Abstract
We examined suicidal ideation among 399 active duty Soldiers and Marines engaged in mental health treatment. Using a generalized linear model controlling for demographic and military factors, depression, and positive traumatic brain injury screen, we confirmed our hypothesis that self-report measures of current PTSD symptoms uniquely predicted suicidal ideation. The association between PTSD severity and suicidal ideation was moderated by gender with women at higher risk as PTSD severity increased. Female Soldiers and Marines with high levels of PTSD should receive additional monitoring and intervention. Self-report measures may aid with risk assessment and identify symptom-related distress associated with suicide risk.
Keywords: Military Suicide, Suicidal ideation, PTSD, Depression, Traumatic Brain Injury, Active Duty, Army, Marine, Treatment-Engagement
Suicide among United States active duty service members is increasing and is a leading cause of death (Armed Forces Health Surveillance Center, 2012; Black, Gallaway, Bell & Ritchie, 2011). Between 2011 and 2013, suicide rates per 100,000 service members ranged from 23.0 to 29.6 for Soldiers and 15.4 to 23.1 for Marines (Smolenski et al., 2013). Across service branches, Soldiers and Marines comprised a large proportion of the total suicides reported in the 2013 Department of Defense Suicide Event Reports (DoDSERs): Air Force-43 (17.6%), Army-115 (46.9%), Marine Corps-45 (18.4%), and Navy-42 (17.1%). Suicide rates are increasing in parallel with increases in the prevalence of mental illness (Bachynski et al., 2012). The present study examines psychiatric symptoms and suicidal ideation among active duty Soldiers and Marines beginning mental health treatment in randomized controlled trials (RCTs). Our primary aim is to describe how self-reported psychiatric distress is associated with current suicidal ideation, a known precursor to suicide. Our secondary aim is to test whether suicidal thoughts covary with PTSD symptoms over and above other known risks. We also conduct exploratory analyses to assess for the conditional influence of gender on PTSD and suicide ideation.
Suicidal Ideation: Standardized Measures for Risk Assessment
Psychiatric symptomology and comorbidity is common among service members. In the recent Army STARRS study, 25.1% of the large representative sample of non-deployed, active duty U.S. Soldiers met criteria for a disorder within the last 30 days (Kessler et al., 2014). In another study, seventeen percent of the Operation Enduring Freedom and Operation Iraqi Freedom (OEF/OIF) cohort of deployed Army and Marine Corps combatants reported psychiatric symptoms (Smith et al., 2008). Highlighting cumulative risk for developing psychiatric disorders, researchers disaggregated the risk of severe impairment by the age of onset, finding impairment associations with pre-enlistment disorders (21.7%), post-enlistment (24.3%) or both (43.4%). Among service members who attempt or complete suicide, the Marine and Army suicide event reports (DoDSERs) indicate diagnosis with a single disorder, 41.3% (completers) and 59% (attempters), or with comorbid disorders, 20.0% (completers) and 30.0% (attempters) was common (Smolenski et al., 2013). With these prevalence estimates, the potential demand for mental health services among the OEF/OIF cohort is high, and there is an urgent need to effectively match Soldiers and Marines with the most appropriate mental health treatments to prevent loss of life to suicide.
Many service members report suicidal ideation, but do not make a suicide attempt. Moreover, suicidal ideation is relatively common. In a study of deployed service members as many as 30% reported suicidal ideation within the last month (Hill, Johnson & Barton, 2006). However, one-third of individuals with suicidal ideation transition to making a plan, and 72% of those with suicidal plans will attempt (Kessler, Borges, & Walters, 1999). For this reason, standardized assessments of suicidal ideation are valuable for identifying intervals of increased risk. Among DoDSER Marine/Soldier suicide completers, only 11.9% had a history of one or more prior suicide attempts. Given that the majority had no documented prior attempt, measures of elevated, current suicidal ideation may provide a more temporally attuned way to identify risk at any point in time (Smolenski et al., 2013). In fact, over 60% of suicide attempts occur within one year of ideation onset (Nock et al., 2008). At the same time, the relatively high prevalence of suicidal ideation indicates that it is only one contributor to a suicidal crisis. Therefore, assessing for both suicidal thoughts and self-reported psychopathology remain critical components of mental health services for the secondary prevention of suicide.
Vulnerability Stress Models and Suicide Prevention: Proximal, Modifiable Risk
In this investigation we prioritize distinguishing between the stress of proximal PTSD and depression symptoms and control for distal or historical suicide vulnerability factors (Ingram & Luxton, 2005). A limitation of retrospective, epidemiological or administrative studies of suicide attempts or completion is that they rarely have access to patient-reported antecedent stressors, such as symptom-related distress, or the severity of recent suicidal ideation, both of which can precipitate suicidal behaviors. For example, a historical diagnosis of PTSD identified via chart review likely does not confer the same level of acute suicide risk as an assessment indicating severe PTSD symptoms within the last 30 days. We are focusing on the relative importance of current symptomology at the beginning of treatment because unlike a history of diagnosis, it is a potentially modifiable risk factor, particularly with appropriate treatment.
Depression and PTSD have each been shown to differentially impact suicidal ideation, and the relative importance may differ according to what part of the suicidal process (e.g., suicidal ideation, plan, attempts, death) is being predicted (Nock et al. 2013). Major depression is strongly associated with suicidal ideation, but among samples with high levels of suicidal ideation, PTSD is more likely to predict the transition from suicide ideation to attempt (Nock, Hwang, Sampson, & Kessler, 2010; Nock et al., 2009). We hypothesize that PTSD uniquely contributes to the severity of suicidal ideation, even when controlling for depression. We focus on distinguishing PTSD from depression because these disorders are each associated with suicidal ideation and commonly co-occur. Both have standardized measures in routine use that detect recent symptom severity. And, the VA/DoD Clinical Practice Guidelines (VA/DoD CPGs) for PTSD (2010) and depression (2009) recommend routine use of these standardized self-report measures to inform clinical decision-making regarding evidence based treatments.
Proximal symptoms as modifiable risk factors for suicidal ideation
PTSD
PTSD is associated with an increased risk of suicide (American Psychiatric Association, 2004). Rates of PTSD are high among active duty military and positive screens for PTSD tend to increase following a combat deployment (Milliken, Auchterlonie, & Hoge, 2007; Thomas et al., 2010). Even sub-threshold PTSD symptoms have been shown to be significantly, positively associated with the risk for suicidal ideation, after controlling for depression (Marshall et al., 2001). Fortunately, recent RCT findings show that evidence-based treatment for PTSD reduces suicidal thoughts among women (Gradus, Suvak, Wisco, Marx & Resick, 2013). Specifically, a civilian RCT of two PTSD treatments outlined in the VA/DOD PTSD CPGs (2010), cognitive processing therapy and prolonged exposure therapy, each led to significant reductions in suicidal ideation, which were explained by reductions in PTSD symptoms during treatment and were independent from depression diagnoses. We hypothesize that PTSD symptoms are significantly positively associated with suicidal ideation, even after controlling for current depression symptoms.
Gender-based differences in trauma and PTSD symptomology
Research regarding PTSD risk among active duty personnel indicates that associations between traumatic stressors and the experience of PTSD symptoms can vary by gender. Among the U.S. active duty force, women generally reported more PTSD-related distress than men on the re-experiencing, avoidance, emotionally numb, and hyperarousal symptom clusters; but not on hypervigilance (Hourani, Williams, Bray & Kandel, 2015). There were also gender-based differences based on trauma type. Women reported more distress from combat trauma than men, whereas men reported more distress from sexual trauma than women. Women and men also tended to report differences in pre-military trauma, and in readjustment experiences after deployment that can impact the development of PTSD (Street, Vogt, & Dutra, 2009). Given these gender-based differences, we explored whether gender moderates the PTSD and suicidal ideation association in our analyses.
Depression
Depression increases risk of suicide. Over 60% of individuals who complete suicide suffer from depression (Goldney, Wilson, DalGrande, Fisher, & McFarlane, 2000). While depression is an important risk factor for suicide, the widespread prevalence, frequent comorbidity with other disorders, and chronicity of the disorder, mean that diagnosis alone may provide poor specificity for identifying the most acute periods of suicide risk. Service members must receive ongoing depression screening and receive treatment when suffering from episodic increases in symptoms to reduce risk (VA/DoD, 2009). Like PTSD, depression is treatable, especially when identified and treated early, which makes the identification and treatment of depression a high priority for suicide prevention (Goldberg & Steury, 2001). The VA/DoD Depression CPGs (2009) outline the following steps: 1) screen annually for depression, 2) assess suicide risk, 3) obtain a standardized symptom score, 4) diagnose based on Diagnostic and Statistical Manual Criteria, 5) evaluate for alternative diagnosis (e.g., PTSD), then 5) initialize treatment by engaging in “shared decision-making” with the patient (VA/DoD 2009). To test our hypothesis regarding the importance of PTSD as distinct from depression symptoms – an important differentiation to make when selecting a treatment focus (see steps 5 and 6 above) – we aggregated data collected via depression self-report measures across our three study samples to control for associations between depression and current suicidal ideation.
Suicide vulnerability factors: historical and distal control variables
Prior suicide attempts
Several factors contribute to suicide vulnerability that cannot be directly changed. For example, a history of prior suicide attempts helps to identify individuals at higher relative risk for suicide completion, but this personal history is not modifiable.
Traumatic brain injury
Other non-modifiable suicide vulnerability factors based on history include traumatic brain injury (TBI). Among active duty patients referred for a head injury in Iraq, the number of TBIs has been shown to influence suicidal ideation directly when symptoms of depression and PTSD are controlled (Bryan & Clemans, 2013). TBI is also associated with increased risk for both depression and PTSD (Hoge et al., 2004; Hoge et al., 2008; Kreutzer, Seel, & Gourley, 2001; Schneiderman, Braver & Kang, 2008). In the present study, we do not have a measure of current TBI-related impairment or recent TBI-related distress. Therefore, we are limited to including the 4-item TBI-4 history screen (Olson-Madden, Brenner, Forster, Emrick, Corrigan & Thompson, 2010) to control for the predisposing risk of self-reported TBI injury in our model of current suicidal ideation.
Deployment
Among Marines/Soldiers in the 2013 DoDSER report 72.5% of suicide completers and 50.8% of suicide attempters had deployed. Research from prior military cohorts indicated a dose–response effect between the degree of traumatic injury suffered during deployment and suicide risk (Bullman & Kang, 1995). But in a more recent large study, researchers examined the role of the combat experience, number of deployments, and cumulative days deployed, and found no increases in suicide risk (LeardMann et al., 2013; Reger et al., 2015). Although a link was not made to suicide, in a representative Army sample, the number of deployments was positively associated with PTSD and depression (Kessler et al., 2014). Deployment may exacerbate social risks as well. For example, the most commonly identified psychosocial stressor among suicide completers in the DoDSERs was a failed relationship within the last 90 days (Smolenski et al., 2013). Directly comparing these studies is difficult because of differences among samples, study measures and assessment intervals. Due to some divergence among prior research findings, we control for combat deployments.
Summary
Clinicians working with treatment-engaged service members need empirical guidance to effectively develop and implement treatment plans during periods of acute suicide risk. One approach consistent with VA/DoD CPGs is to use standardized measures to guide treatments by assessing for areas of greatest current clinical need. The purpose of our investigation is to evaluate covariation between current suicidal ideation and current self-reported PTSD symptoms at the beginning of research-related treatment. We test whether suicidal ideation severity is associated with PTSD symptom severity. We hypothesize that self-report measures of PTSD symptoms will be significantly associated with current suicidal ideation, even after controlling for other prominent risk factors. Due to research identifying gender-based differences in PTSD symptomology, we conduct exploratory analyses to test for the conditional effect of gender on the association between PTSD and suicidal ideation.
Methods
Procedures
This report presents an analysis of pooled baseline data from three RCTs examining suicide interventions in active duty military personnel (Bryan, 2013; Comtois, McDonnell, & Ries, 2013; Jobes, Comtois, Gutierrez, & Brenner, 2011). Data were collected between 2011 and 2015. Participants were Soldiers and Marines with current suicidal ideation and/or a lifetime suicide attempt. Common exclusion criteria were inability to speak and understand English, psychiatric or medical condition severe enough to preclude consent, and judicially ordered or involuntary treatment. All studies were approved by appropriate military and university IRBs prior to enrollment and all relevant IRBs approved pooling of data for the purposes of secondary data analyses. De-identified, individual, item-level data were pooled into a single dataset containing 399 cases.
Participants
Detailed descriptions of sample characteristics are displayed in the introduction to this special section. Active duty service members (N=399) included in these analyses were Soldiers and Marines (18.7% female) with mean ages ranging from 22–27 years old. The majority of participants were white, and race and ethnicity varied based on the study site. On average, participants had been on active duty for five years and approximately half the sample had served during a combat deployment.
Measures
Suicide ideation dependent variable
All source studies used the Beck Scale for Suicide Ideation – Current (SSI; Beck, Brown, & Steer, 1997), which asks participants to indicate the intensity of 19 items relating to their current attitudes, behaviors, and plans to commit suicide within the last two weeks on a 0 to 2 scale, with higher ratings reflecting more severe suicidal ideation. This self-report measure has demonstrated strong concurrent validity with clinician assessments and strong internal consistency (Luxton, Rudd, Reger & Gahm, 2011). The SSI has demonstrated discriminant validity for identifying suicide attempters and non-attempters (Mann, Waternaux, Haas, & Malone, 1999), predictive validity for completed suicide (Brown, Beck, Steer, & Grisham, 2000), and the measure is sensitive to detecting change, even over a period of 24 hours (Russ, Kashdan, Pollack, & Bajmakovic-Kacila, 1999). The item mean for all 19 SSI items was our outcome variable (range 0–2; alpha in current study = .77).
Posttraumatic Stress predictor variable
The Posttraumatic Stress Disorder Checklist – Military Version (PCL-M; Weathers, Huska, & Keane, 1991) is a 17-item self-report measure that was used to assess PTSD symptom severity based on criteria from the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2000). Respondents rate symptoms in “response to stressful military experiences” over the last month. It has demonstrated excellent test-retest reliability and internal consistency. The measure is used in clinical and non-clinical samples, and among the OEF/OIF cohort to identify PTSD (Elhai, Gray, Kashdan & Franklin, 2005). Due to previous research findings that even subthreshold PTSD increases suicidal ideation, items were summed to create the total symptom severity score ranging from 17–85. Internal consistency (alpha = .93) of the PCL-M in this sample was consistent with other studies. The PTSD variable was standardized in analyses.
Control variables
Demographic and military covariates
We included gender and race covariates. Current relationship status was coded as single/divorced/separated/widowed = 0 and dating/engaged/married = 1. Military covariates included years of military service (a continuous variable, standardized in analyses) and combat deployment (no = 0, yes = 1).
Suicide attempt history covariate
We controlled for a history of previous suicide attempt (no = 0, yes = 1).
Depression covariate
A harmonized measure of current depressive symptoms was created based on the following three self-report measures in use across the source studies. The Patient Health Questionnaire-9 (PHQ-9; Martin, Rief, Klaiberg, & Braehler, 2006), asks participants to indicate the frequency that they were bothered by each of nine symptoms of depression in the last two weeks (0 = Not at all to 3 = Nearly every day). The Outcome Questionnaire-45 (OQ-45; Umphress, Lambert, Smart, Barlow, & Clouse, 1997) asks participants to indicate the frequency of each symptom over the last week on a 5-point scale ranging from 0 = Never to 4 = Almost always. The Beck Depression Inventory II (BDI-II; Beck, Steer, & Brown, 1996) asks participants to rate the severity of 21 symptoms of depression in the last two weeks on a 0 to 3 scale. Across the three instruments, five common symptoms of depression, excluding suicidal ideation, were assessed: (a) little interest or pleasure, (b) depressed mood or hopelessness, (c) change in sleep, (d) fatigue or loss of energy, (e) feelings of worthlessness. Suicide ideation items were omitted from the harmonized measure to avoid a potential confound, since the intended use as a covariate in this study was to control for effects of depression symptoms on suicidal ideation. PHQ-9 and BDI items were rated on a 3-point frequency scale whereas OQ-45 items were rated on a 4-point frequency. We harmonized the OQ-45 items to a 3-point scale by combining the 0 = Never and 1 = rarely responses into a single category. A total score was calculated across the five harmonized symptoms of depression, ranging from 0 to 15, with higher scores reflecting greater depression severity. This variable was standardized for our analyses.
Traumatic brain injury covariate
History of TBI was assessed with a 4-item self-report screen (Olson-Madden, et al., 2010). Participants were asked if they have ever been injured in the neck or head as a result of a fight, fall, or motor vehicle accident, and whether such an injury resulted in loss of consciousness, emergency treatment, or hospitalization. Scoring was dichotomized to indicate a possible history of TBI (1) or likely no history of TBI (0).
Data Analysis
Analyses included data visualization, descriptive statistics, correlations, and a generalized linear model of current suicidal ideation. Using data plots we confirmed that assumptions of linearity were met and standard errors were normally distributed at each level of the outcome variable. We examined Pearson correlations among covariates, PTSD, and suicidal ideation. Using the Statistical Package for Social Sciences (IBM, 2015) we ran a generalized linear model using maximum likelihood estimation to test our hypothesis that self-reported PTSD symptoms covary with current suicidal ideation; 337 complete cases were included in the model. Prior to modeling our three continuous variables (years of service, depression and PCL-M scores) were standardized as z-scores. We controlled for the contributions of other risk factors, such as a prior suicide attempt, possible history of TBI, as well as concurrent depression, which could be an alternative focus of clinical attention. We also adjusted for gender, race, current relationship status, years of military service, and combat deployment. Due to research finding gender differences in PTSD-related distress, we tested whether gender moderated the PTSD and suicidal ideation relationship.
Results
Descriptive Statistics
Descriptive statistics and Pearson correlations for the model variables are displayed in Table 1. The bottom row of Table 1 displays either the scale mean and standard deviation (for continuous variables) or the percent coded as 1 (for dichotomous variables). The modal number of previous suicide attempts was one. Female service members had been in the military fewer years and served fewer combat deployments. Female service members were significantly less likely to be in a current relationship (dating, engaged or married) and reported significantly more previous suicide attempts. The average score on the PCL-M in this sample (49.54) is consistent with a probable diagnosis of PTSD. Higher PTSD symptom severity was associated with more service years and combat deployment. Approximately 4 out of 5 service members reported a possible traumatic brain injury. A positive TBI screen was significantly correlated with depression, but not PTSD. PTSD and depression were significantly positively associated with current suicidal ideation.
Table 1.
Means, Standard Deviations, and Intercorrelations for Model Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Gender | – | .02 | −.11* | −.11* | −.20** | .15** | .00 | .06 | .00 | .08 |
| 2. Race | – | .05 | .00 | .02 | .01 | .04 | .02 | .03 | .02 | |
| 3. Relationship | – | .20** | .24** | −.11* | −.08 | −.02 | .13** | −.05 | ||
| 4. Years served | – | .52** | −.16** | −.09 | −.02 | .23** | −.11* | |||
| 5. Deployment | – | −.12* | −.09 | −.06 | .22* | −.01 | ||||
| 6. Prior attempt | – | −.05 | −.01 | −.06 | −.22** | |||||
| 7. TBI history | – | .11* | .04 | .01 | ||||||
| 8. Depression | – | .57** | .23** | |||||||
| 9. PTSD | – | .14** | ||||||||
| 10. Suicidal ideation | – | |||||||||
| Mean Percent or (SD) |
18.7 | 50.7 | 44.8 | 5.10 (4.98) |
56.4 | 49.0 | 79.8 | 9.29 (3.75) |
49.45 (16.62) |
1.01 (.34) |
Note. For dichotomous variables the bottom row displays the percent coded as 1. 1. Gender (male = 0; % female). 2. Race (white = 0; % non-white). 3. Relationship (in current relationship; 0 = no/1= yes; % in not in relationship). 4. Years of military service. 5. Combat deployment (0 = no/1 = yes; % deployed). 6. History of suicide attempt (0 = no/1 = yes; % with history of attempt). 7. History of traumatic brain injury (0 = no/1 = yes; % with history of TBI). 8. Harmonized depression measure. 9. PTSD = Posttraumatic stress checklist – Military version. 10. Average item score on Beck Suicidal Ideation Inventory. M = mean; SD = standard deviation.
p < .05.
p < .01.
Analyses
In our generalized linear model (see Table 2), the most robust predictors of current suicidal ideation were two covariates: the harmonized measure of depression (with suicidal ideation items omitted) and reporting a history of a prior suicide attempt. Consistent with our hypothesis, the full model with PTSD and the PTSD by gender interaction (df = 10; log likelihood = −95, AIC 214, BIC 260) provided a significantly better fit to the data X2 (2, N = 337) = 10, p <.01, than the restricted depression model without PTSD and the PTSD by gender interaction (df = 8; log likelihood = −100, AIC 220, BIC 259). The association between PTSD symptoms and suicidal ideation depended on gender. The significant gender by PTSD interaction indicated a stronger positive association between PTSD and suicidal ideation for women (see Figure 1), with the mean suicidal ideation score for women crossing over the mean for men when PTSD symptom severity exceeded cut-points for probable PTSD diagnosis (PCL-M scores > 45–50 in treatment-engaged military samples). The overall model accounted for 12.7% of the variance in suicidal ideation, but the equation for the fit line for men (R2 = .05) accounted for less variance than did the fit line for women (R2 = .69).
Table 2.
Generalized linear model of current suicidal ideation
| Predictors | B | SE | 95% Confidence Interval | Wald Chi-Square | p | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Intercept | 0.934 | 0.051 | 0.834 | 1.035 | 330.880 | 0.000 |
| 1. Gender | 0.031 | 0.048 | −0.063 | 0.125 | 0.422 | 0.516 |
| 2. Race | −0.037 | 0.036 | −0.107 | 0.034 | 1.031 | 0.310 |
| 3. Relationship | −0.013 | 0.037 | −0.086 | 0.060 | 0.117 | 0.732 |
| 4. Years of service* | −0.035 | 0.020 | −0.075 | 0.004 | 3.058 | 0.080 |
| 5. Combat deployment | 0.046 | 0.044 | −0.040 | 0.131 | 1.110 | 0.292 |
| 6. History of attempt | 0.136 | 0.036 | 0.066 | 0.206 | 14.463 | 0.000 |
| 7. TBI history | −0.032 | 0.050 | −0.130 | 0.066 | 0.400 | 0.527 |
| 8. Depression* | 0.081 | 0.022 | 0.037 | 0.124 | 13.123 | 0.000 |
| 9. PCL-M* | −0.011 | 0.025 | −0.060 | 0.037 | 0.207 | 0.649 |
| 10. Gender × PTSD | 0.101 | 0.045 | 0.013 | 0.189 | 5.059 | 0.024 |
Note. Model n = 337.
Continuous variables were standardized. 1. Gender (male = 0). 2. Race (white = 0). 3. Relationship (in current relationship; 0 = no/1= yes). 4. Years of military service. 5. Combat deployment (0 = no/1 = yes). 6. History of suicide attempt (0 = no/1 = yes). 7. History of traumatic brain injury (0 = no/1 = yes). 8. Harmonized depression measure. 9. PTSD = Posttraumatic stress checklist – Military version. 10. Interaction between gender and PTSD symptom severity. B = unstandardized beta. SE = standard error. R2 for model = 12.7.
Figure 1. Gender moderates the relationship between PTSD symptom severity and suicidal ideation.
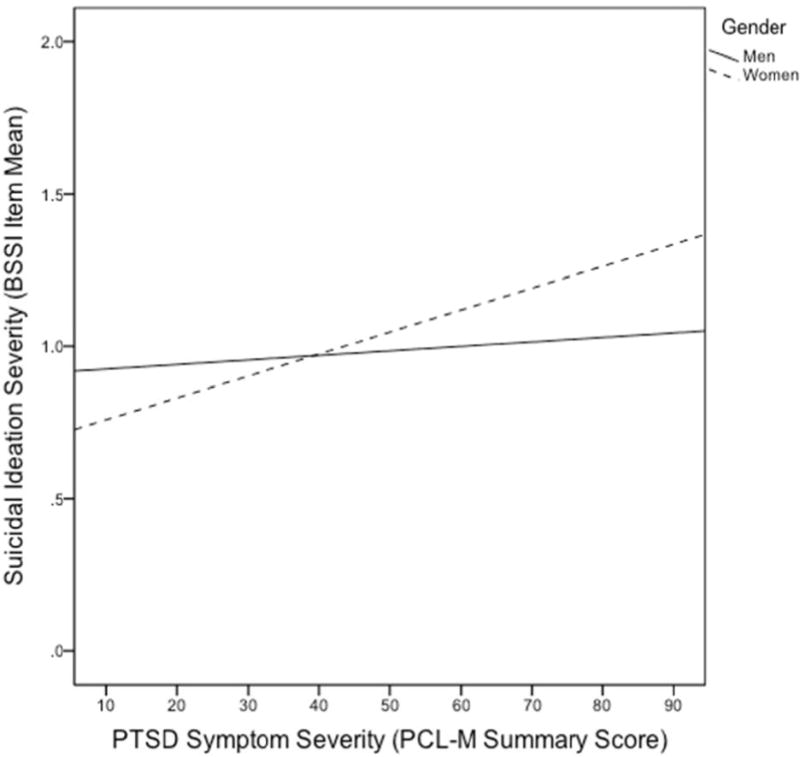
Note: The dependent variable (DV) is the item mean across the 19 items from the Beck Scale for Suicide Ideation (BSSI; range 0–2) and is listed on the y-axis. The independent variable (IV) is Posttraumatic Stress Disorder (PTSD) symptom severity assessed with the PTSD Checklist – Military Version (PCL-M; range 17–85) and listed on the x-axis. The gender moderator variable (MV) is identified by line (Men = 0) or dotted line (Women = 1) in the legend.
Discussion
This study examined the strength of associations among current PTSD symptoms assessed via self-report, other suicide vulnerability factors, and current suicidal ideation. We focused on PTSD symptom-related distress, which has the potential to be modifiable with evidence-based treatment, and we differentiated this proximal risk from depression and distal/historical vulnerability control variables in our model. The average score on the PCL-M in this sample is consistent with a probable diagnosis of PTSD, based on cut-points used in military studies. The relationship between PTSD symptoms and suicidal ideation was conditional based on gender. Among women, the positive association between suicidal ideation and PTSD was stronger as PTSD symptom severity increased.
Our findings indicate that among female service members in treatment, those with more severe PTSD symptoms may be at greater risk for suicide. Female Soldiers and Marines with high levels of PTSD should be closely monitored and offered empirically supported treatments shown to reduce PTSD symptoms, and thereby suicidal thoughts (Gradus, Suvak, Wisco, Marx & Resick, 2013). Female service members may also benefit from suicide-specific interventions (Jobes, Wong, Conrad, Drozd, & Neal-Walden, 2005). These findings should be considered within the research literature highlighting differential experiences of PTSD symptomology among male and female service members (Hourani, Williams, Bray & Kandel, 2015). We did not propose an a priori directional hypothesis about how gender would interact with PTSD to predict suicidal ideation, in part because the PCL-M does not identify a specific traumatic stressor (e.g., combat versus sexual assault). Therefore, we were not able to account for the prevalence of military sexual trauma, which is likely to be higher among women than men (Lipari, Cook, Rock, & Matos, 2008), and we did not assess for childhood or pre-enlistment trauma, which is also likely to vary by gender (Street et al., 2009). Pre-military sexual trauma and military sexual trauma have both been shown to differentially impact suicidal ideation, plans, and attempts for men and women (Bryan, Bryan, & Clemans, 2015). Male and female Soldiers and Marines may experience other differences in stressors related to their service that are not captured in our study (Street et al., 2015). In addition, there were other gender differences in this sample that may contribute to our findings. Women were significantly less likely to endorse a current relationship than men and women also reported significantly more previous suicide attempts.
In the present analyses, a previous suicide attempt remained one of the strongest predictors of current suicidal ideation. Suicidal ideation is strongly associated with future suicide attempts and completion, and in this cross-sectional study, we only assessed current suicidal ideation not a history of past ideation. Although no single risk factor, or set of risk factors, provides reliable prediction of which individuals will die by suicide, our findings are consistent with best practices, including screening for current suicidal ideation, and asking about a history of prior suicide attempts (VA/DoD, 2009).
We did not observe the independent contribution of positive TBI screens to suicidal ideation that was observed among military personnel receiving TBI-related medical attention in theatre (Bryan & Clemans, 2013). Positive screenings for TBI in this study were high (80%) as compared to other military mental health treatment seeking samples, such as patients in the Veterans Health Administration (Brenner et al., 2013). Beyond setting and sub-population differences, another explanation for our discrepant findings is the potential for measurement error associated with the 4-item TBI screen. In another study, the sensitivity (.74) and specificity (.56) analyses for this screener indicated that it may have limited specificity as compared to more extensive expert assessment, or screens that include past and current TBI-related symptoms (Brenner et al., 2013; Bryan & Clemans, 2013).
Limitations
Suicidal ideation is but one measure of suicide risk and this is a cross-sectional study, not a prospective study or population-level epidemiological investigation. The present study did not examine suicide attempts or suicide completion rates as outcomes. Instead, the focus of the present investigation was on potential associations between self-report measures that have strong psychometric properties, are commonly used to assess for symptoms of PTSD and depression, and are validated for use among the active duty population. Self-report measures provide strengths as an affordable and efficient way for mental health clinicians and researchers to identify probable PTSD or depression and acute suicidal ideation. However, there are also measurement limitations with using self-report measures of psychiatric symptomology that may interfere with the ability to parse out the unique variance associated with one particular disorder. For example, rather than distinguishing between PTSD and depression, our measures may be tapping generalized distress rather than specific aspects of either disorder (Arbisi et al., 2012).
Although we used standardized, validated measures of suicidal ideation and PTSD, due to our need to harmonize depression measures across studies, the advantages to using standardized depression measures were unavailable. We were interested in accounting for the relative contribution of PTSD symptoms to suicidal ideation over and above depression symptoms, and enlisted the advantages of using data harmonization methods to create a combined measure of depression across studies and military duty stations. This was necessary to account for current depression symptoms in our analyses, but is a suboptimal way to measure depression. Unlike our PTSD predictor variable, we were not able to compare our samples’ depression severity with validated population norms. Despite this, we identified a strong relationship between depression and suicidal ideation, even after removing suicidality items, which were likely to be confounded without suicidal ideation outcome. This strong correlational finding supports the validity of the harmonized depression measure. Use of measure harmonization and z-score transformation for analyses enabled us to pool data across clinical settings, but use of the same depression measure at each site would have strengthened our study (Eton et al., 2014).
Finally, these active duty samples were engaged in treatment studies and participants may or not be representative of treatment-seeking military personnel outside of the research context. For example, participants were included due to high levels of suicidal ideation or previous suicide attempts. However, given that measures were collected at baseline of a treatment study conducted at their local duty station, there is still a high potential for the generalization of these findings to other active duty personnel beginning mental health treatment on base. The study confers strengths of assessing for associations with suicidal ideation at the baseline of a treatment-episode and our findings point to potentially fruitful areas for future research.
Future Research Directions
Future research should capitalize on ongoing improvements in PTSD measurement that might better unpack our gender-based interaction findings. The newly validated Clinician Administered PTSD Scale (CAPS-5; Weathers et al., 2013) and the new self-report PTSD Checklist (PCL-5; Weathers et al., 2013) were both developed to be consistent with the DSM-5 diagnostic criteria (American Psychiatric Association, 2013). The PCL-5 asks about symptoms related to a specific traumatic stressor and there are no longer separate civilian and military versions of the PCL. This is an important improvement because the PCL-M does not ask about a specific traumatic stressor, and previous research indicates that male and female service members’ PTSD-related distress can vary based on trauma type (Street et al., 2009). Gender has also been shown to moderate the factor structure of PTSD (Elhai & Palmieri, 2011) and the interaction between gender and PTSD in predicting suicidal ideation should be re-examined with the new DSM-5 criteria, using the new measures in other active duty samples.
Conclusions
It is a national priority to reduce rates of suicide among the military (Armed Forces Health Surveillance Center, 2012; Black, Gallaway, Bell, & Ritchie, 2011). Our study assessed several military-specific factors related to suicide risk among active duty military. Despite some diversity in previous research regarding the relative contribution of a given risk factor or set of risk factors, a central finding is the increase in suicide risk associated with functional impairments or recent increases in distress (Marshall et al., 2001). Among service members seeking help, the use of standardized assessments to identify current psychiatric symptoms and current suicidal ideation is critical for meeting the treatment needs of both male and female Soldiers and Marines.
Acknowledgments
This work was in part supported by the Military Suicide Research Consortium (MSRC), an effort supported by the Office of the Assistant Secretary of Defense for Health Affairs under Award No. (W81XWH-10-2-0181). Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the MSRC or the Department of Defense. This work was in part supported by the Military Operational Medicine Research Program (MOMRP) and the US Army Medical Research and Material Command (USAMRMC) Telemedicine and Advanced Technology Research Center (TATRC) under Award No. (W81XWH-11-1-0164). Opinions, interpretations, conclusions and recommendations are those of the authors and not necessarily endorsed by the MOMRP, USAMRMC, TATRC, or the Department of Defense. Research reported in this publication was also supported by the National Institute on Alcohol Abuse and Alcoholism under award number T32 AA007455 and National Institute of Mental Health under award number T32 MH082709. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The National Institute on Alcohol Abuse and Alcoholism and National Institute of Mental Health had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 2000. text rev. [Google Scholar]
- American Psychiatric Association. Practice Guidelines for the Treatment of Psychiatric Disorders Compendium. 2nd. VA: Arlington: 2004. Practice guidelines for the assessment and treatment of patients with suicidal behaviors; pp. 835–1027. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Washington, DC: Author; 2013. [Google Scholar]
- Arbisi PA, Kaler ME, Kehle-Forbes SM, Erbes CR, Polusny MA, Thuras P. The predictive validity of the PTSD Checklist in a nonclinical sample of combat-exposed National Guard troops. Psychological Assessment. 2012;24(4):1034–1040. doi: 10.1037/a0028014. http://doi.org/10.1037/a0028014. [DOI] [PubMed] [Google Scholar]
- Armed Forces Health Surveillance Center (AFHSC) Deaths by suicide while on active duty, active and reserve components, US Armed Forces, 1998–2011. Medical Surveillance Monthly Report. 2012;19(6):7–10. [PubMed] [Google Scholar]
- Bachynski KE, Canham-Chervak M, Black SA, Dada EO, Millikan AM, Jones BH. Mental health risk factors for suicides in the US Army, 2007–2008. Injury Prevention. 2012 doi: 10.1136/injuryprev-2011-040112. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown GK, Steer RA. Psychometric characteristics of the scale for suicide ideation with psychiatric outpatients. Behavior Research and Therapy. 1997;35:1039–1046. doi: 10.1016/S0005-7967(97)00073-9. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Black SA, Gallaway MS, Bell MR, Ritchie EC. Prevalence and risk factors associated with suicides of army soldiers 2001–2009. Military Psychology. 2011;23(4):433–451. doi: 10.1037/h0094766. [DOI] [Google Scholar]
- Brenner LA, Homaifar BY, Olson-Madden JH, Nagamoto HT, Huggins J, Schneider AL, Corrigan JD. Prevalence and screening of traumatic brain injury among veterans seeking mental health services. Journal of Head Trauma and Rehabilitation Services. 2013;28(1) doi: 10.1097/HTR.0b013e31827df0b5. [DOI] [PubMed] [Google Scholar]
- Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. Journal of Consulting and Clinical Psychology. 2000;68(3):371–377. doi: 10.1037//0022-006X.68.3.371. [DOI] [PubMed] [Google Scholar]
- Bryan CJ. Brief Cognitive Behavioral Therapy for Military Populations. 2011 Retrieved May 5, 2015 from https://clinicaltrials.gov/ct2/show/NCT02038075.
- Bryan CJ, Bryan AO, Clemans TA. The association of military and premilitary sexual trauma with risk for suicide ideation, plans, and attempts. Psychiatry Research. 2015;227(2–3):246–252. doi: 10.1016/j.psychres.2015.01.030. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Clemans TA. Repetitive traumatic brain injury, psychological symptoms, and suicide risk in a clinical sample of deployed military personnel. JAMA Psychiatry. 2013;70(7) doi: 10.1001/jamapsychiatry.2013.1093.. [DOI] [PubMed] [Google Scholar]
- Bullman TA, Kang HK. Posttraumatic stress disorder and the risk of traumatic deaths among Vietnam veterans. The Journal of Nervous and Mental Disease. 1994;182(11):604–10. doi: 10.1097/00005053-199411000-00002. [DOI] [PubMed] [Google Scholar]
- Comtois KA, McDonell MG, Ries RK. Military Continuity Project (MCP) 2013 Retrieved May 5, 2015 from https://clinicaltrials.gov/ct2/show/study/NCT01829620?term=comtois&rank=1.
- Department of Veterans Affairs and Department of Defense. VA/DoD Clinical practice guideline for the management of major depressive disorder (MDD) 2009 Retrieved on July 1, 2015 from: http://www.healthquality.va.gov/guidelines/MH/mdd/MDDFULL053013.pdf.
- Department of Veterans Affairs and Department of Defense. VA/DoD Clinical practice guideline for the management of post-traumatic stress. 2010 Retrieved on July 1, 2015 from: http://www.healthquality.va.gov/guidelines/MH/ptsd/cpgPTSDFULL201011612c.pdf.
- Elhai JD, Gray MJ, Kashdan TB, Franklin CL. Which instruments are most commonly used to assess traumatic event exposure and posttraumatic effects? A survey of traumatic stress professionals. Journal of Traumatic Stress. 2005;18:541–545. doi: 10.1002/jts.20062. [DOI] [PubMed] [Google Scholar]
- Elhai JD, Palmieri PA. The factor structure of posttraumatic stress disorder: A literature update, critique of methodology, and agenda for future research. Journal of Anxiety Disorders. 2011;25(5):849–854. doi: 10.1016/j.janxdis.2011.04.007. [DOI] [PubMed] [Google Scholar]
- Eton DT, Beebe TJ, Hagen PT, Halyard MY, Montori VM, Naessens JM, Wood DL. Harmonizing and consolidating the measurement of patient-reported information at health care institutions: a position statement of the Mayo Clinic. Patient Related Outcome Measures. 2014;5:7–15. doi: 10.2147/PROM.S55069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg RJ, Steury S. Depression in the workplace: costs and barriers to treatment. Psychiatric Services. 2001;52:1639–43. doi: 10.1176/appi.ps.52.12.1639. [DOI] [PubMed] [Google Scholar]
- Goldney RD, Wilson D, DalGrande E, Fisher LJ, McFarlane AC. Suicidal ideation in a random community sample: attributable risk due to depression and psychosocial and traumatic events. Australian and New Zealand Journal of Mental Health Nursing. 2000;34:98–106. doi: 10.1046/j.1440-1614.2000.00646.x. [DOI] [PubMed] [Google Scholar]
- Gradus JL, Suvak MK, Wisco BE, Marx BP, Resick PA. Treatment of posttraumatic stress disorder reduced suicidal ideation. Depression and Anxiety. 2013;30(10):1046–1053. doi: 10.1002/da.22117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, Mc-Gurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. soldiers returning from Iraq. New England Journal of Medicine. 2008;358(5):453–463. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- Hill JV, Johnson RC, Barton RA. Suicidal and homicidal soldiers in deployment environments. Military Medicine. 2006;171(3):228–232. doi: 10.7205/milmed.171.3.228. [DOI] [PubMed] [Google Scholar]
- Hourani L, Williams J, Bray R, Kandel D. Gender differences in the expression of PTSD symptoms among active duty military personnel. Journal of Anxiety Disorders. 2015;29:101–108. doi: 10.1016/j.janxdis.2014.11.007. http://doi.org/10.1016/j.janxdis.2014.11.007. [DOI] [PubMed] [Google Scholar]
- IBM Corporation. IBM SPSS Statistics for Windows, Version 23. Armonk, NY: IBM Corp; 2015. [Google Scholar]
- Ingram RE, Luxton DD. Vulnerability-stress models. In: Hankin BL, Abela JRZ, editors. Development of psychopathology: A vulnerability-stress perspective. London: Sage; 2005. pp. 32–46. [Google Scholar]
- Jobes DA, Wong SA, Conrad AK, Drozd JF, Neal-Walden T. The collaborative assessment and management of suicidality versus treatment as usual: A retrospective study with suicidal outpatients. Suicide & Life Threatening Behavior. 2005;35(5):483–497. doi: 10.1521/suli.2005.35.5.483. [DOI] [PubMed] [Google Scholar]
- Jobes D, Comtois KA, Gutierrez P, Brenner L. Operation Worth Living Project With Suicidal Soldiers at Ft. Stewart (OWL) 2011 Retrieved May 5, 2015 from https://clinicaltrials.gov/ct2/show/study/NCT01300169?term=jobes+suicide&rank=1.
- Kessler RC, Borges B, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617.. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Heeringa SG, Stein MB, Colpe LJ, Fullerton CS, Hwang I, Ursano RJ. Thirty-day prevalence of DSM-IV mental disorders among nondeployed soldiers in the us army. JAMA Psychiatry. 2014;71(5):504–10. doi: 10.1001/jamapsychiatry.2014.28. http://doi.org/10.1001/jamapsychiatry.2014.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreutzer JS, Seel RT, Gourley E. The prevalence and symptom rates of depression after traumatic brain injury: A comprehensive examination. Brain Injury. 2001;15(7):563–576. doi: 10.1080/02699050010009108. [DOI] [PubMed] [Google Scholar]
- LeardMann CA, Powell TM, Smith TC, Bell MR, Smith B, Boyko EJ, Hoge CW. Risk factors associated with suicide in current and former us military personnel. Journal of the American Medical Association. 2013;310(5):496–11. doi: 10.1001/jama.2013.65164. http://doi.org/10.1001/jama.2013.65164. [DOI] [PubMed] [Google Scholar]
- Lipari RN, Cook PJ, Rock LM, Matos K. 2006 Gender Relations Survey of Active Duty Members. Arlington, VA: Department of Defense Manpower Data Center; 2008. (DMDC Report No. 2007-002). [Google Scholar]
- Luxton DD, Rudd MD, Reger MA, Gahm GA. A psychometric study of the Suicide Ideation Scale. Archives of Suicide Research. 2011;15(3):250–258. doi: 10.1080/13811118.2011.589720. [DOI] [PubMed] [Google Scholar]
- Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. American Journal of Psychiatry. 1999;156:181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- Marshall RD, Olfson M, Hellman F, Blando C, Guardino M, Struening EL. Comorbidity, impairment, and suicidality in subthreshold PTSD. American Journal of Psychiatry. 2001;158(9):1467–1473. doi: 10.1176/appi.ajp.158.9.1467. [DOI] [PubMed] [Google Scholar]
- Martin A, Rief W, Klaiberg A, Braehler E. Validity of the brief Patient Health Questionnaire Mood Scale (PHQ-9) in the general population. General Hospital Psychiatry. 2006;28:71–77. doi: 10.1016/j.genhosppsych.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. Journal of the American Medical Association. 2007;298:2141–2148. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiologic Reviews. 2008;30:133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Deming CA, Fullerton CS, Gilman SE, Goldenberg M, Kessler RC, Ursano RJ. Suicide among soldiers: a review of psychosocial risk and protective factors. Psychiatry. 2013;76(2):97–125. doi: 10.1521/psyc.2013.76.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson N, Kessler RC. Mental disorders, comorbidity, and suicidal behaviors: Results from the National Comorbidity Survey Replication. Molecular Psychiatry. 2010;15(8):868–876. doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A, Ursano RJ. Cross-national analysis of the associations among mental disorders and suicidal behavior: Findings from the WHO World Mental Health Surveys. PLOS Medicine. 2009;6:e1000123. doi: 10.1371/journal.pmed.1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson-Madden JH, Brenner LA, Forster JEF, Emrick CD, Corrigan JD, Thompson C. Traumatic brain injury and psychiatric diagnoses in veterans seeking outpatient substance abuse treatment. Journal of Head Trauma Rehabilitation. 2010;225(6):470–479. doi: 10.1097/HTR.0b013e3181d717a7. [DOI] [PubMed] [Google Scholar]
- Reger MA, Smolenski DJ, Skopp NA, Metzger-Abamukang MJ, Kang HK, Bullman TA, Gahm GA. Risk of suicide among US military service members following Operation Enduring Freedom or Operation Iraqi Freedom deployment and separation from the US military. JAMA Psychiatry. 2015;72(6):561–569. doi: 10.1001/jamapsychiatry.2014.3195. [DOI] [PubMed] [Google Scholar]
- Russ MJ, Kashdan T, Pollack S, Bajmakovic-Kacila S. Assessment of suicide risk 24 hours after psychiatric hospital admission. Psychiatric Services. 1999;50:1491–1493. doi: 10.1176/ps.50.11.1491. [DOI] [PubMed] [Google Scholar]
- Schneiderman AI, Braver ER, Kang HK. Understanding sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in Iraq and Afghanistan: Persistent postconcussive symptoms and posttraumatic stress disorder. American Journal of Epidemiology. 2008;167(12):1446–1452. doi: 10.1093/aje/kwn068. [DOI] [PubMed] [Google Scholar]
- Smith TC, Ryan MAK, Wingard DL, Slymen DJ, Sallis JF, Kritz–Silverstein D. New onset and persistent symptoms of post-traumatic stress disorder self reported after deployment and combat exposures: prospective population based US military cohort study. British Medical Journal. 2008;336:366–371. doi: 10.1136/bmj.39430.638241.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smolenski DJ, Reger MA, Bush N, Skopp NA, Zhang Y, Campise RL. Department of defense suicide event report: Calendar year 2013 annual report. Silver Spring, MD: National Center for Telehealth and Technology; 2013. Accessed July 9, 2015 from http://t2health.org/programs/DoDser. [Google Scholar]
- Street AE, Vogt D, Dutra L. A new generation of women veterans: Stressors faced by women deployed to Iraq and Afghanistan. Clinical Psychology Review. 2009;29(8):685–694. doi: 10.1016/j.cpr.2009.08.007. http://doi.org/10.1016/j.cpr.2009.08.007. [DOI] [PubMed] [Google Scholar]
- Street A, Gilman S, Rosellini A, Stein M, Bromet E, Cox K, Kessler R. Understanding the elevated suicide risk of female soldiers during deployments. Psychological Medicine. 2015;45(04):717–726. doi: 10.1017/S003329171400258X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, Hoge CW. Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Archives of General Psychiatry. 2010;67:614–623. doi: 10.1001/archgenpsychiatry.2010.54. [DOI] [PubMed] [Google Scholar]
- Umphress VJ, Lambert MJ, Smart DW, Barlow SH, Clouse G. Concurrent and construct validity of the Outcome Questionnaire. Journal of Psychoeducational Assessment. 1997;15:40–55. [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) 2013 doi: 10.1037/pas0000486. Scale available from the National Center for PTSD at www.ptsd.va.gov. [DOI] [PMC free article] [PubMed]
- Weathers FW, Huska JA, Keane TM. PCL-M for DSM-IV. Boston: National Center for PTSD –Behavioral Science Division; 1991. [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) 2013 Scale available from the National Center for PTSD at www.ptsd.va.gov.


