Abstract
PURPOSE
To evaluate spherical aberration and through-focus optical performances of 5 premium and 2 monofocal intraocular lenses (IOLs) in optical bench tests.
SETTING
Flaum Eye Institute, University of Rochester, Rochester, New York, USA.
METHODS
Five premium IOLs, ReSTOR +4D (SN6AD3), ReSTOR +3D (SA6AD1), ReZoom (NXG1), Tecnis multifocal (ZM900) and Crystalens HD (HD500), were tested using an optical bench system consisting of a wet cell with an artificial pupil, a custom-developed Shack-Hartmann wavefront sensor, and an image capturing device. Two monofocal IOLs, SofPort AO (LI60AOV) and AcrySof (SN60AT), were used as controls. No accommodation was simulated in the system. The spherical aberration profiles of each IOL were measured using the wavefront sensor. Through-focus images of a 1951 United States Air Force resolution target were analyzed. To evaluate image quality cross-correlation coefficients, comparing the likenesses of captured images and perfect reference image, were calculated.
RESULTS
For a 5 mm pupil the SN6AD3, SA6AD1, NXG1, ZM900 and HD500 premium IOLs had spherical aberrations of −0.27 μm, −0.24 μm, −0.35 μm, −0.33 μm and +0.12 μm, respectively. Image quality for distant objects was poorer with multifocal and accommodating IOLs than with monofocal IOLs. All multifocal IOLs had effective distant and near image quality, but showed loss in intermediate image quality. Due to bispheric optic design, an accommodating IOL, HD 500, showed slightly increased depth of field compared with the monofocal IOLs.
CONCLUSIONS
Each premium IOL has different design strategy and optical characteristics, including spherical aberration profile and through-focus image quality. Thus, the choice of premium IOLs should be based on optical characteristics.
INTRODUCTION
Presbyopia, the age-related loss of accommodation resulting in poor near vision,1 has substantial negative effects on quality of life.2 Because presbyopia eventually affects everyone, developing an effective solution and achieving a better understanding of its underlying mechanism have become increasingly important in ophthalmology. Presbyopia may be corrected by cataract surgery, followed by the implantation of several types of premium intraocular lenses (IOLs), including accommodating and multifocal IOLs. Accommodating IOLs are designed to mimic natural accommodation in response to ciliary muscle contraction by shifting axially in the eye via hinged haptics.3 Crystalens (Bausch & Lomb; Rochester, New York, USA), an accommodating IOL approved by the United States Food and Drug Administration (US FDA), may function through accommodative lens arching, which creates a central refractive power gradient.4 Other accommodating IOLs, such as Synchrony (Abbott Medical Optics; Santa Clara, California, USA), which has dual-optics, are currently in clinical trials.5
Multifocal IOLs have specially designed optics to allow for both distance and near vision by increasing the depth of focus. These IOLs include ReZoom (Abbott Medical Optics), ReSTOR (Alcon Laboratories; Fort Worth, Texas, USA), and Tecnis multifocal (Abbott Medical Optics) all of which have been approved by the US FDA. Each IOL has unique optic designs, with these three having zonal refractive, apodized diffractive, and full-optic diffractive designs, respectively.5–7 Regardless of their optic designs, these multifocal IOLs are designed to produce multiple focal points and simultaneous vision of distant and near objects. Although this basic mechanism increases depth of field, it compromises distance image quality, an important limitation of multifocal IOLs when compared with accommodating or monofocal IOLs.8–10 Many clinical studies have assessed the image quality of multifocal IOLs.10–12 Although these studies were designed to represent realistic conditions, there were limited in their ability to control for other factors, such as corneal aberrations and natural pupil diameters. Therefore, it is important to first examine differences in optical performance of these IOLs, independent from other factors. Optical bench testing of IOLs can quantify through-focus image quality objectively, thus allowing cataract surgeons to select the optimal IOLs for each individual patient.
A few studies to date have evaluated the optical performance of premium IOLs in optical bench systems,13–15 but even these studies did not assess through-focus image quality. Moreover, little has been done to quantify higher order aberrations of these premium IOLs.
To further understand the optical performance of premium IOLs, we tested them in an optical bench system. These tests included measurements of wavefront errors and analysis of through-focus images to simulate distance and near visual quality for different pupil sizes.
MATERIALS AND METHODS
Intraocular Lenses
We studied 5 premium IOLs with 20 diopters (D): ReSTOR +4D (SN6AD3, Alcon Laboratories), ReSTOR +3D (SA6AD1, Alcon Laboratories), ReZoom (NXG1, Abbott Medical Optics), Tecnis multifocal (ZM900, Abbott Medical Optics) and Crystalens HD (HD500, Bausch & Lomb).
Each IOL has different strategies to improve near vision. ReSTOR has an apodized diffractive multifocal optic, covering the central 3.6 mm of the total 6.0 mm optical zone.8, 16 ReZoom has a zonal refractive multifocal optic.15 Tecnis has a full-aperture diffractive multifocal optic.15 The Crystalens HD is an accommodating IOL with a bispheric design, with positive power added to the central optical zone.17 For comparison, we also studied 2 monofocal IOLs, SofPort AO (LI60AOV, Bausch & Lomb) and AcrySof (SN60AT, Alcon Laboratories).
SofPort AO has an aspheric aberration-free optic, whereas AcrySof has a spherical optic. All IOLs had an optic diameter of 6.0 mm, except for HD500, which has an optic diameter of 5.0 mm.
Optical Bench Testing System
A schematic of the optical bench metrology, developed to measure the optical properties of IOLs in vitro, is shown in Figure 1 A. The wavefront profile of each IOL was measured with a Shack-Hartmann wavefront sensor equipped with a 635 nm wavelength laser-diode (OZ Optics, Ottawa, Ontario, Canada). The lenslet array sampled the pupil plane with a 66.7 μm lenslet pitch resolution, forming over 5600 wavefront sensing spots for a 5 mm pupil. An artificial pupil (AP) was placed in the pupil plane and imaged onto the IOL surface using the two relay optics (L2 and L3). A pupil camera imaged the artificial pupil, the alignment reference, and an IOL in the wet cell simultaneously and was used to accurately determine the pupil diameter and axial position of an IOL. The IOL was submerged in a wet cell, with the front and back surfaces of the latter covered by flat optical windows. An artificial cornea was not included in the system. The IOL was mounted onto a stage with three axis translation and tip/tilt adjustment, allowing for more accurate alignment within the wet cell. To quantify the image quality of the IOLs, we captured through-focus images of a 1951 United States Air Force resolution target (Edmund Optics; Barrington, New Jersey, USA). The resolution target was back-illuminated with an incoherent white-light source, representative of natural viewing conditions. This target was placed in a plane conjugate to the IOL image plane (retinal plane), followed by relay onto a charge-coupled device (CCD) sensor with 2× magnification to improve sampling resolution. The 20/20 and 20/40 Snellen Acuity letter sizes corresponded approximately to group 2/element 2, and group 1/element 2 of the resolution target, respectively (Figure 1 B). Near vision was simulated by using trial lenses in front of the wet cell to change the object vergence at the IOL. Simulated object distances ranged from −1.0D (beyond infinity) to +5.0 D (near vision), in 0.5 D increments.
Figure 1.
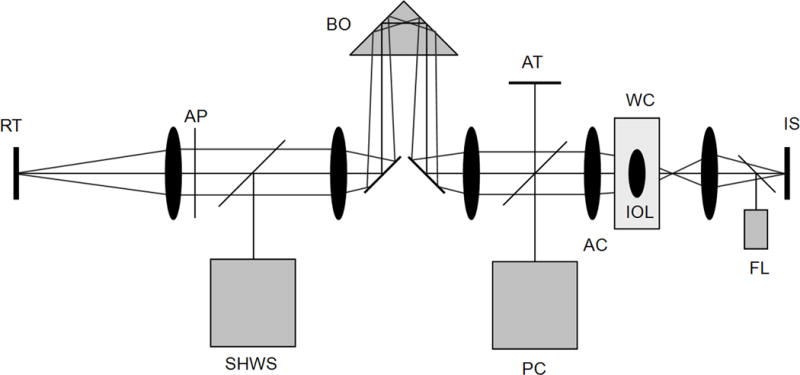
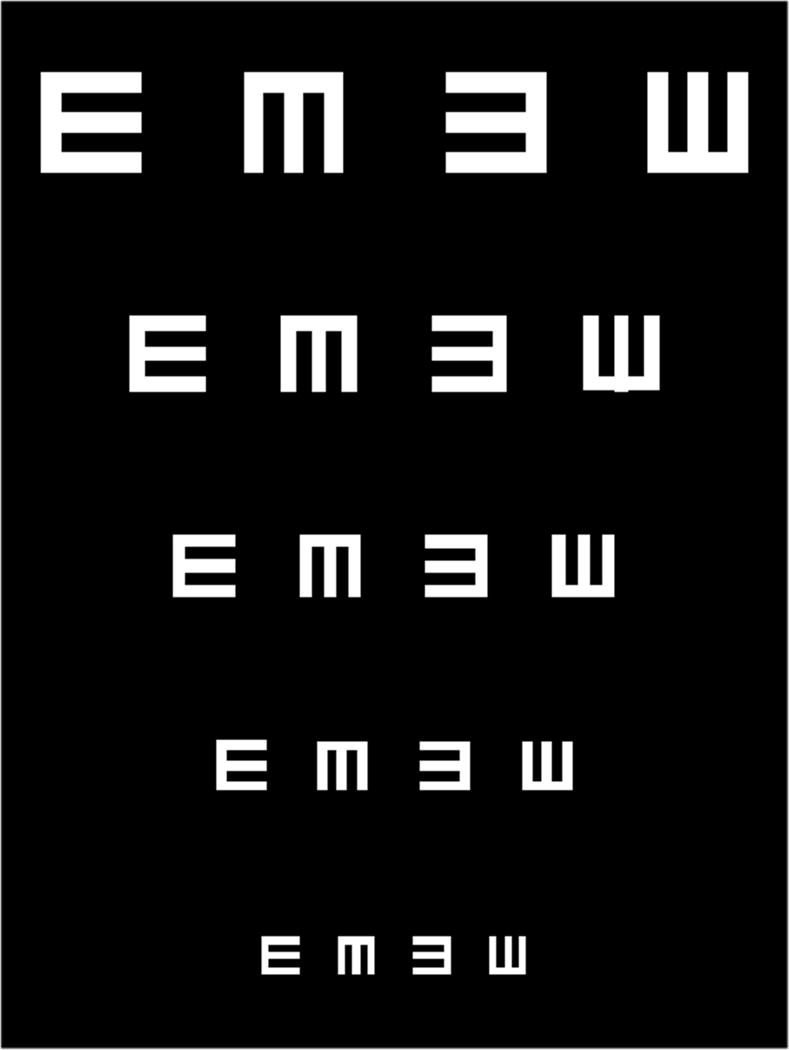
A: Diagram of an optical bench (FL: fiber laser, AFRT: air force resolution target, L1: lens 1, L2: lens 2, L3: lens 3, AP: artificial pupil, PC: pupil camera, AT: alignment target, TL: trial lens, WC: wet cell, IOL: intraocular lens, WS: wavefront sensor, IS: image sensor). B: Cropped image of a 1951 United States Air Force resolution target.
Data Analysis
Wavefront sensor data were analyzed using custom-developed software that computed Zernike coefficients up to the tenth order including primary (fourth) and higher (sixth, eighth and tenth) order spherical aberrations. These aberrations were analyzed for pupil sizes of 5, 4, and 3 mm, except for the HD500 IOL, for which 4.8, 4 and 3 mm were used. All Zernike coefficients were based on Optical Society of America (OSA) standards.18
To quantify through-focus image quality of the resolution target through different IOLs, we computed their cross-correlation coefficients (CCs), which quantify the likenesses of captured images and the perfect reference image. Each CC ranged from −1 to +1, where +1 corresponds to perfect image quality and CC<1 corresponds to poorer image quality than the reference image (due to, for example, aberrations and scattering). The captured target images were cropped to include only groups 1 and 2, and registered prior to the CC calculations. CCs were calculated using MATLAB software (version R2009a, MathWorks; Natick, Massachusetts, USA). The distance (0 D) image was chosen to maximize CC of an image for a 3 mm pupil and defocus points for the rest of the images were shifted accordingly.
RESULTS
Spherical Aberration Analysis
Figure 2 summarizes the primary spherical aberrations of the IOLs for three pupil diameters of 3, 4 and 5 mm. As expected, the aberration-free IOL, LI60AOV, showed minimal (<0.02 μm) spherical aberrations for all pupil sizes. SN60AT, which has a spherical monofocal optic, had a positive spherical aberration of 0.18 μm for a 5 mm pupil, which became negligibly small (< 0.02 μm) for a 3 mm pupil.
Figure 2.
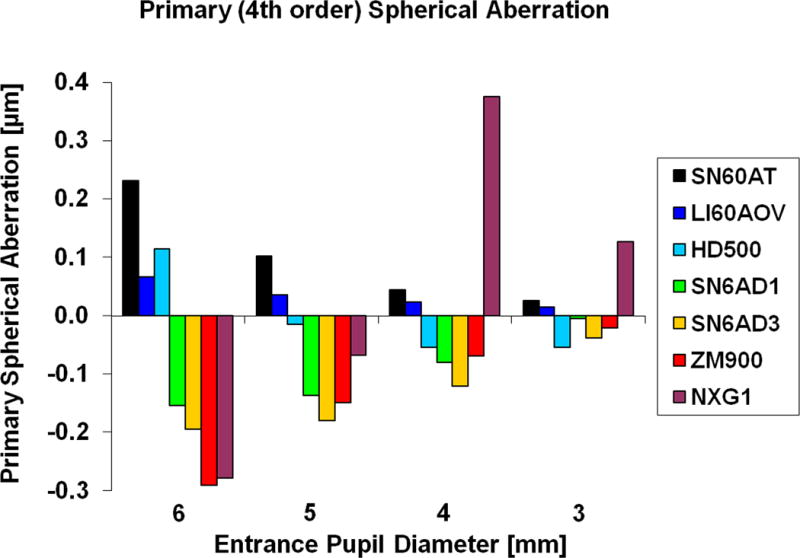
Change in primary spherical aberration as a function of pupil size.
All the multifocal IOLs had negative spherical aberrations of different magnitudes for 5 mm pupils. The measured spherical aberrations of the SN6AD3, SA6AD1, NXG1 and ZM900 IOLs were −0.27 μm, −0.24 μm, −0.35 μm and −0.33 μm, respectively. Similar to SN60AT, the spherical aberrations of the multifocal IOLs decreased as pupil diameter decreased. For 3 mm pupils, the spherical aberrations were negative, but their magnitudes were relatively small (≤ 0.1 μm). The spherical aberration of NXG1, which was −0.35 μm for a 5 mm pupil, became +0.28 μm for a 3 mm pupil.
An accommodating IOL, HD500, had a positive spherical aberration of +0.12 μm for a 5 mm pupil, decreasing to <0.05 μm for smaller pupils of 4 and 3 mm, becoming negative for the latter.
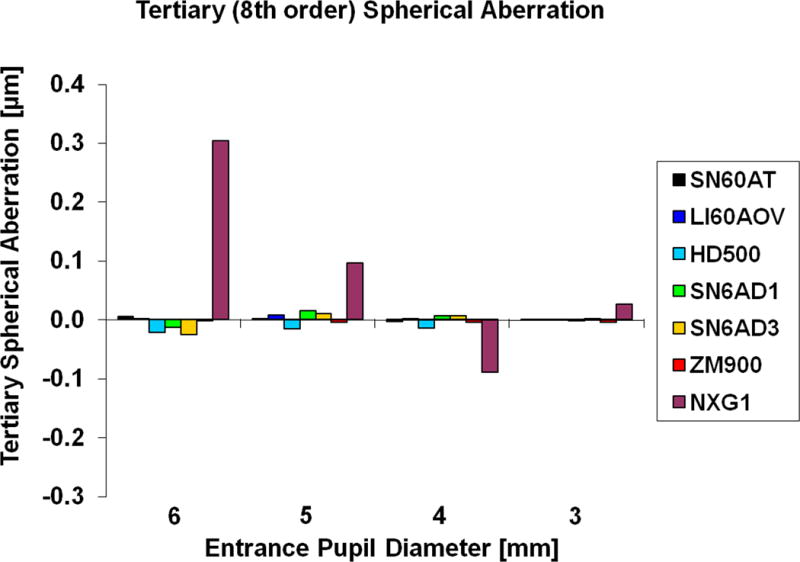
The magnitudes of higher order spherical aberrations (sixth, eighth, and tenth) for a 5 mm pupil were <0.05 μm in all the IOLs except for HD500 and NXG1. HD500 had the sixth spherical aberration of +0.07 μm for a 4.8 mm pupil. The eighth and tenth order spherical aberrations for NXG1 were +0.22 μm and −0.18 μm, respectively.
Through-Focus Images
Figure 3 illustrates through-focus images of the resolution target for a 3 mm pupil. We chose 3 mm because most elderly cataract patients have relatively small pupils with miosis for near vision. Although the two monofocal IOLs had superior image quality at an object distance of 0 D, substantial degradation of image quality was observed when even relatively small amounts of defocus were induced.
Figure 3.
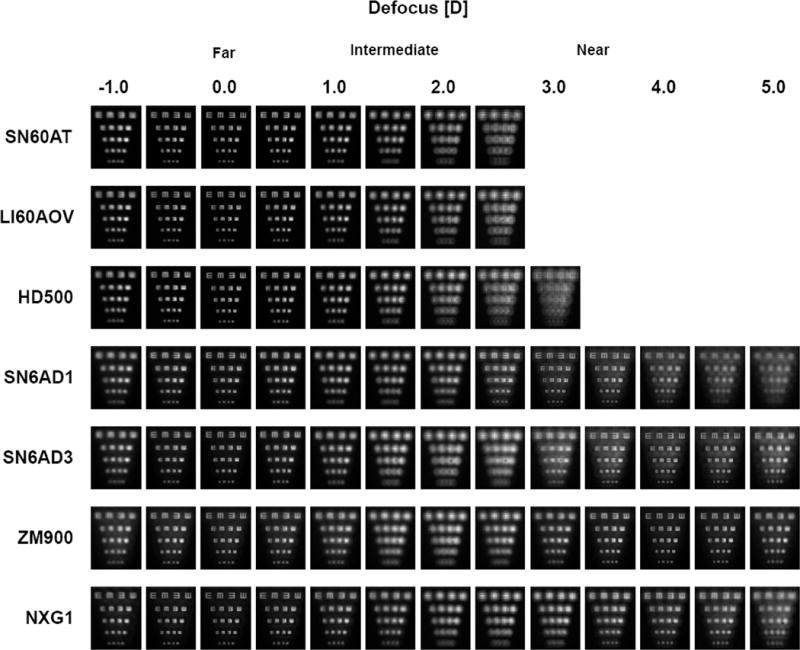
Through-focus images for a 3 mm pupil.
All premium IOLs showed an increase in depth of focus compared with the monofocal lenses. As predicted, the multifocal IOLs showed a compromise of distance image quality, but significant improvements in image quality at near object distances (3~4 D).
Peak near image quality for the SN6AD3, SA6AD1, NXG1 and ZM900 lenses was observed at 4.0 D, 3.0 D, 3.5 D and 4.0 D, respectively. The depth of focus of the HD500 was higher than that of the monofocal IOLs, but substantially smaller than that with the multifocal IOLs. The intermediate image quality of the multifocal IOLs was significantly degraded by enhancing near image quality.
Through-focus image quality quantified from the captured resolution target images using CC showed the same trends. At 0 D defocus and for a 3 mm pupil, the CCs of the LI60AOV and SN60AT monofocal IOLs were 0.77 and 0.75, respectively. Distance CCs for multifocal IOLs ranged from 0.61 to 0.74, and was lowest for NXG1, with a range of decrease from 3.9% to 20.8% when compared with the LI60AOV. The CC of HD500 was 0.72, 6.5% lower than that of LI60AOV. At 1 D defocus, the CC for all pupils was highest with HD500. The peak levels for near objects with a 3 mm pupil ranged from 0.57 to 0.70. For all IOLs tested, the trends were consistent for 3, 4 and 5 mm pupils although overall image quality decreased with an increase in the pupil size.
DISCUSSION
We have evaluated the optical characteristics of several premium IOLs using an optical bench, which enables quantification of spherical aberration profiles and changes in image quality with different amounts of defocus, simulating distant, intermediate, and near objects.
Many methods have been used to assess the image quality of IOLs.13–15, 19 Optical bench systems with resolution targets remain the most common way to evaluate current IOL technologies. The International Organization for Standardization (ISO) 11979-2 specifies the use of a model eye, including an aberration-free model cornea, so that any aberrations and their impact on image quality will be from the IOL itself.20 Since we measured optical aberrations and the through-focus imaging capability inherent to the IOL, and objectively compared them among IOLs, we did not include an artificial cornea in the system.
Following the introduction of multifocal IOLs in the 1980s, reduced image contrast and unwanted visual phenomena have been reported.21–25 In agreement with these reports, we observed contrast degradation in the multifocal IOLs we tested. We assessed the relative contributions of spherical aberration and multifocality on blurring of the image. A small pupil diameter (3 mm), with negligible spherical aberration, still had a significant amount of blur, indicating that the major factor causing contrast degradation and image blur is the multifocal nature of the IOLs.
In the past few years, IOLs with varying amounts of negative spherical aberration have become available.26 Such IOLs are designed to counteract positive corneal spherical aberrations.27 To enhance distance contrast sensitivity, aspheric optic designs were applied to both multifocal and monofocal IOLs. All the multifocal IOLs tested had negative spherical aberrations, −0.27 μm, −0.24 μm, −0.33 μm, and −0.35 μm for the SA6AD3, SA6AD1, ZM900, and NXG1, respectively, and a 5 mm pupil. The average anterior corneal spherical aberration for a 6-mm aperture diameter at the cornea has been reported to be +0.27 μm.27 Clinical studies have demonstrated that such aspheric IOLs resulted in better contrast sensitivity.28–30 Because of the large optical power of the cornea, a physical size of 5.2 mm on the iris aperture appears as 6 mm on the corneal surface.31 As IOLs are positioned behind the iris, a 6 mm diameter at the cornea would be compatible with an IOL plane <5.2 mm in diameter, indicating that multifocal IOLs compensate for most of the positive spherical aberration of the cornea. Multifocal IOLs would therefore significantly reduce the spherical aberration of eyes, which may enhance the image contrast. In contrast, correcting spherical aberrations in presbyopia is of great interest, since spherical aberrations32 as well as other higher order aberrations can increase depth of focus. Pupil size should also be considered, since, as shown here, the magnitude of spherical aberration is strongly dependent on pupil size.
The ability of a Shack-Hartmann type wavefront sensor to measure diffractive multifocal IOLs may be limited due to the split of lenslet spots caused by more than one diffractive zone within the same lenslet (“lenslet splitting”).33 Although our custom-developed wavefront sensor was designed to minimize this error by sampling a wavefront at a high lateral resolution, this limitation was not completely ruled out and some local wavefront slopes may have been estimated inaccurately.
Spherical aberrations, especially primary spherical aberrations (i.e. fourth order), were the main contributor to higher order aberration since the IOLs tested in this study were designed with radially symmetrical optics. HD500, which showed enhanced depth of focus, had significant amounts of secondary spherical aberration (sixth order), suggesting that secondary spherical aberrations may play a role in extending depth of focus. However, the role of secondary spherical aberrations in enhancing depth of focus has not yet been determined. A refractive multifocal IOL, NXG1, showed large changes in spherical aberration as pupil size changed. Furthermore, this lens had large amounts of higher order spherical aberrations (eighth and tenth orders). These findings may be due to the optic design of this multifocal IOL, which is characterized by alternating distance and near refractive zones along with intermediate transitional zones.
A greater understanding of the optical performance of multifocal IOLs requires an evaluation of through-focus image quality. The ability to quantify image quality is also desirable. Despite other image quality metrics available, such as the Strehl ratio and modulation transfer function, we assessed cross-correlation coefficients calculated from the captured images through various IOLs. This technique was originally derived from digital image correlations, which employ tracking and image registration techniques to measure deformations of digital images.34–35 One advantage of this metric is its use of a single value metric that can be easily correlated with subjective image quality. While this metric needs to be fully tested to demonstrate its reliability in representing visual performance such as visual acuity and contrast sensitivity, we found that it well represented subjectively observed through-focus image quality.
In multifocal IOLs, out-of-focus images are superimposed with in-focus images on the retina simultaneously and cause background glare resulting in the reduction in image contrast as shown in Figure 3. It is interesting to note that the amount of the background glare of ZM900 does not vary with defocus, although SN6AD3 and SA6AD1 showed a significant increase in the background glare with defocus. This may be due to the difference in energy distribution between distant and near objects. The latter two IOL have apodized diffractive optics, delivering more light energy for distant objects than near objects at pupil sizes > 2 mm. In contrast, the ZM900, which has a full-aperture diffractive optic, splits light energy equally for distant and near objects for all pupil sizes. Therefore, SA6AD1 and SN6AD3 show relatively lower background glare that ZM900 for distant image quality. In quantifying image quality using CC, LI60AOV was better than SN60AT (0.77 versus 0.75) due to the positive spherical aberration noted with the SN60AT. Monofocal IOLs were superior to multifocal IOLs (CC range, 0.69 to 0.74) because of compromise of distance image quality of the latter. A new image quality metric based on CC calculated from a captured image allows for quantifying through-focus image quality easily shown in Figure 4. All multifocal IOLs showed a bimodal trend in through-focus image quality (Figures 3 and 4), with two peaks of image quality for distant (0 D) and near (3–4 D) objects, along with the significant degradation of intermediate (1.5–2.0 D) image quality. HD500, an accommodating IOL, had a similar pattern in through-focus image quality to that of the monofocal IOLs with a high distance quality and a relatively narrow depth of focus. However, because of its bispheric optical design, the HD500 had an approximately 1.5 D increase in depth of focus compared with monofocal IOLs. Poor near vision is expected with this IOL unless it moves forward axially, along with accommodative efforts. Intermediate performance may be further improved by refining the bispheric design, for example by increasing its additive power.
Figure 4.
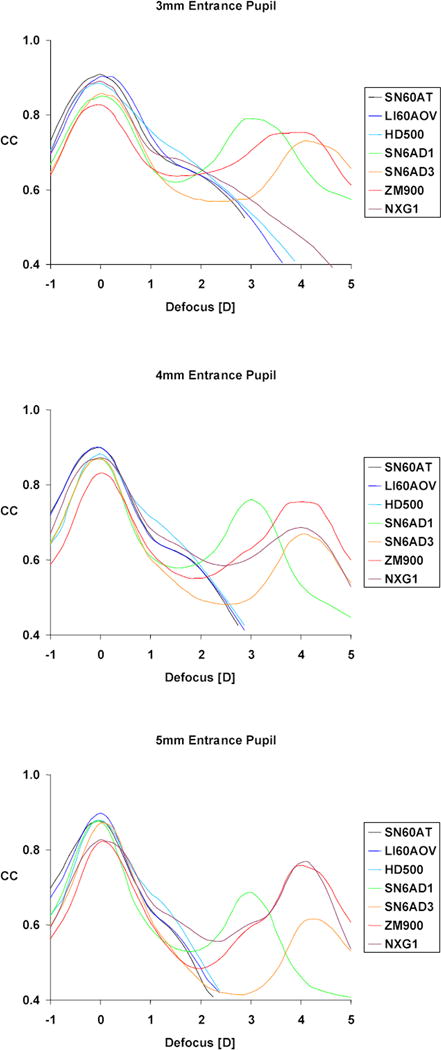
Cross-correlation coefficients for a 3 mm pupil.
In summary, we found that the optical characteristics of premium IOLs could be accurately determined using an optical bench system, which can objectively assess through-focus image quality. Information from optical bench systems will not only enhance the ability to predict and explain clinical outcomes after IOL implantation but may allow clinicians to choose an optimal IOL for individual patients based on their corneal spherical aberration and expectation.
Acknowledgments
Supported in part by RPB, NIH grant (EY014999), NYSTAR/Bausch & Lomb grant.
Footnotes
Presented in part at the ASCRS Symposium on Cataract, IOL and Refractive Surgery, Boston, Massachusetts, USA, April, 2010.
Financial Disclosure: No author has a financial or proprietary interest in any material or method mentioned.
References
- 1.Glasser A, Campbell MC. Presbyopia and the optical changes in the human crystalline lens with age. Vision Res. 1998;38:209–29. doi: 10.1016/s0042-6989(97)00102-8. [DOI] [PubMed] [Google Scholar]
- 2.McDonnell PJ, Lee P, Spritzer K, Lindblad AS, Hays RD. Associations of presbyopia with vision-targeted health-related quality of life. Arch Ophthalmol. 2003;121:1577–1581. doi: 10.1001/archopht.121.11.1577. [DOI] [PubMed] [Google Scholar]
- 3.Menapace R, Findl O, Kriechbaum K, Leydolt-Koeppl Ch. Accommodating intraocular lenses: a critical review of present and future concepts. Graefes Arch Clin Exp Ophthalmol. 2007;245:473–489. doi: 10.1007/s00417-006-0391-6. [DOI] [PubMed] [Google Scholar]
- 4.Pepose JS. Maximizing satisfaction with presbyopia-correcting intraocular lenses: the missing links. Am J Ophthalmol. 2008;146:641–648. doi: 10.1016/j.ajo.2008.07.033. [DOI] [PubMed] [Google Scholar]
- 5.Buznego C, Trattler WB. Presbyopia-correcting intraocular lenses. Curr Opin Ophthalmol. 2009;20:13–18. doi: 10.1097/ICU.0b013e32831c4cf5. [DOI] [PubMed] [Google Scholar]
- 6.Santaella R, Afshari N. Presbyopia-correcting intraocular lenses: ‘one lens does not fit all’. Curr Opin Ophthalmol. 2010;21:1–3. doi: 10.1097/ICU.0b013e3283340dce. [DOI] [PubMed] [Google Scholar]
- 7.Packer M, Chu YR, Waltz KL, Donnenfeld ED, Wallace RB, 3rd, Featherstone K, Smith P, Bentow SS, Tarantino N. Evaluation of the aspheric tecnis multifocal intraocular lens: one-year results from the first cohort of the food and drug administration clinical trial. Am J Ophthalmol. 2010;149:577–584. doi: 10.1016/j.ajo.2009.10.022. [DOI] [PubMed] [Google Scholar]
- 8.Pepose JS, Qazi MA, Davies J, Doane JF, Loden JC, Sivalingham V, Mahmoud AM. Visual performance of patients with bilateral vs combination Crystalens, ReZoom, and ReSTOR intraocular lens implants. Am J Ophthalmol. 2007;144:347–357. doi: 10.1016/j.ajo.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 9.Vingolo EM, Grenga P, Iacobelli L, Grenga R. Visual acuity and contrast sensitivity: AcrySof ReSTOR apodized diffractive versus AcrySof SA60AT monofocal intraocular lenses. J Cataract Refract Surg. 2007;33:1244–1247. doi: 10.1016/j.jcrs.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 10.Ortiz D, Alió JL, Bernabéu G, Pongo V. Optical performance of monofocal and multifocal intraocular lenses in the human eye. J Cataract Refract Surg. 2008;34:755–762. doi: 10.1016/j.jcrs.2007.12.038. [DOI] [PubMed] [Google Scholar]
- 11.Castillo-Gómez A, Carmona-González D, Martínez-de-la-Casa JM, Palomino-Bautista C, García-Feijoo J. Evaluation of image quality after implantation of 2 diffractive multifocal intraocular lens models. J Cataract Refract Surg. 2009;35:1244–1250. doi: 10.1016/j.jcrs.2009.02.024. [DOI] [PubMed] [Google Scholar]
- 12.Martínez Palmer A, Gómez Faiña P, España Albelda A, Comas Serrano M, Nahra Saad D, Castilla Céspedes M. Visual function with bilateral implantation of monofocal and multifocal intraocular lenses: a prospective, randomized, controlled clinical trial. J Refract Surg. 2008;24:257–264. doi: 10.3928/1081597X-20080301-07. [DOI] [PubMed] [Google Scholar]
- 13.Terwee T, Weeber H, van der Mooren M, Piers P. Visualization of the retinal image in an eye model with spherical and aspheric, diffractive, and refractive multifocal intraocular lenses. J Refract Surg. 2008;24:223–232. doi: 10.3928/1081597X-20080301-03. [DOI] [PubMed] [Google Scholar]
- 14.Maxwell WA, Lane SS, Zhou F. Performance of presbyopia-correcting intraocular lenses in distance optical bench tests. J Cataract Refract Surg. 2009;35:166–171. doi: 10.1016/j.jcrs.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 15.Choi J, Schwiegerling J. Optical performance measurement and night driving simulation of ReSTOR, ReZoom, and Tecnis multifocal intraocular lenses in a model eye. J Refract Surg. 2008;24:218–222. doi: 10.3928/1081597X-20080301-02. [DOI] [PubMed] [Google Scholar]
- 16.Maxwell WA, Cionni RJ, Lehmann RP, Modi SS. Functional outcomes after bilateral implantation of apodized diffractive aspheric acrylic intraocular lenses with a +3.0 or +4.0 diopter addition power Randomized multicenter clinical study. J Cataract Refract Surg. 2009;35:2054–2061. doi: 10.1016/j.jcrs.2009.06.041. [DOI] [PubMed] [Google Scholar]
- 17.Weinstock R, Desai NR. Microincisional cataract surgery in the era of refractive cataract surgery. In: Argawal A, Lindstrom R, editors. Microincisional Cataract Surgery: The Art and Science. Thorofare, NJ: Slack, Inc; 2010. pp. 173–181. [Google Scholar]
- 18.Thibos LN, Applegate RA, Schwiegerling JT, Webb R, VSIA Standards Taskforce Members Vision science and its applications. Standards for reporting the optical aberrations of eyes. J Refract Surg. 2002;18:S652–60. doi: 10.3928/1081-597X-20020901-30. [DOI] [PubMed] [Google Scholar]
- 19.Tognetto D, Sanguinetti G, Sirotti P, Cecchini P, Marcucci L, Ballone E, Ravalico G. Analysis of the optical quality of intraocular lenses. Invest Ophthalmol Vis Sci. 2004;45:2682–2690. doi: 10.1167/iovs.03-1024. [DOI] [PubMed] [Google Scholar]
- 20.International Organization for Standardization. Ophthalmic Implants – Intraocular Lenses – Part 2: optical Properties and Test Methods. Geneva, Switzerland: ISO; 1999. pp. 1–27. (ISO 11979-2). [Google Scholar]
- 21.Montés-Micó R, Alió JL. Distance and near contrast sensitivity function after multifocal intraocular lens implantation. J Cataract Refract Surg. 2003;29:703–711. doi: 10.1016/s0886-3350(02)01648-6. [DOI] [PubMed] [Google Scholar]
- 22.Gimbel HV, Sanders DR, Raanan MG. Visual and refractive results of multifocal intraocular lenses. Ophthalmology. 1991;98:881–887. doi: 10.1016/s0161-6420(91)32205-x. [DOI] [PubMed] [Google Scholar]
- 23.Jay JL, Chakrabarti HS, Morrison JD. Quality of vision through diffractive bifocal intraocular lenses. Br J Ophthalmol. 1991;75:359–366. doi: 10.1136/bjo.75.6.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pieh S, Weghaupt H, Skorpik C. Contrast sensitivity and glare disability with diffractive and refractive multifocal intraocular lenses. J Cataract Refract Surg. 1998;24:659–662. doi: 10.1016/s0886-3350(98)80261-7. [DOI] [PubMed] [Google Scholar]
- 25.Schmitz S, Dick HB, Krummenauer F, Schwenn O, Krist R. Contrast sensitivity and glare disability by halogen light after monofocal and multifocal lens implantation. Br J Ophthalmol. 2000;84:1109–1112. doi: 10.1136/bjo.84.10.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pieh S, Fiala W, Malz A, Stork W. In vitro strehl ratios with spherical, aberration-free, average, and customized spherical aberration-correcting intraocular lenses. Invest Ophthalmol Vis Sci. 2009;50:1264–1270. doi: 10.1167/iovs.08-2187. [DOI] [PubMed] [Google Scholar]
- 27.Holladay JT, Piers PA, Koranyi G, van der Mooren M, Norrby NE. A new intraocular lens design to reduce spherical aberration of pseudophakic eyes. J Refract Surg. 2002;18:683–691. doi: 10.3928/1081-597X-20021101-04. [DOI] [PubMed] [Google Scholar]
- 28.Bellucci R, Scialdone A, Buratto L, Morselli S, Chierego C, Criscuoli A, Moretti G, Piers P. Visual acuity and contrast sensitivity comparison between Tecnis and AcrySof SA60AT intraocular lenses: A multicenter randomized study. J Cataract Refract Surg. 2005;31:712–717. doi: 10.1016/j.jcrs.2004.08.049. [DOI] [PubMed] [Google Scholar]
- 29.Muñoz G, Albarrán-Diego C, Montés-Micó R, Rodríguez-Galietero A, Alió JL. Spherical aberration and contrast sensitivity after cataract surgery with the Tecnis Z9000 intraocular lens. J Cataract Refract Surg. 2006;32:1320–1327. doi: 10.1016/j.jcrs.2006.02.055. [DOI] [PubMed] [Google Scholar]
- 30.Rocha KM, Soriano ES, Chalita MR, Yamada AC, Bottós K, Bottós J, Morimoto L, Nosé W. Wavefront analysis and contrast sensitivity of aspheric and spherical intraocular lenses: a randomized prospective study. Am J Ophthalmol. 2006;142:750–756. doi: 10.1016/j.ajo.2006.06.031. [DOI] [PubMed] [Google Scholar]
- 31.Waltz KL, Rubin ML. Capsulorhexis and corneal magnification. Arch Ophthalmol. 1992;110:170. doi: 10.1001/archopht.1992.01080140020007. [DOI] [PubMed] [Google Scholar]
- 32.Rocha KM, Soriano ES, Chamon W, Chalita MR, Nosé W. Spherical aberration and depth of focus in eyes implanted with aspheric and spherical intraocular lenses: a prospective randomized study. Ophthalmology. 2007;114:2050–2054. doi: 10.1016/j.ophtha.2007.01.024. [DOI] [PubMed] [Google Scholar]
- 33.Gatinel D. Limited accuracy of Hartmann-Shack wavefront sensing in eyes with diffractive multifocal IOLs. J Cataract Refract Surg. 2008;34:528. doi: 10.1016/j.jcrs.2007.11.038. [DOI] [PubMed] [Google Scholar]
- 34.Peters WH, Ranson WF. Digital imaging techniques in experimental stress analysis. Opt Eng. 1982;21:427–431. [Google Scholar]
- 35.Sutton MA, McNeill SR, Helm SD, Chao YJ. Advances in two-dimensional and three-dimensional computer vision. In: Rastogi PK, editor. Photomechanics. Springer; 2000. pp. 323–372. [Google Scholar]


