Abstract
Objectives.
Sleep problems are common across the adult life span and may exacerbate depressive symptoms and the effect of common risk factors for depressive symptoms such as life stress. We examine sleep disturbance as a moderator of the association between stressful life events and depressive symptoms across five waves (25 years) of the nationally representative, longitudinal American Changing Lives Study.
Method.
The sample includes 3,597 adults aged 25 years or older who were surveyed up to five times over 25 years. Multilevel models were run to examine between- and within-person variability in sleep disturbance and life event stress as predictors of depressive symptoms, and an interaction to test sleep disturbance as a moderator is included in a second step.
Results.
Life events and sleep disturbance were associated with elevated depressive symptoms at the between- and within-person levels. A significant sleep disturbance by interaction of life events was found, indicating that when individuals experienced an above average number of life events and slept more restlessly than usual, they had a higher risk for depressive symptoms than individuals who experienced above average stress but slept well.
Discussion.
Sleeping restfully may allow individuals the rejuvenation needed to manage stress adaptively and reduce depressive symptom burden.
Key Words: Depressive symptoms, Sleep disturbance, Stressful life events
Although insomnia is a major health concern, even in the absence of other medical or psychiatric conditions, disturbed sleep is also considered to be a core contributing factor to the development and expression of major depressive disorder (Baglioni et al., 2011; Maglione et al., 2012). Sleep disturbance may increase risk for depressive symptom onset through its impact on emotion regulation and emotion reactivity, though psychophysiological mechanisms are still being studied (Baglioni, Lombardo, et al., 2010; Baglioni, Spiegelhalder, Lombardo, & Riemann, 2010; Riemann et al., 2010). Although researchers still question the function of sleep, sleep has known implications for attention, memory, alertness, psychomotor performance, mood, and the neuroendocrine stress system, and is generally seen as a restorative and adaptive process (Bonnet & Arand, 2003; Lim & Dinges, 2008; Meerlo, Sgoifo, & Suchecki, 2008).
Moreover, although sleep disturbance is directly and negatively related to mental health, sleep disturbance could compound the effect of other common risk factors on depressive symptoms by reducing the body’s ability to adaptively respond to these stressors (Hamilton, Catley, & Karlson, 2007). Using a nationally representative sample of adults in the United States drawn from the American Changing Lives (ACL) study (House, Kessler, & Herzog, 1990; House, Lantz, & Herd, 2005), we consider restless sleep as a potential moderator of the association between stressful life events and the expression of depressive symptoms. A better understanding of these associations may lead to increased knowledge regarding the way sleep functions to impact mental health and how interventions might best target depressive mood by addressing risk factors such as life stress in combination with sleep disturbance.
It is widely accepted that social stressors, including the experience of stressful life events, are key risk factors, which may precipitate the development of depressive symptoms across the adult life course. Stressful life events are distinct changes in an individual’s life that can challenge the ability to adapt (such as job loss or death of a loved one), may overwhelm mental and physical capacity of individuals, and may lead to psychological distress (George, 2011). Life events can threaten the self and close others bringing about negative feelings in individuals, or they can disrupt an individual’s life and lead to necessary readjustment (Bruce, 2002). Both Blazer (2002) and George (2004) have proposed similar stage models regarding social precursors of mental illnesses, such as major depressive disorder, and stressful life events are included in these models. George’s model presents six stages: demographic variables, early events and achievements, later events and achievements, social integration, vulnerability and protective factors, and provoking agents and coping efforts, with each subsequent stage including factors that are more proximate precursors of mental illness. The final stage of provoking agents and coping efforts includes sudden stressors such as life events. This level in the social precursor model is the most specific and immediate in relating to risk of developing depression relative to the prior stages, which are more general.
In confirmation of this stage model, research has found that individuals may experience a depressive episode for the first time following a severe stressor. For example, response to a significant loss has long been discussed as a primary risk factor for depressive illness (Blazer, 2002). The total number of stressful life events experienced over a period of time has further been associated with increased depressive symptoms (Devanand, Kim, Paykina, & Sackeim, 2002; Kessler, 1997; Kraaij, Arensman, & Spinhoven, 2002). Though most individuals who experience a life event do not subsequently develop more depressive symptoms, most individuals experiencing an episode of depression report the occurrence of a life event closely before their depression onset and report a more negative impact of the event than nondepressed individuals (Devanand et al., 2002; Kessler, 1997). This may pose increasing challenge to mental health with age, as older adults commonly report sleep disturbances and may be exposed to specific types of life events such as bereavement (National Sleep Foundation, 2013). In this analysis, we propose that not sleeping well could magnify the impact of these stressors on mood by preventing the restoration and energy that individuals need to cope and adapt adequately.
Beyond simply assessing whether this proposed association is present for life events in general, we also examine whether a moderating impact of sleep on the association between life stress and depressive symptoms is consistent across distinct domains of life event stress or whether it is specific to particular types of life events. The ACL study measures stressful life events across three domains: violence (victim of a serious attack, robbed/burglarized), interpersonal loss (parent/step-parent died, close friend or relative died, divorce, widowed, child died), and financial strain (involuntarily lost a job for reasons other than retirement, serious financial problems or difficulties). Though single events or domains of events may have more modest associations with depressive symptoms relative to a summed scale of all life events experienced, each of these types of life stress has previously been associated with both increased depressive symptoms and sleep problems in other studies. For example, experiencing violence has been linked to depressive symptoms. High rates of post-traumatic stress disorder, depression, and anxiety have even been found among victims of physical violence up to 8 years following the assault (Johansen, Eilertsen, Nordanger, & Weisaeth, 2013). Prior work, however, found that categories of interpersonal violence were associated with cognitive symptoms of depression in adjusted models but not with somatic symptoms of depression (Hebenstreit, DePrince, & Chu, 2014; Hedtke et al., 2008). Interpersonal violence also has been associated with sleep disturbance. Women who had experienced intimate partner violence, for example, had high prevalence of both insomnia (46%) and nightmares (32%). Insomnia was associated with an almost eightfold increased risk of being depressed in these women who had insomnia compared with assault victims who didn’t have insomnia (Pigeon et al., 2011).
Regarding the second domain of life events, interpersonal loss, bereavement and depressive symptoms have been a common area of study. Bereaved individuals often experience depressive symptoms, though the line between what is considered grief versus depression is still a topic of debate (Jozwiak, Preville, & Vasiliadis, 2013). Zisook and Shuchter (1991) found a 24% prevalence of depression in the 2 months following spousal bereavement with high prevalence continuing over the course of a year. Sleep disturbance is also common among the bereaved. A relative risk for sleep disturbances among a sample of widows was found to be 1.9 (confidence interval: 1.5–2.4) compared with age-matched married women (Valdimarsdóttir, Helgason, Fürst, Adolfsson, & Steineck, 2003). Those experiencing complicated grief, in particular, report poor sleep quality on average (Germain, Caroff, Buysse, & Shear, 2005).
Financial strain is a common stressor across adults who are working and those who are retired. Chronic and perceived financial strain has been found to increase depressive symptoms (Aranda & Lincoln, 2011). In a sample of older adults, Hall and colleagues (2008) found that chronic financial strain was associated with worse wakefulness, sleep efficiency, and sleep latency. After adjusting for mental and physical health covariates in addition to demographic characteristics, however, financial strain remained associated only with poorer sleep efficiency. Clearly, various domains of life event stressors are similarly associated with risk for depressive symptoms and sleep problems. Therefore, we hypothesize that sleep disturbance will act similarly as a moderator across all three of these domains of life events in their association with depressive symptoms.
Finally, although factor analyses suggest that there are distinct dimensions of depressive symptom scales such as the Center for Epidemiological Studies Depression Scale (CES-D; Radloff, 1977), most studies consider depressive symptoms as a unidimensional construct. It may be important, however, to determine whether sleep disturbance and stress are differentially associated with specific aspects of mood. Prior work has found that stressful life events were similarly associated with each of the subdomains of depressive symptoms (Hays et al., 1998). Further, sleep disturbance has consistently been associated with depressive disorders and mood (Baglioni et al., 2011; Maglione et al., 2012). This study builds on prior work by considering whether sleep disturbance moderates the association between life events and each of the subdomains of depressive symptoms: depressive mood, positive affect, interpersonal interaction, and somatic symptoms. In particular, associations with the subdomains of interpersonal interaction and somatic symptoms are less examined. It may be that sleep disturbance, which directly impacts physical health, will magnify the association of stress on somatic symptoms. Likewise, poor sleep may increase the impact of life stressors, altering how individuals perceive their interactions with others who may be supporting or interacting with them during their time of stress. We hypothesize that sleep disturbance will moderate the association between life events and each of the depressive symptom subdomains.
In summary, as sleep is a naturally restorative process with important implications for health, it may be that disturbed sleep strengthens the association of stressful life events with depressive symptoms. If so, improving sleep may reduce fatigue and help individuals better manage or adaptively respond to life stressors and ultimately lead to better mental health. Additionally, limited research has examined within-person trajectories of change involving negative life events and depressive symptoms as the majority of studies utilize cross-sectional data. Between-person analyses can only tell us whether individuals who have more negative life events have more mental health symptoms than individuals with less negative life events. On the other hand, within-person analyses can display whether individuals who experience negative life events subsequently develop more depressive symptoms (George, 2011). Therefore, using a longitudinal multilevel approach that takes advantage of multiple observations for each respondent, we first consider independent associations between sleep disturbance and stressful life events with depressive mood. Although these associations among these constructs are well documented, our longitudinal model extends this research exploring how sleep disturbance and life event stress vary over time and whether individual variation in these factors is associated with changes in depressive symptoms. The main focus of the current study, however, is the potential moderating impact of sleep disruption on the association between stressful life events with depressive symptoms. In additional analyses, we examine whether sleep disruption is also a moderator between three categories of life events—violence, interpersonal loss, and financial strain—and also consider whether sleep disturbance moderates the association between life events and the depressive symptom subdomains—interpersonal interaction, somatic symptoms, depressive mood, and positive affect. We consider these questions of moderation in a nationally representative sample of noninstitutionalized U.S. adults aged 25 and older who were interviewed up to five times over a 25-year period.
Method
Data
Data come from the ACL survey (House et al., 1990; House et al., 2005), a cohort longitudinal study based on a stratified, multistage area probability sample of noninstitutionalized adults aged 25 and older, living in the coterminous United States, and followed over a 25-year period. African Americans and adults aged 60 and older were over sampled. The first wave of the survey was conducted in 1986 with 3,617 adults (68% sample response rate for individuals or 70% for households). Surviving respondents were reinterviewed in 1989 (N = 2,867, 83% of survivors), in 1994 (N = 2,562, 83% of survivors), in 2001/2002 (N = 1,787, 74% of survivors), and again in 2011/2012 (N = 1,427, 81% of survivors). The final analytic sample includes 3,597 participants who completed the CES-D items during at least one wave. A sampling weight is used to adjust for nonresponse and a poststratification adjustment to the 1986 Census estimates of the U.S. population aged 25 years and older to ensure that the sample is representative of the gender, age, and race distribution of the U.S. population living in the United States in 1986 (House et al., 2005).
Measures
The outcome of interest was depressive symptoms measured at each wave with an 11-item short form of the CES-D adapted by Kohout, Berkman, Evans, and Cornoni-Huntley (1993) from Radloff (1977)’s original scale. Kohout’s 11-item scale was found to be reliable and contain the same four-factor solution as the original 20-item scale. In our analyses, the CES-D item on sleep (“my sleep was restless”) was used as a covariate, and thus a mean of the 10 remaining items was used as the measure of depressive symptoms, logged to correct for the positive skew (at least four items must have been responded to for a mean score). The Cronbach’s alpha for our 10-item scale also showed strong reliability across waves ranging from .809 to .847. The 10-item scale contains three depressive affect items (felt depressed, lonely, sad), three somatic items (everything was an effort, could not get going, didn’t feel like eating), two positive affect items (feel happy, enjoy life), and two interpersonal interaction items (people dislike me, were unfriendly). Participants responded on a 1 to 3 scale indicating how frequently the symptom was experienced in the past week (1 = hardly ever, 2 = some of the time, or 3 = most of the time).
The CES-D item “my sleep was restless” was used to indicate disturbed sleep. It was assessed in the same way in each survey wave and showed good variability between and within individuals. Additionally, prior work by the ACL study team found the item to be associated with other predictors in the same way that more detailed measures of sleep were associated with those predictors (Burgard & Ailshire, 2009).
Participants also reported at each survey wave whether they experienced any of the following stressful life events since the previous interview: victim of a serious attack, robbed/burglarized, involuntarily lost a job for reasons other than retirement, serious financial problems or difficulties, parent/step-parent died, close friend or relative died, divorce, widowed, and child died. To account for varying lengths between ACL interview waves, we consider only events that occurred in the prior 2 years to the measurement wave based on participants’ reported year of the event (compared with the date of the interview in which they reported it). Events were summed at each wave for a possible zero to nine events. Events were also summed to compose three domains of events: violence (victim of a serious attack, robbed/burglarized), interpersonal loss (parent/step-parent died, close friend or relative died, divorce, widowed, child died), and financial strain (involuntarily lost a job for reasons other than retirement, serious financial problems or difficulties).
Time-invariant demographic controls were taken from baseline (wave 1) and included participants’ age (in years), gender (female, male), education (years ranging 0 to 17), and race (White, non-White). Additionally, given the comorbidity of sleep problems and other physical health conditions, chronic health conditions and functional ability were included as time-varying controls. To assess chronic health conditions, participants reported whether they experienced any of the following chronic conditions in the past 12 months: hypertension, diabetes, chronic lung disease, heart attack or other heart trouble, stroke, cancer, arthritis, broken or fractured bones, and urinary incontinence. The number of conditions experienced was summed for each participant with a possible zero to nine conditions. Functional ability was assessed with a Gutman-type scale ranging from 1 (most severe functional impairment) to 4 (no impairment or high functional ability). Items incorporated in the scale include being in bed/chair most/all of the day, difficulty bathing by oneself, difficulty climbing stairs, difficulty walking several blocks, and difficulty with heavy housework.
Analysis Plan
We employed multilevel modeling (Littell, Milliken, Stroup, & Wolfinger, 1996; Raudenbush & Bryk, 2002) using SAS PROC MIXED to examine variability in depressive symptoms across participants (person level) and “within” participants across their survey interviews from up to five waves (wave level) conducted over up to 25 years. A benefit of this approach, given the commonality of missing waves of data among individuals in longitudinal measurement, is that multilevel models utilize all waves of data that are available for an individual in the model (Raudenbush & Bryk).
To examine whether restless sleep served as a moderator of the association between life stress and depressive symptoms, interactions between life events and disturbed sleep at both the between- and within-person levels were included. Nonsignificant interactions were trimmed for parsimony in the final model. The model was built in three steps, beginning with the control variables only (Model 1). Next, restless sleep and stressful life events were added at both the between- and within-person levels (Model 2). Predictors at the between-person level were entered as person-specific means (i.e., an individual’s average across five waves) and within-person level predictors were time-varying (i.e., deviations in a given wave from an individual’s own mean across up to five waves) (Hoffman & Stawski, 2009). Finally the focal interactions were added to test for moderation (Model 3). The equation presented below represents the final, trimmed model. Depressive symptoms for the wth wave for the ith person are modeled as:
β1i = γ10
β2i = γ20
β3i = γ30
β4i = γ40
β5i = γ50 (Model 3)
where the intercept (β0i) represents the mean level of depressive symptoms for each individual (averaged across waves). The first slope (β1i) represents the effect of stressful life events occurring in the 2 years prior to wave w (w = 1–5) on the respondent’s depressive symptoms. The second slope parameter (β2i) represents the association of wave w’s restless sleep with depressive symptoms and the third slope parameter (β3i) tests whether the wave-level association between life events and depressive symptoms is moderated by the level of restless sleep. The fourth and fifth slope parameters (β4i, β5i) are within-person level controls for chronic illness burden and functional ability. These covariates reflect deviations from an individual’s own mean and were calculated by centering around the person-mean.
At Level 2, person-mean levels of life events (γ07) and restless sleep (γ08) are entered as between-person covariates predicting the level of depressive symptoms at the intercept (β0i). Each of these covariates indicates an individuals’ average level of that characteristic across waves. Age (γ01), gender (γ02), ethnicity (γ03), education (γ04), chronic illness (γ05), and functional ability (γ06) were also entered as wave-invariant, between-person controls. All models also adjust for a wave indicator variable (w = 1–4). γ10, γ20, γ30, γ40, and γ50 represent the average effects of within-person slopes from Level 1 for life events, restless sleep, the within-person level interaction of restless sleep and life events, chronic illness, and functional ability respectively. γ00 reflects the group mean level of individual depressive symptom levels and u 0i reflects individual deviations from that mean.
Two additional sets of secondary analyses were run. First, life events were categorized into three classes—interpersonal loss, financial difficulty, and violence—and considered as individual predictors of depressive symptoms. Second, the four subdomains of the CES-D, depressive affect, positive affect, somatic symptoms, and interpersonal interaction, were considered as individual outcomes in our model in place of the full CES-D scale to test for differential associations with restless sleep and stressful life events.
Results
Demographic characteristics and summary statistics of key variables across waves are found in Table 1. The average number of life events in the prior 2 years stayed relatively stable across waves, ranging from 0.62 to 0.76 (SD = 0.74–0.86; range 0–5). On average, participants reported a mean restless sleep score of 1.57 to 1.65 (SD = 0.66–0.70; range 1–3) across waves with approximately half of participants reporting experiencing restless sleep some or most of the time. On average, participants reported a mean depressive symptom score of 1.27 to 1.37 (SD = 0.31–0.35; range 1–3) across waves.
Table 1.
Sample Characteristics and Comparison of Key Variables across Waves
| Wave 1 | Wave 2 | Wave 3 | Wave 4 | Wave 5 | |
|---|---|---|---|---|---|
| (1986) | (1989) | (1994) | (2001/2002) | (2011) | |
| Age | |||||
| Mean | 47.11 | ||||
| Range | 24–96 | ||||
| SD | 16.45 | ||||
| Female (%) | 52.9% | ||||
| Education (years) | |||||
| Mean | 12.36 | ||||
| Range | 0–17 | ||||
| SD | 3.14 | ||||
| Non-White (%) | 16.5% | ||||
| Functional ability | N = 3,617 | N = 2,867 | N = 2,559 | N = 1,785 | N = 1,427 |
| Mean | 3.73 | 3.74 | 3.66 | 3.64 | 3.46 |
| Range | 1–4 | 1–4 | 1–4 | 1–4 | 1–4 |
| SD | 0.71 | 0.69 | 0.83 | 0.83 | 1.01 |
| Life events | N = 3,617 | N = 2,867 | N = 2,559 | N = 1,779 | N = 1,422 |
| Mean | 0.73 | 0.76 | 0.63 | 0.64 | 0.62 |
| Range | 0–5 | 0–5 | 0–5 | 0–5 | 0–5 |
| SD | 0.86 | 0.84 | 0.74 | 0.80 | 0.77 |
| Financial problems | N = 3,617 | N = 2,867 | N = 2,557 | N = 1,774 | N = 1,422 |
| Mean | 0.22 | 0.19 | 0.16 | 0.15 | 0.15 |
| Range | 0–2 | 0–2 | 0–2 | 0–2 | 0–2 |
| SD | 0.48 | 0.45 | 0.40 | 0.39 | 0.38 |
| % Reporting event | 18.8 | 16.7 | 14.5 | 13.1 | 13.8 |
| Violence | N = 3,617 | N = 2,867 | N = 2,559 | N = 1,775 | N = 1,422 |
| Mean | 0.12 | 0.09 | 0.06 | 0.05 | 0.04 |
| Range | 0–2 | 0–2 | 0–2 | 0–2 | 0–2 |
| SD | 0.34 | 0.30 | 0.25 | 0.23 | 0.21 |
| % Reporting event | 11.3 | 8.9 | 5.7 | 4.9 | 3.5 |
| Interpersonal loss | N = 3,617 | N = 2,867 | N = 2,559 | N = 1,779 | N = 1,422 |
| Mean | 0.39 | 0.48 | 0.41 | 0.45 | 0.43 |
| Range | 0–3 | 0–3 | 0–3 | 0–3 | 0–3 |
| SD | 0.55 | 0.58 | 0.55 | 0.60 | 0.58 |
| % Reporting event | 36.2 | 43.6 | 37.9 | 39.4 | 40.0 |
| Chronic illness | N = 3,617 | N = 2,867 | N = 2,559 | N = 1,785 | N = 1,423 |
| Mean | 0.78 | 0.80 | 0.96 | 1.22 | 1.28 |
| Range | 0–6 | 0–8 | 0–7 | 0–7 | 0–7 |
| SD | 1.05 | 1.08 | 1.13 | 1.22 | 1.18 |
| CESD-D 10 | N = 3,605 | N = 2,859 | N = 2,394 | N = 1,682 | N = 1,316 |
| Mean | 1.37 | 1.34 | 1.28 | 1.27 | 1.28 |
| Range | 1–2.90 | 1–2.9 | 1–3 | 1–2.8 | 1–3 |
| SD | 0.35 | 0.34 | 0.32 | 0.31 | 0.34 |
| Restless sleep | N = 3,585 | N = 2,852 | N = 2,390 | N = 1,682 | N = 1,316 |
| Mean | 1.65 | 1.61 | 1.57 | 1.62 | 1.59 |
| Range | 1–3 | 1–3 | 1–3 | 1–3 | 1–3 |
| SD | 0.70 | 0.66 | 0.70 | 0.70 | 0.69 |
Note. Descriptive statistics are weighted. CES-D = Center for Epidemiological Studies Depression Scale.
An intraclass correlation for depressive symptoms revealed that 44% of the variance in depressive symptoms is between-person (across respondents) and 56% is within-person (for the same person, across survey waves) (Model 0). Significant variability at both levels provides justification for the multilevel modeling approach. Results from our two-level multilevel model are displayed with coefficients and standard errors in Table 2. In Model 1, person-level covariate adjustments revealed that individuals who were younger (γ01; B = −0.001, p < .001), female (γ02; B = 0.008, p < .01), non-White (γ03; B = 0.026, p < .001), less educated (γ04; B = −0.005, p < .001), suffering from more chronic health conditions (γ05; B = 0.011, p < .001), and with poorer functional ability (γ06; B = −0.039, p < .001) reported more depressive symptoms. In addition, wave-level covariates also showed significant associations, such that a wave when an individual had more than their average number of chronic health conditions (γ04; B = 0.005, p < .001) and a wave when an individual had below average levels of functional ability (indicating greater functional limitations; γ04; B = −0.021, p < .001) were associated with more depressive symptoms.
Table 2.
Two-level Multilevel Model of Demographic Characteristics, Sleep Disturbance, Life Events, and Chronic Illness on Depressive Symptoms (Model 1)
| Depressive mood | ||||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||
| B | (SE) | B | (SE) | B | (SE) | |
| Fixed effects | ||||||
| Intercept, γ00 | 0.338*** | (0.013) | 0.141*** | (0.013) | 0.141*** | (0.013) |
| Within-person covariatesa | ||||||
| Life events, γ10 | — | — | 0.006*** | (0.001) | 0.006*** | (0.001) |
| Restless sleep, γ20 | — | — | 0.034*** | (0.001) | 0.034*** | (0.001) |
| Life events * Restless Sleep, γ30 | — | — | — | — | 0.007** | (0.002) |
| Chronic illness, γ40 | 0.005*** | (0.001) | 0.003* | (0.001) | 0.003* | (0.001) |
| Functional ability, γ50 | −0.021*** | (0.001) | −0.018*** | (0.001) | −0.018*** | (0.001) |
| Between-person covariatesb | ||||||
| Age, γ01 | −0.001*** | (0.000) | −0.001*** | (0.000) | −0.001*** | (0.000) |
| Gender, γ02 | 0.008** | (0.003) | 0.005* | (0.002) | 0.005* | (0.002) |
| Ethnicity, γ03 | 0.026*** | (0.003) | 0.025*** | (0.003) | 0.025*** | (0.003) |
| Education, γ04 | −0.005*** | (0.001) | −0.004*** | (0.000) | −0.004*** | (0.000) |
| Chronic illness, γ05 | 0.011*** | (0.002) | 0.003* | (0.001) | 0.003 | (0.002) |
| Functional ability, γ06 | −0.039*** | (0.002) | −0.026*** | (0.002) | −0.026*** | (0.002) |
| Life events, γ07 | — | — | 0.016*** | (0.002) | 0.016*** | (0.002) |
| Restless sleep, γ08 | — | — | 0.068*** | (0.002) | 0.068*** | (0.002) |
| Random effects | ||||||
| Intercept, | 0.003*** | (0.000) | 0.002*** | (0.000) | 0.002*** | (0.000) |
| Residual, | 0.006*** | (0.000) | 0.005*** | (0.000) | 0.005*** | (0.000) |
| −2 Log likelihood | −21355.1 | −22735.8.2 | −22736.0 | |||
Notes. All models adjust for a wave indicator variable where w = 1–4. Step 1: Participant N = 3,605, Observation N = 11,833; Steps 2 and 3: Participant N = 3,597, Observation N = 11,791.
aPerson-mean centered scores (i.e., time-varying).
bPerson-mean across waves (i.e., time-invariant).
*p < .05. **p < .01. ***p < .001.
In Model 2, we tested between- and within-person associations between stressful life events and restless sleep with depressive symptoms. At the wave level, respondents reported more depressive symptoms at waves when they reported more recent life events (γ10; B = 0.006, p < .001) or more restless sleep (γ20; B = 0.034, p < .001) than their average levels. Turning to the person-level findings, individuals who on average experienced more life events (γ07; B = 0.016, p < .001) or reported more restless sleep (γ08; B = 0.068, p < .001) expressed more depressive symptoms.
Finally, Model 3 included interactions at both the between- and within-person levels to test whether sleep moderated the effect of life events on depressive symptoms. The between-person level interaction was not significant and was trimmed for parsimony of the model. However, the within-person level interaction was significant, showing that sleep influenced the strength of the association between stressful life events and depressive symptoms (γ30: B = 0.007, p < .01). At waves when individuals experienced above average life events and slept more restlessly than usual (γ30), they had a higher risk for depressive symptoms. A visual display of the interaction can be found in Figure 1. Figure 1 shows that experiencing a wave with above average stress was only associated with increased depressive symptoms if it coincided with a wave of above average restless sleep. Thus even if individuals had experienced more stressful life events in the recent past than was typical for them, they weren’t at increased risk of depressive symptoms unless they were also sleeping poorly at the time of that interview wave.
Figure 1.
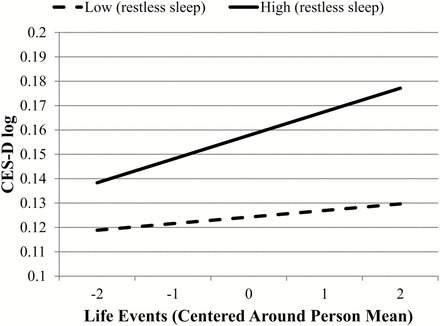
Wave-specific variation in restless sleep as a significant moderator of the stressful life events and depressive symptoms association (wave-level interaction, γ30). High and low restless sleep indicating 1 SD above and below the within-person level mean. Depressive symptoms are logged to adjust for skew. Life events are centered around the individual’s mean such that 0 indicates the mean, positive numbers indicate above average number of experienced events, and negative numbers indicate a below average number of experienced events.
Additional Analyses
To consider whether each class of life events had similar associations with depressive symptoms and was similarly moderated by sleep disturbance, we ran three additional models replacing the summed life events measure with the summed measure for the three classes of life events, one at a time: interpersonal loss, financial difficulty, and violence. In this way, we are able to determine whether the summed life events measure is not solely representing a large effect of one class but has a similar association with each type of life events. We found similar results for all three dimensions to our full life events model. Sleep disturbance significantly moderated the association between interpersonal loss and depressive symptoms at the within-person level (B = 0.008, p < .05). Sleep disturbance significantly moderated financial difficulties at the between-person level (B = 0.015, p < .05) and finally violence at the within-person level (B = 0.015, p < .05). Therefore, restless sleep carried a similar moderating impact regardless of stressor domain.
Finally, the four subdomains of the CES-D scale (depressive affect, positive affect, somatic symptoms, and interpersonal interaction) were also considered as separate outcome measures in place of the full CES-D. A similar pattern of results was found for both depressive affect and positive affect subdomain scales as those reported earlier for Model 3. A significant within-person interaction showed that sleep moderated the association between life events and the depressive affect subdomain scale (B = 0.009, p < .01) and the positive affect scale at both the within- (B = −0.007, p < .01) and between-person levels (B = −0.013, p < .01). Although more life events and sleep disturbance at both the between- and within-person level were associated positively with the somatic symptoms subdomain scale, a sleep-by-life events interaction was not significant for this subdomain (within-person level: B = 0.004, p = .19; between-person level: B = −0.000, p = .95). Finally, sleep disturbance was associated positively with the interpersonal interaction subdomain scale at the between- and within-person levels but life events were not. (Thus a sleep-by-life events interaction was not significant for the interpersonal interaction subdomain; within-person level: B = 0.002, p = .51; between-person level: B = 0.004, p = .42)
Discussion
In this nationally representative, longitudinal sample of U.S. adults, findings indicate that the stress–mood relationship was strongest at poor levels of sleep. Consistent with existing work (Devanand et al., 2002; Kessler, 1997; Kraaij et al., 2002), stressful life events were associated with higher levels of depressive symptoms, and a time when individuals were experiencing above average levels of stress was also associated with more depressive symptoms. Similarly, restless sleep was associated with more depressive symptoms, and times when individuals reported worse sleep than was typical for them were associated with increased depressive symptoms. We uniquely find that variability over time in stress and sleep, and not just the average level of these factors, appeared to be related to depressive symptoms.
In addition, we found a significant interaction between stressful life events and restless sleep at the within-person level showing that restless sleep strengthens the association between life events and depressive symptoms. In other words, those experiencing stress above what is typical for them are at particular risk for elevated depressive symptoms if they are sleeping more restlessly than usual. Sleeping restfully may therefore be allowing individuals the rejuvenation needed to manage their stress adaptively. Further, this association shows that stressors and risk factors may not always act independently of one another, and intervening on one risk factor, such as sleep disturbance, may have a positive impact on the entire pathway of biopsychosocial risk to depressive symptoms.
It is important to keep in mind, however, that the associations found in this analysis cannot be interpreted as causal and other interpretations of our findings are possible. Disturbed sleep is a risk factor for developing depressive mood but also an established symptom and indicator of the severity of major depressive disorder (Baglioni et al., 2011; Maglione et al., 2012). Sleep disturbance may result from depressive mood and negative feelings associated with the occurrence of a life event, as opposed to leading to depressive mood, as we have proposed here. Indeed, prior work has identified a bidirectional association between insomnia and depressive mood (Jansson-Fröjmark & Lindblom, 2008). Nonetheless, sleep disturbance during periods of life stress is clearly associated with depressive symptoms. Although negative life events (e.g., widowhood) may not be preventable, it is possible to modify and improve one’s sleep, which may improve both mood and levels of stress.
Our study supports prior work finding a cumulative impact of life stress (Devanand et al., 2002; Kessler, 1997; Kraaij et al., 2002); and also that specific domains of life stressors (violence, finance, and interpersonal loss) are individually associated with increased depressive symptoms (Brown & Harris, 1989; Dohrenwend & Dohrenwend, 1974; McGonagle & Kessler, 1990). Restless sleep was a significant moderator across these domains of life stress and thus impacts ability to cope regardless of the type of stress being encountered. Consequently, sleep disturbance or health might be considered as an indicator differentiating individuals in terms of resilience or reserve in the face of stress. Future research may consider adaptive sleep behaviors, in addition to other emotional and physical health factors or coping mechanisms, as an indicator of successful aging, psychosocial and physical health.
In addition, the pattern of results is largely consistent in magnitude and direction of associations across subdomains of depressive symptoms. Though a life event by restless sleep interaction was only found in association with depressive affect and positive affect, results may be affected by issues of power due to slicing the outcome measure into its subdomains: depressive mood, positive affect, interpersonal interaction, and somatic symptoms. However, sizeable differences in the magnitude of the interaction coefficients across the significant and insignificant interactions lead us to believe that there may be nuanced differences in associations between sleep, life events, and depressive symptoms subdomains. Both stress and sleep disturbance have been linked with mood in a large body of prior research, and our results also show significant associations linking life events and sleep disturbance, as well as a life event by sleep disturbance interaction, with the depressive symptom subdomains of depressive mood and positive affect. Prior work is mixed, however, regarding the association between stressful life events and interpersonal interaction (Hays et al., 1998; Krause, 1986). In our analyses, we do not find a significant main effect of life events in models predicting this subdomain of the CES-D, nor do we find an interaction between life events and sleep in predicting the interpersonal interaction subdomain. The interpersonal interaction subdomain captures perceptions of others’ negative interactions with the respondent, and it may be that life events which might result in negative, internal self-perceptions, such as divorce or unintended loss of a job, may have a different impact than, for example, being robbed or the death of a loved one, with these latter events less likely to elicit self-blame. Indeed, classic attributional theory suggests that depression is associated with internal attributions of negative events (Abramson, Seligman, & Teasdale, 1978), leading us to expect a stronger association with the interpersonal interaction subdomain. Finally, it is surprising that although both sleep and life events were independently associated with the somatic symptoms subdomain of the CES-D in our results, poor sleep didn’t magnify the impact of stress on this subdomain. It appears that sleep drives the association with somatic symptoms independent of the experience of stress. Future work should further explore the nuances of the associations between stressful life events, sleep, and subdomains of the CES-D.
As a caveat, our sample was representative of the U.S. population and thus levels of depressive symptoms were generally very low among ACL respondents. Findings may apply to subclinical variations in mood but may not inform risk for depressive illness. Prior work has shown, however, that even minor or subsyndromal symptoms of depression are associated with a host of negative outcomes including problems with physical functioning, greater disability, poorer self-rated health, high health service use, high absenteeism from work responsibilities, poor perceived quality of life, and more suicidal ideations (Beekman, Deeg, Braam, Smit, & Van Tilburg, 1997; Blazer, 2003; Meeks, Vahia, Lavretsky, Kulkarni, & Jeste, 2011). Therefore, increases in depressive symptoms are important to consider even in a community-based and nonclinical sample, and interventions targeting sleep disturbance may be useful across the range of depressive symptomatology. However, replication of these findings in clinical and noncommunity-based samples would be useful.
Limitations
Due to the longitudinal nature of the ACL study that followed individuals over 25 years and covered a broad scope of psychological, social, and behavioral factors that are associated with health, condensed measures were used so as not to burden participants. Therefore, a shortened and nonstandardized version of the CES-D was included as the primary outcome measure of depressive symptoms. Given the nature of this scale, we cannot make assumptions about major depressive disorder but rather assessed depressive symptomatology. However, the shortened scale we used includes items from all four originally identified dimensions (negative affect, positive affect, somatization, and interpersonal relations) of depressive symptoms and showed strong reliability across study waves (Radloff, 1977). Additionally, though it has been used to assess sleep in prior studies and showed good variability both between and within individuals over time (Burgard & Ailshire, 2009; Kutner, Bliwise, Brogan, & Zhang, 2001), the CES-D sleep item, “my sleep was restless,” was the only sleep item collected at all study waves. Future studies should consider validated subjective and objective measures of sleep. The ACL study did not assess a full range of stressful live events, only the three dimensions included: interpersonal loss, financial difficulty, and violence, nor did it assess the severity of the life events. As severity may have an impact on sleep and mood, future work should consider this question. In spite of these limitations, our study has the major advantage of a large, nationally representative sample of the U.S. population and considers associations spanning up to 25 years.
Implications and Future Directions
In this study, we demonstrate the importance of sleeping well, not just as an independent predictor of depressive symptoms but as a moderator of the stress–mood association. Poor sleep has the ability to compound the effects of stress, whereas sleeping well can protect individuals from increased depressive symptomatology and help them respond to life stress more adaptively. When adults are undergoing stressful experiences such as the loss of a loved one or unemployment, taking steps to improve one’s sleep may benefit both physical and mental health. Morin, LeBlanc, Daley, Gregoire, and Mérette (2006) found the majority of individuals reporting insomnia did not seek help from a health care provider for their sleep difficulties. However, over the counter sleep aids are commonly used among adults and particularly among older adults (Johnson, Roehrs, Roth, & Breslau, 1998; Kantar Health, 2013). Concerns surround extended use of these aids, however, given their anticholinergic effects and potential risk for falls or accidents. Given sleep’s independent and multiplicative effects on physical and mental health, when sleep problems occur in the face of stressful life events, working with a health care provider to determine appropriate coping techniques for dealing with stress, and behavioral modifications (such as sleep hygiene changes or Cognitive Behavioral Therapy for Insomnia; CBT-I) or safe sleep treatments for sleep disturbance, may result in individual and public health benefit.
Funding
This work was supported by the National Institute on Aging (R01AG018418), Department of Veterans Affairs (IIR 10-176) to K. Zivin and the National Institute of Mental Health (T32 MH073553) to A. Leggett.
Acknowledgments
A. Leggett was responsible for the development of the hypothesis, writing the manuscript, and running all analyses. S. Burgard was responsible for assisting in development of the hypothesis and editing the manuscript. K. Zivin was responsible for assisting in development of the hypothesis and editing the manuscript.
References
- Abramson L. Y. Seligman M. E., & Teasdale J. D (1978). Learned helplessness in humans: Critique and reformulation. Journal of Abnormal Psychology, 87, 49–74. doi:10.1037/0021-843X.87.1.49 [PubMed] [Google Scholar]
- Aranda M. P., & Lincoln K. D (2011). Financial strain, negative interaction, coping styles, and mental health among low-income latinos. Race and Social Problems, 3, 280–297. doi:10.1007/s12552-011-9060-4 [Google Scholar]
- Baglioni C. Battagliese G. Feige B. Spiegelhalder K. Nissen C. Voderholzer U. … Riemann D (2011). Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. Journal of Affective Disorders, 135, 10–19. doi:10.1016/j.jad.2011.01.011 [DOI] [PubMed] [Google Scholar]
- Baglioni C. Lombardo C. Bux E. Hansen S. Salveta C. Biello S. … Espie C. A (2010). Psychophysiological reactivity to sleep-related emotional stimuli in primary insomnia. Behaviour Research and Therapy, 48, 467–475. doi:10.1016/j.brat.2010.01.008 [DOI] [PubMed] [Google Scholar]
- Baglioni C., Spiegelhalder K., Lombardo C., Riemann D. (2010). Sleep and emotions: A focus on insomnia. Sleep Medicine Reviews, 14, 227–238. doi:10.1016/j.smrv.2009.10.007 [DOI] [PubMed] [Google Scholar]
- Beekman A. T. Deeg D. J. Braam A. W. Smit J. H., & Van Tilburg W (1997). Consequences of major and minor depression in later life: A study of disability, well-being and service utilization. Psychological Medicine, 27, 1397–1409. doi:10.1017/S0033291797005734 [DOI] [PubMed] [Google Scholar]
- Blazer D. (2002). Depression in late life. New York: Springer Publishing Company. [Google Scholar]
- Blazer D. G. (2003). Depression in late life: Review and commentary. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 58, 249–265. doi:10.1176/foc.7.1.foc118 [DOI] [PubMed] [Google Scholar]
- Bonnet M. H., & Arand D. L (2003). Clinical effects of sleep fragmentation versus sleep deprivation. Sleep Medicine Reviews, 7, 297–310. doi:10.1053/smrv.2001.0245 [DOI] [PubMed] [Google Scholar]
- Brown G. W., & Harris T. O (1989). Depression. In T. O., Harris, G. W., Brown (Eds.), Life events and illness. New York, NY: Guilford Press. [Google Scholar]
- Bruce M. L. (2002). Psychosocial risk factors for depressive disorders in late life. Biological Psychiatry, 52, 175–184. doi:10.1016/S0006-3223(02)01410-5 [DOI] [PubMed] [Google Scholar]
- Burgard S. A., & Ailshire J. A (2009). Putting work to bed: Stressful experiences on the job and sleep quality. Journal of Health and Social Behavior, 50, 476–492. doi:10.2307/20617656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devanand D. P. Kim M. K. Paykina N., & Sackeim H. A (2002). Adverse life events in elderly patients with major depression or dysthymic disorder and in healthy-control subjects. The American Journal of Geriatric Psychiatry, 10, 265–274. doi:10.1097/00019442-200205000-00005 [PubMed] [Google Scholar]
- Dohrenwend B. S., & Dohrenwend B. P (1974). Stressful life events: Their nature and effects. Oxford, UK: John Wiley & Sons. [Google Scholar]
- George L. K. (2004). Social and economic factors related to psychiatric disorders in late life In D. G.Blazer D. C. Steffens, & E. W.Busse (Eds.), Textbook of geriatric psychiatry (pp. 139–161). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- George L. K.(Ed.). (2011). Social factors, depression, and aging (7th ed). London: Elsevier. [Google Scholar]
- Germain A., Caroff K., Buysse D. J., Shear M. K. (2005). Sleep quality in complicated grief. Journal of Traumatic Stress, 18, 343–346. doi:10.1002/jts.20035 [DOI] [PubMed] [Google Scholar]
- Hall M., Buysse D. J., Nofzinger E. A., Reynolds C. F., 3rd, Thompson W., Mazumdar S., Monk T. H. (2008). Financial strain is a significant correlate of sleep continuity disturbances in late-life. Biological Psychology, 77, 217–222. doi:10.1016/j.biopsycho.2007.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton N. A. Catley D., & Karlson C (2007). Sleep and the affective response to stress and pain. Health Psychology, 26, 288–295. doi:10.1037/0278-6133.26.3.288 [DOI] [PubMed] [Google Scholar]
- Hays J. C. Landerman L. R. George L. K. Flint E. P. Koenig H. G. Land K. C., & Blazer D. G (1998). Social correlates of the dimensions of depression in the elderly. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 53, 31–39. doi:10.1093/geronb/53B.1.P31 [DOI] [PubMed] [Google Scholar]
- Hebenstreit C. L. DePrince A. P., & Chu A. T (2014). Interpersonal violence, depression, and executive function. Journal of Aggression, Maltreatment & Trauma, 23, 168–187. doi:10.1080/10926771.2014.872749 [Google Scholar]
- Hedtke K. A., Ruggiero K. J., Fitzgerald M. M., Zinzow H. M., Saunders B. E., Resnick H. S., Kilpatrick D. G. (2008). A longitudinal investigation of interpersonal violence in relation to mental health and substance use. Journal of Consulting and Clinical Psychology, 76, 633–647. doi:10.1037/0022-006X.76.4.633 [DOI] [PubMed] [Google Scholar]
- Hoffman L., & Stawski R (2009). Persons as contexts: Evaluating between-person and within-person effects in longitudinal analysis. Research in Human Development, 6, 97–120. doi:10.1080/15427600902911189 [Google Scholar]
- House J. S. Kessler R. C., & Herzog A. R (1990). Age, socioeconomic status, and health. The Milbank Quarterly, 68, 383–411. doi:10.2307/3350111 [PubMed] [Google Scholar]
- House J. S. Lantz P. M., & Herd P (2005). Continuity and change in the social stratification of aging and health over the life course: Evidence from a nationally representative longitudinal study from 1986 to 2001/2002 (Americans’ Changing Lives Study). The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60, 15–26. doi:10.1093/geronb/60.Special_Issue_2.S15 [DOI] [PubMed] [Google Scholar]
- Jansson-Fröjmark M., Lindblom K. (2008). A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. Journal of Psychosomatic Research, 64, 443–449. doi:10.1016/j.jpsychores.2007.10.016 [DOI] [PubMed] [Google Scholar]
- Johansen V. A., Eilertsen D. E., Nordanger D., Weisaeth L. (2013). Prevalence, comorbidity and stability of post-traumatic stress disorder and anxiety and depression symptoms after exposure to physical assault: An 8-year prospective longitudinal study. Nordic Journal of Psychiatry, 67, 69–80. doi:10.3109/08039488.2012.732112 [DOI] [PubMed] [Google Scholar]
- Johnson E. O., Roehrs T., Roth T., Breslau N. (1998). Epidemiology of alcohol and medication as aids to sleep in early adulthood. Sleep, 21, 178–186. [DOI] [PubMed] [Google Scholar]
- Jozwiak N., Preville M., Vasiliadis H. M. (2013). Bereavement-related depression in the older adult population: A distinct disorder? Journal of Affective Disorders, 151, 1083–1089. doi:10.1016/j.jad.2013.08.038 [DOI] [PubMed] [Google Scholar]
- Kantar Health. (March 2013). National Health and Wellness Survey. Princeton, NJ. [Google Scholar]
- Kessler R. C. (1997). The effects of stressful life events on depression. Annual Review of Psychology, 48, 191–214. doi:10.1146/annurev.psych.48.1.191 [DOI] [PubMed] [Google Scholar]
- Kohout, F. J., Berkman, L. F., Evans, D. A., & Cornoni-Huntley, J. (1993). Two Shorter Forms of the CES-D Depression Symptoms Index. Journal of Aging and Health, 5, 179–193. doi:10.1177/089826439300500202 [DOI] [PubMed] [Google Scholar]
- Kraaij V. Arensman E., & Spinhoven P (2002). Negative life events and depression in elderly persons: A meta-analysis. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 57, 87–94. doi:10.1093/geronb/57.1.P87 [DOI] [PubMed] [Google Scholar]
- Krause N. (1986). Social support, stress, and well-being among older adults. Journal of Gerontology, 41, 512–519. doi:10.1093/geronj/41.4.512 [DOI] [PubMed] [Google Scholar]
- Kutner N. G. Bliwise D. L. Brogan D., & Zhang R (2001). Race and restless sleep complaint in older chronic dialysis patients and nondialysis community controls. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 56, 170–175. doi:10.1093/geronb/56.3.P170 [DOI] [PubMed] [Google Scholar]
- Lim J., Dinges D. F. (2008). Sleep deprivation and vigilant attention. Annals of the New York Academy of Sciences, 1129, 305–322. doi:10.1196/annals.1417.002 [DOI] [PubMed] [Google Scholar]
- Littell R. C. Milliken G. A. Stroup W. W., & Wolfinger R. D (1996). SAS system for mixed models. Cary, NC: SAS Institute. [Google Scholar]
- Maglione J. E., Ancoli-Israel S., Peters K. W., Paudel M. L., Yaffe K., Ensrud K. E., Stone K. L. (2012). Depressive symptoms and subjective and objective sleep in community-dwelling older women. Journal of the American Geriatrics Society, 60, 635–643. doi:10.1111/j.1532-5415.2012.03908.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGonagle K., & Kessler R (1990). Chronic stress, acute stress, and depressive symptoms. American Journal of Community Psychology, 18, 681–706. doi:10.1007/BF00931237 [DOI] [PubMed] [Google Scholar]
- Meeks T. W., Vahia I. V., Lavretsky H., Kulkarni G., Jeste D. V. (2011). A tune in “a minor” can “b major”: A review of epidemiology, illness course, and public health implications of subthreshold depression in older adults. Journal of Affective Disorders, 129, 126–142. doi:10.1016/j.jad.2010.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meerlo P., Sgoifo A., Suchecki D. (2008). Restricted and disrupted sleep: Effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep Medicine Reviews, 12, 197–210. doi:10.1016/j.smrv.2007.07.007 [DOI] [PubMed] [Google Scholar]
- Morin C. M. LeBlanc M. Daley M. Gregoire J. P., & Mérette C (2006). Epidemiology of insomnia: Prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Medicine, 7, 123–130. doi:10.1016/j.sleep.2005.08.008 [DOI] [PubMed] [Google Scholar]
- National Sleep Foundation. (2013). Aging and sleep. Retrieved from http://www.sleepfoundation.org/article/sleep-topics/aging-and-sleep
- Pigeon W. R., Cerulli C., Richards H., He H., Perlis M., Caine E. (2011). Sleep disturbances and their association with mental health among women exposed to intimate partner violence. Journal of Women’s Health (2002), 20, 1923–1929. doi:10.1089/jwh.2011.2781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi:10.1177/014662167700100306 [Google Scholar]
- Raudenbush S. W., & Bryk A. S (2002). Hierarchical linear models: Applications and data analysis methods (2nd ed). London, UK: Sage. [Google Scholar]
- Riemann D. Spiegelhalder K. Feige B. Voderholzer U. Berger M. Perlis M., & Nissen C (2010). The hyperarousal model of insomnia: A review of the concept and its evidence. Sleep Medicine Reviews, 14, 19–31. doi:10.1016/j.smrv.2009.04.002 [DOI] [PubMed] [Google Scholar]
- Valdimarsdóttir U. Helgason Á. R. Fürst C.-J. Adolfsson J., & Steineck G (2003). Long-term effects of widowhood after terminal cancer: A Swedish nationwide follow-up. Scandinavian Journal of Public Health, 31, 31–36. doi:10.1080/14034940210165109 [DOI] [PubMed] [Google Scholar]
- Zisook S., & Shuchter S (1991). Depression through the first year after the death of a spouse. American Journal of Psychiatry, 148, 1346–1352. doi:10.1176/ajp.148.10.1346 [DOI] [PubMed] [Google Scholar]


