Abstract
Isolated injuries to the teres major muscle occur in competitive sporting activities such as baseball pitching, hockey and tennis. We report a similar event of a physically fit man sustaining an isolated teres major rupture while waterskiing. Non-operative management was chosen, with pain resolution and no appreciable functional limitations at follow up. Because teres major muscle injury was suspected at the time of imaging, we present a dedicated imaging protocol to optimize assessment for teres major injury.
Keywords: teres major, water skiing, rotator cuff tear, myotendinous injury, muscle strain
CASE REPORT
A 53-year-old right hand dominant male presented with left shoulder pain two weeks after a waterskiing accident. The injury occurred after he lost his balance and had a forceful traction event pulling his left arm forward. Pain was reported with the initial injury, but he expressed little pain afterwards. He noticed a change in contour along his posterior axilla and the need to compensate in athletic activity with his right arm.
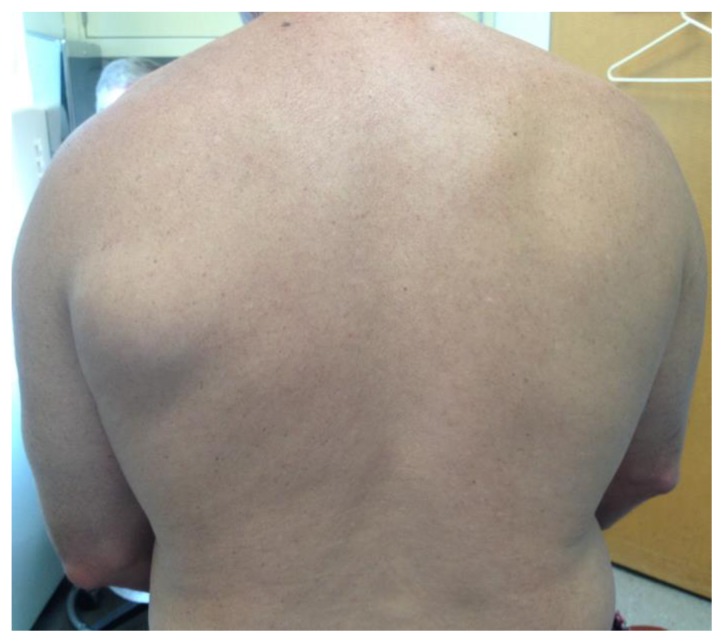
On physical exam, he was a fit male in no distress. Neurovascular status was intact. Forward elevation was 180 degrees actively and passively. External rotation was 60 degrees actively and passively. Internal rotation was to T8 (normal T4–T8). All planes of motion were symmetric with the contralateral side. Resisted abduction and abduction and external rotation were mildly painful. No appreciable weakness was noted in forward flexion, external rotation, internal rotation or latissimus dorsi testing. There was a visible asymmetry in the patient’s posterior axillary fold (Figure 1).
Figure 1.
53 year-old man with isolated left teres major rupture.
Findings: Clinical photograph demonstrates a visible asymmetry of the left posterior axillary region with a palpable soft tissue mass.
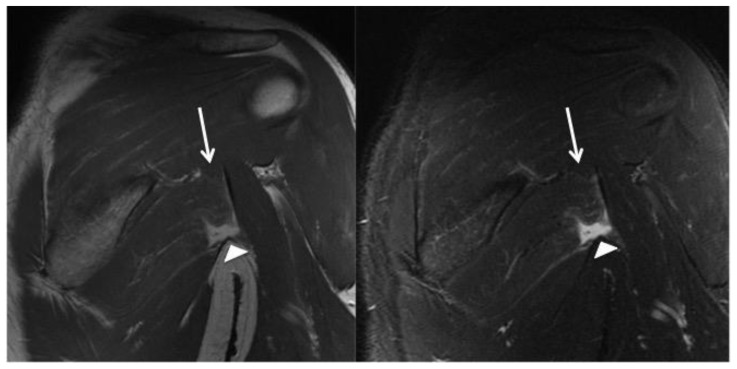
A standard series of shoulder radiographs were normal. Dedicated, 1.5 Tesla magnetic resonance imaging (MRI) was performed, to assess for teres major injury, which was suspected at the time of imaging. This required a larger field of view than a standard shoulder MRI. True axial imaging plane was obtained for initial assessment for the teres major tendon insertion and muscle orientation. Subsequent coronal oblique and sagittal oblique imaging planes were performed parallel and perpendicular to the axis/orientation of the teres major muscle fibers respectively. Intermediate fast spin echo and short-tau inversion recovery images demonstrated a mild strain at the tendon insertion, partial myotendinous tear of the superior (cranial) muscle fibers of the teres major with complete myotendinous tearing of the inferior (caudal) fibers, with a fluid signal gap at the site of complete tearing. The rotator cuff was intact. MRI images are demonstrated in Figures 2 and 3.
Figure 2.
53 year-old man with isolated left teres major rupture.
FINDINGS: Normal location of the teres major inferior to the scapula. There is partial (grade II myotendinous junction) tearing of the superior (cranial) most fibers, which demonstrate mild increased signal intensity and an undulating contour (arrows). There is a complete tear (grade III myotendinous injury) of the inferior (caudal) tendon fibers with a fluid filled gap at the site of the complete tear (arrowheads).
TECHNIQUE: Coronal oblique intermediate fast spin echo [TR: 3500 TE: 37.128; field of view 24 cm; matrix 384 × 288; slice thickness: 4 mm with no gap] (left) and short-tau inversion recovery [TR: 2750; TE: 50.48; field of view: 24; matrix: 288 × 224; slice thickness 5mm with no gap] (right).
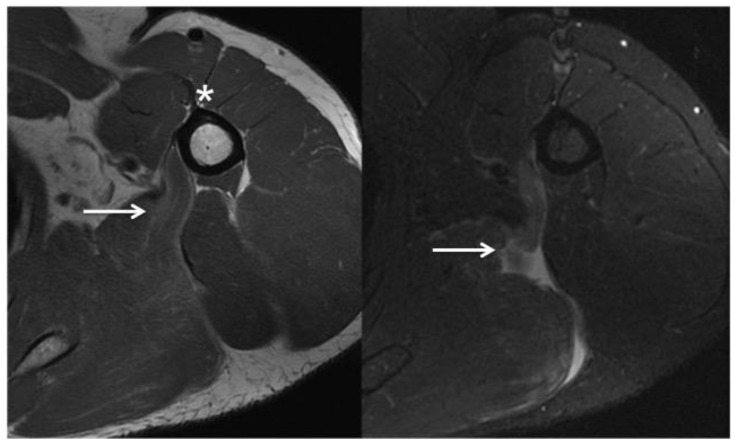
Figure 3.
53 year-old man with isolated left teres major rupture.
FINDINGS: The teres major demonstrates tapering of the muscle fibers from posterior medial to anterior lateral. The normal teres major tendon attaches to the medial ridge of the intertubercular groove, just posterior medial to the pectoralis major tendon (asterisk, left). Intermediate fast spin echo images of the superior tendon fibers demonstrate mild increased signal intensity and undulation of the fibers compatible with partial tearing (arrow, left). T2-weighted fat saturated images more inferiorly demonstrate complete tearing of the inferior-most muscle fibers with a fluid filled gap at the site of tearing (arrow, right).
TECHNIQUE: Axial intermediate fast spin echo [TR: 3850 TE: 33.408; field of view 22cm; matrix: 384 × 288; slice thickness: 4 mm with no gap] (left) and short-tau inversion recovery [TR: 3,500; TE: 49.28; field of view: 22; matrix: 288 × 224; slice thickness 5mm with no gap] (right).
The patient was treated nonoperatively with physical therapy. The therapy instructions were for deltoid, rotator cuff and peri-scapular musculature range of motion, strengthening and proprioception, and modalities including ultrasound therapy and massage. Therapy was prescribed at a frequency of three times per week for six weeks.
The patient returned 14 weeks after the injury. He reported compliance with the therapy protocol, and he continued to do a series of exercises at home. His visual analog scale pain score was 0. His range of motion passively and actively was 180 degrees of forward elevation, 60 degrees of external rotation and internal rotation to T8. The motion was symmetric to his contralateral side. Dynamometer strength testing demonstrated the following averages: Abduction strength was 18.1 lbs on the left and 19.4 lbs on the right. Forward elevation strength was 17.6 lbs on the left and 20.2 lbs on the right. External rotation strength was 16.8 lbs on the left and 19.2 lbs on the right. Internal rotation strength was 25.5 lbs on the left and 24.4 lbs on the right. The patient reported he was back to all normal activities and swimming with no appreciable limitations.
DISCUSSION
Anatomy
The teres major muscle arises from the posterior surface of inferior scapula, at the angle. It courses superiorly and laterally ending as a short tendon, which inserts on the medial lip of the intertubercular groove. It is innervated from the posterior cord of the brachial plexus by the lower subscapular nerve. The teres major muscle is thought to function as a unit with the latissimus dorsi, where it acts in synergy to extend, adduct and internally rotate the shoulder [1,2].
Etiology
The teres major and latissimus dorsi muscles act in the acceleration and follow through phases of the throwing motion [3] which is likely why the reported cases of injury in pitchers occurs during throwing of off-speed pitches and can be injured during traction of the upper extremity while waterskiing, as in this case.
Demographics, Treatment & Prognosis
Malcolm et al. [4] treated a 22 year-old baseball pitcher with an isolated teres major rupture nonoperatively. Six months later, the patient returned with no loss of performance and no pain. Leland et al. [5] described isolated teres major injuries in two professional baseball pitchers. Both tears were confirmed by MRI, and both pitchers were treated nonoperatively. Both pitchers returned to professional pitching without limitation within the same year. Schickendantz et al. [6] described a case series of ten professional baseball pitchers. Five had isolated latissimus dorsi tears, four had isolated teres major tears, and one had a combined injury. All ten pitchers were treated nonoperatively. All the players, except for the pitcher who tore both, returned to pitching in the same season at the same or higher level.
Isolated teres major injuries have also been reported in tennis and professional hockey. Takase [7] reported on a 21 year old male tennis player who sustained an isolated teres major rupture while completing an overhead serve. The patient was treated nonoperatively, and after six months, he made a full recovery back to tennis. Grosclaude et al. [8] reported on two professional ice hockey players who sustained an isolated teres major rupture. One injury occurred during the windup phase of a slap shot, and the other occurred while striking an opponent’s stick during a faceoff. Both players were treated nonoperatively, and both players returned to professional play within one week.
Three reports in the literature were similar to the patient described in this report. Maldjian et al. [9] reported on a 30 year-old male who sustained an isolated teres major injury while waterskiing. This patient had a similar mechanism of injury with the tow rope causing forceful forward flexion. Lester et al. [10] reported an isolated teres major injury sustained by a 30 year-old male while waterskiing. The patient was treated nonoperatively, and after 16 weeks, no pain or functional limitations were noted. Garrigues et al. [11] reported on a 33 year old male who sustained a teres major injury while waterskiing. This patient had a surgical repair, and at 1 year, the patient reported the shoulder was back to normal, and standardized outcome measures were excellent.
Clinical & Imaging Findings
There is limited data available regarding isolated teres major injuries. Patients describe similar symptoms including ecchymosis, swelling and pain and the posterior inferior axilla. The teres major is not a regularly evaluated structure on a standard shoulder MRI. If a tear of the teres major or latissimus dorsi is suspected, the radiologist should be alerted so the standard field of view for a shoulder MRI can be expanded to include the teres major in its entirety. Leland et al. [5] recommended a large field of view MRI including the bilateral shoulder girdles. Given current MRI and coil technology, this is not necessary as large field of view images greatly limit anatomic detail. Because the teres major takes a unique course from posterior medial to anterior lateral, special coronal oblique and sagittal oblique images of the teres major should be obtained. These views are parallel and perpendicular, respectively, to the normal course of the tendon and muscle fibers (figure 4) and give a more detailed view of the muscle belly, myotendinous junction and tendinous insertion for accurate description of the injury. This is analogous to the imaging protocol for a pectoralis major tendon injury [12]. Aside from the proper imaging planes, intermediate fast spin-echo and fluid sensitive sequences should be obtained to provide a complete evaluation. We advocate use of an 8 channel cardiac coil with tri-plane, intermediate fast spin echo and fluid sensitive (T2 weighted with fat saturation or short-tau inversion recovery) weighted sequences.
Teres major injury should not be confused with an injury of the latissimus dorsi. Both muscles function synergistically and can be injured by a common mechanism. Compared to the teres major, the latissimus dorsi is a much larger, fan-shaped muscle, which originates below the teres major, emanating from the thoracic spinous processes, ribs and iliac crest. Like the teres major, the latissimus dorsi terminates as a thin tendon, inserting on the humerus at the floor of the intertubercular groove, between the teres major tendon medially and the pectoralis major tendon laterally.
Differential Diagnoses
Differential diagnosis of abnormal muscle signal is non-specific and includes a number of entities; findings on imaging studies must be corroborated with clinical history. Myotendinous strain or tear results from forced muscle stretch during contraction, known as eccentric contraction. Increased signal between muscle fibers on fluid sensitive images can be seen in grade 1 myotendinous injury (first degree strain), which is characterized by edema tracking along the muscle fascicles producing a “feathery” pattern with perifascial edema. Grade 1 strains are characterized by minimal to no fiber disruption without deformity of the myotendinous unit.
Grade II myotendinous injury is moderate strain characterized by partial disruption at the myotendinous junction. This characterized by hemtoma formation at the site of tear and variable loss of strength. Grade II injures usually resolve without intervention. Complete disruption of the myotendinous junction is seen in the setting of grade III myotendinous injury or severe strain, which results in frank discontinuity of the muscle fibers and possible fiber retraction, which requires surgical intervention. These findings can appear similar to acute muscle transaction from penetrating trauma and results in loss of strength.
Muscle contusion from a direct blow appears similar to myotendinous injury, with a more focal area of increased signal between muscle fibers, similar to a grade 1 strain, with muscle enlargement. No distinct muscle fiber disruption is present. This can be accompanied by the formation of intramuscular hematoma with possible development of myonecrosis and myositis ossificans.
Increased fluid signal within the muscle fibers can also be seen in in acute denervation. This is differentiated from muscle strain because of the lack of perifascial edema, involves a nerve territory and increased fluid sensitive signal and/or enhancement in the peripheral nerve. Subacute denervation will also demonstrate a combination of increased muscle signal as well as fatty infiltration. Chronic muscle denervation will demonstrate fatty replacement as well as decreased muscle bulk without significant signal abnormality. Muscle inflammation in the setting of infectious, inflammatory, vascular insult or iatrogenic myositis will also produce increased signal within the muscle on fluid sensitive images and usually requires biopsy to determine the etiology and definitive diagnosis [13–14].
Based on our literature review, most teres major injuries occur at the myotendinous junction. Injury assessment is based on the standard MRI grading criteria for muscle and myotendinous injuries [15]. Most cases reported in the literature were described as grade II injuries with high fluid sensitive signal noted along with muscle fascicles with attenuation of the myotendinous junction. Our cases had a mixed injury with high fluid sensitive signal and attenuation of the myotendinous junction of the superior/cranial fibers consistent with a grade II injury as well as frank muscle fiber disruption of the inferior/caudal fibers classified as a grade III injury.
Summary
We report an isolated teres major rupture sustained while waterskiing, evaluated utilizing a dedicated imaging protocol obtained relative to the plane of the teres major muscle and tendon for optimal assessment revealing a mixed grade II–III myotendinous injury. Nonoperative treatment has been the standard for all but one of the reported cases in the literature, and all reported cases, including ours, have demonstrated excellent outcomes. At follow up he reported no pain or functional limitations and he was back to competitive athletics.
TEACHING POINT
Isolated teres major rupture is uncommon and can occur from a variety of sporting activities that exert traction on the shoulder girdle. Injury assessment can be performed using a dedicated MRI imaging protocol with utilizing planes parallel and perpendicular to the axis of the myotendinous junction to grade the degree of injury.
Table 1.
Summary table for Teres major tear.
| Etiology | Traumatic, usually due to forceful traction on an outstretched arm or during throwing motion. |
| Incidence | Rare. Reported in the orthopedic literature, mostly in overhead athletes (pitchers) |
| Gender Ratio | Unknown. All of the reported cases were in males. |
| Risk Factors | Any action or motion that places excessive stress on the shoulder girdle: throwing in high-level athletes, water skiing, hockey, tennis etc. |
| Treatment | Conservative management with pain management and physical therapy. Only one report of operative treatment where the patient returned to normal function. |
| Prognosis | Good. Most athletes return to sport without restriction (as reported in this case and the literature). |
Table 2.
Differential diagnosis table for Teres major tear.
| Teres Major Tear | MRI: Increased signal within the muscle fibers of teres major muscle with variable disruption of the myotendinous junction. The teres major courses laterally towards the humerus from the inferior scapular angle, ending as a thin tendon, which inserts on the intertubercular groove medial to the pectoralis tendon. |
| Latissimus Dorsi Tear | MRI: Increased signal within the muscle fibers of latissimus dorsi muscle with variable disruption of the myotendinous junction. The latissimus dorsi muscle, compared to the teres major, is a larger, more inferior, fan shaped muscle, which has origins from the spinous process, the iliac crest and inferior ribs, tapering to a fasciculus as it courses towards the humerus, passing anterior to the teres major, inserting anterior and lateral to the teres major tendon. |
| Teres Major Myositis | MRI: Increased signal within the musculature on fluid sensitive can represent infectious or inflammatory myositis (including Parsonage Turner syndrome). This is manifest by increased fluid sensitive signal within the muscle without disruption of the myotendinous junction or muscle fiber disruption. |
| Teres Major Denervation | MRI: Increased signal within the muscle fibers of the teres major on fluid sensitive sequences can represent sequela of denervation. Acute denervation will manifest simply as increased muscle signal on fluid sensitive sequences without involvement of the tearing myotendinous junction or muscle fiber disruption and is difficult to differentiate from myositis. Fat replacement within the muscle fibers on non-fat-saturated sequences represents subacute or chronic denervation change, which is not seen in the setting of an acute traumatic tear, but can be a finding of chronic injury. |
ABBREVIATIONS
- lbs
pounds
- MRI
magnetic resonance imaging
REFERENCES
- 1.Broome HL, Basmajian JV. The function of the teres major muscle: an electromyographic study. Anat Rec. 1971;170:309–10. doi: 10.1002/ar.1091700307. [DOI] [PubMed] [Google Scholar]
- 2.Beck PA, Hoffer MM. Latissimus dorsi and teres major tendons: a separate or conjoint tendons? J Pediatr Orthop. 1989;9:308–9. [PubMed] [Google Scholar]
- 3.Gowan ID, Jobe FW, Tibone JE, Perry J, Moynes DR. A Comparative electromyographic analysis of the shoulder during pitching. Professional versus amateur pitchers. Am J Sports Med. 1987;15:586–90. doi: 10.1177/036354658701500611. [DOI] [PubMed] [Google Scholar]
- 4.Malcolm PN, Reinus WR, London SL. Magnetic resonance imaging appearance of teres major injury in a baseball pitcher. Am J Sports Med. 1999;27:98. doi: 10.1177/03635465990270012401. [DOI] [PubMed] [Google Scholar]
- 5.Leland JM, Ciccotti MG, Cohen SB, Zoga AC, Frederick RJ. Teres major injuries in two professional baseball pitchers. J Shoulder Elbow Surg. 2009;18:e1–5. doi: 10.1016/j.jse.2009.01.025. [DOI] [PubMed] [Google Scholar]
- 6.Schickendantz MS, Kaar SG, Meister K, Lund P, Beverly L. Latissimus dorsi and teres major tears in professional baseball pitchers: a case series. Am J Sports Med. 2009;37:2016–2020. doi: 10.1177/0363546509335198. [DOI] [PubMed] [Google Scholar]
- 7.Takase K. Isolated rupture of the teres major muscle. J Orthop Sports Phys Ther. 2008;38:439. doi: 10.2519/jospt.2008.0407. [DOI] [PubMed] [Google Scholar]
- 8.Grosclaude M, Najihi N, Ladermann A, Menetrey J, Ziltener JL. Teres major muscle tear in two professional ice hockey players: Cases study and literature review. Orthop Traumatol Surg Res. 2012;98(1):122–125. doi: 10.1016/j.otsr.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 9.Maldjian C, Adam R, Oxberry B, Chew F, Kelly J. Isolated tear of the teres major: a waterskiing injury. J Comput Assist Tomogr. 2000;24(4):594–595. doi: 10.1097/00004728-200007000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Lester JD, Boselli KJ, Kim PD, Ahmad CS. Isolated rupture of the teres major tendon. Orthopedics. 2010;33(11):847. doi: 10.3928/01477447-20100924-32. [DOI] [PubMed] [Google Scholar]
- 11.Garrigues GE, Lazarus MD. Operative treatment of isolated teres major ruptures. J Shoulder Elbow Surg. 2012;21:e6–11. doi: 10.1016/j.jse.2011.10.014. [DOI] [PubMed] [Google Scholar]
- 12.Connel DA, Potter HG, Sherman MF, Wickiewicz TL. Injuries of pectoralis major muscle: evaluation with MR imaging. Radiology. 1999;210:785–791. doi: 10.1148/radiology.210.3.r99fe43785. [DOI] [PubMed] [Google Scholar]
- 13.Bourint Rd, Fritz RC, Steinbach LS. Imaging of sports-related muscle injuries. Radiol Clinc North Am. 2002 Mar;40(2):333–62. vii. doi: 10.1016/s0033-8389(02)00008-8. [DOI] [PubMed] [Google Scholar]
- 14.Shelly MJ, Hodnett PA, MacMahon PJ, Moynagh MR, Kavanagh EC, Eustace SJ. MR Imaging of Muscle Injury. Magn Reson Imaging Clin N Am. 2009 Nov;17(4):757–73. vii. doi: 10.1016/j.mric.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 15.Armfield DR, Kim DH, Towers JD, Bradlye JP, Robertson DD. Sports related muscle injury in the lower extremity. Clin Sports Med. 2006;25:803–42. doi: 10.1016/j.csm.2006.06.011. [DOI] [PubMed] [Google Scholar]