Abstract
Purpose:
We examined the prevalence and correlates of unmet assistance need with respect to activities of daily living (ADLs) and instrumental activities of daily living (IADLs) among older American Indians.
Design and Methods:
Data for our analyses were collected in 2006–2008 as part of the Native Elder Care Study, a cross-sectional study of community-dwelling American Indians aged ≥55 years. In-person interviewer-administered surveys were used to collect data on demographic characteristics, physical functioning, mental and physical health, personal assistance needs, and psychosocial resources.
Results:
Among those with an assistance need, 47.8% reported an unmet need with one or more ADLs or IADLs. Significant adjusted correlates of unmet assistance need included greater number of ADL and IADL difficulties and lower levels of social support.
Implications:
Initiatives and programs aimed at increasing social support and augmenting informal care networks can support efforts to meet American Indian adults’ personal assistance needs.
Key Words: American Indians, Functional disability, Unmet assistance need, Social support
In 2011, approximately 22.7 million (62%) of community-dwelling older adults in the United States aged ≥65 years had at least one basic functional disability (National Center for Health Statistics, 2013). Assessment of difficulties in performing activities of daily living (ADL) and instrumental activities of daily living (IADL) can identify functional disability and can be used to determine whether persons with such disability are relying on personal assistance or assistive devices (Agree & Freedman, 2003; Diwan & Moriarty, 1995). ADLs include a variety of basic self-care activities, and difficulty performing ADLs usually suggests that persons are burdened by more severe physical and/or cognitive disabilities. Still, persons with milder disabilities may only have difficulties in performing IADLs, which include tasks such as managing finances, preparing meals, shopping, and taking medications as prescribed.
Unmet assistance need is a lack of or insufficient amount of assistance from either a person or an assistive device when there is a need to perform ADLs and/or IADLs (Desai, Lentzner, & Weeks, 2001; Diwan & Moriarty, 1995). Research has identified several factors associated with an increased risk for unmet assistance need among adults including greater number of ADL limitations, greater morbidity, dementia, lower income, younger age, and living alone (Allen & Mor, 1997, Desai et al., 2001; Kennedy, 2001; LaPlante, Kaye, Kang, & Harrington, 2004; Lima & Allen, 2001; Newcomer, Kang, LaPlante, & Kaye, 2005; Sands et al., 2006; Williams, Lyons, & Rowland, 1997).
Racial and ethnic minorities are particularly at risk for having an unmet assistance need (Kennedy, 2001; LaPlante et al., 2004). Data from the 1994 and 1995 National Health Interview Surveys indicated a substantively higher prevalence and significantly increased odds of unmet assistance need among minority adults aged ≥18 years compared with their same-aged white counterparts. Specifically, Hispanics and African Americans had 1.5 and 1.9, respectively, greater odds of having either an unmet assistance need compared with whites (Kennedy, 2001). Examination of more recent National Health Interview Survey data found a substantially greater unmet ADL and IADL assistance need among African American, Hispanic, and Other Race adults compared with same-aged whites (LaPlante et al., 2004).
Numerous negative consequences of having an unmet assistance need have also been identified in the research literature. In particular, older adults with an unmet assistance need have been shown to have an increased likelihood of experiencing weight loss, dehydration, falls, burns (LaPlante et al., 2004), increased number of emergency room and hospital visits (Allen & Mor, 1997), increased number of hospitalizations and nursing home placements (Sands et al., 2006), and higher mortality rates (Blazer, Sachs-Ericsson, & Hybels, 2005). Therefore, with identification of unmet assistance need and timely intervention, these unwanted outcomes may be avoided.
With respect to racial and ethnic minorities, older American Indians have been shown to have some of the highest prevalence of functional disability (Goins, Moss, Buchwald, & Guralnik, 2007) and many chronic health conditions (Goins & Pilkerton, 2010) compared with the general U.S. older adult population. Specifically, the 2000U.S. Census data among adults aged ≥55 years indicated that 36% of American Indians and Alaska Natives, compared with 33% of African Americans and 25% of whites, had a functional disability (Goins et al., 2007). Given the disproportionate burden of disability and chronic health problems in older American Indians, it is important to identify the prevalence and correlates of unmet assistance need in this population. Although the health profile of older American Indians suggests a greater need for support with ADLs and IADLs, there is surprisingly little empirical information about the extent of personal assistance received by older American Indians.
To guide our study in identifying correlates of unmet assistance need among older adults, we used the Disablement Process model (Verbrugge & Jette, 1994). The Disablement Process model describes how chronic and acute conditions affect functioning and describes the personal and environmental factors that speed or slow the progression toward disability. According to the model, the main pathway to disability is through impairment and physical functioning. In order to obtain a full sociomedical scope, this model accounts for other contributing influences including demographic characteristics and extra- and intrapersonal factors. We have extended the Disablement Process model’s main pathway to capture assistance needs as a direct result of a disability.
Thus, the objectives of our study were to examine the prevalence and correlates of unmet assistance need among older American Indians. As delineated by the Disablement Process model and found in prior research (Allen & Mor, 1997; Desai et al., 2001; Kennedy, 2001, LaPlante et al., 2004; Newcomer et al., 2005; Williams et al., 1997), we hypothesized that the prevalence of unmet assistance need will be greater in our sample of older American Indians compared with what has been found in other older adult populations. With respect to correlates of unmet assistance need, we hypothesized that younger age, female sex, unmarried, living alone, lower education, greater number of chronic conditions and ADL/IADL disabilities, poorer lower body physical functioning, clinically significant number of depressive symptoms, and lower social support would be associated with greater unmet need.
Methods
Data Collection and Analytic Sample
Data for our analyses were collected as part of the Native Elder Care Study, a cross-sectional study of community-dwelling older members of a federally recognized American Indian tribe in the Southeast (Goins, Garroutte, Leading Fox, Geiger, & Manson, 2011). From 2006 to 2008, using in-person interviewer-administered surveys, data were collected on demographic characteristics, physical functioning, mental and physical health, personal assistance needs, and psychosocial resources. Inclusion criteria for this study included being an enrolled tribal member, aged ≥55 years, residing in the tribe’s service area, noninstitutionalized, and having passed a cognitive screen. We used an age threshold of 55 years rather than 65 years because it was requested by the project’s tribal stakeholders and data have shown rapid declines in health status and shorter life expectancy among American Indians compared with other racial and ethnic groups (Hayward & Heron, 1999; Indian Health Service, 2013).
According to the tribal enrollment records, 1,430 persons were potentially eligible for study inclusion based on residential location and age. This list was randomized and the names and contact information were distributed to interviewers. Equal numbers of respondents were sought for the age groups 55–64, 65–74, and ≥75 years with a total targeted sample size of 500. Randomly selected persons were recruited via telephone call or home visit by an interviewer to participate in the study. We assessed 633 persons for eligibility and 50 were deemed ineligible. Of these 50 individuals, 3 resided outside of the tribe’s service area, 14 were in a nursing home, 19 were deceased, and 14 did not pass the cognitive screen. Most interviews were conducted in the participant’s home (87%) and the remaining conducted in a tribal office building. Seventy-eight persons refused to participate, yielding an 87% response rate and a final sample size of 505.
Measures
Unmet Assistance Need.—
We defined functional disability as having any degree of difficulty in performing ADLs and/or IADLs. Assistance was defined as reporting receipt of paid or unpaid help, supervised or hands-on help, or use of an assistive device to aid with any ADL and IADL in which the participant had difficulty. Unmet assistance need was determined for respondents who reported having difficulty performing at least one ADL or IADL and reported either a lack of personal assistance or insufficient amount of personal assistance.
Figure 1 illustrates how we determined need for assistance for ADLs and IADLs. Those who reported some level of difficulty with ADLs and/or IADLs were asked if they needed assistance with that particular activity. Need was classified into three categories: no need, met need, or unmet assistance need. This classification scheme was based on the flow of conditional responses to skip-patterned questions for each ADL and IADL. Respondents with functional disability were classified as having no need with any ADL or IADL if they reported needing no assistance. Respondents were classified as having a met need if they reported having some level of difficulty performing or did not perform an ADL or IADL due to a health condition, received assistance for that activity, and reported no need for more assistance. Respondents were classified as having an unmet need if they reported some level of difficulty performing or did not perform an ADL or IADL due to a health condition and reported needing assistance not currently received or needing more assistance than they currently received. For the analyses, we dichotomized unmet need as having no unmet assistance need versus having an unmet assistance need in one or more ADLs and/or IADLs.
Figure 1.
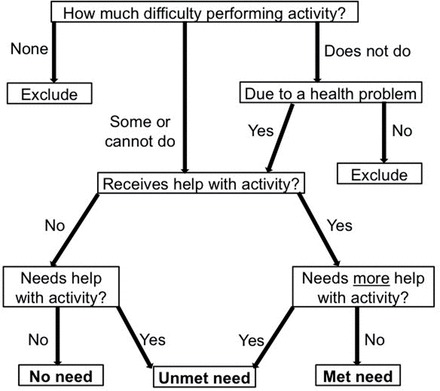
Determination of assistance need for activities of daily living and instrumental activities of daily living.
Correlates of Unmet Assistance Need.—
As guided by the Disablement Process model and prior evidence of unmet assistance need correlates (Allen & Mor, 1997; Desai et al., 2001; Kennedy, 2001, LaPlante et al., 2004; Newcomer et al., 2005; Williams et al., 1997), we examined a number of demographic, physical health, physical functioning, and psychosocial measures. The demographics characteristics that we examined included age, sex, marital status (single vs married), living arrangements (living alone vs with others), and educational attainment (<12 vs ≥12 years).
Physical health was measured by the number of self-reported chronic health conditions (Rigler, Studenski, Wallace, Reker, & Duncan, 2002). This measure comprised the number of 12 common chronic medical conditions that the respondent had been diagnosed since age 55, including heart disease, stroke, angina, congestive heart failure, heart attack, lung disease, Parkinson’s disease, cancer, diabetes, high blood pressure, kidney disease, and liver disease. Respondents were asked if, since age 55, a doctor had told them they had one of the listed 12 conditions with “yes” and “no” response options. This measure was scored by summing the “yes” responses to create a count scale from 0 to 12.
Physical functioning was measured with functional disability and the Short Physical Performance Battery (SPPB). The functional disability measure was generated as the count of reported difficulties in performing any of the eight ADLs and eight IADLs. Scores on this measure ranged from 0 to 16, with higher scores indicating greater functional disability. The SPPB assesses lower body functioning abilities via testing balance, gait speed, and chair stands (Guralnik et al., 1994). Scores on this measure ranged from 0 to 12, with higher scores indicating greater physical functioning ability.
We conceptualized the psychosocial measures as the extra- and intrapersonal factors influencing the main pathway and measured these with the Center for Epidemiological Studies-Depression (CES-D) scale (Radloff, 1977) and the Medical Outcomes Study Social Support (MOSSS) survey (Sherbourne & Stewart, 1991). For the CES-D, respondents were asked the frequency they experienced 20 depressive symptoms within the last week, with a response scale ranging from 0 (rarely or none of the time) to 3 (most or all of the time). This measure was treated as a binary measure with an established cutoff score of ≥16 to determine clinically significant depressive symptomatology (Radloff, 1977). The MOSSS survey is a 19-item scale gauging the frequency of the availability of social support with response items ranging from 1 (none of the time) to 5 (all of the time). Scores were tiered into low, medium, and high levels of social support.
Statistical Analyses
We weighted individual responses to account for differential sampling rates across the three age groups. We used descriptive statistics to examine the prevalence of those indicating difficulty in performing ADLs and IADLs for the entire analytic sample (n = 505). Then, for those indicating difficulty with at least one of the eight ADLs or eight IADLs, we determined the prevalence of those indicating no need, met need, and unmet need by each activity. We then determined the prevalence of those with an unmet assistance need among those reporting a need by each activity. Our analytic sample to examine assistance need status (no need, met need, and unmet need) was restricted to those who reported one or more ADL or IADL difficulties (n = 262), and our inferential analytic sample to detect correlates of unmet assistance need was restricted to those who reported one or more ADL or IADL assistance needs (met need and unmet need status; n = 195).
Logistic regression was used to determine significant correlations with unmet assistance need. Odds ratios (ORs) and corresponding 95% confidence intervals (CIs) were calculated. We first used bivariate regression to assess the correlations of unmet assistance need by the demographic, physical health, physical functioning, and psychosocial measures. Significant correlates found in the bivariate analysis were retained in the multivariate model. Prior to estimating the multiple variable regression models, we estimated the variance inflation factor to test for multicollinearity among the remaining independent variables. The variance inflation factor value was low, indicating that multicollinearity was not a substantive issue in the regression models.
We examined the missing values in ADL and IADL measures and found them to be minimally present (<1% of respondents) on any one activity. Based on the skip patterns for questions that determined need status, we used logical inference to replace missing values (Little & Smith, 1987). We used multiple imputation by chained equations to impute any remaining missing data for the independent variables (Royston & White, 2011). Data were imputed on 6 cases for living arrangements, 2 cases for educational attainment, 13 cases for the CES-D, and 9 cases for the MOSSS survey. All analyses were performed using the Stata Statistical Software version 12.1 (Stata Statistical Software, 2007).
Results
Table 1 presents descriptive statistics for ADL and IADL difficulties (n = 505), assistance need status (n = 262), and unmet assistance need (n = 195) in our sample. Overall, 49.0% of participants indicated difficulty with one or more ADLs/IADLs. ADLs with the largest percent of our sample reporting a difficulty included walking (35.6%), transferring (19.2%), bathing/showering (11.7%), and getting outside (10.8%). IADLs with the largest percent of our sample reporting a difficulty included heavy housework (29.0%), light housework (17.9%), shopping (15.7%), and preparing meals (12.7%).
Table 1.
Prevalence of Need and Unmet Assistance Need With ADLs and/or IADLs
| Difficulty performing (n = 505)a | Assistance need statusb (n = 262) | Unmet assistance needc (n = 195) | |||
|---|---|---|---|---|---|
| No need | Met need | Unmet need | |||
| n (%) | n (%) | n (%) | n (%) | (%) | |
| ADLs | |||||
| Bathing/showering | 68 (11.7) | 16 (31.1) | 33 (38.6) | 19 (30.2) | (43.9) |
| Dressing | 46 (8.6) | 9 (22.2) | 30 (67.9) | 7 (9.9) | (12.8) |
| Eating | 12 (1.7) | 6 (45.3) | 5 (48.2) | 1 (6.5) | (11.9) |
| Transferring | 98 (19.2) | 56 (55.7) | 27 (29.3) | 15 (15.0) | (33.8) |
| Walking | 181 (35.6) | 114 (64.7) | 49 (24.2) | 18 (11.2) | (31.6) |
| Toileting | 34 (6.2) | 15 (47.4) | 8 (20.7) | 11 (31.9) | (60.6) |
| Grooming | 20 (3.9) | 5 (40.5) | 11 (45.7) | 4 (13.8) | (23.2) |
| Getting outside | 54 (10.8) | 17 (32.6) | 23 (35.5) | 14 (31.9) | (47.4) |
| IADLs | |||||
| Using telephone | 46 (7.7) | 14 (29.4) | 23 (56.5) | 9 (14.1) | (20.0) |
| Light housework | 90 (17.9) | 18 (20.7) | 47 (50.8) | 25 (28.5) | (35.9) |
| Heavy housework | 145 (29.0) | 25 (20.4) | 69 (43.5) | 51 (36.0) | (45.3) |
| Preparing meals | 66 (12.7) | 11 (20.2) | 40 (58.7) | 15 (21.1) | (26.5) |
| Shopping | 85 (15.7) | 7 (9.5) | 60 (69.3) | 18 (21.2) | (23.4) |
| Managing money | 41 (8.0) | 8 (27.3) | 27 (55.9) | 6 (16.7) | (23.0) |
| Managing medications | 39 (6.9) | 1 (2.4) | 34 (88.3) | 4 (9.4) | (9.6) |
| Transportation | 67 (11.8) | 4 (5.9) | 48 (72.1) | 15 (21.9) | (23.3) |
| Any ADL/IADL | 262 (49.0) | 67 (28.0) | 104 (37.5) | 91 (34.4) | (47.8) |
Notes: Percentages are weighted. ADLs = activities of daily living; IADLs = Instrumental activities of daily living.
aReported “some” or “a lot of” difficulty, or “cannot do because of health condition.”
bDenominator represents persons with a stated difficulty in each ADL or IADLs.
cDenominator represents persons with need (either met need or unmet need) for ADL and IADL assistance.
More than 34% of persons with an ADL and/or IADL difficulty had one or more unmet needs. Among those with an ADL difficulty, the highest percent of unmet ADL assistance need was with toileting (31.9%), getting outside (31.9%), bathing/showering (30.2%), and transferring (15.0%). Among those with an IADL difficulty, the highest percent of unmet IADL need was with heavy housework (36.0%), light housework (28.5%), transportation (21.9%), and preparing meals (21.1%).
Nearly 48% of persons with one or more assistance needs had one or more unmet needs. Among those with an ADL assistance need (i.e., met need or unmet need), the highest percent of unmet ADL assistance need was with toileting (60.6%), getting outside (47.4%), bathing/showering (43.9%), and transferring (33.8%). Among those with an IADL assistance need, the highest percent of unmet IADL assistance need included heavy housework (45.3%), light housework (35.9%), preparing meals (26.5%), and shopping (23.4%).
Prevalence of need and unmet assistance need by participant characteristics are shown in Table 2. ORs and corresponding 95% CIs are presented for the bivariate associations with one or more unmet assistance needs. The highest prevalence of unmet assistance need was exhibited in those who had lower educational attainment, ≥4 chronic conditions, ≥5 ADL and/or IADL difficulties, lower levels of physical functioning, clinically significant depressive symptomatology, and lower levels of social support. Having one or more unmet assistance needs was significantly associated with ≥5 ADL and IADL difficulties (OR = 3.15, 95% CI = 1.43, 6.90), clinically significant depressive symptomatology (OR = 2.48, 95% CI = 1.11, 5.57), and inversely with higher levels of social support (OR = 0.25, 95% CI = 0.11, 0.60). The multivariate analysis indicates that ADL and IADL difficulty (OR = 1.64, 95% CI = 1.08, 2.48) and social support (OR = 0.30, 95% CI = 0.56, 0.67) were significantly associated with having an unmet assistance need.
Table 2.
Prevalence and Correlations of Unmet ADL and IADL Assistance Need
| Variablea | With needb | Unmet needc | Odds ratiod | 95% confidence interval |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Age | ||||
| 55–64 | 52 (67.5) | 26 (50.0) | — | — |
| 65–74 | 58 (72.5) | 28 (48.3) | 0.93 | 0.44–2.00 |
| ≥75 | 85 (81.0) | 37 (43.5) | 0.77 | 0.38–1.56 |
| Sex | ||||
| Male | 45 (62.1) | 18 (47.0) | — | — |
| Female | 150 (76.4) | 73 (48.2) | 1.05 | 0.50–2.21 |
| Marital status | ||||
| Single | 123 (71.9) | 59 (49.0) | — | — |
| Married | 72 (71.2) | 32 (46.3) | 0.90 | 0.47–1.72 |
| Living arrangements | ||||
| Live with other(s) | 48 (57.9) | 21 (58.5) | — | — |
| Lives alone | 145 (77.6) | 72 (44.1) | 0.50 | 0.24–1.03 |
| Education | ||||
| ≥12 | 98 (65.6) | 43 (45.3) | — | — |
| <12 | 96 (81.3) | 48 (50.5) | 1.23 | 0.65–2.33 |
| Chronic conditions | ||||
| 0–1 | 65 (61.4) | 25 (39.1) | — | — |
| 2–3 | 82 (73.2) | 41 (50.9) | 1.54 | 0.73–3.24 |
| ≥4 | 48 (89.1) | 25 (52.6) | 1.64 | 0.70–3.83 |
| ADL and IADL difficulty | ||||
| 1–2 | 53 (44.9) | 17 (33.5) | — | — |
| 3–4 | 44 (77.7) | 17 (34.3) | 1.04 | 0.41–2.62 |
| ≥5 | 98 (100) | 57 (61.3) | 3.15** | 1.43–6.90 |
| Physical functioning | ||||
| 0–2 | 61 (94.5) | 28 (48.2) | — | — |
| 3–5 | 34 (81.0) | 19 (62.1) | 1.76 | 0.68–4.59 |
| 6–8 | 55 (75.1) | 22 (40.0) | 0.72 | 0.31–1.64 |
| 9–12 | 45 (54.4) | 22 (47.4) | 0.97 | 0.41–2.28 |
| Depressive symptoms | ||||
| <16 symptoms | 141 (69.6) | 61 (42.1) | — | — |
| ≥16 symptoms | 41 (83.0) | 27 (59.2) | 2.48* | 1.11–5.57 |
| Social support | ||||
| Low | 5 (71.5) | 5 (100) | — | — |
| Medium | 34 (74.3) | 24 (68.9) | 0.26** | 0.12–0.56 |
| High | 156 (71.5) | 62 (40.7) | 0.25** | 0.11–0.60 |
Notes: Counts are unadjusted and percentages age adjusted. All percentages are weighted. ADLs = activities of daily living; IADLs = instrumental activities of daily living.
aFirst listed category is referent group. *p < .05; **p < .01 for chi-square test.
bTotal and percent of disabled persons with need (either met or unmet need) for personal assistance with one or more ADLs and IADLs (n = 262).
cPersons with unmet need; denominator is total disabled persons declaring met or unmet need (n = 195).
dBivariate logistic regression analyses.
Discussion
Overall, our sample of community-dwelling American Indians aged ≥55 years had a high prevalence of functional disability, need for assistance, and unmet assistance need. Using a more inclusive measure of functional disability (i.e., ADL difficulty in addition to IADL difficulty), the prevalence of unmet need was 47.8% among those with one or more ADL and/or IADL difficulties. We were only able to identify one other study that examined unmet assistance need among an age-comparable sample of older adults. Specifically, Sands and colleagues (2006) examined a large sample of noninstitutionalized frail adults aged ≥55 years that were enrolled in the All-inclusive Care for the Elderly (PACE) program; data indicated 18.5% of study participants with an unmet need with ADLs. Another study with a nationally representative sample of adults aged ≥70 years showed a slightly higher prevalence (20.7%) of ADL unmet assistance need (Desai et al., 2001). Our findings support others demonstrating greater unmet assistance need among American Indians (Barnes, Powell-Griner, & Adams, 2005) and other racial and ethnic minorities (Kennedy, 2001; LaPlante et al., 2004). However, we recommend exercising caution in drawing direct comparisons of these studies to ours, namely for differences in measurement and study inclusion criteria. The denominator used in the PACE study included all persons with an ADL limitation, not with a stated need. Even so, the estimated prevalence in our sample with the same denominator was higher (34.4% compared with 18.5%). Second, our higher prevalence estimate may also be, in part, due to the inclusion of IADLs, in addition to ADLs. Future studies that assess unmet assistance need with this more inclusive measure in nationally representative samples are warranted to understand the assistance needs beyond those of ADLs. With respect of study inclusion criteria, the PACE participants were eligible for receiving nursing home level care and our study excluded persons exhibiting signs of dementia. The PACE study showed a significantly higher prevalence of unmet need among those with dementia (Sands et al., 2006), suggesting that our results likely underestimated unmet need.
Our findings demonstrated that the degree of functional disability is associated with the odds of having one or more unmet assistance needs among older American Indians, controlling for depressive symptomatology and perceived social support. These findings are consistent with prior studies that the degree of functional disability is positively and strongly associated with greater unmet assistance need, controlling for other factors (Allen & Mor, 1997; Desai et al., 2001; Newcomer et al., 2005). Yet, when examining the associations with other physical functioning measures such as chronic conditions and physical functioning, we found no significant associations with unmet assistance need.
Our results also demonstrated that lower levels of social support were associated with having an unmet assistance need. Overall, social support is an American Indian value (Hopkins, Kwachka, Lardon, & Mohatt, 2007), which reflects the importance of extended family systems that foster interdependence. This is particularly relevant for older American Indians, who have been traditionally viewed as respected and treasured community members (Hopkins et al., 2007). Interventions that tap into these cultural values may provide effective and culturally appropriate strategies for reducing unmet assistance need in Native communities (Hogan, Linden, & Najarian, 2002).
In contrast to prior studies, none of the demographic characteristics were significantly associated with unmet assistance need; although, the relationship with unmet assistance need for each of these characteristics was in the hypothesized direction. Other research had indicated that those with greater unmet assistance need are more likely to be female (LaPlante et al., 2004), be of younger age (Allen & Mor, 1997), have lower income, and live alone (Desai et al., 2001; Kennedy, 2001). Our inability to detect significant correlations may, in part, be due to our lower sample size compared with studies with large national samples of older adults.
Our study has several limitations worth acknowledgement. First, because our study was based on cross-sectional data, we are unable to examine causality between the variables correlated with unmet assistance need. Second, unmet assistance need was established via self-report, which could provide potentially biased results. It has been posited that American Indians are more reluctant to report needing assistance than their racial and ethnic peers (Loftin, 1983; Moss, 2005), and therefore it is plausible that participants in our study underreported actual assistance needs. Third, researchers have indicated that for some, social support can also have negative impacts on health (Croezen et al., 2012), and our measure did not capture the potentially negative impact of social support. Fourth, our study participants were all members of a single American Indian tribe. Given the considerable regional and tribal variation documented in health (Indian Health Service, 2009) and functional disability (Moss, Schell, & Goins, 2006) among different populations of American Indians, caution is warranted in generalizing our findings to other American Indian communities. We believe it is also important to note that given our inclusion criteria of residing in the tribal service area, our study participants resided on tribal lands as well as nontribal lands although all were considered rural. Last, as stated prior, our prevalence comparisons of unmet assistance were limited in that studies differed in measurement, study inclusion and exclusion criteria, and sampling frames.
Given the high prevalence of functional disability and unmet assistance need among older American Indians, there is an overall high level of interest among tribes for providing long-term services to their older members (Goins, Bogart, & Roubideaux, 2010). Provided that social support appears to be instrumental to older adults with functional disabilities in achieving assistance with ADLs and IADLs, efforts to strengthen social networks for this segment of the population are recommended. However, those with functional disabilities also could benefit from increasing the availability and accessibility of a variety of formal long-term care services (Jervis, Jackson, & Manson, 2002). Since 2009, the Indian Health Care Improvement Act Amendments (H.R. 2708) bill has authorized the Indian Health Service to provide long-term care services and to increase outreach and enrollment of American Indians into the Medicaid program (H.R. 2708—111th Congress, 2009), an important national stride toward narrowing the gap between existing available and accessible long-term care services and personal assistance needs among elders with functional disabilities. However, funding is not the only barrier to ensuring that older American Indians receive adequate long-term care (Goins et al., 2010); major funders of long-term care services, such as Medicaid, should partner with tribal leaders to address nonfiscal barriers such as low literacy, high staff turnover rate, and mistrust of federal government to these services.
We have identified several areas for further research. Longitudinal research examining predictors and consequences of unmet assistance need is critical to extend our understanding of factors contributing to and resulting from unmet assistance need among older adults. In addition to positive social support, future health studies should examine the potential negative role that social support might have on functional disability, need, and unmet need. Currently, there are no contemporary studies that have empirically examined the presence of Native traditional cultural values of social support and to the extent that it translates into elder care today. Research into this area would contribute to a better understanding as to why there are reservation-based tribal elders who report substantial unmet assistance needs. Provided the relatively recent changes to provision of long-term care services in tribal communities, studies are needed to examine how tribally delivered long-term care services are developed and administered, and affect the assistance needs for older American Indians. Furthermore, research can help by identifying specific types of tribal service needs and barriers to providing and accessing long-term care services.
Funding
The authors receive support by award AG022336 from the National Institute on Aging .
Acknowledgments
We would like to give our special thanks to Dr. Alan Acock for his contributions on the statistical analyses.
References
- Agree E. M., Freedman V. A. (2003). A comparison of assistive technology and personal care in alleviating disability and unmet need. The Gerontologist, 43, 335–344. doi:10.1093/geront/43.3.335 [DOI] [PubMed] [Google Scholar]
- Allen S. M., Mor V. (1997). The prevalence and consequences of unmet need. Contrasts between older and younger adults with disability. Medical Care, 35, 1132–1148. [DOI] [PubMed] [Google Scholar]
- Barnes P. M., Powell-Griner E., Adams P. F. (2005). Health characteristics of the American Indian and Alaska Native adult population, United States, 1999–2003. Advanced Data, 356, 1–24. [PubMed] [Google Scholar]
- Blazer D. G., Sachs-Ericsson N., Hybels C. F. (2005). Perception of unmet basic needs as a predictor of mortality among community-dwelling older adults. American Journal of Public Health, 95, 299–304. doi:10.2105/AJPH.2003.035576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croezen S., Picavet H. S., Haveman-Nies A., Verschuren W. M., de Groot L. C., van’t Veer P. (2012). Do positive or negative experiences of social support relate to current and future health? Results from the Doetinchem Cohort Study. BMC Public Health, 12, 65. doi:10.1186/1471-2458-12-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai M. M., Lentzner H. R., Weeks J. D. (2001). Unmet need for personal assistance with activities of daily living among older adults. The Gerontologist, 41, 82–88. doi:10.1093/geront/41.1.82 [DOI] [PubMed] [Google Scholar]
- Diwan S., Moriarty D. (1995). A conceptual framework for identifying unmet health care needs of community dwelling elderly. Journal of Applied Gerontology, 14, 47–63. doi:10.1177/073346489501400104 [Google Scholar]
- Goins R. T., Bogart A., Roubideaux Y. (2010). Service provider perceptions of long-term care access in American Indian and Alaska Native communities. Journal of Health Care for the Poor and Underserved, 21, 1340–1353. doi:10.1353/hpu.2010.0934 [DOI] [PubMed] [Google Scholar]
- Goins R. T., Garroutte E. M., Leading Fox S., Geiger S. D., Manson S. M. (2011). Theory and practice in participatory research: Lessons from the Native Elder Care Study. The Gerontologist, 51, 285–294. doi:10.1093/geront/gnq130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goins R. T., Moss M., Buchwald D., Guralnik J. M. (2007). Disability among older American Indians and Alaska Natives: An analysis of the 2000 Census Public Use Microdata Sample. The Gerontologist, 47, 690–696. doi:10.1002/gps.282510.1002/ gps.2825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goins R. T., Pilkerton C. S. (2010). Comorbidity among older American Indians: The Native Elder Care Study. Journal of Cross-Cultural Gerontology, 25, 343–354. doi:10.1007 /s10823-010-9119-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik J. M., Simonsick E. M., Ferrucci L., Glynn R. J., Berkman L. F., Blazer D. G, … Wallace R. B. (1994). A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology, 49, M85–M94. doi:10.1093/geronj/49.2.M85 [DOI] [PubMed] [Google Scholar]
- Hayward M. D., Heron M. (1999). Racial inequality in active life among adult Americans. Demography, 36, 77–91. doi:10.2307/2648135 [PubMed] [Google Scholar]
- Hogan B. E., Linden W., Najarian B. (2002). Social support interventions: Do they work? Clinical Psychology Review, 22, 383–442. [DOI] [PubMed] [Google Scholar]
- Hopkins S. E., Kwachka P., Lardon C., Mohatt G. V. (2007). Keeping busy: A Yup’ik/Cup’ik perspective on health and aging. International Journal of Circumpolar Health, 66, 42–50. [DOI] [PubMed] [Google Scholar]
- H.R. 2708—111th Congress. (2009). Indian Health Care Improvement Act Amendments of 2009. www.GovTrack.us. Retrieved from http://www.govtrack.us/congress/bills/111/hr2708
- Indian Health Service. (2009). Regional differences in Indian health, 2002 - 2003. Washington, DC: U.S Department of Health and Human Services. [Google Scholar]
- Indian Health Service. (2013). Facts on Indian health disparities. Washington, DC: U.S. Department of Health and Human Services. [Google Scholar]
- Jervis L. L., Jackson M. Y., Manson S. M. (2002). Need for, availability of, and barriers to the provision of long-term care services for older American Indians. Journal of Cross-Cultural Gerontology, 17, 295–311. doi:10.1023/A:1023027102700 [DOI] [PubMed] [Google Scholar]
- Kennedy J. (2001). Unmet and undermet need for activities of daily living and instrumental activities of daily living assistance among adults with disabilities: Estimates from the 1994 and 1995 disability follow-back surveys. Medical Care, 39, 1305–1312. [DOI] [PubMed] [Google Scholar]
- LaPlante M. P., Kaye H. S., Kang T., Harrington C. (2004). Unmet need for personal assistance services: Estimating the shortfall in hours of help and adverse consequences. Journal of Gerontology: Psychological Sciences and Social Sciences, 59, S98–S108. doi:10.1093/geronb/59.2.S98 [DOI] [PubMed] [Google Scholar]
- Lima J. C., Allen S. M. (2001). Targeting risk for unmet need: Not enough help versus no help at all. Journal of Gerontology: Psychological Sciences and Social Sciences, 56, S302–S310. [DOI] [PubMed] [Google Scholar]
- Little R. J. A., Smith P. J. (1987). Editing and imputation for quantitative survey data. Journal of the American Statistical Association, 82, 58–68. doi:10.1080/016 21459.1987.10478391 [Google Scholar]
- Loftin J. D. (1983). The “Harmony Ethic” of the conservative Eastern Cherokees: A religious interpretation. Journal of Cherokee Studies, 8, 40–43. [Google Scholar]
- Moss M. P. (2005). TOLERATED ILLNESS concept and theory for chronically ill and elderly patients as exemplified in American Indians. Journal of Cancer Education, 20(Suppl. 1), 17–22. doi:10.1207/s15430154jce2001s_05 [DOI] [PubMed] [Google Scholar]
- Moss M. P., Schell M. C., Goins R. T. (2006). Using GIS in a first national mapping of functional disability among older American Indians and Alaska Natives from the 2000 census. International Journal of Health Geographics, 5, 37. doi:10.1111/j.1748-0361.2010.00315.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. (2013). Health, United States, 2012: With special feature on emergency care. Hyattsville, MD: Author. [PubMed] [Google Scholar]
- Newcomer R., Kang T., Laplante M., Kaye S. (2005). Living quarters and unmet need for personal care assistance among adults with disabilities. Journal of Gerontology: Psychological Sciences and Social Sciences, 60, S205–S213. doi:10.1093/geronb/60.4.S205 [DOI] [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. doi:10.1177/01466216 7700100306 [Google Scholar]
- Rigler S. K., Studenski S., Wallace D., Reker D. M., Duncan P. W. (2002). Co-morbidity adjustment for functional outcomes in community-dwelling older adults. Clinical Rehabilitation, 16, 420–428. doi:10.1191/0269215502cr515oa [DOI] [PubMed] [Google Scholar]
- Royston P., White I. R. (2011). Multiple imputation by chained equations (MICE): Implementation in Stata. Journal of Statistical Software, 45, 1–20. [Google Scholar]
- Sands L. P., Wang Y., McCabe G. P., Jennings K., Eng C., Covinsky K. E. (2006). Rates of acute care admissions for frail older people living with met versus unmet activity of daily living needs. Journal of the American Geriatrics Society, 54, 339–344. doi:10.1111/j.1532-5415.2005.00590.x [DOI] [PubMed] [Google Scholar]
- Sherbourne C. D., Stewart A. L. (1991). The MOS social support survey. Social Science & Medicine (1982), 32, 705–714. doi:10.1016/0277-9536(91)90150-B [DOI] [PubMed] [Google Scholar]
- Stata Statistical Software. (2007). Version 12 [computer program]. College Station, TX: StataCorp LP. [Google Scholar]
- Verbrugge L. M., Jette A. M. (1994). The disablement process. Social Science & Medicine (1982), 38, 1–14. doi:10.1016/0277-9536(94)90294-1 [DOI] [PubMed] [Google Scholar]
- Williams J., Lyons B., Rowland D. (1997). Unmet long-term care needs of elderly people in the community: A review of the literature. Home Health Care Services Quarterly, 16, 93–119. doi:10.1300/J027v16n01_0 [DOI] [PubMed] [Google Scholar]


