Abstract
Multiple national initiatives seek to curb spending in order to address increasing health care costs in the United States. The Choosing Wisely® initiative is one popular initiative that focuses on reducing health care spending by setting guidelines to limit tests and procedures requested by patients and ordered by physicians. To reduce spending on neuroimaging, the Choosing Wisely® initiative and other organizations have offered guidelines to limit neuroimaging for headaches. Although the intentions are laudable, these guidelines are inconsistent with the neurosurgeon’s experience with brain tumor patients. If adopted by governing or funding organizations, these guidelines threaten to negatively impact the care and outcomes of patients with brain tumors, who frequently present with minimal symptoms or isolated headaches syndromes. As we grapple with the difficult conflict between evidence-based cost-cutting guidelines and individualized patient-tailored medicine, a physician must carefully balance the costs and benefits of discretionary services such as neuroimaging for headaches. By participating in the development of validated clinical decision rules on neuroimaging for headaches, neurosurgeons can advocate for their patients and improve their patients’ outcomes.
Keywords: Choosing Wisely, Headaches, Neuroimaging, Magnetic Resonance Imaging
Health care spending in the United States reached 2.8 trillion dollars, nearly $9,000 per person, in 2012.1 The United States spends more of its gross domestic product on healthcare than any other country in the world.2 Hence, healthcare economics reform has dominated the United States political scene and health care reforms will continue to shape patient care and physician practices. To direct healthcare reform, national organizations have implemented initiatives to address waste in the medical field. The Choosing Wisely® initiative focuses on reducing health care spending by setting guidelines to limit tests and procedures requested by patients and ordered by physicians.
Epidemiological analysis has shown that lifetime prevalence of headaches is 93–99%.3 In the primary care setting, headaches are the chief complaint in 1.5% of all visits4. Countless medical textbooks and journal articles provide insight and guidance on the clinical diagnosis of headache disorders, and most primary headaches can be diagnosed through careful history and physical examination.5 Nonetheless, neuroimaging in the United states between 2007 and 2010 for migraines and headaches approached $1.2 billion.6 In “Choosing Wisely in Headache Medicine: The American Headache Society's List of Five Things Physicians and Patients Should Question,” Loder et al. draw attention to improving health care efficiency in the diagnosis and treatment of headache disorders.7 Loder et al. discourage neuroimaging in patients with stable headaches that meet criteria for migraine. In a parallel, Choosing Wisely® guidelines by The American College of Radiology and Consumer Reports similarly suggested, “Don't do imaging for uncomplicated headaches.”8, 9 Further guidelines suggest that neuroimaging should only be ordered if a stable headache patient displays localizing neurological symptoms or signs.10
The proposed neuroimaging guidelines for headaches are inconsistent with the common experience of many neurosurgeons who treat brain tumors: specifically, patients with brain tumors may present with isolated headaches in the absence of other neurological symptoms and signs. Early diagnosis of brain tumors allows for prompt treatment before more severe symptoms, reduced performance status and worsened outcomes. In this manuscript, we discuss the presentation of brain tumor patients who often present with headaches alone or minimal symptoms. Although we applaud and support efforts to identify excessive and harmful spending in the medical system, we caution against creating over-reaching guidelines which could harm specific patient populations. In an atmosphere where medical care is under harsh economic pressures, population health care initiatives and guidelines are not always best for the neurosurgical patient.
BRAIN TUMOR SYMPTOMOLOGY
Brain tumors may present with focal or non-focal manifestations or no symptoms at all. Non-focal symptoms may include headaches, mental status changes, papilledema or seizures. Mental status changes may include impaired cognitive function, confusion, delirium or reduced consciousness. Seizures may occur in 15–50% of patients with brain tumors.11 Papilledema is seen in <20% of brain tumor patients.11 Focal findings vary depending on the anatomical location of the lesion and range from speech dysfunction to motor or sensory deficits.
Headaches secondary to brain tumors are thought to occur from traction on basal meningeal structures and occur in 48% of patients with brain tumors.11 Headaches associated with brain tumors may be worse in the morning and slowly progressive.11 However, despite classic teachings, headaches that are caused by tumors may be similar to tension-type or migraine-type headaches in 77% and 9% of cases, respectively.11
SYMPTOMS OF BRAIN TUMORS: WASHINGTON UNIVERSITY EXPERIENCE
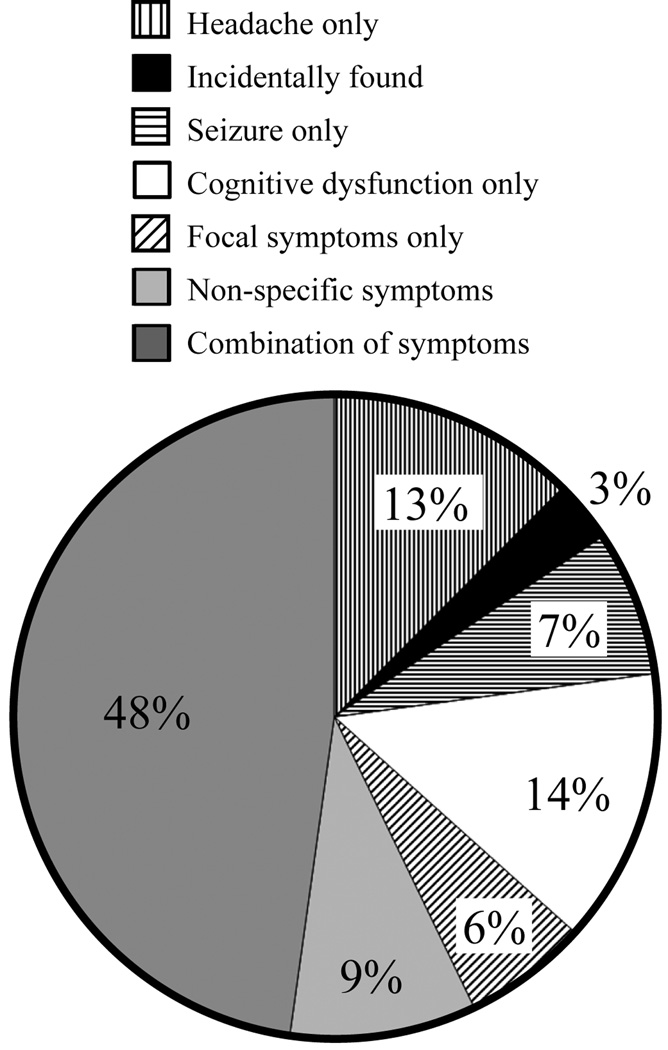
After approval by the Washington University Institutional Review Board, we performed a retrospective review of patients who were diagnosed with a brain neoplasm from an open brain biopsy12. Preoperative histories and physical examinations were reviewed for presenting symptoms. Superficial open brain biopsies were performed through a small craniotomy in order to obtain diagnostic pathology. Pathology reports were reviewed and only neoplasms were included in the study. The cohort’s pathology results included 68% glial neoplasms, 12% meningiomas and 20 % other tumor types (Table 1). Seizures were the presenting symptom in 7.4% of brain tumor patients. Cognitive and speech dysfunction were the presenting symptoms in 13.7% of patients. Six percent of brain tumor patients presented with isolated focal motor, sensory or visual symptoms. Ten percent of patients presented with non-focal symptoms including non-localizing subjective sensory or perceptual symptoms, facial swelling and an endocrinopathy. Forty-eight percent of patients presented with a combination of symptoms. Three percent of patients with brain tumors presented with asymptomatic lesions that were found incidentally on unrelated radiographic examinations. Finally, isolated headaches were the only complaint in 11.6% of brain tumor patients (Table 2, Figure 1). Not surprisingly, isolated-headache patients did not experience resolution of their symptoms after brain biopsy; however, etiology-specific therapies were initiated. Hence, 24.2% of patients with brain tumors diagnosed by brain biopsy presented with isolated headaches, no symptoms or non-specific symptoms.
Table 1.
Brain Tumor Diagnoses
| Pathology | Number | Percent |
|---|---|---|
| Glial Neoplasm | 64 | 68% |
| Meningioma | 11 | 12% |
| Metastasis | 3 | 3% |
| Lymphoma | 9 | 9% |
| Other | 8 | 8% |
Table 2.
Presentation of Brain Tumor Patients
| Symptom/Sign | Incidence |
|---|---|
| Headache only | 11/95 (11.6%) |
| Asymptomatic/Incidentally-found | 3/95 (3.2%) |
| Seizures only | 7/95 (7.4%) |
| Cognitive dysfunction only | 13/95 (13.7%) |
| Focal symptoms only | 6/95 (6.3%) |
| Non-specific symptoms | 9/95 (9.5%) |
| Combination of symptoms | 46/95 (48.4%) |
Figure 1.
Presentation of Patients with Brain Tumors.
The proposed neuroimaging recommendations for isolated headaches are contingent on symptom onset, duration, nature and type of isolated headaches that affect a patient. In our series, 4/11 isolated headache patients presented with new-onset symptomology. These patients would have qualified for imaging by all the proposed guidelines. The other seven patients had non-acute isolated headaches. In these 7 patients, the duration of the headaches prompted neuroimaging by the referring physician and discovery of their brain tumor. Three of these patients presented with migrainous, unilateral headaches that were without any recent change. If Loder et al.’s and Frishberg et al.’s recommendations had been followed, diagnosis would have been delayed or missed for these 3 of 11 isolated headache patients (3.2% of all brain tumor patients; Table 3). The remaining four patients presented with stable, non-acute headaches and no clear migraine component. Two were suspected to have tension-headache qualities, two were bilateral and one was occipital. No auras, gastrointestinal symptoms, visual disturbances, paresthesias, olfactory symptoms, aphasia or other atypical symptoms were reported in the 11 isolated headache patients. If the American College of Radiology/Consumer Reports recommendations had been followed, a diagnostic delay/error would have occurred for 7 of 11 isolated headache patients (7.4% of all patients). Hence, under the proposed guidelines, neuroimaging may have been delayed or missed in 3–7% of patients with brain tumors.
Table 3.
Potential tumors missed with proposed guidelines
DISCUSSION
Choosing Wisely guidelines are written from a population medicine perspective where only a tiny fraction of patients who present with headaches will have brain tumors on neuroimaging. Conversely, in our experience, one-quarter of brain biopsy patients with brain tumors present with an incidentally-found lesion, non-specific symptoms or headaches alone. The historical review and series in this report serve to illustrate a widespread observation that neurosurgeons frequently treat brain tumors patients who presented with headaches alone, non-specific symptoms or incidentally. Although patients with headaches do not frequently harbor brain tumors, patient with brain tumors frequently present with isolated headaches or minimal symptoms. Therefore, the premise that brain tumors always present with more than headaches is incorrect. Assuming this false premise may lead to medical errors.
Despite the recently published guidelines,6–10 Callaghan et al. report progressive increases in neuroimaging for headaches in the United States.13 Physicians wish to avoid failures in making the correct diagnosis for high-stakes situations, such as a brain tumor diagnosis. Medical providers have likely continued high utilization of neuroimaging for headaches due to concerns over potential missed diagnoses and medical errors, which would adversely affect patient outcomes and, in turn, affect malpractice liability.14 The practice of defensive medicine to reduce medical errors and the subsequent malpractice liability is well described among neurosurgeons, neurologists and general practitioners. For example, to reduce potential medical errors and malpractice liability, 72% of neurosurgeons report ordering additional neuroimaging solely for defensive purposes.15 Nonetheless, the role of defensive medicine on increasing health care costs is under debate as health policy experts and physicians carry contrary views.16 Policy experts argue that tort reform alone will have little effect on health care costs.17 Meanwhile, physicians contend that defensive medicine significantly contributes to snowballing health care costs.18 In regions with tort reform, the risks and costs associated with malpractice have been reduced.19 There is also data to support that malpractice reform reduces excessive medical utilization and defensive medicine.18 The proposed guidelines intersect with medical-error, patient outcome and liability perceptions and realities faced daily by practicing physicians.
One exacerbating factor to this dilemma is the high cost of imaging tests. Outpatient magnetic resonance imaging performed between 2007 and 2010 in the United States cost $7.5 billion.6 The cost of brain computed topography and magnetic resonance imaging to each patient approaches $2,000.20 The cost of medical neuroimaging is complicated by a lack of healthcare price transparency.21 Health care reform will require multi-faceted approach which addresses cost of missed diagnoses, medical-legal expenditures and the relative value of neuroimaging and other diagnostic tests.
Neuroimaging for isolated headaches are typically obtained to rule out a brain tumor. For gliomas and other brain tumors, histology, age, extent of resection and baseline performances status correlate with outcomes.22–27 Early diagnosis allows for prompt treatment, more surgical options and better baseline performance status. This translates to improved outcomes. Here we showed that following the neuroimaging recommendations for isolated headaches would delay or miss diagnosis in 3–7% of brain tumor patients. Therefore, we believe this rate of false-negatives in the evaluation of patients would be detrimental to patients seeking care for headaches.
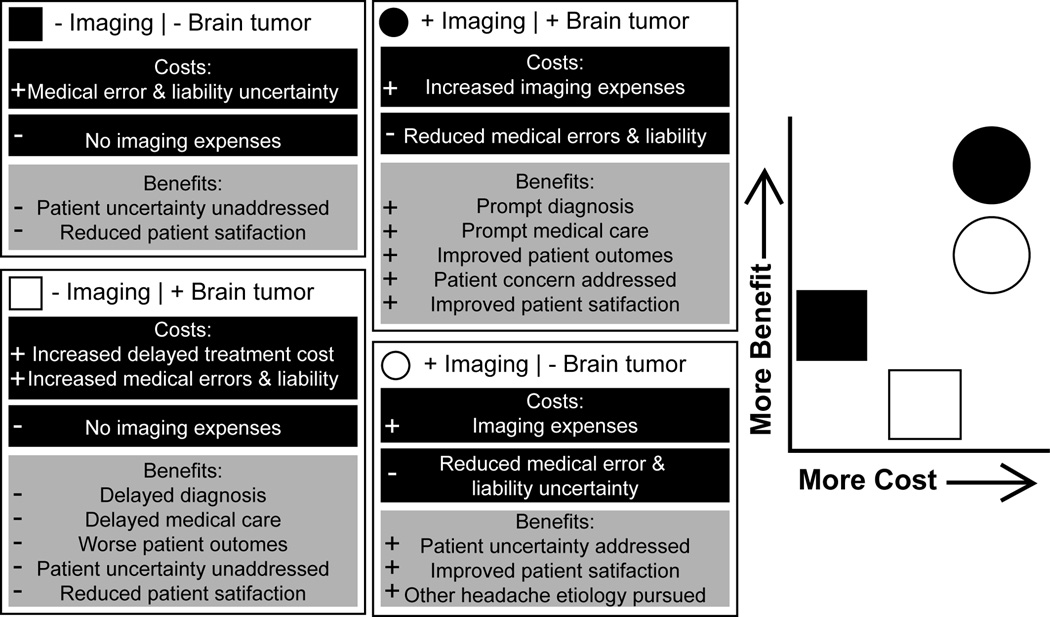
In a dynamic healthcare market, physicians must play a major role in curtailing medical costs. Callaghan et al. have astutely discussed that typical Choosing Wisely® initiatives do not always discuss relative values of tests (i.e. benefit/cost).28 In their analysis, Callaghan et al. evaluate relative values of neuroimaging and electroencephalograms for headaches. They suggest that neuroimaging for headaches should generally be avoided because it provides only slightly more benefit than electroencephalograms at a much higher cost. However, this claim is not consistent with the data presented here, historical data, and the neurosurgeon’s experience. Indeed, neuroimaging is extremely beneficial for patients who have brain tumors because it is the primary means for diagnosis. In addition, there are added costs and benefits that must be discussed when it comes to ordering neuroimaging for headaches. Reduction in medical errors and, in turn, malpractice liability costs are associated with ordering tests. Meanwhile, failure to diagnose a brain tumor due to lack of imaging may increase costs due to delays in treatment. Ordering imaging would allow for prompt diagnosis and care, which are associated with improved outcomes.22–27 There are also less tangible benefits to neuroimaging for headaches that revolve around the fact that a patient has arrived to a physician’s office to address a complaint. Addressing this complaint and acquiescing to requests of discretionary services are associated with higher patient satisfaction.29–31 A patient-centered approach would suggest that there is value in assuring a concerned patient with headaches that he or she does not harbor a brain tumor. Therefore, ordering neuroimaging for headaches would generally address patient uncertainty while improving patient satisfaction. In a patient-centered health care system, we must tailor our decisions for each patient to balance the potential costs and benefits of neuroimaging for headaches (Fig. 2).
Figure 2.
Schematic representation of relative costs and benefits of neuroimaging for a patient with headaches in evaluation of a brain tumor. Increased costs (+), reduced costs (−), increased benefits (+) and reduced benefits (−) are shown for each condition on the left. Generalized patient-tailored cost-benefit schematic is shown on the right. For example, neuroimaging in a headache patient who ultimately does not harbor a brain tumor (bottom right) leads to imaging expenses but reduces perceived costs in medical errors and liability. Benefits for this patient includes addressing patient uncertainty, improved patient satisfaction and rapid pursuit of other headache etiologies.
The ostensible friction between patient-tailored medicine and population medicine initiatives underscores the need for further research to develop guidelines on neuroimaging for headaches. Guidelines must be developed carefully and thoughtfully and must adhere to methodological standards pioneered by those who study clinical decision rules.32–34 Development of a clinical decision tool requires derivation of a model using a wide spectrum of subjects, clearly-defined outcomes, predictors, weights and a large sample size. For this model, failure to diagnose a brain tumor in a headache patient is not desirable; therefore, the model must be weighted to generate an extremely low false-negative rate. The second phase of guideline development is model validation, in which the decision rule is blindly applied to a set of new patients. Our preliminary retrospective evaluation determines that the current models fail to diagnose 27–64% of brain tumor patients with isolated headaches. Finally, the model should be implemented in a clinical trial to assess of impact on use, accuracy, physician acceptability and patient acceptability.32 Based on these standards, the current guidelines have been derived but not completely validated. Hence, the current guidelines constitute Level 4 clinical decision rule criteria,32, 34 which suggest that they require further evaluation before they can be applied clinically. In order to develop accurate and viable guidelines on neuroimaging for headaches, additional resources must be allocated toward evidence-based medicine studies.
CONCLUSION
The debate of neuroimaging for headaches highlights the divide between population-driven healthcare methods and individualized patient-tailored medicine. We support careful and sensible use of neuroimaging where physicians exercise excellent clinical judgment to reduce waste in the medical system. The expectation is that when a patient seeks medical attention for symptoms or an incidentally-found abnormality, he or she will be deliberately and carefully evaluated by a physician. Although we do not recommend routine screening for the general population, we do contend that a substantial number of patients with brain tumors will present with isolated headaches. In addition, a noteworthy number of brain tumor patients will also present with non-specific symptoms or no symptoms. Unvalidated guidelines to prevent neuroimaging in patients with headaches may reduce the perceived global economic burden at the expense of medical errors, delayed diagnoses and inferior outcomes for brain tumor patients. Ultimately, further research is crucial for the development of validated and tested clinical decision rules on neuroimaging for headaches.
Acknowledgments
We thank Drs. Sylvia Awadalla and Christopher Carpenter for helpful discussions and suggestions.
This study was supported by the Department of Neurosurgery at Washington University and grant funding from the National Institutes of Health (T32NS007205-32).
Footnotes
Disclosure: The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
REFERENCES
- 1.Centers for Medicare & Medicaid Services. National Health Expenditures 2012 Highlights 2012. [Accessed 2/4/2014]; [Google Scholar]
- 2.Organization WH. Geneva: World Health Organization; 2011. World Health Statistics 2011. [Google Scholar]
- 3.Rasmussen BK, Jensen R, Schroll M, Olesen J. Epidemiology of headache in a general population--a prevalence study. Journal of clinical epidemiology. 1991;44(11):1147–1157. doi: 10.1016/0895-4356(91)90147-2. [DOI] [PubMed] [Google Scholar]
- 4.Ambulatory Sentinel Practice Network. A study of headache in North American primary care. The Journal of the Royal College of General Practitioners. 1987 Sep;37(302):400–403. [PMC free article] [PubMed] [Google Scholar]
- 5.Evans RW. Diagnostic testing for migraine and other primary headaches. Neurologic clinics. 2009 May;27(2):393–415. doi: 10.1016/j.ncl.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 6.Burke JF, Skolarus LE, Callaghan BC, Kerber KA. Choosing Wisely: highest-cost tests in outpatient neurology. Annals of neurology. 2013 May;73(5):679–683. doi: 10.1002/ana.23865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loder E, Weizenbaum E, Frishberg B, Silberstein S American Headache Society Choosing Wisely Task F. Choosing Wisely in Headache Medicine: The American Headache Society's List of Five Things Physicians and Patients Should Question. Headache. 2013 Nov;53(10):1651–1659. doi: 10.1111/head.12233. [DOI] [PubMed] [Google Scholar]
- 8.American College of Radiology. Choosing Wisely: Five Things Patients and Physicians Should Question. [Accessed 01/07/2014]; [Google Scholar]
- 9.Consumer Reports & ABIM Foundation. Choosing Wisely: Imaging Tests for Headaches. In: foundation CWA, editor. 2012. http://www.choosingwisely.org/doctor-patient-lists/imaging-tests-for-headaches/: Consumer Reports. [Google Scholar]
- 10.Frishberg B, Rosenberg J, Matchar D, et al. Evidence-Based Guidelines in the Primary Care Setting: Neuroimaging in Patients with Nonacute Headache. American Academy of Neurology: US Headache Consortium; http://tools.aan.com/professionals/practice/pdfs/gl0088.pdf. [Google Scholar]
- 11.Forsyth PA, Posner JB. Headaches in patients with brain tumors: a study of 111 patients. Neurology. 1993 Sep;43(9):1678–1683. doi: 10.1212/wnl.43.9.1678. [DOI] [PubMed] [Google Scholar]
- 12.Hawasli AH, Buckley RT, Gao F, et al. Biopsy of the superficial cortex: predictors of effectiveness and outcomes. Neurosurgery. 2013 Aug;73(2):224–231. doi: 10.1227/01.neu.0000430310.63702.3e. discussion 231-222; quiz 232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Callaghan BC, Kerber KA, Pace RJ, Skolarus LE, Burke JF. Headaches and Neuroimaging: High Utilization and Costs Despite Guidelines. JAMA internal medicine. 2014 Mar 17; doi: 10.1001/jamainternmed.2014.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carrier ER, Reschovsky JD, Katz DA, Mello MM. High physician concern about malpractice risk predicts more aggressive diagnostic testing in office-based practice. Health affairs (Project Hope) 2013 Aug;32(8):1383–1391. doi: 10.1377/hlthaff.2013.0233. [DOI] [PubMed] [Google Scholar]
- 15.Nahed BV, Babu MA, Smith TR, Heary RF. Malpractice liability and defensive medicine: a national survey of neurosurgeons. PloS one. 2012;7(6):e39237. doi: 10.1371/journal.pone.0039237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hermer LD, Brody H. Defensive medicine, cost containment, and reform. Journal of general internal medicine. 2010 May;25(5):470–473. doi: 10.1007/s11606-010-1259-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salem O, Forster C. Defensive medicine in general practice: recent trends and the impact of the Civil Liability Act 2002 (NSW) Journal of law and medicine. 2009 Oct;17(2):235–248. [PubMed] [Google Scholar]
- 18.Rubin RJ, Mendelson DN. How much does defensive medicine cost? The Journal of American health policy. 1994 Jul-Aug;4(4):7–15. [PubMed] [Google Scholar]
- 19.Stewart RM, Geoghegan K, Myers JG, et al. Malpractice risk and cost are significantly reduced after tort reform. Journal of the American College of Surgeons. 2011 Apr;212(4):463–467. doi: 10.1016/j.jamcollsurg.2010.12.025. 467.e461-442; discussion 467–469. [DOI] [PubMed] [Google Scholar]
- 20.Sidorov E, Reynolds M, Feng W, Selim M. Healthcare Delivery to Patients with Cerebrovascular Disease: Cost-Minimization Analysis of CT vs. MRI in the Evaluation of Patients with Transient Ischemic Attacks at a Large Academic Center. Neurology. 2012;78 doi: 10.1159/000360521. (Meeting Abstracts 1):P05.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carroll J. No informed consumers without price transparency. Managed care (Langhorne Pa.) 2013 Oct;22(10):17–18. [PubMed] [Google Scholar]
- 22.Auchter RM, Lamond JP, Alexander E, et al. A multiinstitutional outcome and prognostic factor analysis of radiosurgery for resectable single brain metastasis. International journal of radiation oncology, biology, physics. 1996 Apr 1;35(1):27–35. doi: 10.1016/s0360-3016(96)85008-5. [DOI] [PubMed] [Google Scholar]
- 23.Burger PC, Vogel FS, Green SB, Strike TA. Glioblastoma multiforme and anaplastic astrocytoma. Pathologic criteria and prognostic implications. Cancer. 1985 Sep 1;56(5):1106–1111. doi: 10.1002/1097-0142(19850901)56:5<1106::aid-cncr2820560525>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 24.Grant R, Liang BC, Page MA, Crane DL, Greenberg HS, Junck L. Age influences chemotherapy response in astrocytomas. Neurology. 1995 May;45(5):929–933. doi: 10.1212/wnl.45.5.929. [DOI] [PubMed] [Google Scholar]
- 25.Nelson JS, Tsukada Y, Schoenfeld D, Fulling K, Lamarche J, Peress N. Necrosis as a prognostic criterion in malignant supratentorial, astrocytic gliomas. Cancer. 1983 Aug 1;52(3):550–554. doi: 10.1002/1097-0142(19830801)52:3<550::aid-cncr2820520327>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 26.Rosenblum ML, Gerosa M, Dougherty DV, et al. Age-related chemosensitivity of stem cells from human malignant brain tumours. Lancet. 1982 Apr 17;1(8277):885–887. doi: 10.1016/s0140-6736(82)92154-7. [DOI] [PubMed] [Google Scholar]
- 27.Wong ET, Hess KR, Gleason MJ, et al. Outcomes and prognostic factors in recurrent glioma patients enrolled onto phase II clinical trials. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 1999 Aug;17(8):2572–2578. doi: 10.1200/JCO.1999.17.8.2572. [DOI] [PubMed] [Google Scholar]
- 28.Callaghan BC, Burke JF, Feldman EL. How neurologists can choose (even more) wisely: prioritizing waste reduction targets and identifying gaps in knowledge. JAMA : the journal of the American Medical Association. 2014 Apr 23–30;311(16):1607–1608. doi: 10.1001/jama.2014.1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fenton JJ, Jerant AF, Bertakis KD, Franks P. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Archives of internal medicine. 2012 Mar 12;172(5):405–411. doi: 10.1001/archinternmed.2011.1662. [DOI] [PubMed] [Google Scholar]
- 30.Kravitz RL, Epstein RM, Feldman MD, et al. Influence of patients' requests for direct-to-consumer advertised antidepressants: a randomized controlled trial. JAMA : the journal of the American Medical Association. 2005 Apr 27;293(16):1995–2002. doi: 10.1001/jama.293.16.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Macfarlane J, Holmes W, Macfarlane R, Britten N. Influence of patients' expectations on antibiotic management of acute lower respiratory tract illness in general practice: questionnaire study. BMJ (Clinical research ed.) 1997 Nov 8;315(7117):1211–1214. doi: 10.1136/bmj.315.7117.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jesse M, Pines J, Carpenter C, Raja A, Schuur J. Evidence-Based Emergency Care: Diagnostic Testing and Clinical Decision Rules. 2. Chichester, UK: John Wiley & Sons, Ltd; 2013. Clinical Decision Rules; pp. 36–43. [Google Scholar]
- 33.McGinn T, Guyatt G, Wyer P, Naylor CD, Stiell I. Diagnosis: Clinical Prediction Rules. In: Guyatt G, Rennie D, Meade M, Cook D, editors. Users; Guides to the medical liturature. New York, NY: McGraw-Hill Publishing Company; 2002. pp. 471–483. [Google Scholar]
- 34.Stiell IG, Wells GA. Methodologic standards for the development of clinical decision rules in emergency medicine. Annals of emergency medicine. 1999 Apr;33(4):437–447. doi: 10.1016/s0196-0644(99)70309-4. [DOI] [PubMed] [Google Scholar]