Abstract
Pulmonary alveolar microlithiasis (PAM) is a rare chronic lung disease characterized by deposition of intra alveolar calcium and phosphate in bilateral lung parenchyma with predominance in lower and mid zones. Etiology and pathogenesis is not fully understood. However, mutation in SLC34A2 gene that encodes a sodium phosphate co-transporter in alveolar type-II cells resulting in formation and accumulation of microliths rich in calcium phosphate due to impaired clearance is considered the cause of disease. Patients with PAM are asymptomatic till development of hypoxemia and cor pulmonale. It remains static, while in some it progresses to pulmonary fibrosis, respiratory failure and cor pulmonale. We report a case of 44 year old male patient presenting with progressive shortness of breath on exertion for one year in duration with dry cough, more since last six months. Chest radiograph showed dense micronodular opacities giving classical sandstorm appearance. High resolution computed tomography (HRCT) showed microcalcification, subpleural cystic changes and calcified pleura. Lung biopsy showed calcospherites within alveolar spaces.
Keywords: Pulmonary Alveolar microlithiasis, HRCT, Type-II sodium dependent phosphate co-transporter, calcospherites, microliths and micronodular opacities
CASE REPORT
A forty-four-year male presented with progressive shortness of breath on exertion for one year duration with dry cough, more since last six months. There was no history of smoking or previous known pulmonary disease. He was tailor by occupation. There was no clubbing or cyanosis or peripheral edema on clinical examination. On chest auscultation, it revealed course crackles and random wheezes. Cardiac auscultation was normal. Blood counts and serum biochemistry were normal. Echocardiography and pulmonary function tests showed no significant abnormality. Sputum was negative for Acid fast bacilli (AFB). Human immunodeficiency virus (HIV) test was negative. As a diagnostic workup chest radiograph posteroanterior view showed diffuse dense bilateral micronodular opacities (sandstorm appearance) obscuring the cardiac and diaphragmatic silhouette. There was no pleural effusion (Figure 1A, 1B). HRCT at lung window (window level −600, window width 1600) revealed bilateral diffuse intra-alveolar as well as interlobular septal calcifications with calcification of pleura (Figure 2A–2F). Transbronchial bronchoalveolar lavage (BAL) and lung biopsy were performed. The lavage fluid was negative for both AFB and fungi. Lung biopsy showed intra-alveolar laminated calcospherites diagnostic of PAM (Figure 3). Patient was given symptomatic treatment for dry cough and breathlessness and was referred to tertiary care centre for lung transplantation.
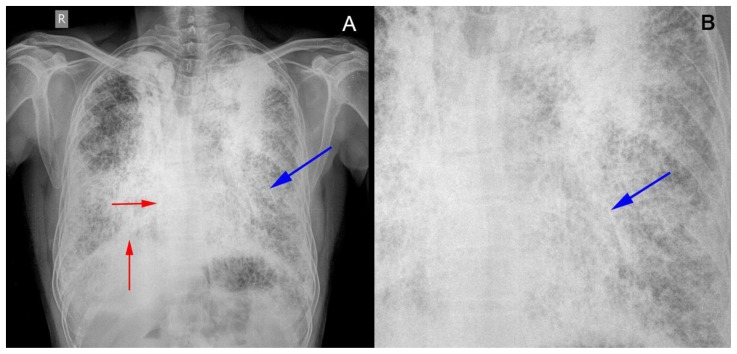
Figure 1.
A 44 year old male with pulmonary alveolar microlithiasis.
Technique: Frontal (posterior to anterior technique) chest radiograph.
Findings: (A) Frontal view showing diffuse dense bilateral micronodular opacities (sandstorm appearance) (blue arrow) obscuring the cardiac and diaphragmatic silhouette (red arrow), more in mid and lower zones. There is no pleural effusion. There is no mediastinal or hilar lymphadenopathy. (B) Magnified view of frontal view (A) confirming the presence of micronodular opacities (sandstorm appearance) (blue arrow) obscuring cardiac silhouette.
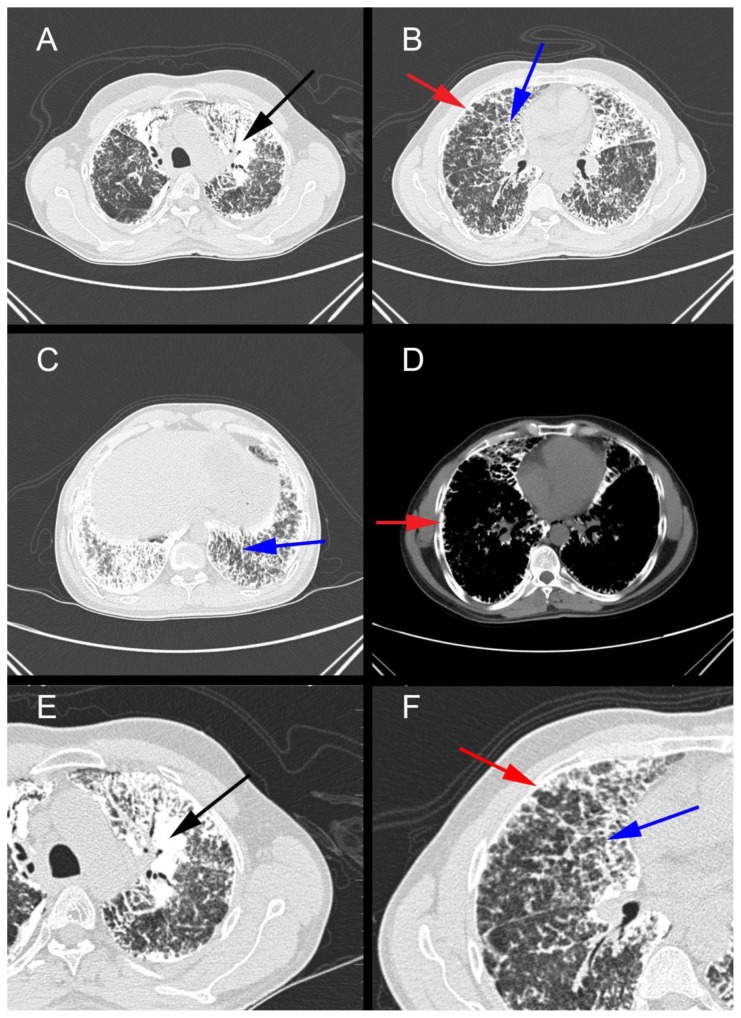
Figure 2.
A 44 year old male presenting with progressive breathlessness and dry cough subsequently diagnosed as pulmonary alveolar microlithiasis.
Findings: Axial HRCT thorax at lung window (figures A, B and C) and mediastinal window (Figure D) showing bilateral diffuse intra alveolar (black arrow), as well as interlobular septal calcifications (blue arrow), with calcification of pleura (red arrow). There is no pleural or pericardial effusion, no hilar lymphadenopathy or cardiomegaly. (E) And (F) shows magnified views of axial HRCT thorax at lung window (A) and (B) respectively confirming intra alveolar (black arrow) and interlobular septal calcification (blue arrow) with calcification of pleura (red arrow).
Technique: Axial CT images from a 128 slice CT scanner with lung windows figures 2A, B and C (−600 window level and 1600 window width), 120 KVp, exposure time 1279ms, 110 mA, slice thickness 1 mm, non-contrast, 1 mm thickness at 10 mm interval in axial mode. Figure 2D - mediastinal window (60 window level and 400 window width), 120 KVp, exposure time 1279ms, 110 mA, slice thickness 5 mm at 5 mm interval in axial mode, non-contrast.
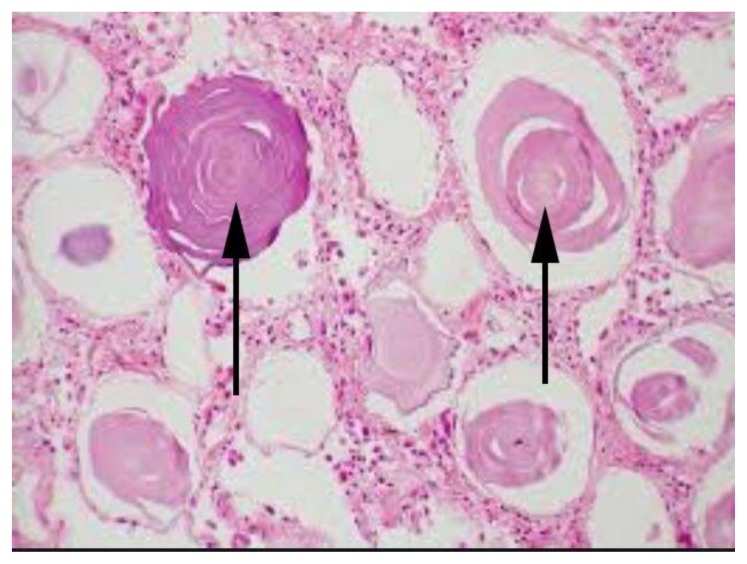
Figure 3.
A 44 year old male presenting with progressive breathlessness and dry cough subsequently diagnosed as pulmonary alveolar microlithiasis.
Findings (Hematoxylin-eosin stain sections): shows multiple laminated calcospherites (black arrow) within the alveoli of lung parenchyma suggestive of PAM of lung (100x).
DISCUSSION
Demographics
Pulmonary Alveolar microlithiasis is a rare chronic disease of lungs characterized by presence of innumerable diffuse minute calculi called microliths/calcospherites in the alveoli of lungs. PAM was first reported by Norwegian Harbitz in 1918, also called Harbitz syndrome [1]. It was named PAM by Puhr of Hungary in 1933 [2]. In medical literature, less than 800 cases have been reported worldwide to date without any particular race or geographic predominance. Most cases have been reported from Turkey, Japan and Italy. Asia and Europe share nearly one-third cases each. PAM is seen in all age groups and is frequently diagnosed from birth to 40 years of age [3]. The youngest reported cases were premature twins and two newborn, while the most elderly was of 80years of age [4]. Sporadic and familial cases are reported. Familial cases account for nearly 30–50% of reported cases. No sex predilection was seen. Male predominance was reported in sporadic cases. Both sexes are affected with equal frequency in familial cases [5]. Most of the cases are coming from Europe (42.7%) and Asia (40.6%).
Etiology & Pathogenesis
PAM is a rare disease with poorly defined etiology and pathogenesis, characterized by numerous microcalculi (microliths, calcospherites, and denominated calciferites) with air spaces [6]. It appears to be due to autosomal recessive inheritance due to mutations of SLC34A2 gene, which encodes a Type-IIb sodium dependent phosphate Co-transporter (NaPi-IIb). SLC34A2 is primarily expressed in lung in alveolar type II cells. These cells are responsible for production of surfactant. Loss of function of gene due to mutation lead to decreased cell uptake of phosphate which lead to formation of intra-alveolar microliths as a result of phosphate chelating calcium in extracellular fluid [5]. Both horizontal accumulation of patients in a family and presence of consanguineous marriages in parents are suggestive of PAM as an autosomal recessive disease with high penetrance. Inborn errors of metabolism are also suggested due to high incidence within families [3].
The composition of calcospherites is calcium and phosphate in the ratio of 2:1. Microliths are spherical-ovoid shaped with concentric laminated appearance [7]. Their size varies from 0.01 to 3mm within the alveoli. In early stages, alveolar cells are normal. With disease progression, interstitial thickening and giant cells are seen with resultant fibrosis. Apical blebs and bullae may cause recurrent pneumothorax.
Pathology
Lung histology shows intra-alveolar calcospherites and fibrosis of alveolar wall. Lung biopsy shows characteristic intra-alveolar lamellar microliths. In advanced cases, microliths are seen in interlobular septa, bronchovascular bundles and subpleural space where fibrosis and ossification are often observed [3].
Clinical Findings
Information of initial phase, evolution and stabilization of PAM is less available. The disease is detected from birth up to 40 years of age and is usually detected on chest radiographs for other reasons. Many patients are asymptomatic and either have normal pulmonary function or mild restrictive pattern. Symptomatic patients have dyspnoea and nonproductive cough. In some cases, both symptoms and radiological findings remains static, while in some other cases it worsens at different rates leading to pulmonary fibrosis, respiratory failure and cor pulmonale [2]. Cough may occur at any stage of the disease with expectoration of microliths at times. As disease progresses, breathlessness on exertion occurs with symptoms of cor pulmonale as terminal manifestation which may lead to death.
Elevated serum concentration of surfactant protein (SP)-A and (SP)-D is usually seen in PAM, whose levels increase as disease progresses (normal serum SP-A level is 24.9 + 9.6 ng/ml; normal serum SP-D level is 48.7 ng/ml). Hence, (SP)-A and (SP)-D is serum markers in monitoring disease activity and disease progression [2].
Imaging Findings
Characteristic chest radiograph show fine sand like micronodulation of calcific densities bilaterally involving mainly middle and lower zones with sandstorm appearance. Increased calcific densities in both lower zones are due to larger surface area and greater thickness of lower part of lungs. Extensive microliths cause obscuration of mediastinal and diaphragmatic silhouette. Black pleura sign- a vertical linear radiolucency between ribs and lung parenchyma can also be seen which is secondary to subpleural cystic changes often seen on HRCT and on pathological evaluation. Apical bullae are another typical feature with an associated pneumothorax. HRCT is preferred method of evaluation of PAM as it allows detection of early structural changes of lung parenchyma which cannot be detected on radiograph and other CT technique. HRCT shows characteristic finding of innumerable microliths involving both lungs with predisposition for anterior segments of upper lobes and posterior segments of lower lobes. The medial aspects of lungs are more heavily involved than lateral aspect. Confluent areas of calcification are seen in upper lobes [8]. These findings correlate with hard calcified micronodular appearance of lung parenchyma at gross pathologic evaluation and classic concentric lamellar calcified microliths seen in alveoli and interstitium at Hematoxylin and Eosin staining. High concentration of microliths within periphery of secondary pulmonary lobule is responsible for thickening of interlobular septa and micronodulation on HRCT. Microliths are also seen along subpleural and peribronchovascular interstitium with resultant thickened micronodular appearance of these structures. Calcification of pleura is also reported. Microliths with diameter of less than 1mm produce ground glass opacities which with appropriate windowing are seen as discrete calcifications [8]. Multiple small thin walled subpleural cysts are also seen which cause dark pleural line on HRCT. Ground glass opacities with interlobular septal thickening due to microliths resemble crazy paving pattern seen in pulmonary alveolar proteinosis. Appropriate window settings visualize microcalcification which helps in differentiating between the two types.
Differential Diagnoses
Differential diagnosis of pulmonary alveolar microlithiasis includes pulmonary alveolar proteinosis, sarcoidosis, silicosis, pulmonary hemosiderosis, amyloidosis and metastatic calcification in chronic renal failure (table 2, figure 5). In pulmonary alveolar proteinosis, chest radiograph shows bilateral central and symmetrical lung opacities with relative sparing of apices and costophrenic angles. HRCT lung shows ground glass opacities, reticular or reticulo-nodular markings and crazy paving pattern. No cardiomegaly or pleural effusion will be seen. In sarcoidosis, adenopathy and parenchymal abnormality will be seen depending on stage. Parenchymal abnormality is seen in stage II to IV. Chest radiograph shows bilateral symmetric reticulo-nodular opacities in mid and lower zones in 46% cases, acinar pattern in 20% cases and end stages fibrosis in 20% cases. HRCT lung shows nodular thickening of interlobular septum, peribronchial and perivascular interstitium and subpleural interstitium. Ground glass opacities are found due to extensive interstitial sarcoid granulomas rather than alveolitis which are below resolution of HRCT. Fibrosis is found in stage IV radiating away from hila causing distortion of lung architecture. Paracicatricial emphysema is found adjacent to areas of fibrosis. Calcified lymph nodes show eggshell calcification. Silicosis has two forms- simple and complicated. Simple silicosis manifests as multiple small nodules with upper lobe predominance with calcification. Hilar and mediastinal lymph nodes may precede parenchymal nodule. Lymph nodes show eggshell calcification. Complicated silicosis manifests as large symmetric bilateral opacities of more than 1 cm diameter with irregular margins, commonly in mid zones or peripheral one third of lung which gradually migrate toward hilum leaving emphysematous lung between fibrotic tissue and pleural surface. Pulmonary hemosiderosis manifests as multiple dense nodules of size 1–5mm in mid and lower zones with tendency to coalesce. Amyloidosis has nodular and diffuse form. Nodular deposits are found in lower lobes and peripheral and subpleural areas and show multiple nodules of size 0.5–15cms with smooth lobulated contours. Calcification found in nodules in 50% cases can be central or irregular. Diffuse form of amyloidosis shows reticular markings on chest radiograph. HRCT lung show interlobular septal thickening often associated with nodular form. Metastatic calcification in chronic renal failure manifests as patchy areas of consolidation with calcium deposition usually affecting upper lobes due to high ventilation/perfusion ratio. Small calcified nodules may be unilateral or diffuse. Calcification may be seen in vessels and chest wall. HRCT lung show ground glass opacities, consolidation and cavitation [9].
Table 2.
Differential diagnosis table for pulmonary alveolar microlithiasis.
| Entity | Chest radiograph | HRCT thorax |
|---|---|---|
| Pulmonary Alveolar Microlithiasis |
|
|
| Pulmonary alveolar proteinosis |
|
|
| Sarcoidosis |
|
|
| Silicosis: 2 forms Simple and complicated (PMF) |
|
|
| Pulmonary hemosiderosis |
|
|
Amyloidosis 2 forms
|
|
|
| Metastatic calcifications in chronic renal failure |
|
|
Extrapulmonary manifestations and Co-morbidities
Extrapulmonary calcifications are reported in different cases of pulmonary alveolar microlithiasis such as medullary nephrocalcinosis, nephrolithiasis, calcification of lumbar sympathetic chain, testicles, punctuate calcifications in seminal vesicles, epididymal and periurethral calcifications causing obstructive azoospermia. As SLC34A2 gene is expressed in the other tissues, mutations in gene may result in extrapulmonary calcification [2]. Cardiac co-morbidities are also described in few cases. Co-morbidities in PAM include milk alkali syndrome, diaphyseal aclasis and autosomal recessive Waardenburg-anophthalmia syndrome.
Treatment
No effective treatment for PAM is known except for lung transplantation. Therapeutic BAL and corticosteroids are ineffective. Recurrence of disease after lung transplantation was not reported yet. Disodium acetedronate known to inhibit microcrystal growth of hydroxyl appetite used in the dose of 10mg/kg/day orally for 1 year can cause considerable regression of calcific densities in PAM because in these there is deposition of calcium embedded particles in lung interstitium which are not dislodged during BAL [3]. Long term survival of unilateral or bilateral sequential lung transplantation is yet to be proved [10].
TEACHING POINT
PAM is a rare chronic disease with poorly defined etiology which shows clinico-radiological dissociation. It is characterized by deposition of calcospherites/microliths within alveoli in bilateral lung parenchyma with predominance in lower and mid zones causing dense micro- nodular opacities with classical sandstorm appearance with black pleura sign (due to subpleural cystic changes) on chest radiograph and micro- calcification, subpleural cystic changes and calcified pleura on HRCT.
Table 1.
Summary table of pulmonary alveolar microlithiasis.
| Incidence | Rare. Less than 800 cases reported worldwide and less than 30 cases in India |
| Etiology | Autosomal recessive disease due to mutations of SLC34A2 gene leading to decreased cell uptake of phosphate with resultant formation of intra-alveolar microliths due to phosphate chelating calcium in extracellular fluid. |
| Gender Ratio | No sex predilection, male predominance in sporadic cases. |
| Age Predilection | Birth to 40 years of age. |
| Risk Factors | None |
| Treatment | Lung transplantation, therapeutic BAL and corticosteroids are ineffective. Disodium acedronate. |
| Prognosis | It remains static, while in some it progresses to pulmonary fibrosis, respiratory failure due to cor pulmonale. |
| Imaging | Multiple dense micronodular opacities in bilateral lung parenchyma with predominance in lower and mid zones giving classical sandstorm appearance and black pleura sign on chest radiograph. Multiple microliths in lungs, subpleural cystic changes, septal thickening and calcified pleura on HRCT. |
ABBREVIATIONS
- AFB
Acid Fast Bacilli
- BAL
Bronchoalveolar Lavage
- CT
Computed Tomography
- HIV
Human Immunodeficiency Virus
- HRCT
High Resolution Computed Tomography
- PAM
Pulmonary alveolar microlithiasis
REFERENCES
- 1.Harbitz E. Extensive calcification of the lungs as a distinct disease. Arch Intern Med. 1918;21:139–46. [Google Scholar]
- 2.Jönsson ÅL1, Simonsen U, Hilberg O, Bendstrup E. Pulmonary alveolar microlithiasis: two case reports and review of the literature. EurRespir Rev. 2012 Sep 1;21(125):249–56. doi: 10.1183/09059180.00009411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kashyap S1, Mohapatra PR. Pulmonary alveolar microlithiasis. Lung India. 2013 Apr;30(2):143–7. doi: 10.4103/0970-2113.110424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Castellana G, Lamorgese V. Pulmonary alveolar microlithiasis. World cases and review of the literature. Respiration. 2003;70:549–55. doi: 10.1159/000074218. [DOI] [PubMed] [Google Scholar]
- 5.Castellana G1, Gentile M, Castellana R, Fiorente P, Lamorgese V. Pulmonary alveolar microlithiasis: clinical features, evolution of the phenotype, and review of the literature. Am J Med Genet. 2002 Aug 1;111(2):220–4. doi: 10.1002/ajmg.10530. [DOI] [PubMed] [Google Scholar]
- 6.Abdalla G1, Marchiori E, Zanetti G, Mucillo A, Pereira ML, Ventura N, Martins P, Constantino CP, Canellas R, Brandão V. Varella de Oliveira RPulmonary alveolar microlithiasis: a case report with emphasis on imaging findings. Case Rep Med. 2010;2010:819242. doi: 10.1155/2010/819242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pracyk JB, Simonson SG, Young SL, Ghio AJ, Roggli VL, Piantadosi CA. Composition of lung lavage in pulmonary alveolar microlithiasis. Respiration. 1996;63:254–60. doi: 10.1159/000196556. [DOI] [PubMed] [Google Scholar]
- 8.Siddiqui NA1. Fuhrman CRBest cases from the AFIP: Pulmonary alveolar microlithiasis. Radiographics. 2011 Mar-Apr;31(2):585–90. doi: 10.1148/rg.312105157. [DOI] [PubMed] [Google Scholar]
- 9.Webb WR. Diffuse lung diseases associated with calcification. In: Webb WR, Higgins CB, editors. Thoracic imaging: Pulmonary and cardiovascular imaging. 2nd revised North American ed edition. Philadelphia, PA: Lippincott Williams and Wilkins; 2010. pp. 536–544. [Google Scholar]
- 10.Mariotta S, Ricci A, Papale M, De Clementi F, Sposato B, Guidi L, et al. Pulmonary alveolar microlithiasis: Report on 576 cases published in the literature. Sarcoidosis Vasc Diffuse Lung Dis. 2004;21:173–81. [PubMed] [Google Scholar]