Abstract
The current study utilized the intersectionality framework to explore whether smoking outcome expectancies (i.e., cognitions about the anticipated effects of smoking) were predicted by gender and ethnicity, and the gender-by-ethnicity interaction. In a cross-sectional design, daily smokers from the general community [32.2% women; Non-Hispanic African American (N=175), Non-Hispanic White (N=109), or Hispanic (N=26)] completed self-report measures on smoking expectancies and other co-factors. Results showed that women reported greater negative reinforcement (i.e., anticipated smoking-induced negative affect reduction) and weight control (i.e., anticipated smoking-induced appetite/weight suppression) expectancies than men. Hispanic (vs. African American or White) smokers endorsed greater negative reinforcement expectancies. A gender by ethnicity interaction was found for weight control expectancies, such that White women reported greater weight control expectancies than White men, but no gender differences among African American and Hispanic smokers were found. Ethnicity, gender, and their intersectionality should be considered in smoking cessation programs to target smoking-related cognitions.
Keywords: ethnic minority, gender differences, health disparities, smoking expectancies
Tobacco control efforts in the U.S have not equally benefited all members of society, contributing to tobacco-related health disparities among certain cross-sections of the population (American Cancer Society, 2014; Gadgeel & Kalemkerian, 2003; Haiman et al., 2006; Jemal et al., 2008; Siegel, Ward, Brawley, & Jemal, 2011; Underwood et al., 2012; USDHHS, 1998). Evidence suggests that ethnic minorities (vs. majorities) and women (vs. men) have had less marked reductions in smoking prevalence over time (Agaku, King, & Dube, 2013; Barbeau, Krieger, & Soobader, 2004; Dube, Asman, Malarcher, & Carabollo, 2009; King, Dube, Kaufmann, Shaw, & Pechacek, 2011; USDHHS, 1998) and may be at greater risk for relapse following a cessation attempt (Barbeau et al., 2004; Caraballo et al., 2014; Croghan et al., 2010; Pang & Leventhal, 2013; Piper, 2010; USDHHS, 1998). Understanding psychosocial factors that underlie smoking in women and ethnic minorities is important for elucidating sources of tobacco-related health disparities and informing targets for ethnicity- and gender-specific smoking cessation treatments that maximize clinical outcomes.
Of the various psychosocial factors implicated in the etiology of persistent smoking, smoking outcome expectancies—one’s cognitions about the consequences of cigarette use—are particularly important to study because of their: (a) putative role as a proximal mediator of motivation to smoke; and (b) suitability to target in psychosocial interventions aimed at modifying maladaptive cognitions that may impede cessation and enhancing adaptive cognitions that may facilitate cessation. Domains of smoking outcome expectancies can be parsed into: (1) negative consequences (i.e., expectations of smoking’s negative effects on health and social impressions); (2) positive reinforcement (i.e., expectations that smoking produces positive sensory effects and social facilitation); (3) negative reinforcement (i.e., expectations that smoking produces negative affect reduction); and (4) weight control (i.e., expectation that smoking aids in weight and hunger management; Brandon & Baker, 1991). Individuals who endorse stronger pro-smoking outcome expectancies tend to be at greater risk for greater cigarette dependence and smoking relapse following a quit attempt (Gwaltney, Shiffman, Balabanis, & Paty, 2005; Herd, Borland, & Hyland, 2009; Jeffries et al., 2004; Pang, Khoddam, Guillot, & Leventhal, 2014; Pomerleau, Zucker, & Stewart, 2001), putatively because they are motivated to continue smoking in order to obtain the anticipated positive emotional, social, sensory, and weight-related outcomes they believe that smoking provides.
Extant disparities research on smoking outcome expectancies has shown that women (vs. men) endorse greater negative reinforcement smoking expectancies (Brandon & Baker, 1991; Pang, Zvolensky, Schmidt, & Leventhal, 2015; J. D. Robinson, Lam, Carter, Wetter, & Cinciripini, 2012; Weinberger, George, & McKee, 2011; Weinberger, McKee, & George, 2010) as well as greater weight control smoking expectancies (Brandon & Baker, 1991; Copeland, Brandon, & Quinn, 1995). The scant literature on ethnic differences in smoking outcome expectancies has shown that Non-Hispanic African Americans report less strong weight control outcome expectancies than Non-Hispanic Whites, but do not differ on other smoking outcome expectancies (Sánchez-Johnsen, Ahluwalia, & Fitzgibbon, 2006; Sánchez-Johnsen, Carpentier, & King, 2011; Sánchez-Johnsen, Spring, Sommerfeld, & Fitzgibbon, 2005). While we are unaware of any study that compares the smoking expectancies of Hispanic smokers to those of smokers of other ethnic groups, studies suggest that expectancy measures demonstrate good convergent validity with measures of smoking rate, cigarette dependence, craving, and smoking withdrawal in samples of Hispanic smokers (Cepeda-Benito & Reig Ferrer, 2000; Reig-Ferrer & Cepeda-Benito, 2007; Vidrine et al., 2009). A past study (Cepeda-Benito & Reig Ferrer, 2000) found gender differences in negative reinforcement smoking expectancies in Hispanics, with Hispanic women endorsing them more than Hispanic men, but did not allow for comparisons between Hispanics and other ethnic groups (Cepeda-Benito & Reig Ferrer, 2000).
There is also reason to believe that gender and ethnicity will interact in the prediction of smoking outcome expectancies. The intersectionality framework simultaneously consider the interaction of multiple identities (Cole, 2009), and suggest that gender and ethnicity do not simply have additive effects on health-relevant behavior. Rather, the combination of being both a woman and a member of an ethnic minority group may generate a qualitatively unique psychosocial context that increases the likelihood of a specific pattern of health behavior that is not adequately reflected by exploring the independent/additive effects of gender and ethnicity. Hence, an initial test of possible intersectionality of gender and ethnicity is to explore the statistical interaction between these two variables in the prediction of smoking expectancies in order to elucidate whether the presence and nature of any gender differences in smoking expectancies are equivalent or distinct across different ethnic groups, or whether any ethnic differences in smoking expectancies vary across gender. Because of possible gender-specific ethno-cultural variation such intersectionality in smoking expectancies is plausible. For instance, the salience of smoking’s expected effects on weight control may be more salient for Non-Hispanic White (vs. Non-Hispanic African American) women because culturally-specific ideals that value thinness among women may be strong in Non-Hispanic Whites, yet weaker in Non-Hispanic African American communities in which cultural norms for women’s body shapes place less value on thinness (Kronenfeld, Reba-Harrelson, Von Holle, Reyes, & Bulik, 2010; Molloy & Herzberger, 1998; Rogers Wood & Petrie, 2010; Watson, Ancis, White, & Nazari, 2013). Consistent with this notion, extensive literature shows gender differences in weight control expectancies in largely Non-Hispanic White samples (Copeland et al., 1995), but a study in Non-Hispanic African Americans reported no gender differences in weight control expectancies (Pulvers et al., 2004). However, the interaction of gender and ethnicity on weight control expectancies has not been directly addressed by a study. Moreover, identifying ethnicity by gender interactions in the prediction of smoking expectancies may facilitate targeted smoking cessation programs that adapt treatments by considering both the ethnicity and gender of patients.
The current cross-sectional study examined differences in smoking expectancies by ethnicity (Non-Hispanic African American vs. Hispanic vs. Non-Hispanic White), gender (women vs. men), and their interaction in a community sample of non-treatment-seeking smokers. Regarding gender differences, we hypothesized that we would replicate prior results by demonstrating that women would report stronger weight control and negative reinforcement smoking outcome expectancies than men (Brandon & Baker, 1991; Copeland et al., 1995; Pang et al., 2015; J. D. Robinson et al., 2012; Weinberger et al., 2011, 2010). Due to the scarce theory and data on ethnicity and gender by ethnicity intersectionality in smoking outcome expectancies, we did not put forth any hypothesis regarding negative consequences and positive reinforcement smoking outcome expectancies. However, based on the previously mentioned literature, we expected women to endorse greater negative reinforcement expectancies than men and for weight control expectancies to differ by ethnicity and show an ethnicity-by-gender interaction, with Non-Hispanic White women endorsing stronger weight control expectations than Non-Hispanic White men. Hence, our primary analytic approach utilized the agnostic strategy of profile analysis, a multivariate approach that tests whether group differences exist across a set of response domains. Profile analysis permits testing whether group differences reflect disparities in magnitude that are equivalent across response domains (e.g., women hold stronger expectancies that smoking causes any type of effect, regardless of domain) or whether disparities exist in quality or kind such that the nature of group differences vary as a function of response domains (e.g., women endorse stronger expectancies for negative reinforcement and weight control than men but do not differ from men in expectancies that smoking is associated with positive reinforcement or negative consequences).
Methods
Participants
Participants were recruited in the Los Angeles Area via online and newspaper advertisements to participate in a study on individual differences in tobacco abstinence effects, which included a baseline assessment visit and two additional experimental visits involving manipulation of overnight tobacco abstinence (Leventhal et al., 2014); this report is based upon data collected during the baseline visit. Eligibility criteria included being 18 years of age or older, regular cigarette smoker for at least 2 years, and currently smoking at least 10 cigarettes per day. Participants self-identifying as both Non-Hispanic African American and Hispanic (n=3) or both Non-Hispanic White and Hispanic (n=15) were excluded from the analyses in order to create three, distinct ethnic groups (Non-Hispanic African Americans, Non-Hispanic Whites, and Hispanics). Similar categorizations have also been utilized in previous multi-ethnic studies (Reitzel et al., 2011, 2014). Participants were also excluded if they expressed a desire to quit in the next 30 days, had a breath carbon monoxide (CO) level <10 parts per million (ppm) during session, used other tobacco products (i.e. cigars, cigarillos, electronic cigarettes), were currently using a nicotine replacement product (i.e., nicotine gum, spray, patch), were currently pregnant, met criteria for current DSM-IV substance abuse or dependence, met criteria for current DSM-IV psychiatric disorders, and currently used psychiatric medications. Participants (N=515) who met eligibility criteria after completing a telephone pre-screen were scheduled for a session, whereby more extensive screening took place. Of those who were found potentially eligible through the telephone pre-screen and came in for their session, 152 were found ineligible during their session, due to low CO levels, current psychiatric disorders or psychiatric medication use, and other criteria. Participants who completed the baseline visit were compensated $15. The study was approved by the University of Southern California Institutional Review Board.
Procedures
At the baseline session, participants provided informed consent and then completed a CO levels analysis and a structured clinical interview for DSM-IV Non-Patient Edition (First, Spitzer, Gibbon, & Williams, 2002) mood disorders, psychotic disorders, and substance use disorder modules to assess for psychiatric eligibility. Eligible participants then completed several self-report measures (described below).
Measures
Demographics included gender (Forced choice: Woman or Man) ethnicity (Forced choice: American Indian/Alaskan Native, Asian, Non-Hispanic African American, Middle Eastern, Pacific Islander, Non-Hispanic White, and Hispanic), income (i.e., which category best describes your total pre-tax household income last year; coded as 0= < $15,000 and 1= ≥$15,000), education (0=No college and 1=Some college completed or higher), and employment (i.e., indicate your employment status as of today; coded as 0=Unemployed and 1=Part-time or higher). Smoking characteristics included number of cigarettes smoked per day and age of onset of regular smoking. The Fagerström Test of Cigarette Dependence (Heatherton, Kozlowski, Frecker, & Fagerström, 1991)—a well-validated six-item measure assessing cigarette dependence severity—was also included to describe the degree of tobacco addiction in the sample.
The Smoking Consequences Questionnaire (SCQ; Brandon & Baker, 1991; Wetter et al., 1994) is a 50-item self-report measure with four subscales that assess four domains of smoking outcome expectancies : (a) negative reinforcement (12 items; e.g., “Cigarettes help me deal with anxiety or worry”); (b) positive reinforcement (15 items; e.g., “When I smoke, the taste is pleasant”); (c) negative consequences (18 items; e.g., “Smoking is taking years off my life”), and (d) weight control (5 items; e.g., “Smoking controls my appetite”). Participants rated each item in a Likert scale format (1= Not true of me at all to 7=Very true of me) and an average score per item is computed for each subscale.
Data Analysis
Data was analyzed using IBM SPSS Version 21 (IBM Corp., Armonk, NY). Preliminary analyses included reporting descriptive statistics and ethnic and gender comparisons (via chi-squared and ANOVA tests) on sample demographic and smoking characteristics. Primary analyses utilized profile analysis, a MANOVA-based analytic technique (Tabachnick & Fidell, 2001), which allowed for the investigation of differences in between-subjects variable(s) (i.e., gender and ethnic group) across a within-subject variable reflecting different domains within an outcome variable response set (i.e., the four SCQ subscales). Profile analysis tested whether each of three null-type hypotheses were rejected. The flatness hypothesis proposes that the mean score (averaged across groups) is equivalent across the four domains of outcomes (i.e., the slope is flat across each response domain). For the current study, rejection of the flatness hypothesis would suggest that in the overall sample, cognitions regarding the consequences of smoking are not equivalent across all expectancy subscales (i.e., within-subject effect of subscale). We do not report or interpret analyses of the flatness hypothesis, as the focus of this paper is on describing ethnic and gender difference rather than noting trends in expectancies in the overall sample. The levels hypothesis proposes that average across response domains the magnitude of scores is equivalent across groups. In this study, rejection of the levels hypothesis would suggest that there are significant differences in the overall strength of cognitions regarding the outcomes of smoking (i.e., between-subjects effect of group). Equivalent to standard MANOVA, rejection of the levels hypothesis suggest that group profiles differ in magnitude/quantity, such that some groups hold stronger expectancies about smoking overall that generalize across domains. The parallelism hypothesis proposes that the extent to which groups differ from one another is equivalent across response domains. In this study, rejection of the parallelism hypothesis would suggest that group profiles differ in shape/quality, such that the nature or degree of group differences varies across the specific expectancy domains (i.e., within-between subject variable interaction between group and subscale).
In profile analyses, we reverse coded the negative consequences SCQ subscale such that each was scored in the pro-smoking direction to facilitate interpretation of levels and parallelism tests. We tested three sets of profile analysis models: (a) 2 (Between: women vs. men) × 4 (Within: SCQ subscale) a model in which gender was the between-participants group variable; (b) 3 (Between: Non-Hispanic African American vs. Hispanic vs. Non-Hispanic White) × 4 (Within: SCQ subscale) a model in which ethnicity was the between-subjects group variable; and (c) 3 (Between: Non-Hispanic African American vs. Hispanic vs. Non-Hispanic White) × 2 (Between: men vs. women) × 4 (Within: SCQ subscale) three way model to test for interactions across gender and ethnicity. Significant effects leading to the rejection of the parallelism hypothesis were followed up in secondary analyses utilized adjusted ANOVA based on the general linear model for unbalanced cell sizes to investigate the main and interactive effects of gender and ethnicity. For each outcome, each model was tested twice—once unadjusted using ANOVA and once in ANOVA adjusted for education and age because these two sample characteristics significantly differed according to ethnicity (see Table 1), and we followed up significant adjusted ANOVAs involving the ethnicity with pairwise comparisons utilizing pairwise t-tests.
Table 1.
Baseline Characteristics by Ethnicity and Gender
|
Overall Sample
(N = 311) |
African American
(N = 175) |
White
(N = 109) |
Hispanic
(N = 26) |
||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Variable: M (SD) or % | Women (N=56) |
Men (N=119) |
Women (N=34) |
Men (N=75) |
Women (N=10) |
Men (N=16) |
|
| Demographics | |||||||
| Age | 44.42 (10.56) | 44.04 (11.36) | 47.95 (8.52) | 42.29 (10.27) | 40.8 (11.86) | 42.70 (12.28) | 42.38 (7.59) |
| Annual Income | |||||||
| < $15,000 | 59.5 | 54.9 | 58.2 | 68.8 | 60.9 | 66.7 | 53.3 |
| ≥ $15,000 | 40.5 | 45.0 | 41.7 | 31.3 | 39.1 | 33.3 | 46.7 |
| Education | |||||||
| No College | 44.9 | 55.6 | 48.3 | 41.2 | 29.3 | 44.4 | 68.8 |
| Some College or Higher | 55.1 | 44.4 | 51.7 | 58.8 | 70.6 | 55.5 | 31.3 |
| Employment | |||||||
| Unemployed | 75.6 | 77.8 | 74.6 | 70.5 | 74.6 | 88.9 | 81.3 |
| Part-Time or Higher | 24.4 | 22.2 | 25.4 | 29.4 | 25.4 | 11.1 | 18.8 |
| Smoking Characteristics | |||||||
| Age onset regular smoking | 19.12 (5.60) | 19.55 (5.32) | 19.39 (6.16) | 19.36 (5.59) | 19.36 (5.59) | 17.10 (4.80) | 18.19 (5.0) |
| FTND | 5.43 (1.93) | 5.57 (1.75) | 5.47 (1.96) | 5.26 (1.75) | 5.26 (1.75) | 5.90 (1.66) | 5.69 (2.09) |
| Cigarettes/day | 16.77 (7.05) | 15.25 (6.87) | 16.28 (8.0) | 17.71 (6.52) | 17.71 (6.52) | 16.80 (5.37) | 17.17 (6.32) |
| SCQ | |||||||
| Negative Consequences | 3.17 (1.18) | 3.15 (1.24) | 3.20 (1.08) | 2.86 (1.47) | 3.34 (1.18) | 3.23 (0.93) | 3.02 (1.11) |
| Positive Reinforcement | 4.52 (1.20) | 4.51 (1.12) | 4.48 (1.14) | 4.45 (1.36) | 4.59 (1.31) | 4.59 (1.15) | 4.62 (1.30) |
| Negative Reinforcement | 4.34 (1.72) | 4.80 (1.88) | 4.10 (1.71) | 4.75 (1.77) | 3.89 (1.50) | 5.47 (1.17) | 5.11 (1.57) |
| Weight Control | 3.05 (2.06) | 3.28 (2.19) | 3.05 (1.95) | 3.93 (2.33) | 2.45 (1.73) | 2.40 (1.85) | 3.58 (2.62) |
Note: FTND = Fagerström Test of Nicotine Dependence (range 0-10); SCQ = Smoking Consequences Questionnaire (range 1-7).
p < .05,
p < .01,
p < .001,
p < .0001
Results
Preliminary Analyses
Descriptive statistics for demographics, smoking characteristics, and SCQ subscales are reported in Table 1 by gender, ethnicity, and for gender within each ethnicity. The sample was predominantly men (68%) and there were significant ethnic differences in education and age (Table 2), therefore, we as adjusted for these covariates in our primary and secondary analyses. Chi-squared tests [X2= 10.73, p<.01] showed that 67% of Non-Hispanic Whites reported having attended at least some college vs. 49% of Non-Hispanic African Americans and 40% of Hispanics. Pairwise comparisons showed that Non-Hispanic African Americans were significantly older than Non-Hispanic Whites [t(280)=4.28, p<.0001] and Hispanics [t(197)=2.06, p<.05].
Table 2.
ANOVA Models for Main Effects of Ethnicity and Gender, and Ethnicity × Gender Interaction for Individual SCQ Subscales
|
Ethnicity
Main Effect |
Gender
Main Effect |
Ethnicity × Gender
Interaction |
|
|---|---|---|---|
|
|
|||
| F or X2 | t or X2 | F or X2 | |
| Demographics | |||
| Age | 9.76**** | −1.27 | 2.15 |
| Gender | 0.52 | 0.2 | - |
| Women | |||
| Men | |||
| Annual Income | 1.02 | 0.11 | 0.78 |
| < $15,000 | 0.44 | ||
| ≥ $15,000 | |||
| Education | 10.73** | 1.12 | 0.70 |
| No College | 2.22 | ||
| Some College or Higher | |||
| Employment | 1.24 | 0.05 | 0.36 |
| Unemployed | 0.47 | ||
| Part-Time or Higher | |||
| Smoking Characteristics | |||
| Age onset regular smoking | 1.07 | 0.2 | 0.20 |
| FTND | 1.11 | 0.45 | 0.02 |
| Cigarettes/day | 2.65 | −0.81 | 0.07 |
| SCQ | |||
| Negative Consequencesa | 0.06, 0.57 a | −1.19 | 1.34, 0.96a |
| Positive Reinforcement | 0.15, 0.02 a | −0.24 | 0.14, 0.01a |
| Negative Reinforcement | 4.31*, 3.24 a * | 3.65**** | 0.23, 0.31a |
| Weight Control | 0.37, 0.07 a | 2.15 | 5.17**, 4.13*a |
Note: FTND = Fagerström Test of Nicotine Dependence (range 0-10); SCQ = Smoking Consequences Questionnaire (range 1-7).
Adjusted models (covariates: education & age).
p < .05,
p < .01,
p < .001,
p < .0001
Primary Analyses
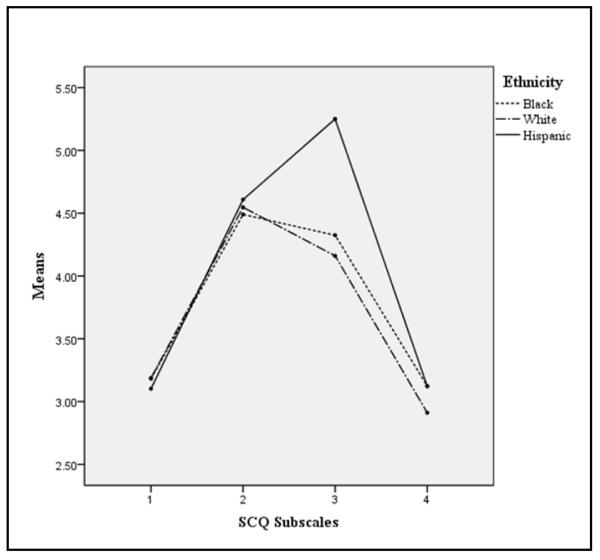
Ethnicity as the group variable
The parallelism hypothesis [λ=0.96, F(6, 610)=2.14, p<.05, partial η2=0.021]; between-subjects by within-subject interaction between gender and SCQ subscale) was rejected, but the levels hypothesis was not [F(2, 307)=1.27, p=.28], suggesting the ethnic differences in expectancies varied as a function of expectancy domain (i.e., the shape of expectancy profiles differed across ethnicity; see Figure 1). Follow-up adjusted ANOVAs showed significant ethnic differences in the SCQ negative reinforcement subscale, but no ethnic differences on the other SCQ subscales (see Table 2). Pairwise comparisons elucidated that Hispanics endorsed stronger negative reinforcement smoking expectancies than Non-Hispanic African Americans [t(199)=−2.52, p<.05] and Non-Hispanic Whites [t(133)=−3.14, p<.01], but that Non-Hispanic African Americans and Non-Hispanic Whites did not differ from each other on this domain (p=.44).
Figure 1. Profile Plots for Main Effects by Ethnicity.
Note: SCQ = Smoking Consequences Questionnaire subscales (range 1-7; 1 = Negative Consequences, 2 = Positive Reinforcement, 3 = Negative Reinforcement, 4 = Weight Control).
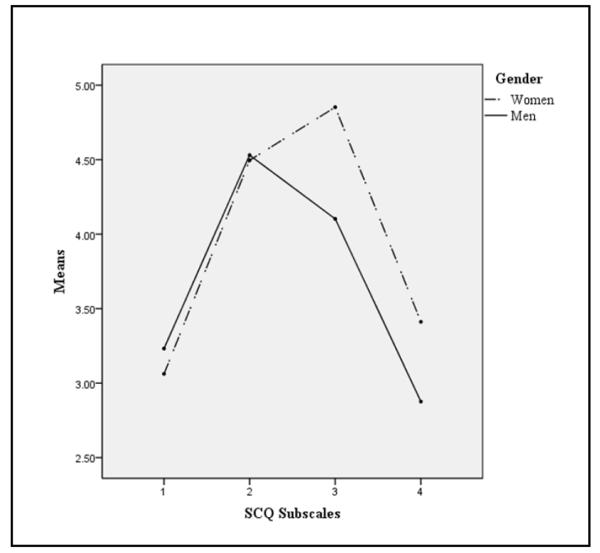
Gender as the group variable
Both the levels ([F(1, 308)=5.88, p<.05]; i.e., between-subjects effect of gender) and parallelism ([λ=0.93, [F(3, 306)=7.42, p<.0001, partial η2=0.068]; between-by-within interaction between gender and subscale) hypotheses were rejected, which indicated that there were gender differences averaged over all SCQ domains and that the nature of gender differences varied as a function of expectancy domain (i.e., qualitative differences in expectancy profile shape; see Figure 2). Follow-up adjusted ANOVAs showed that women scored significantly higher than men on both negative reinforcement and weight control expectancies, but that there were no gender differences on any other SCQ scales (see Table 2).
Figure 2. Profile Plots for Main Effects by Gender.
Note: SCQ = Smoking Consequences Questionnaire subscales (range 1-7; 1 = Negative Consequences, 2 = Positive Reinforcement, 3 = Negative Reinforcement, 4 = Weight Control).
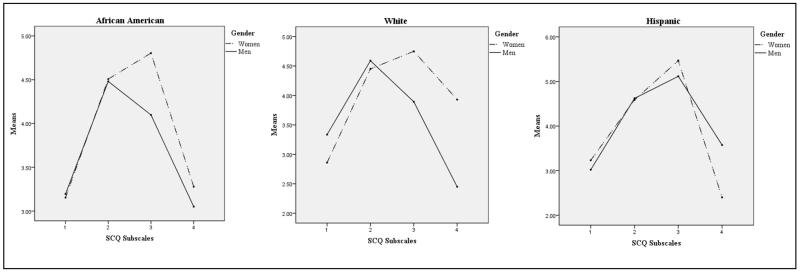
Gender and ethnicity as concomitant group variables
Tests of the parallelism hypothesis regarding the gender × ethnicity interaction yielded a non-significant trend ([λ=0.96, F(6, 604)=2.08, p=.054, partial η2=0.020]; Gender × Ethnicity × Subscale three-way between-between-within interaction, see Figure 3). Tests of the levels hypothesis were not significant [F(2, 304)=1.07, p=.34; Gender × Ethnicity between-by-between interaction). Follow-up adjusted ANOVAs examining the Gender × Ethnicity interaction separately for each subscale revealed an interaction for weight control expectancies, but no corresponding interactions for the other expectancy domains (see Table 2). Simple effect analyses to disentangle the interaction showed that Non-Hispanic White women endorsed the weight control smoking expectancies more than Non-Hispanic White men [t(107)=3.695, p<.0001], but there were no gender differences among Non-Hispanic African Americans [t(173)=0.693, p=.49] and Hispanics [t(24)=−1.234, p=.23] on weight control expectancies (see descriptive statistics by gender within ethnicity in Table 1 and profile plots by gender stratified by ethnicity in Figure 3).
Figure 3. Profile Plots for Main Effects by Ethnicity × Gender.
Note: SCQ = Smoking Consequences Questionnaire subscales (range 1-7; 1 = Negative Consequences, 2 = Positive Reinforcement, 3 = Negative Reinforcement, 4 = Weight Control).
Discussion
This study provides novel evidence regarding the role of gender, ethnicity, and their intersectionality in the expression of smoking outcome expectancies. We found qualitative differences in expectancy profiles by gender, such that women (vs. men) reported stronger weight control and negative reinforcement smoking expectancies, yet there were no gender differences in expectancies for positive reinforcement or negative consequences. These findings provide further evidence that women compared to men endorse greater weight control expectancies (Brandon & Baker, 1991; Copeland et al., 1995) and negative reinforcement expectancies (Pang et al., 2015; Pulvers et al., 2004; Weinberger et al., 2010; Wetter et al., 1994). This pattern account for prior findings showing women are at greater risk of relapse following a cessation attempt than men (Bjornson, Rand, Connett, Lindgren, & Et al, 1995; Piper, 2010; Swan, Jack, & Ward, 1997; Wetter et al., 1999) as smokers who report greater negative reinforcement expectancies have been shown to have poorer smoking cessation outcomes (Wetter et al., 1994)..
This study found novel evidence indicating qualitative differences in expectancy profiles by ethnicity, such that Hispanics reported stronger negative reinforcement expectancies than Non-Hispanic Whites and Non-Hispanic African Americans. Given the small sample of Hispanics in this study, the generalization of these results is yet unknown. If this pattern were to be replicated in future work, one potential area inquiry for future research on the underpinnings of ethnic differences in negative reinforcement expectancies may be ethnic stratification in the experience of negative affect-related states. Previous research has demonstrated that Hispanics endorse greater depressive symptoms in comparison to Non-Hispanic Whites (Blazer, Kessler, McGonagle, & Swartz, 1994; Bock, Niaura, Neighbors, Carmona-Barros, & Azam, 2005). A recent study illustrated that depressed mood was associated with a greater likelihood of currently smoking in Hispanics (Ellis, Orom, Giovino, & Kiviniemi, 2015); thus, among Hispanic smokers, smoking to alleviate negative affect symptomatology could be important. Hispanics are more likely to report perceived discrimination than Non-Hispanic Whites (Purnell et al., 2012), which may explain ethnic differences in psychological distress. Because psychological distress has been shown to mediate the relationship between discrimination and smoking (Purnell et al., 2012), some minority ethnic groups may place higher value on negative reinforcing properties of smoking. However, as Hispanics are poorly represented in the tobacco research literature, our finding potentially marks an important insight into this population and provides a basis for future study.
We also found evidence of possible intersectionality between gender and ethnicity on weight control (but not other forms of) smoking expectancies. Weight control smoking expectancies were stronger in women versus men in Non-Hispanic Whites, but did not differ by gender among Hispanics or Non-Hispanic African Americans. A prior study in adolescents showed that Non-Hispanic White adolescent girls reported smoking to lose or control weight as a reason for smoking more often than Hispanic and Non-Hispanic African American girls (Fulkerson & French, 2003). Cultural differences in acceptance of a wider range of body shapes and sizes for women may influence the salience of smoking’s weight controlling effects as a function of ethnicity. Although Non-Hispanic African Americans have higher prevalence rates of obesity than Non-Hispanic Whites (Patel et al., 2011; Pomerleau, Zucker, Namenek, et al., 2001), they are more likely to be satisfied with their body shape (Schwartz & Brownell, 2004), and are less likely to perceive themselves as overweight than Non-Hispanic White ( Robinson, Webb, & Butler-Ajibade, 2011). Furthermore, Hispanics do not differ from Non-Hispanic African Americans in body image attitudes or distress (Hrabosky & Grilo, 2007) and in self-perception of being overweight (Paeratakul, White, Williamson, Ryan, & Bray, 2002). Therefore, Hispanic and Non-Hispanic African American smokers may not be as concerned with controlling their weight as Non-Hispanic White smokers. Additionally, these results are consistent with studies showing that gender differences in weight expectancies exist in studies utilizing samples that have a high proportion of Non-Hispanic Whites (Copeland et al., 1995), but no gender differences in studies using an Non-Hispanic African American sample (Pulvers et al., 2004).
Several limitations in this study are worth noting. First, our use of self-report measures may be more vulnerable to response biases, which has been shown to differ by ethnicity (Bardwell & Dimsdale, 2001). While self-report is the most common and ideal standard for assessing expectancies; alternative methods that assess the accessibility or degree to which expectancies are activated from memory might be useful (Hendricks & Brandon, 2005). Second, although our inclusion of Hispanics as an ethnic group in our sample is novel in smoking outcome expectancy research, it is a small sample (N=26) in comparison to our samples of Non-Hispanic African Americans (N=175) and Non-Hispanic White (N=109), which may have decreased the power to detect differences involving this group. Additionally, we did not distinguish between Hispanic subgroups based on country of origin or other differentiating factors. Future studies should investigate Hispanic subgroup differences in expectancies as previous reports suggest that smoking behavior differs between Puerto Ricans and Dominicans (Borrelli, Hayes, Gregor, Lee, & McQuaid, 2011). Third, our sample was collected via convenience and was restricted to a single geographic area; hence, future extension to other locations is warranted to enhance generalizability.
This study offers novel data on smoking expectancies as a possible mechanism to consider in gender and ethnic disparities in smoking (American Cancer Society, 2014; Gadgeel & Kalemkerian, 2003; Haiman et al., 2006; Jemal et al., 2008; Siegel et al., 2011; Underwood et al., 2012; USDHHS, 1998). Future studies should utilize an intersectionality approach (Cole, 2009), by considering one’s concurrent multiple ethno-cultural or gender-specific identities to elucidate the psychosocial and socio-cultural context that may influence smoking-related cognitions and behaviors. Our findings suggest that, more broadly, certain cognitions relevant to smoking may not manifest when exploring gender and ethnicity independently, but becomes apparent when both factors are considered. Therefore, intersectionality of ethnicity and gender should be considered in smoking cessation programs to target smoking-related cognition that might be more salient in some combinations of gender and ethnicity, but perhaps not others.
Author Biographies
Claudia Aguirre graduated from the University of Southern California with a B.A. in Psychology. She is currently employed as a Project Assistant in the USC Health, Emotion, and Addiction Laboratory at the Keck School of Medicine. Her research interest include expectancies, alcohol abuse, and risk-taking behavior.
Mariel Bello received her B.S. in Psychology at the University of California, Riverside. She is currently employed as a Project Specialist in the USC Health, Emotion, and Addiction Laboratory at the Keck School of Medicine. Her research interests include health disparities in underserved populations, substance abuse, and behavioral genetics.
Raina Pang graduated from University of Southern California with a Ph.D. in Neuroscience. She is currently a postdoctoral research fellow in the Department of Preventive Medicine at USC. Her main research focus is female specific factors in addiction.
Nafeesa Andrabi received her B.A. in Sociology from Occidental College in 2014. She is currently a Project Assistant in the USC Health, Emotion, and Addiction Laboratory at the Keck School of Medicine. Her research interest include Health and Illness and ethnography.
Peter Hendricks, Ph.D., is a clinical psychologist and Associate Professor in the Department of Health Behavior of the School of Public Health at the University of Alabama at Birmingham. His area of expertise involves the development of novel and potentially more effective treatments for addictive behaviors.
Ricky Bluthenthal, Ph.D., is a sociologist and Professor in the Department of Preventive Medicine and the Institute for Prevention Research at the Keck School of Medicine, University of Southern California. His research interests include drug use epidemiology, prevention interventions, and community-based participatory research methods among others.
Adam Leventhal, Ph.D., is a clinical psychologist and Associate Professor of Preventive Medicine and Psychology at the University of Southern California Keck School of Medicine. He is Director of the USC Health, Emotion, & Addiction Laboratory, which applies psychopharmacology and epidemiology to understand the intersection between mental health, addiction, and health behavior.
References
- Agaku I, King B, Dube S. Current Cigarette Smoking Among Adults—United States, 2011. JAMA. 2013;309(6):539–541. doi: 10.1001/jama.2012.114523. [DOI] [Google Scholar]
- American Cancer Society . Cancer facts & figures. American Cancer Society, (Generic); 2014. [Google Scholar]
- Barbeau EM, Krieger N, Soobader M-J. Working Class Matters: Socioeconomic Disadvantage, Race/Ethnicity, Gender, and Smoking in NHIS 2000. American Journal of Public Health. 2004;94(2):269–278. doi: 10.2105/AJPH.94.2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardwell WA, Dimsdale JE. The Impact of Ethnicity and Response Bias on the Self-Report of Negative Affect. Journal of Applied Biobehavioral Research. 2001;6(1):27–38. doi: 10.1111/j.1751-9861.2001.tb00105.x. [DOI] [Google Scholar]
- Bjornson W, Rand C, Connett JE, Lindgren P, et al. Gender differences in smoking cessation after 3 years in the Lung Health Study. American Journal of Public Health. 1995;85(2):223–30. doi: 10.2105/ajph.85.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blazer DG, Kessler RC, McGonagle KA, Swartz MS. The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. The American Journal of Psychiatry. 1994;151(7):979–986. doi: 10.1176/ajp.151.7.979. [DOI] [PubMed] [Google Scholar]
- Bock BC, Niaura RS, Neighbors CJ, Carmona-Barros R, Azam M. Differences between Latino and non-Latino White smokers in cognitive and behavioral characteristics relevant to smoking cessation. Addictive Behaviors. 2005;30(4):711–724. doi: 10.1016/j.addbeh.2004.08.017. [DOI] [PubMed] [Google Scholar]
- Borrelli B, Hayes RB, Gregor K, Lee CS, McQuaid EL. Differences in smoking behavior and attitudes among Puerto Rican, Dominican, and non-Latino white caregivers of children with asthma. American Journal of Health promotion : AJHP. 2011;25(5 Suppl):S91–S95. doi: 10.4278/ajhp.100624-ARB-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandon TH, Baker TB. The Smoking Consequences Questionnaire: The subjective expected utility of smoking in college students. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3(3):484–491. doi: 10.1037/1040-3590.3.3.484. [DOI] [Google Scholar]
- Caraballo RS, Kruger J, Asman K, Pederson L, Widome R, Kiefe CI, Jacobs J, David R. Relapse among cigarette smokers: the CARDIA longitudinal study - 1985-2011. Addictive Behaviors. 2014;39(1):101–106. doi: 10.1016/j.addbeh.2013.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cepeda-Benito A, Reig Ferrer A. Smoking Consequences Questionnaire—Spanish. Psychology of Addictive Behaviors. 2000;14(3):219–230. doi: 10.1037/0893-164X.14.3.219. [DOI] [PubMed] [Google Scholar]
- Cole ER. Intersectionality and Research in Psychology. American Psychologist. 2009;64(3):170–180. doi: 10.1037/a0014564. [DOI] [PubMed] [Google Scholar]
- Copeland AL, Brandon TH, Quinn EP. The Smoking Consequences Questionnaire-Adult: Measurement of smoking outcome expectancies of experienced smokers. Psychological Assessment. 1995;7(4):484–494. doi: 10.1037/1040-3590.7.4.484. [DOI] [Google Scholar]
- Croghan IT, Hurt RD, Ebbert JO, Croghan GA, Polk OD, Jr, Stella PJ, Loprinzi CL. Racial differences in smoking abstinence rates in a multicenter, randomized, open-label trial in the United States. Journal of Public Health. 2010;18(1):59–68. doi: 10.1007/s10389-009-0277-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube S, Asman K, Malarcher A, Carabollo R. Cigarette Smoking Among Adults and Trends in Smoking Cessation—United States, 2008. JAMA: The Journal of the American Medical Association. 2009;302(24):2651–2654. [Google Scholar]
- Ellis EM, Orom H, Giovino GA, Kiviniemi MT. Relations Between Negative Affect and Health Behaviors by Race/Ethnicity: Differential Effects for Symptoms of Depression and Anxiety. Health Psychology. 2015 doi: 10.1037/hea0000197. (Journal Article) [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-Patient Edition. Biometrics Research, New York State Psychiatric Institute; New York: 2002. [Google Scholar]
- Fulkerson JA, French SA. Cigarette smoking for weight loss or control among adolescents: gender and racial/ethnic differences. Journal of Adolescent Health. 2003;32(4):306–313. doi: 10.1016/S1054-139X(02)00566-9. [DOI] [PubMed] [Google Scholar]
- Gadgeel SM, Kalemkerian GP. Racial differences in lung cancer. Cancer and metastasis reviews. 2003;22(1):39–46. doi: 10.1023/A:1022207917249. [DOI] [PubMed] [Google Scholar]
- Gwaltney CJ, Shiffman S, Balabanis MH, Paty JA. Dynamic Self-Efficacy and Outcome Expectancies: Prediction of Smoking Lapse and Relapse. Journal of Abnormal Psychology. 2005;114(4):661–675. doi: 10.1037/0021-843X.114.4.661. [DOI] [PubMed] [Google Scholar]
- Haiman CA, Stram DO, Wilkens LR, Pike MC, Kolonel LN, Henderson BE, Le Marchand L. Ethnic and Racial Differences in the Smoking-Related Risk of Lung Cancer. The New England journal of medicine. 2006;354(4):333–342. doi: 10.1056/NEJMoa033250. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström K-O. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hendricks PS, Brandon TH. Smoking expectancy associates among college smokers. Addictive Behaviors. 2005;30(2):235–245. doi: 10.1016/j.addbeh.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Herd N, Borland R, Hyland A. Predictors of smoking relapse by duration of abstinence: Findings from the International Tobacco Control (ITC) four country survey. Addiction. 2009;104(12):2088–2099. doi: 10.1111/j.1360-0443.2009.02732.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hrabosky JI, Grilo CM. Body image and eating disordered behavior in a community sample of Black and Hispanic women. Eating Behaviors. 2007;8(1):106–114. doi: 10.1016/j.eatbeh.2006.02.005. [DOI] [PubMed] [Google Scholar]
- Jeffries SK, Catley D, Okuyemi KS, Nazir N, McCarter KS, Grobe JE, Ahluwalia JS. Use of a Brief Smoking Consequences Questionnaire for Adults (SCQ-A) in African American Smokers. Psychology of Addictive Behaviors. 2004;18(1):74–77. doi: 10.1037/0893-164X.18.1.74. [DOI] [PubMed] [Google Scholar]
- Jemal A, Thun MJ, Ries LAG, Howe HL, Weir HK, Center MM, Edwards BK. Annual Report to the Nation on the Status of Cancer, 1975-2005, Featuring Trends in Lung Cancer, Tobacco Use, and Tobacco Control. Journal of the National Cancer Institute. 2008;100(23):1672–1694. doi: 10.1093/jnci/djn389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King B, Dube S, Kaufmann R, Shaw L, Pechacek T. Vital Signs: Current Cigarette Smoking Among Adults Aged ≥18 Years—United States, 2005-2010. JAMA. 2011;306(17):1857–1860. [Google Scholar]
- Kronenfeld LW, Reba-Harrelson L, Von Holle A, Reyes ML, Bulik CM. Ethnic and racial differences in body size perception and satisfaction. Body Image. 2010;7(2):131–136. doi: 10.1016/j.bodyim.2009.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal AM, Trujillo M, Ameringer KJ, Tidey JW, Sussman S, Kahler CW. Anhedonia and the relative reward value of drug and nondrug reinforcers in cigarette smokers. Journal of abnormal psychology. 2014;123(2):375–386. doi: 10.1037/a0036384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molloy BL, Herzberger SD. Body image and self-esteem: A comparison of African-American and Caucasian women. Sex Roles. 1998;38(7-8):631–643. doi: 10.1023/A:1018782527302. [DOI] [Google Scholar]
- Paeratakul S, White MA, Williamson DA, Ryan DH, Bray GA. Sex, Race/Ethnicity, Socioeconomic Status, and BMI in Relation to Self-Perception of Overweight. Obesity research. 2002;10(5):345–350. doi: 10.1038/oby.2002.48. [DOI] [PubMed] [Google Scholar]
- Pang RD, Khoddam R, Guillot CR, Leventhal AM. Depression and anxiety symptoms moderate the relation between negative reinforcement smoking outcome expectancies and nicotine dependence. Journal of studies on alcohol and drugs. 2014;75(5):775. doi: 10.15288/jsad.2014.75.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pang RD, Leventhal AM. Sex differences in negative affect and lapse behavior during acute tobacco abstinence: a laboratory study. Experimental and clinical psychopharmacology. 2013;21(4):269–276. doi: 10.1037/a0033429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pang RD, Zvolensky MJ, Schmidt NB, Leventhal AM. Gender differences in negative reinforcement smoking expectancies. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2015;17(6):750. doi: 10.1093/ntr/ntu226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel K, Hargreaves MK, Liu J, Schlundt D, Sanderson M, Matthews CE, Blot WJ. Relationship between smoking and obesity among women. American Journal of Health Behavior. 2011;35(5):627. doi: 10.5993/ajhb.35.5.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ME. Gender, race, and education differences in abstinence rates among participants in two randomized smoking cessation trials. Nicotine and Tobacco Research. 2010;12(6):647–657. doi: 10.1093/ntr/ntq067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pomerleau CS, Zucker AN, Namenek RJ, Brouwer N, Pomerleau OF, Stewart AJ. Race differences in weight concerns among women smokers: results from two independent samples. Addictive Behaviors. 2001;26(5):651–663. doi: 10.1016/S0306-4603(00)00148-9. [DOI] [PubMed] [Google Scholar]
- Pomerleau CS, Zucker AN, Stewart AJ. Characterizing concerns about post-cessation weight gain: results from a national survey of women smokers. Nicotine & Tobacco Research. 2001;3(1):51–60. doi: 10.1080/14622200125675. [DOI] [PubMed] [Google Scholar]
- Pulvers KM, Catley D, Okuyemi K, Scheibmeir M, McCarter K, Jeffries SK, Ahluwalia JS. Gender, smoking expectancies, and readiness to quit among urban African American smokers. Addictive Behaviors. 2004;29(6):1259–1263. doi: 10.1016/j.addbeh.2004.03.028. [DOI] [PubMed] [Google Scholar]
- Purnell J. Q. PhD, MPH, Peppone L. J. PhD, MPH, Alcaraz KMPH, McQueen A. PhD, Guido JJMS, Carroll JKMD,MPH, Morrow G. R. PhD, MS. Perceived Discrimination, Psychological Distress, and Current Smoking Status: Results From the Behavioral Risk Factor Surveillance System Reactions to Race Module, 2004-2008. American Journal of Public Health. 2012;102(5):844–851. doi: 10.2105/AJPH.2012.300694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reig-Ferrer A, Cepeda-Benito A. Smoking expectancies in smokers and never smokers: An examination of the smoking Consequences Questionnaire-Spanish. Addictive Behaviors. 2007;32(7):1405. doi: 10.1016/j.addbeh.2006.10.004. [DOI] [PubMed] [Google Scholar]
- Reitzel LR, Cromley E, Li Y, Cao Y, Mater RD, Mazas CA, Wetter DW. The effect of tobacco outlet density and proximity on smoking cessation. American Journal of Public Health. 2011;101(2):315–320. doi: 10.2105/AJPH.2010.191676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reitzel LR, Nguyen N, Li N, Xu L, Regan SD, Sturgis EM. Trends in Thyroid Cancer Incidence in Texas from 1995 to 2008 by Socioeconomic Status and Race/Ethnicity. Thyroid : official journal of the American Thyroid Association. 2014;24(3):556–567. doi: 10.1089/thy.2013.0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson JD, Lam CY, Carter BL, Wetter DW, Cinciripini PM. Negative reinforcement smoking outcome expectancies are associated with affective response to acute nicotine administration and abstinence. Drug and Alcohol Dependence. 2012;120(1-3):196–201. doi: 10.1016/j.drugalcdep.2011.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson SA, Webb JB, Butler-Ajibade PT. Body image and modifiable weight control behaviors among black females: a review of the literature. Obesity (Silver Spring, Md.) 2011;20(2):241–252. doi: 10.1038/oby.2011.54. [DOI] [PubMed] [Google Scholar]
- Rogers Wood NA, Petrie TA. Body dissatisfaction, ethnic identity, and disordered eating among African American women. Journal of Counseling Psychology. 2010;57(2):141–153. doi: 10.1037/a0018922. [DOI] [PubMed] [Google Scholar]
- Sánchez-Johnsen L, Ahluwalia JS, Fitzgibbon M. Ethnic similarities and differences in reasons for smoking. Addictive Behaviors [H.W.Wilson - SSA] 2006;31(3):544. doi: 10.1016/j.addbeh.2005.05.029. [DOI] [PubMed] [Google Scholar]
- Sánchez-Johnsen L, Carpentier MR, King AC. Race and sex associations to weight concerns among urban African American and Caucasian smokers. Addictive Behaviors. 2011;36(1-2):14–17. doi: 10.1016/j.addbeh.2010.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sánchez-Johnsen L, Spring BJ, Sommerfeld BK, Fitzgibbon ML. Weight concerns and smoking in Black and White female smokers. Addictive Behaviors. 2005;30(3):601–605. doi: 10.1016/j.addbeh.2004.07.007. [DOI] [PubMed] [Google Scholar]
- Schwartz MB, Brownell KD. Obesity and body image. Body Image. 2004;1(1):43–56. doi: 10.1016/S1740-1445(03)00007-X. [DOI] [PubMed] [Google Scholar]
- Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011. CA: A Cancer Journal for Clinicians. 2011;61(4):212–236. doi: 10.3322/caac.20121. [DOI] [PubMed] [Google Scholar]
- Swan GE, Jack LM, Ward MM. Subgroups of smokers with different success rates after use of transdermal nicotine. Addiction. 1997;92(2):207–17. [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. Allyn and Bacon; Boston: 2001. 1936. [Google Scholar]
- Underwood JM, Townsend JS, Tai E, Davis SP, Stewart SL, White A, Fairley TL. Racial and regional disparities in lung cancer incidence. Cancer. 2012;118(7):1910–1918. doi: 10.1002/cncr.26479. [DOI] [PubMed] [Google Scholar]
- USDHHS Tobacco use among U.S. racial/ethnic minority groups : African Americans, American Indians and Alaska natives, Asian Americans and Pacific Islanders, Hispanics : a report of the Surgeon General. 1998. [PubMed]
- Vidrine JI, Vidrine DJ, Costello TJ, Mazas C, Cofta-Woerpel L, Mejia LM, Wetter DW. The Smoking Consequences Questionnaire: Factor structure and predictive validity among Spanish-speaking Latino smokers in the United States. Nicotine & Tobacco Research. 2009;11(11):1280–1288. doi: 10.1093/ntr/ntp128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson LB, Ancis JR, White DN, Nazari N. Racial identity buffers African American women from body image problems and disordered eating. Psychology of Women Quarterly. 2013;37(3):337–350. doi: 10.1177/0361684312474799. [DOI] [Google Scholar]
- Weinberger AH, George TP, McKee SA. Differences in smoking expectancies in smokers with and without a history of major depression. Addictive Behaviors. 2011;36(4):434–437. doi: 10.1016/j.addbeh.2010.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger AH, McKee SA, George TP. Changes in smoking expectancies in abstinent, reducing, and non-abstinent participants during a pharmacological trial for smoking cessation. Nicotine & Tobacco Research. 2010;12(9):937–943. doi: 10.1093/ntr/ntq120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetter DW, Kenford SL, Smith SS, Fiore MC, Jorenby DE, Baker TB. Gender differences in smoking cessation. Journal of Consulting and Clinical Psychology. 1999;67(4):555–562. doi: 10.1037/0022-006X.67.4.555. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Smith SS, Kenford SL, Jorenby DE, Fiore MC, Hurt RD, Baker TB. Smoking Outcome Expectancies: Factor Structure, Predictive Validity, and Discriminant Validity. Journal of Abnormal Psychology. 1994;103(4):801–811. doi: 10.1037//0021-843x.103.4.801. [DOI] [PubMed] [Google Scholar]