 1.66 and 2.66, respectively at 3 years postoperatively.
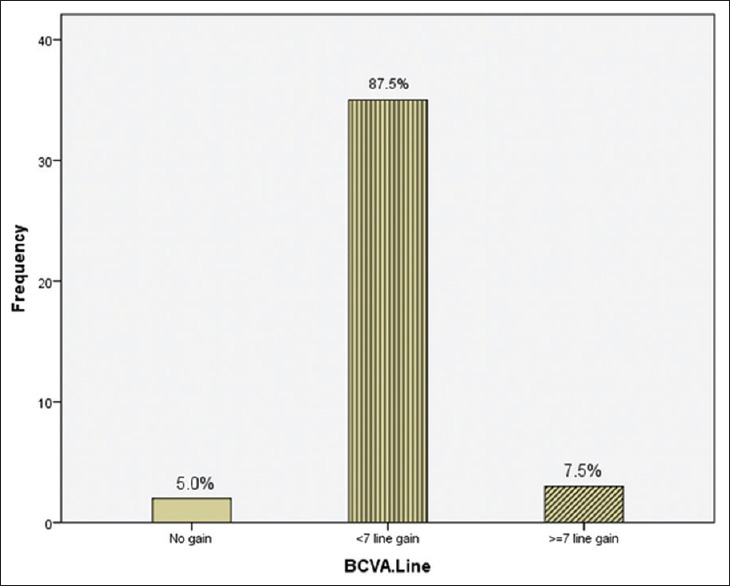
Table 1.
Pre- and post-operative visual and refractive data
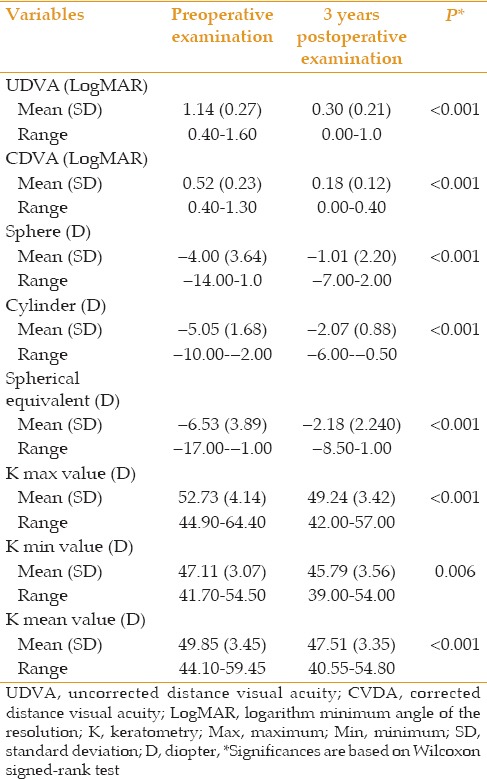
Figure 2.
Bar nomogram illustrates the percentage of eyes gaining lines of uncorrected distance visual acuity (UDVA) 3 years after surgery.
Figure 3.
Bar nomogram illustrates the percentage of eyes gaining lines of best spectacle corrected distance visual acuity (CDVA) 3 years after surgery.
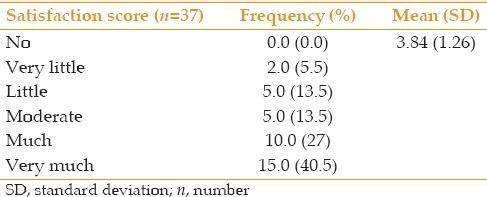
We observed a statistically significant reduction in mean spherical equivalent refractive error from − 6.53 D preoperatively to − 2.18 postoperatively (P< 0.001) [Table 1]. Additionally mean K reading was decreased by 2.34 D (from 49.85 D to 47.51 D, P = 0.001) [Figures 3 and 4 and Table 1]. All patients were satisfied with MyoRing implantation. Likewise, on a scale of 0 to 5 for current overall satisfaction, 81.0% of patients had moderate to high satisfaction with the operation (score 3-5) [Table 2].
Figure 4.
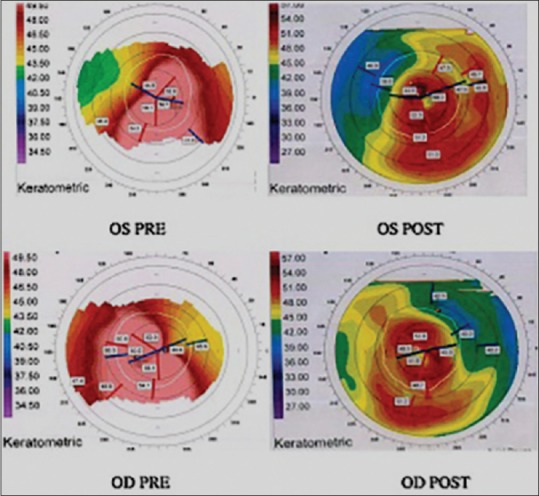
Preoperative (left), and postoperative (right) corneal topography maps 3 years after MyoRing implantation in a keratoconic cornea.
Table 2.
Satisfaction scores after 3 years
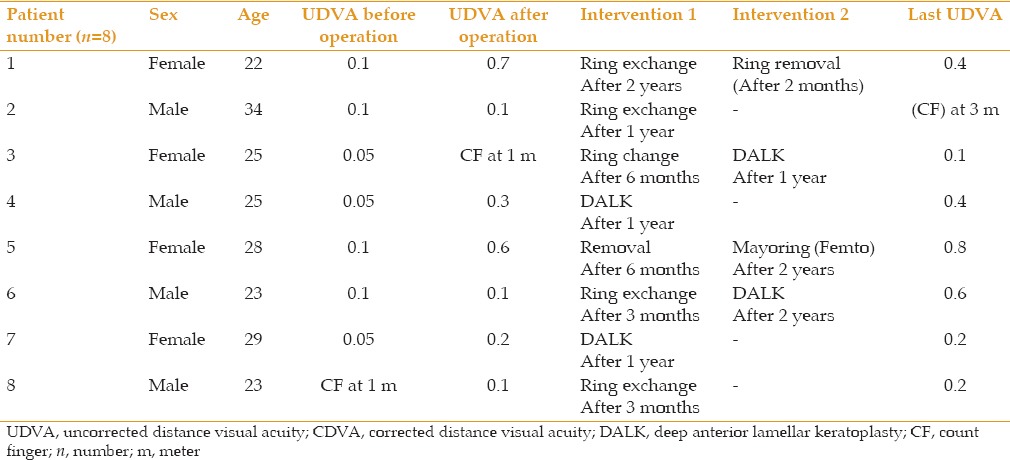
No major complications occurred in the reported group of 40 eyes. However, patient dissatisfaction led to additional procedures in eight eyes including MyoRing removal (1 eye), exchange (5 eyes) or deep anterior lamellar keratoplasty (2 eyes). Details of these patients are shown in Table 3.
Table 3.
Clinical data in eyes requiring reoperation
DISCUSSION
To our knowledge, this series is the first to report 3-year follow-up results of MyoRing implantation for keratoconus in a considerable number of patients. ICRSs have been shown to be safe and effective in correcting ectatic corneal disorder.[27,28] Nevertheless, segment extrusion, epithelial plug at the initial incision site, corneal neovascularization, segment migration, infectious keratitis, channel deposits, chronic pain, corneal haze, corneal melting, persistent incisional gaping, night halos and focal edema were reported as complications and limitations of ICRS implantation. Daxer et al[29] have shown that visual outcomes of MyoRing implantation for keratoconus does not depend on whether the corneal pocket is created by the femtosecond laser or mechanical dissection using the Pocket Maker microkeratome. In addition, no correlation was found between the type and location of the cone, and outcomes of MyoRing implantation.[30] In our study, the efficacy and safety index were above 1 at the last follow-up. These results are in concordance with most similar studies reporting the outcomes of MyoRing implantation for myopia and keratoconus.[20,21,31]
In our study, the rate of MyoRing exchange and removal was 16.6% (8/48). Studies by Clinch et al,[32] and Asbell et al[33] reported a 6.87% and 4.7% rate of ICRS removal, respectively. MyoRing removal was not associated with loss of UDVA, induction of myopia or astigmatism in the current study [Table 3]. Our results are in agreement with studies with shorter follow-up periods after MyoRing implantation[20,21,30,31]
Three years after surgery, significant reductions of 3.0 D and 2.98 D were observed in sphere and cylinder, respectively. These levels of refractive changes are consistent with those previously reported after MyoRing implantation using mechanical dissection.[20,21,30,34] In the current series, mean improvement in UDVA and CDVA was equivalent to 8 and 4 Snellen lines, respectively, which is compatible with previous studies by Mahmood et al,[21] Daxer et al[20] and Mojaled Nobari et al[34] Compared to some other MyoRing studies, our results showed greater improvement in UDVA. Jabbarvand et al operated 95 keratoconic eyes and showed a mean change of six lines.[35] Alio et al reported a mean change in UDVA from 1.36 to 0.61 LogMAR in 12 keratoconic eyes with MyoRing implantation.[36]
Mean improvement in UDVA in our study was more marked than those reported by studies on other ICRSs. Colin and Malet reported that UDVA was improved by five lines after Intacs implantation in 100 keratoconic eyes.[37] Shabayek and Alió found that UDVA was increased by six lines after KeraRing implantation in 21 keratoconic eyes.[38] This difference can be explained by the fact that MyoRing implants have a greater potential for myopic and astigmatic correction in keratoconus than other ICRSs, probably because of the more significant arc-shortening effect achieved with the completely circular mid-peripheral design of the MyoRing implant.
Our study has potential limitations, including lacking evaluation of higher-order aberration and a non-homogeneous number of patients in each stage of keratoconus severity. Thus, it would be interesting to carry out prospective studies to assess the outcomes of this procedure in different stages of disease.
In summary, MyoRing implantation using the Pocket Maker is a minimally invasive procedure that provides favorable clinical outcomes in keratoconus. Additionally, MyoRing implantation is a reversible and adjustable surgical procedure. However, further randomized, multi-centric prospective studies are needed to confirm the results of the current study.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 2.Tomidokoro A, Oshika T, Amano S, Higaki S, Maeda N, Miyata K. Changes in anterior and posterior corneal curvatures in keratoconus. Ophthalmology. 2000;107:1328–1332. doi: 10.1016/s0161-6420(00)00159-7. [DOI] [PubMed] [Google Scholar]
- 3.Gordon-Shaag A, Millodot M, Shneor E. The epidemiology and etiology of keratoconus. Int J Keratoco Ectatic Corneal Dis. 2012;1:7–15. [Google Scholar]
- 4.Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28:293–322. doi: 10.1016/0039-6257(84)90094-8. [DOI] [PubMed] [Google Scholar]
- 5.Barnett M, Mannis MJ. Contact lenses in the management of keratoconus. Cornea. 2011;30:1510–1516. doi: 10.1097/ICO.0b013e318211401f. [DOI] [PubMed] [Google Scholar]
- 6.Snibson GR. Collagen cross-linking: A new treatment paradigm in corneal disease – A review. Clin Experiment Ophthalmol. 2010;38:141–153. doi: 10.1111/j.1442-9071.2010.02228.x. [DOI] [PubMed] [Google Scholar]
- 7.Ertan A, Colin J. Intracorneal rings for keratoconus and keratectasia. J Cataract Refract Surg. 2007;33:1303–1314. doi: 10.1016/j.jcrs.2007.02.048. [DOI] [PubMed] [Google Scholar]
- 8.Piñero DP, Alio JL. Intracorneal ring segments in ectatic corneal disease – A review. Clin Experiment Ophthalmol. 2010;38:154–167. doi: 10.1111/j.1442-9071.2010.02197.x. [DOI] [PubMed] [Google Scholar]
- 9.Zare MA, Hashemi H, Salari MR. Intracorneal ring segment implantation for the management of keratoconus: Safety and efficacy. J Cataract Refract Surg. 2007;33:1886–1891. doi: 10.1016/j.jcrs.2007.06.055. [DOI] [PubMed] [Google Scholar]
- 10.Shetty R, Kurian M, Anand D, Mhaske P, Narayana KM, Shetty BK. Intacs in advanced keratoconus. Cornea. 2008;27:1022–1029. doi: 10.1097/ICO.0b013e318172fc54. [DOI] [PubMed] [Google Scholar]
- 11.Kymionis GD, Siganos CS, Tsiklis NS, Anastasakis A, Yoo SH, Pallikaris AL, et al. Long-term follow-up of Intacs in Keratoconus. Am J Ophthalmol. 2007;143:236–244. doi: 10.1016/j.ajo.2006.10.041. [DOI] [PubMed] [Google Scholar]
- 12.Alió JL, Shabayek MH, Artola A. Intracorneal ring segments for keratoconus correction: Long-term follow-up. J Cataract Refract Surg. 2006;32:978–985. doi: 10.1016/j.jcrs.2006.02.044. [DOI] [PubMed] [Google Scholar]
- 13.Busin M, Scorcia V, Zambianchi L, Ponzin D. Outcomes from a modified microkeratome-assisted lamellar keratoplasty for keratoconus. Arch Ophthalmol. 2012;130:776–782. doi: 10.1001/archophthalmol.2011.1546. [DOI] [PubMed] [Google Scholar]
- 14.Ing JJ, Ing HH, Nelson LR, Hodge DO, Bourne WM. Ten-year postoperative results of penetrating keratoplasty. Ophthalmology. 1998;105:1855–1865. doi: 10.1016/S0161-6420(98)91030-2. [DOI] [PubMed] [Google Scholar]
- 15.Frost NA, Wu J, Lai TF, Coster DJ. A review of randomized controlled trials of penetrating keratoplasty techniques. Ophthalmology. 2006;113:942–949. doi: 10.1016/j.ophtha.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 16.Alió JL, Artola A, Ruiz-Moreno JM, Hassanein A, Galal A, Awadalla MA. Changes in keratoconic corneas after intracorneal ring segment explantation and reimplantation. Ophthalmology. 2004;111:747–751. doi: 10.1016/j.ophtha.2003.08.024. [DOI] [PubMed] [Google Scholar]
- 17.Kubaloglu A, Sari ES, Cinar Y, Cingu K, Koytak A, Coskun E, et al. Comparison of mechanical and femtosecond laser tunnel creation for intrastromal corneal ring segment implantation in keratoconus: Prospective randomized clinical trial. J Cataract Refract Surg. 2010;36:1556–1561. doi: 10.1016/j.jcrs.2010.04.028. [DOI] [PubMed] [Google Scholar]
- 18.Daxer A. Adjustable intracorneal ring in a lamellar pocket for keratoconus. J Refract Surg. 2010;26:217–221. doi: 10.3928/1081597X-20100224-08. [DOI] [PubMed] [Google Scholar]
- 19.Daxer A. Corneal intrastromal implantation surgery for the treatment of moderate and high myopia. J Cataract Refract Surg. 2008;34:194–198. doi: 10.1016/j.jcrs.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 20.Daxer A, Mahmoud H, Venkateswaran RS. Intracorneal continuous ring implantation for keratoconus: One-year follow-up. J Cataract Refract Surg. 2010;36:1296–1302. doi: 10.1016/j.jcrs.2010.03.039. [DOI] [PubMed] [Google Scholar]
- 21.Mahmood H, Venkateswaran RS, Daxer A. Implantation of a complete corneal ring in an intrastromal pocket for keratoconus. J Refract Surg. 2011;27:63–68. doi: 10.3928/1081597X-20100212-11. [DOI] [PubMed] [Google Scholar]
- 22.Koch DD, Kohnen T, Obstbaum SA, Rosen ES. Format for reporting refractive surgical data. J Cataract Refract Surg. 1998;24:285–287. doi: 10.1016/s0886-3350(98)80305-2. [DOI] [PubMed] [Google Scholar]
- 23.Shetty R, Kurian M, Anand D, Mhaske P, Narayana KM, Shetty BK. Intacs in advanced keratoconus. Cornea. 2008;27:1022–1029. doi: 10.1097/ICO.0b013e318172fc54. [DOI] [PubMed] [Google Scholar]
- 24.Daxer A, Fratzl P. Collagen fibril orientation in the human corneal stroma and its implication in keratoconus. Invest Ophthalmol Vis Sci. 1997;38:121–129. [PubMed] [Google Scholar]
- 25.Daxer A, Misof K, Grabner B, Ettl A, Fratzl P. Collagen fibrils in the human corneal stroma: Structure and aging. Invest Ophthalmol Vis Sci. 1998;39:644–648. [PubMed] [Google Scholar]
- 26.Fratzl P, Daxer A. Structural transformation of collagen fibrils in corneal stroma during drying. An x-ray scattering study. Biophys J. 1993;64:1210–1214. doi: 10.1016/S0006-3495(93)81487-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alió J, Salem T, Artola A, Osman A. Intracorneal rings to correct corneal ectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2002;28:1568–1574. doi: 10.1016/s0886-3350(01)01275-5. [DOI] [PubMed] [Google Scholar]
- 28.Lovisolo CF, Calossi A, Ottone AC. Intrastromal inserts in keratoconus and ectatic corneal conditions. In: Lovisolo CF, Fleming JF, Pesando PM, editors. Intrastromal Corneal Ring Segments. Canelli AT, Italy: Fabiano Editore; 2000. pp. 95–163. [Google Scholar]
- 29.Daxer B, Mahmood H, Daxer A. MyoRing treatment for keratoconus: DIOPTEX PocketMaker vs Ziemer LDV for corneal pocket creation. Int J Keratoconus Ectatic Corneal Dis. 2012;1:151–152. [Google Scholar]
- 30.Daxer A. MyoRing for central and noncentral keratoconus. Int J Keratoconus Ectatic Corneal Dis. 2012;1:117–119. [Google Scholar]
- 31.Patel S, Marshall J, Fitzke FW., 3rd Model for deriving the optical performance of the myopic eye corrected with an intracorneal ring. J Refract Surg. 1995;11:248–252. doi: 10.3928/1081-597X-19950701-08. [DOI] [PubMed] [Google Scholar]
- 32.Clinch TE, Lemp MA, Foulks GN, Schanzlin DJ. Removal of INTACS for myopia. Ophthalmology. 2002;109:1441–1446. doi: 10.1016/s0161-6420(02)01090-4. [DOI] [PubMed] [Google Scholar]
- 33.Asbell PA, Uçakhan OO, Abbott RL, Assil KA, Burris TE, Durrie DS, et al. Intrastomal corneal ring segments: Reversibility of refractive effect. J Refract Surg. 2001;17:25–31. doi: 10.3928/1081-597X-20010101-03. [DOI] [PubMed] [Google Scholar]
- 34.Mojaled Nobari S, Villena C, Jadidi K. Predictability, stability and safety of MyoRing implantation in keratoconic eyes during one year follow-up. Iran J Ophthalmol. 2014;26:136–143. [Google Scholar]
- 35.Jabbarvand M, Salamatrad A, Hashemian H, Khodaparast M. Continuous corneal intrastromal ring implantation for treatment of keratoconus in an Iranian population. Am J Ophthalmol. 2013;155:837–842. doi: 10.1016/j.ajo.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 36.Alio JL, Piñero DP, Daxer A. Clinical outcomes after complete ring implantation in corneal ectasia using the femtosecond technology: A pilot study. Ophthalmology. 2011;118:1282–1290. doi: 10.1016/j.ophtha.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 37.Colin J, Malet FJ. Intacs for the correction of keratoconus: Two-year follow-up. J Cataract Refract Surg. 2007;33:69–74. doi: 10.1016/j.jcrs.2006.08.057. [DOI] [PubMed] [Google Scholar]
- 38.Shabayek MH, Alió JL. Intrastromal corneal ring segment implantation by femtosecond laser for keratoconus correction. Ophthalmology. 2007;114:1643–1652. doi: 10.1016/j.ophtha.2006.11.033. [DOI] [PubMed] [Google Scholar]


