Abstract
Retroperitoneal lipomatosis is a rare but distinct clinicopathological entity characterized by non encapsulated lipoma development in the retroperitoneum. Presenting complaints in the early stages are vague, and patients with retroperitoneal lipomatosis are often misdiagnosed because considerable abnormality is not detected by abdomino-pelvic sonography. However, because of the progressive nature of this lesion, most patients eventually present with varying degrees of urinary outflow obstruction and end stage renal disease, or bladder malignancies in few cases. Here we report a case of a 35-year-old Indian woman presenting with complaints of diffuse lumps in the abdomen and constipation. Based on the findings of the imaging [sonography and computed tomography (CT) scan] studies, benign retroperitoneal lipomatosis was preopreratively diagnosed and a confirmatory exploratory laprotomy was performed. Furthermore, we discuss the imaging findings obtained using various radiological modalities such as plain radiographs, intravenous urography, barium enema, sonography, CT and magnetic resonance imaging (MRI). We also discuss the etiopathogenesis, demographics, and various differential diagnoses of retroperitoneal lipomatosis.
Keywords: Lipomatosis, retroperitoneum, fat, hydronephrosis, floating bladder, hyperechoic abdomen
CASE REPORT
A 35 year old woman presented to the surgical out patient department (OPD) of our postgraduate medical college and tertiary health care center in India with complaints of gradual distention of abdomen and vague pain during the past year. Further inquiry revealed that the patient also experienced a history of constipation. The pain was diffuse and non specific. She did not complain of fever, vomiting, and urinary or menstrual problems. No significant medical history was reported. General examination revealed mild pallor. Abdominal examination revealed a generalized dull note on percussion. On palpation, the abdomen and pelvis was soft and non tender with a diffuse lumpy feel. Signs of organomegaly were absent. After clinical examination, the patient was diagnosed with the possibility of a diffuse abdominal lump or loculated ascites and was referred to the radiology department for abdomino-pelvic sonography.
Imaging Findings
Grayscale sonography of the abdomen revealed diffuse, bilateral, and hyperechoic lesion within the abdomen, which resulted in a sleeve-like encasement of the retroperitoneal organs causing their displacement (Fig 1a). These hyperechoic lesion extended to the pelvis on the right, where caused minimal displacement of the urinary bladder toward the left (Fig 1b). Solid organs of the abdomen and pelvis were normal in echotexture, without any focal lesion. Ascites was absent. Based on the sonographically equivocal findings and a clinically suspected lump the case was forwarded for senior review. Considering the retroperitoneal location and the hyperechoic nature of the lesion, a possible diffuse retroperitoneal fat containing lesion was proposed and the patient was advised a contrast-enhanced CT (CECT) scan of the abdomen and pelvis for confirmation. Further imaging with CECT (abdomen + pelvis) was performed using positive oral contrast technique. CECT demonstrated ill-defined, non capsulated, and non enhancing hypodense lesion (mean CT density of - 90 HU) originating from the retroperitoneum and involving the entire abdomen and pelvis. It displaced the small bowel coils laterally to the left and the caecum, ascending colon, and right kidney anteromedially. The celiac axis and superior mesenteric artery (SMA) were displaced laterally to left (Fig 2, 3, 4). The CECT findings suggested diffuse retroperitoneal lipomatosis.
Figure 1.
A 35 year old woman with retroperitoneal lipomatosis. Findings: sonography demonstrates diffusely hyperechoic mass (Fig 1A asterix) causing sleeve like encasement and displacement of right kidney (Fig 1A white arrow). The urinary bladder (fig 1B @) is slightly elongated and seen displaced laterally by the diffuse hyperechoic mass (Fig 1B asterix) in the pelvis. Technique: Right subcostal and transverse ultrasound grayscale views of abdomen and pelvis (Figures 1A and 1B respectively). Sonography was performed using 3.5 Mhz convex transducer.
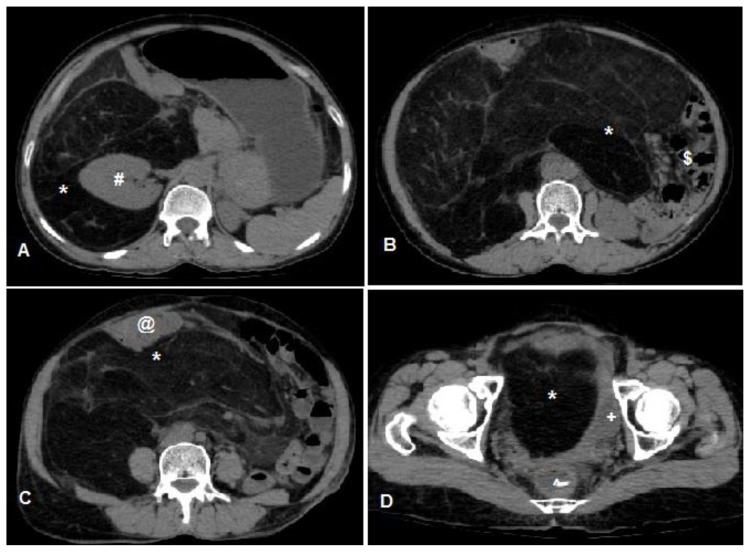
Figure 2.
A 35 year old woman with retroperitoneal lipomatosis (same patient). Findings: Axial Non enhanced CT (NECT) images taken cranio-caudally demonstrate presence of diffuse fat attenuation lesion with some septations within it located in the retroperitoneum and pelvis (Figure 2A, 2B, 2C, 2D asterix). It is also seen displacing the right kidney (Figure 2A #) anteriorly and medially, small bowel loops (Figure 2B $) laterally on left, transverse colon (Figure 2C @) anteriorly and causing compression and mild displacement of urinary bladder (Figure 2D +) and compression of rectum (Figure 2D ^). Technique: Axial NECT images of the abdomen and pelvis on 16 slice MDCT (Multi detector CT) machine, slice thickness 5mm, KV 120 and mAs 250.
Figure 3.
A 35 year old woman with retroperitoneal lipomatosis (same patient). Findings: Axial late arterial phase CECT images taken cranio-caudally demonstrate diffuse non enhancing fat attenuation lesion with some sepatations within it located in the retroperitoneum and pelvis (Figure 3A, 3B, 3C, 3D asterix). The displaced right kidney (Figure 3A white arrow) shows normal enhancement without any hydronephrosis. Displacement and mass effect is demonstrated on small bowel loops filled with positive contrast (Figure 3B white arrow), urinary bladder (Figure 3C #) and sigmoid colon (Figure 3D +). Technique: Axial CECT images of the abdomen and pelvis in late arterial phase on 16 slice MDCT machine, slice thickness 5mm, KV 120, mAs 250, intravenous 100 ml of iohexol at rate of 2.2ml/sec and oral contrast (20 ml iohexol diluted in 2 litres of water).
Figure 4.
A 35 year old woman with retroperitoneal lipomatosis (same patient). Findings: Coronal (figure 4A) and sagittal (Figure 4B) reformatted images of post contrast late arterial phase demonstrate the diffuse and non enhancing nature of the retroperitoneal lipomatosis (Figure 4A and 4B asterix) along with the mass effect caused by it on the adjacent viscera. Technique: Coronal and sagittal reformatted CECT images of the abdomen and pelvis in late arterial phase on 16 slice MDCT machine, slice thickness 5mm, KV 120, mAs 250, intravenous 100 ml of iohexol at rate of 2.2ml/sec and oral contrast (20 ml iohexol diluted in 2 litres of water).
Management and Follow-up
After the correction of anemia, the patient underwent an exploratory laprotomy using a right lateral retroperitoneal approach, which confirmed the imaging findings. She underwent debulking of the lesion with the removal of a large fatty mass weighing approximately 8.5 kg and measuring 40 × 35 × 32 cm (Fig. 5). However, because of extensive and diffuse involvement of the retroperitoneum, parts of the lesion were not removed. During the procedure, major vascular or ureteric injury was not sustained. The abdomen was closed and the mass lesion was sent for histopathological examination. The histopathological results reported that the fat cells were homogeneous in size and shape, showed a lobular growth pattern, and were separated by thin fibrous septa (Fig 6). The final diagnosis was benign retroperitoneal lipomatosis. The immediate postoperative period was uneventful, and the patient was discharged after a 20-day hospital stay and was advised monthly follow-up. After a 1-year follow-up period, the patient is now asymptomatic with complete relief from distention of abdomen and constipation.
Figure 5.
A 35 year old woman with retroperitoneal lipomatosis (same patient). Findings: Right lateral laprotomy (Figure 5A) demonstrates the non encapsulated fat containing lesion (Figure 5A asterix) causing anterior as well as posterior encasement of the right kidney (Figure 5A #). The near total resected gross specimen of the same measuring 40 × 35 × 32 cm and weighing 8.5kg is displayed.
Figure 6.
A 35 year old woman with retroperitoneal lipomatosis (same patient). Findings: The histopathology microscopic image hematoxylin and eosin stain viewed at magnification of 100 times demonstrates multiple fat cells, homogenous in size and shape exhibiting lobular growth pattern separated by thin fibrous septa (Figure 6 asterix).
DISCUSSION
Etiology & Demographics
Retroperitoneal lipomatosis is a benign condition involving the overgrowth of mature fat tissues in the extra-peritoneal compartment of abdomen. It predominantly affects the perirectal and perivesical regions [1]. It was first described by Engels (1959) following the similar findings on pelvic imaging in five men with urinary and bowel complaints and diffuse pelvic lump [2]. Incidence of retroperitoneal lipomatosis is 1.7 cases per 100,000 population [3]. However because of benign nature and low physician awareness of this disease, it is probably under detected and has considerably higher incidence.
Most studies pertaining to lipomatosis are single case reports. In 1991, Hynes published a report based on the review of 130 cases where the mean age of presentation was 48 years [4]. A definite male predominance was observed with a male to female ratio of 18:1 [4]. Retroperitoneal lipomatosis is more common in black people (approximately 67% of all cases) [4]. Very few cases of retroperitoneal lipomatosis have been reported in the Indian or Asian population. A single case was reported in 2003 from India [5]. In addition retroperitoneal lipomatosis was associated with condition known as multiple symmetric lipomatosis which manifests as of non encapsulated lipomas in the subcutaneous tissues of cervical, thoracic, abdominal and pelvic regions and the deltoid muscle. Multiple symmetrical lipomatosis is common in white men aged between 20 and 65 years than solitary lipomatosis [6]. In 1991, Kume et al.[7] described a case of 27-year-old man with achondroplasia and pelvic lipomatosis. Morever several cases are associated with proliferative cystitis, particularly cystitis glandularis [8].
Clinical & Imaging Findings
Patients often present with non specific complaints, such as lower abdominal pain, backache, or feeling of pelvic fullness. Urinary complaints, such as dysuria, frequency, urgency, and sense of incomplete evacuation, are the most commonly observed in approximately 50% patients. Gastrointestinal symptoms are less common (approximately 20%), and constipation is the predominant manifestation among them. In extensive lipomatosis, bilateral ureteral compression can result in severe hydronephrosis and can precipitate renal failure [4].
Plain radiographs of the abdomen may reveal extensive lucent areas, but mostly they are not commented on and instead are re-evaluated in retrospect. Intravenous urography demonstrates medially deviated and compressed ureters with varying grades of hydronephrosis. Cystography demonstrates an abnormally elongated bladder with superior and anterior displacement. Barium enema is not conducted routinely, but if conducted, then it demonstrates an elongated straightened rectum, with increased presacral space [4]. Ultrasonography is the most frequent and first imaging modality conducted for lipomatosis, which displays diffuse hyperechoic lesion causing the encasement of retro peritoneal organs along with their displacement. In extensive pelvic lipomatosis, the bladder appears to float in it and assumes a tubular “cigar” shape [9]. Cross sectional imaging is confirmatory because it identifies the fatty attenuation of the lesion with a great degree of confidence. CT and MRI are equally efficient in the diagnosis. CECT of the abdomen and pelvis reveals a nonenhancing and homogenously fat attenuating mass but there might be few fibrous septae within the lesion. However there is absence of any enhancing soft tissue mass pointing towards its benign nature. Positive oral contrast and delayed post contrast CT scans demonstrate the mass effect on the rectum and urinary bladder in detail, respectively [10]. On MRI, the lesions appear hyperintense on T1- and T2-weighted images, with the complete suppression of signal on fat-saturated sequences [11].
Treatment & Prognosis
There is no definite treatment for lipomatosis. Mostly this is an asymptomatic entity. If it is detected incidentally or is mildly symptomatic, without any deranged renal function, then it is treated conservatively. However, considering the progressive nature of this disease, it eventually leads to renal impairment, and thus, follow-up examinations at regular intervals are advised [12]. Sonography or urography detects obstructive uropathy; however, they are not sensitive to determine the progression of the lesion. Therefore cross-sectional imaging, preferably MRI, is favored because of its non ionizing nature. Pelvic lipomatosis is commonly associated with cystitis glandularis, which has a potential for malignant transformation. A case report on the development of vesical adenocarcinoma following pelvic lipomatosis exists; hence, regular follow-up with cystoscopy is advised in all cases [13]. Patients with severe symptoms or imapired renal function secondary to urinary outflow obstruction caused by this lesion should be managed surgically. Temporary relief from urinary tract complaints can be achieved by stenting the obstructed ureters. Complete fat excision is extremely difficult because of the diffuse nature of this disease. Therefore, this approach is not curative, but is used to relieve the mass effect caused. Several patients finally require ureteral diversion [14,15].
Differential Diagnosis [1]
The differential diagnosis for retroperitoneal lipomatosis includes all retroperitoneal fat containing lesions.
Liposarcoma
Well-differentiated liposarcoma has a close resemblance with the imaging features of benign lipomatosis. However, liposarcoma has a heterogenous appearance with enhancing soft tissue masses in it. Calcification can be observed in some cases.
Lipoblastomatosis
This involves the proliferation of fetal retroperitoneal fat. It is common in pediatric groups and contains areas of myxoid stroma in it which gives variable signal on MRI.
Lipoma
It is rare in the retroperitoneum but shows imaging findings similar to lipomatosis, except that it is well-encapsulated. The two can be confused if the lesion is extremely large.
Hibernoma
This is a rare benign lesion composed of brown fat. It appears to be similar to other retropereitoneal fat containing lesions; however, the intra lesional septations are seen to be enhancing on post contrast CT or MRI studies.
Teratoma
It is a well-defined solid cystic germ cell tumor containing fat and calcification within it.
Myelolipoma
This is a benign diffuse lesion containing fat and hemopoietic components. It has a heterogenous appearance on CT scans and MRI, and with enhancing soft tissue components as well as non enhancing areas of hemorrhage.
TEACHING POINT
It is essential for radiologist to know about the ultrasound appearance of retroperitoneal lipomatosis and its complications especially when confronted with cases of a suspected lump in abdomen with diffuse hyperechoic imaging features on sonography and without any obvious focal mass.
Table 1.
Summary table for retroperitoneal lipomatosis.
| Etiology | Sporadic development of non-encapsulated lipomas in retroperitoneum. Associated with multiple symmetric lipomatosis. |
|
| |
| Incidence | 1.7 cases per 100,000 population. |
|
| |
| Gender ratio | Male to female ratio is 18:1. |
|
| |
| Age predilection | 4th to 5th decade |
|
| |
| Risk factor | Black race |
|
| |
| Treatment | Conservative and follow-up in mild or asymptomatic cases. Surgical excision with or without urinary tract interventions (stenting, ureterostomy). |
|
| |
| Prognosis | Progressive and non-curable nature of disease causing varying degree of urinary tract obstruction eventually leading to end stage renal disease if not treated. Patients subjected to excision with or without urinary diversion lead symptom free life. Life time risk of urinary bladder malignancy. |
|
| |
| Imaging findings | |
| Plain Radiographs | Extensive lucent areas in abdomen and pelvis. |
| Sonography | Diffuse hyperechoic mass causing sleeve like encasement of retroperitoneal organs along with their displacement and cigar shaped elongated and floating bladder in pelvis. |
| Intravenous urography | Varying degree of hydronephrosis and hydroureter. Urinary bladder is elongated in shape. |
| Barium enema | Elongated, straightened rectum with enlarged pre sacral space. |
| CT scan | Non enhancing fat density diffuse mass in retroperitoneum with few fibrous septations within it. |
| MRI scan | Homogenously hyperintense retroperitoneal lesion on both T1W and T2W sequences and showing suppression of signal on fat saturated sequences. No enhancement on post contrast images. |
Table 2.
Differential diagnosis table for retroperitoneal lipomatosis.
| Lesion | X ray | USG | CT Scan | MRI | Enhancement pattern |
|---|---|---|---|---|---|
| Lipomatosis | Diffuse lucency in abdomen | Diffuse hyperechoic mass | Diffuse retroperitoneal mass lesion of fat attenuation with few fibrous septa | Hyper intense on both T1W and T2W images with complete suppression of signal on fat saturated images | None |
| Liposarcoma | Diffuse lucency in abdomen | Diffusely heterogenous, predominantly hyperechoic mass | Diffuse fat attenuation retroperitoneal mass lesion with areas of soft tissue attenuation density within it. Calcification may be seen. |
Fat component is hyperintense on both T1W and T2W, soft tissue component is hypo intense on T1W and iso intense on T2W. Calcification and hemorrhage seen on GRE. |
Solid component shows moderate heterogenous enhancement |
| Lipoblastomatosis | Diffuse lucency in abdomen | Diffusely hyperechoic mass with few septations and cysts in it | Encapsulated fat attenuation lesion with internal septae | Low signal on T1W and high signal on T2W | Mild to none |
| Hibernoma | Diffuse lucency in abdomen | Diffusely hyperechoic mass with increased internal vascularity as seen on color Doppler | Well-defined capsulated hypo attenuating mass with intralesional soft tissue density septations in it | Slightly hypointense to subcutaneous fat on T1W and variable on T2W. Hyperintense than subcutaneous fat on STIR |
Septations may show mild enhancement |
| Teratoma | Normal | Solid cystic lesion with variable echoes and post acoustic shadowing due to calcification | Well defined soft tissue lesion with areas of fat attenuation and calcification in it. | Variable signal intensity due to presence of fat, soft tissue and calcification. Fat is hyperintense on T1W and T2W while calcification appears dark on both. | Soft tissue component shows variable enhancement. |
| Angiomyolipoma | Normal | Well defined highly hyperechoic and homogenous lesion with sharp margins | Hypodense lesion with distinct borders having fat attenuation within it. | Fat component hyper on T1W, soft tissue is hypo on T1W and iso on T2W | Mild to moderate homogenous enhancement. |
ACKNOWLEDGEMENTS
Ravish Fangari from department of Patholgy, Dr V M Govt Medical College & SCSM Gen Hospital, Solapur, India for providing the histopathology images.
Rahul Wagh from department of Surgey, Dr V M Govt Medical College & SCSM Gen Hospital, Solapur, India for providing the gross and intraoperative images.
ABBREVIATIONS
- CECT
Contrast enhanced computed tomography
- CT
Computed Tomography
- HU
Housefield Units
- KV
Kilovolt
- mAs
mili ampere seconds
- MRI
Magnetic resonance imaging
- OPD
Out patient department
- SMA
Superior mesenteric artery
REFERENCES
- 1.Craig WD, Fanburg-Smith JC, Henry LR, Guerrero R, Barton JH. Fat-containing lesions of the retroperitoneum: radiologic-pathologic correlation. Radiographics. 2009 Jan-Feb;29(1):261–90. doi: 10.1148/rg.291085203. [DOI] [PubMed] [Google Scholar]
- 2.Engels EP. Sigmoid colon and urinary bladder in high fixation: roentgen changes simulating pelvic tumor. Radiology. 1959 Mar;72(3):419–22. doi: 10.1148/72.3.419. [DOI] [PubMed] [Google Scholar]
- 3.Radinsky S, Cabal E, Shields J. Pelvic lipomatosis. Urology. 1976 Jan;7(1):108–11. doi: 10.1016/0090-4295(76)90578-1. [DOI] [PubMed] [Google Scholar]
- 4.Heyns CF. Pelvic lipomatosis: a review of its diagnosis and management. J Urol. 1991 Aug;146(2):267–73. doi: 10.1016/s0022-5347(17)37767-4. [DOI] [PubMed] [Google Scholar]
- 5.Zargar AH, Laway BA, Masoodi SR, Bhat MH, Bashir MI, Wani AI, Wani NA. Diffuse abdominal lipomatosis. J Assoc Physicians India. 2003 Jun;51:621–2. [PubMed] [Google Scholar]
- 6.Lomartire N1, Ciocca F, Di Stanislao C, Bologna G, Giuliani M. Multiple symmetrical lipomatosis (MSL): a clinical case and a review of the literature. Ann Ital Chir. 1999 Mar-Apr;70(2):259–62. discussion 262–3. [PubMed] [Google Scholar]
- 7.Kume H, Kume Y, Takamoto K. Achondroplasia associated with pelvic lipomatosis. Lancet. 1999 Mar 20;353(9157):1017. doi: 10.1016/S0140-6736(05)70731-5. [DOI] [PubMed] [Google Scholar]
- 8.Tong RS, Larner T, Finlay M, Agarwal D, Costello AJ. Pelvic lipomatosis associated with proliferative cystitis occurring in two brothers. Urology. 2002 Apr;59(4):602. doi: 10.1016/s0090-4295(01)01609-0. [DOI] [PubMed] [Google Scholar]
- 9.Clark WM, Hatten HP., Jr Ultrasonographic features of pelvic lipomatosis. Urol Radiol. 1(3):1979–1980. 183–6. doi: 10.1007/BF02926626. [DOI] [PubMed] [Google Scholar]
- 10.Waligore MP, Stephens DH, Soule EH, McLeod RA. Lipomatous tumors of the abdominal cavity: CT appearance and pathologic correlation. AJR Am J Roentgenol. 1981 Sep;137(3):539–45. doi: 10.2214/ajr.137.3.539. [DOI] [PubMed] [Google Scholar]
- 11.Torigan DA, Ramchandani P. Retroperitoneum. In: Hagga JR, Dogra VS, Forsting M, Gilkeson RC, Kwon HAH, Sundaram M, editors. CT and MRI of the Whole Body. 5th edition. Philadelphia: Mosby Elsevier; 2009. [Google Scholar]
- 12.Klein FA1, Smith MJ, Kasenetz I. Pelvic lipomatosis: 35-year experience. J Urol. 1988 May;139(5):998–1001. doi: 10.1016/s0022-5347(17)42744-3. [DOI] [PubMed] [Google Scholar]
- 13.Johnston OL, Bracken RB, Ayala AG. Vesical adenocarcinoma occurring in patient with pelvic lipomatosis. Urology. 1980 Mar;15(3):280–2. doi: 10.1016/0090-4295(80)90445-8. [DOI] [PubMed] [Google Scholar]
- 14.Albert DJ, Herman GP, Persky L. Pelvic lipomatosis. Report of three cases. J Med. 1972;3(4):282–92. [PubMed] [Google Scholar]
- 15.Golding PL, Singh M, Worthington B. Bilateral ureteric obstruction caused by benign pelvic lipomatosis. Br J Surg. 1972 Jan;59(1):69–72. doi: 10.1002/bjs.1800590119. [DOI] [PubMed] [Google Scholar]