Abstract
The current study examined internalizing symptoms, affect reactivity, and distress intolerance as prospective predictors of increases in eating disorder (ED)-attitudes during adolescence. Adolescents (n=206) took part in a six-year longitudinal study examining the development of psychopathology. Latent growth curve analysis was used to examine associations between predictors and later ED-attitudes. Distress intolerance and internalizing symptoms were associated with ED-attitudes at baseline, but did not predict increases over time. Affect reactivity, however, was significantly associated with increases in ED-attitudes over time. Baseline affect reactivity did not interact with baseline distress intolerance to predict increases in ED-attitudes; however higher baseline internalizing symptoms interacted with distress intolerance to predict increases in ED-attitudes across adolescence. These results are among the first to document that affect reactivity alone and the combined effect of high internalizing symptoms and high distress intolerance early in adolescence are risk factors for the later development of ED-attitudes.
Keywords: Eating disorders, adolescence, negative affect, affect reactivity, distress tolerance, internalizing symptoms
Introduction
Eating disorders (EDs) are life-threatening conditions that are often associated with significant psychological comorbidity (Swanson, Crow, Le Grange, Swendsen, & Merikangas, 2011) and premature mortality (Keshaviah et al., 2014). Although EDs occur across the age spectrum, anorexia nervosa and bulimia nervosa have the highest incidence and point prevalence during adolescence (Lewinsohn, Striegel-Moore, & Seeley, 2000). In the cognitive-behavioral model of EDs (Fairburn, 2008), the overvaluation of and concern about shape and weight (i.e., ED-attitudes) is a core maintenance factor in the development and maintenance of ED symptoms and behaviors. Indeed, the presence of ED-attitudes in early adolescence significantly predicts continuation of symptoms in late adolescence and early adulthood (Killen et al., 1994; Kotler, Cohen, Davies, Pine, & Walsh, 2001). Despite the high risk for ED symptom development during adolescence (APA, 2013), few longitudinal studies have examined the developmental course, and predictors of ED-attitudes in youth (Bakalar, Shank, Vannucci, Radin, & Tanofsky-Kraff, 2015). Identifying psychological predictors of ED-attitudes in youth can be critical for informing prevention and early intervention targets.
Negative affect-related variables and EDs
Negative affect has long been hypothesized to predict the onset and maintenance of ED pathology. In adolescents, negative affect is cross-sectionally (Stice, 1998) and prospectively (Leon, Fulkerson, Perry, Keel, & Klump, 1999) related to disordered eating. In addition to chronic negative affect, internalizing disorders (e.g., depression) prospectively predict increases in EDs during adolescence (Holm-Denoma, Hankin, & Young, 2014; Measelle, Stice, & Hogansen, 2006), suggesting that negative affect and internalizing symptoms serve as risk and maintenance factors for ED behaviors and attitudes.
Negative affect and internalizing symptoms might be particularly likely to contribute to the later onset of ED symptoms when an individual is unable to tolerate distressing internal experiences. Specifically, distress tolerance, or the capacity to withstand an aversive internal state (Linehan, 1993) has been posited as an etiological mechanism of ED risk. Those with high distress intolerance are driven to engage in behaviors that reduce emotional distress in the short-term, even when such actions eventually result in negative consequences (Simons & Gaher, 2007). Thus, the relation between negative affect and ED psychopathology may depend on one's level of distress intolerance, such that those with high distress intolerance show the strongest relation between negative affect and ED psychopathology. Supporting this notion, several investigations have reported that individuals with eating pathology are more distress intolerant (Corstophine, Mountford, Tomlinson, Waller, & Meyer, 2007; Hambrook et al., 2011; Lavender, Happel, Anestis, Tull, & Gratz, 2015) and engage in maladaptive eating behaviors in order to down-regulate negative emotions (Dir, Karyadi, & Cyders, 2013; Racine et al., 2013).
Relatedly, recent research suggests that changes in negative affect in response to a stressor (i.e., affect reactivity) may be particularly important in the development of EDs (Lingswiler, Crowther, & Stephens, 1987; Smyth et al., 2007; Goldschmidt et al., 2014). For instance, utilizing momentary sampling, Goldschmidt and colleagues (2014) found that increases in negative affect in response to a stressor immediately preceded incidents of binging and purging. It follows that distress intolerant individuals may experience greater increases in negative affect following a stressful event that, in turn, may predict the use of disordered eating behaviors.
Despite a growing body of evidence suggesting that internalizing symptoms, distress intolerance, and affect reactivity contribute to the development and maintenance of ED thoughts and behaviors, numerous unanswered questions remain. For example, the significance of affect reactivity as a predictor of ED symptom development in youth has not yet been evaluated. Additionally, no studies have examined the relationship between distress intolerance and ED symptomology in youth, either cross-sectionally or prospectively. Perhaps most importantly, to our knowledge, no investigations have directly examined the potential moderating role of distress intolerance in the prospective or concurrent relation between negative affect, affect reactivity and ED symptomology.
Current Study
In the current study, we examined internalizing symptoms, affect reactivity, and distress intolerance as predictors of ED-attitudes in a longitudinal community sample of children and adolescents. We hypothesized that ED-attitudes would increase over time and that early internalizing symptoms, distress intolerance, and affect reactivity would predict later increases in ED-attitudes. We also examined interactions between early distress intolerance and both internalizing symptoms and affect reactivity on changes in ED-attitudes over time. Specifically, we hypothesized that the combination of higher internalizing symptoms and higher distress intolerance would predict increases in ED-attitudes over time and the same would be expected for higher distress intolerance and greater affect reactivity.
Method
Participants and Procedures
The current study included youth recruited from a metropolitan area who are taking part in an ongoing longitudinal study examining the development of psychopathology. Youth and their families were recruited for the larger study from the community. Participants were required to be proficient in English and be able to commit to taking part in yearly assessments. The original sample included 277 (46% female) children and their parents; however, because key measures pertaining to the current study were not introduced until the third year of enrollment for participants, the current study utilized data only from those adolescents who completed all measures at this wave (Wave 3 for the parent study, relabeled T1, for clarity in the remainder of the manuscript). Thus, the current sample included 206 adolescents between the ages of 11 and 15 (Mage=13.03, SDage=0.89) at T1. Retention of participants over the course of this study was good; out of the original sample of 206 youth, 193 (Mage=14.00, SDage=0.89) participated in Wave 4 (T2), 175 (Mage=15.02, SDage=0.95) participated in Wave 5 (T3), 152 (Mage=16.06, SDage=0.89) participated in Wave 6 (T4), 130 (Mage=17.00, SDage=0.95) participated in Wave 7 (T5), and 123 (Mage=18.05, SDage=0.97) participated in Wave 8 (T6). In the sample, 49% identified as White/Caucasian, 37% as Black/African-American, 4% as Latino/a, and 10% as “Other.” The study was approved by the Institutional Review Board. Measures.
Eating Disorder Attitudes
The College Eating Disorders Screen (COEDS) (Nowak, Roberson-Nay, Strong, Bucceri, & Lejuez, 2003) is a seven-item self-report measure of youths' attitudes regarding weight and eating behavior. Participants rated the extent to which they had certain ED thoughts or feelings, e.g., “I believe I am fatter than most people say I am.” The COEDS is considered a measure of ED vulnerability and was developed to capture preclinical symptoms of EDs (Nowak et al., 2003; Pearson, Guller, McPherson, Lejuez, & Smith, 2013). The COEDS is correlated with other validated measures of ED pathology. Items on the COEDS appropriately capture ED cognitive symptoms, as they are highly correlated with, subscales assessing body dissatisfaction, body image, and preoccupation with thinness. However, the COEDS exhibits moderate to low correlations with disordered eating behaviors, suggesting the COEDS captures risk for disordered eating versus current disordered eating and is a valid measure of vulnerability. The COEDS is reliable and valid for use in an adolescent population (Pearson et al., 2013). In the current study, Cronbach's alphas ranged from .85 to .91 across all years.
Distress Intolerance
The Behavioral Indicator of Resiliency to Distress (BIRD) (Lejuez, Daughters, Danielson, & Ruggiero, 2006) is a behavioral measure of distress intolerance. In this computerized task, youth click on one of ten boxes designated by a dot. Clicking on the correct box results the participant being awarded a point. Clicking on the wrong box results in a loud and unpleasant noise, and no point is earned. The BIRD task is divided into three levels that increase in difficulty. In the first level there is initially a 5-second latency between dot presentations. This latency increases by 0.5 seconds for incorrect responses and decreases by 0.5 seconds for correct responses. An average latency is calculated based on the youth's performance in the first level. The second level then starts with this average latency; which is then reduced in half for the final minute of the level (termed the challenge latency). Participants are informed at the beginning of the task that they may quit this last level at any point, but that they will forfeit the opportunity to earn more points once they quit. The time the youth persists in the final level of the task is then used as a measure of behavioral distress intolerance, with lower values denoting higher intolerance. The BIRD has been found to be a valid indicator of risk taking, externalizing and internalizing symptoms among both clinical and community samples (Danielson, Ruggiero, Daughters, & Lejuez, 2010).
Internalizing Symptoms
The Revised Children's Anxiety and Depression Scale (RCADS) (Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000) is a 47-item questionnaire that asks youth to self-report their anxiety and depressive symptoms. Higher scores indicate greater levels of internalizing pathology. The measure demonstrates strong reliability and validity in community samples of youth (Chorpita et al., 2000). In the current study, Cronbach's alpha was .95.
Affect Reactivity
Affect reactivity was measured using an adapted version of the Positive and Negative Affect Schedule for Children (PANAS-C) (Laurent et al., 1999). Participants were administered the questionnaire immediately prior to and following the completion of the BIRD task. The current measure utilized five items to assess youths' current levels of negative affect, including “mad,” “frustrated,” “upset,” “embarrassed,” and “nervous,” on a 10-point rating scale ranging from 0 (not at all) to 10 (extremely). The total score was then computed by summing the responses on each item. The measure has been shown to be both reliable and valid in adolescent populations (Laurent et al., 1999). In the present study, Cronbach's alpha was .76 for the pre-BIRD administration and .80 for the post-BIRD evaluation. Affect reactivity was computed by subtracting the post-task PANAS-C score from the pre-task score. Therefore higher (more positive) scores represent greater decreases in negative affect. The resulting change in affect reactivity scores ranged from -40 to 30.
Data Analytic Plan
A latent growth curve (LGC) model was created to examine changes in risk for ED over time. LGC utilizes multiple waves of data to estimate latent factors representing baseline (intercept) levels and trajectories (slope) of ED-risk across all waves of data. In order to estimate the LGC model of risk for ED, regression weights from the latent intercept term to the manifest measure at each wave were set to 1.0. Regression weights for the slope factor were constrained to 0.0, 1.0, 2.0, 3.0, 4.0, and 5.0 (respectively) to represent a linear trend in change over time. Consistent with recommendations from Little (2003), a competing (more parsimonious) model in which error variances were constrained to be equal across repeated measures (i.e., setting residuals to be homoscedastic) was examined. The difference in fit, as indexed by the change in χ2 statistic and accompanying degrees of freedom, was evaluated. If these constraints did not result in a significant perturbation to model fit, the model was retained.
We examined four fit indices to determine how well the model reflected the data: the χ2 statistic, the Comparative Fit Index (CFI) (Bentler, 1990), the Tucker Lewis Index (TLI) (Tucker & Lewis, 1973), and the Root Mean Square Error of Approximation (RMSEA) (Steiger, 1990). Nonsignificant χ2 values indicate good fit; however, this index is sensitive to sample size. CFI and TLI values greater than .90 and RMSEA values less than .08 suggest acceptable fit (Schweizer, 2010). All analyses were completed using Mplus 6.0 (Muthén & Muthén, 2010), which utilizes full information maximum likelihood (ML) estimation methods to handle missing data for continuous and binary variables missing completely at random (MCAR) and missing at random (MAR). This approach provides less biased parameter estimates than procedures such as listwise or pairwise deletion under the missing at random assumption (Little & Rubin, 1989). Thus, we were able to conduct all analyses on the full sample of 206 youth.
Results
Preliminary Analyses
Missing data patterns among key variables at each wave were examined using Little's MCAR test (Little, 1988). Results suggest that the data were missing completely at random, % (78) = 75.93, p = .55. Next, we examined descriptive statistics and correlations between all key study variables (see Table 1). Results indicate that all waves of the COEDS are correlated with one another (rs range from .52 to .77). Further, sex was significantly associated with change in NA, suggesting that girls report greater increases in NA following the BIRD task than boys.
Table 1. Means, standard deviations, and correlations between key study variables.
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sex (Male) | 1.00 | ||||||||||||
| 2. Race/Ethnicity (White) | 0.00 | 1.00 | |||||||||||
| 3. T1 Age | 0.14* | -0.10 | 1.00 | ||||||||||
| 4. T1 COEDS | -0.32** | 0.11 | -0.00 | 1.00 | |||||||||
| 5. T2 COEDS | -0.35** | -0.02 | 0.02 | 0.72** | 1.00 | ||||||||
| 6. T3 COEDS | -0.31** | 0.11 | -0.04 | 0.54** | 0.64** | 1.00 | |||||||
| 7. T4 COEDS | -0.32** | 0.05 | -0.05 | 0.52** | 0.59** | 0.69** | 1.00 | ||||||
| 8. T5 COEDS | -0.36** | 0.08 | -0.03 | 0.57** | 0.66** | 0.74** | 0.67** | 1.00 | |||||
| 9. T6 COEDS | -0.28** | 0.09 | 0.08 | 0.46** | 0.46** | 0.58** | 0.64** | 0.69** | 1.00 | ||||
| 10. T1 BIRD | 0.08 | 0.00 | 0.08 | -0.15* | -0.13 | -0.16* | -0.03 | -0.11 | -0.12 | 1.00 | |||
| 11. Pre-BIRD NA | -0.06 | 0.08 | -0.09 | 0.16* | 0.10 | 0.04 | 0.12 | 0.08 | 0.09 | 0.04 | 1.00 | ||
| 12. Change in NA | 0.19** | -0.08 | 0.02 | -0.16* | -0.04 | -0.13 | -0.23** | -0.33** | -0.25** | 0.06 | 0.32** | 1.00 | |
| 13. T1 RCAD | -0.17** | 0.00 | -0.07 | 0.51** | 0.43** | 0.30** | 0.25** | 0.35** | 0.28** | -0.09 | 0.33** | -0.06 | 1.00 |
| Percent, M(SD) | 54% | 49% | 13.06 (0.90) | 10.79 (4.81) | 11.49 (5.42) | 11.65 (5.21) | 12.26 (5.74) | 12.47 (6.67) | 12.70 (6.06) | 215.94 (101.18) | 4.47 (6.33) | -3.25 (7.93) | 26.55 (16.59) |
Note. Eating attitudes variables are un-transformed for interpretability; COEDS, College Eating Disorders Screen; BIRD, Behavioral Indicator of Resilience to Distress; NA, Negative Affect; Race/ethnicity is coded 1 = white, 0 = non-white; Sex is coded 0 = female, 1 = male.
p < .05,
p < .01.
Unconditional Growth Model
Our first hypotheses theorized rates of ED-attitudes would increase over time. We examined an unconditional linear growth model and found that the model fit the data well: χ2(df=16) = 30.98, p = .014, CFI = 0.98, TLI = .98, RMSEA = 0.060 (90%CI = 0.027 - 0.092). We then compared the fit of this model to an unconditional model in which we constrained the residual variances to be equal across time points. This did not result in a significantly worse fitting model: Δχ2 =3.06, Δdf = 5; thus, we retained the linear growth model with homoscedastic residuals.
The means of both the intercept (M= 3.24, SE= 0.04, p< .001) and slope (M = 0.06, SE = 0.01, p < .001) were significant. Consistent with hypothesis one, these results suggest that youths' initial levels of ED-attitudes were significantly greater than zero and increase across adolescence. Further, both the variances of the mean (variance = 0.29, SE= 0.04, p < .001) and slope (variance = 0.01, SE= 0.002, p < .001) were significant, supporting the inclusion of predictors of individual differences around these estimates. The slope and intercept, however, were not correlated with each other (r= .01, p = .388).
Conditional Growth Models
In order to examine the effect of early distress intolerance on changes in ED-attitudes, we first looked at a model in which the latent intercept and slope were predicted by demographic factors, including children's sex, ethnicity, and age at baseline. Only sex was a significant predictor of the intercept (β = -0.39, p < .001), suggesting that girls report significantly greater levels of ED-attitudes at baseline than boys. Sex was therefore retained for inclusion in all consequent models.
Next, we tested whether internalizing symptoms predicted increases in ED-attitudes by including both internalizing symptoms and sex as predictors of the intercept and slope of the latent growth curve. The model fit the data well: χ2(df=29) = 45.04, p = .029, CFI = 0.98, TLI = .98, RMSEA = 0.047 (90%CI = 0.000 – 0.073). Estimates suggest that internalizing symptoms are a significant predictor of the intercept only (β = 0.52, p < .001), indicating that higher levels of internalizing symptoms are associated with initial ED-attitudes, but not changes in these attitudes over time.
We then examined a model in which both BIRD and sex as predictors of COEDS intercept and slope continued to fit the data well: χ2(df=29) = 41.32, p = .065, CFI = 0.98, TLI = .98, RMSEA = 0.044 (90%CI = 0.000 – 0.072). Results suggested that scores on the BIRD significantly predicted initial levels of ED-attitudes only (β = -.065, p = .023), indicating that higher distress intolerance at baseline was associated with higher initial levels of ED-attitudes. Contrary to our hypothesis, however, the BIRD did not predict changes in ED-attitudes over time.
We also looked at a model testing whether increases in negative emotions following the BIRD were associated with changes in risk for ED across adolescence, controlling for both pre-BIRD negative affect, BIRD scores, and sex. We found that the model fit the data well: χ2(df=37) = 60.76, p = .001, CFI = 0.96, TLI = .96, RMSEA = 0.054 (90%CI = 0.028 – 0.078). Pre-BIRD negative affect scores significantly predicted initial levels of the ED-attitudes indicating that participants who reported higher levels of negative affect before beginning the DT task also evidenced greater rates of ED-attitudes. Only affect reactivity, however, significantly predicted the increase in ED-attitudes over time, controlling for all other predictors (β = -.27, p = .023). These results suggest that youth who evidence greater increases in negative affect following the BIRD task also experienced greater increases in ED-attitudes across adolescence.
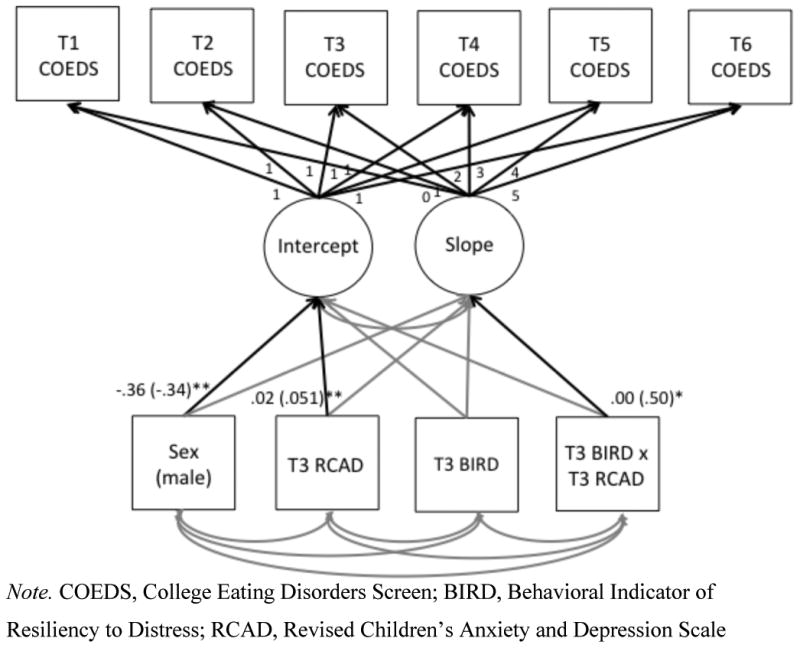
Finally, we examined two separate models in which we included the interaction of the BIRD with (1) internalizing symptoms and (2) affect reactivity (controlling for initial levels of negative affect). The first model (see Figure 1) included internalizing symptoms, the BIRD, and a BIRD x internalizing interaction term (controlling for sex) as predictors of the intercept and slope. This model fit the data well: χ2(df=37) = 52.49, p = .047, CFI = 0.98, TLI = .98, RMSEA = 0.044 (90%CI = 0.005 – 0.069). Results suggest that the interaction term significantly predicted the slope but not the intercept. Follow-up analyses indicate a significant effect of internalizing symptoms on the relation between BIRD scores and ED-attitudes, such that distress intolerant youth who report greater levels of internalizing symptoms at baseline experienced steeper increases in ED-attitudes over time, compared to youth who evidenced greater distress tolerance. Our second model also fit the data well: χ2(df=37) = 52.49, p = .047, CFI = 0.98, TLI = .98, RMSEA = 0.044 (90%CI = 0.005 – 0.069); however, the interaction between the BIRD and affect reactivity was not a significant predictor of the intercept or slope.
Figure 1. Latent growth curve model with significant standardized (and unstandardized) estimates.
Discussion
Consistent with our hypotheses and previous research, ED-attitudes increased from early adolescence through early adulthood. Baseline levels of ED-attitudes did not correlate with changes in attitudes over time, suggesting that other factors may affect changes in ED-attitudes. Distress intolerance and internalizing symptoms were associated with ED-attitudes at baseline, but were not predictive of change over time as initially hypothesized, although distress intolerance and internalizing symptoms did interact to predict change in attitudes over time. Affect reactivity, however, was significantly associated with baseline ED-attitudes as well as changes in ED-attitudes across adolescence.
The finding that distress intolerance was concurrently (but not longitudinally) associated with ED-attitudes provides the first evidence that distress intolerance is associated with ED cognitions in youth. Importantly, while distress intolerance was not associated with changes over time, it did interact with internalizing symptoms to predict increases in ED-attitudes across adolescence. Internalizing symptoms appear to strengthen the relationship between distress intolerance and ED-attitudes over time and this interaction may be an important predictor for the eventual development of further ED-attitudes (and perhaps ED behaviors) over time. For distress intolerant youth, ED symptoms may feed into worsening of ED-attitude symptoms, such as body dissatisfaction. Specifically, distress intolerance in youth with increased internalizing symptoms may trigger a desire to seek out cognitive avenues through which to control or shift focus from their internalizing symptoms (e.g., general anxiety or depression), such as by increasing worry or concerns over one's body shape or weight (i.e., ED-attitudes; see Figure 2 for a visual depiction and extended explanation of this theoretical model). For those whose ED-attitudes transition to ED behaviors, distress intolerance may lead individuals to engage in ED symptoms to serve a negative reinforcement function (i.e., to modulate internalizing symptoms), which, over time, could decrease one's future ability to tolerate internalizing symptoms without engaging in a maladaptive behavior. This process may ultimately maintain ED-attitudes and behavioral symptoms over time.
Figure 2. Proposed model of internalizing symptoms and distress tolerance in association with ED-attitudes and behaviors.
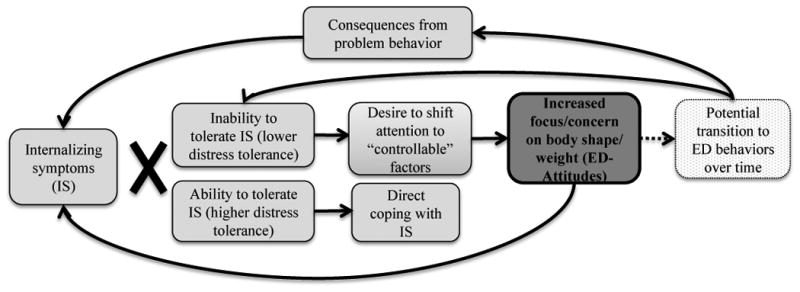
The above figure depicts a proposed model of increased ED-symptoms as supported by our findings. Internalizing symptoms interact with distress tolerance. Those with high distress tolerance are able to directly cope with internalizing symptoms, while those with low distress tolerance seek to place cause of their negative affect on a perceived “controllable” factor, such as body shape and weight. Increased ED-attitudes likely increase overall internalizing symptoms. ED-attitudes are a risk factor for the development of ED behaviors. Those who transition to ED behaviors over time reinforce the inability to tolerate distress, in addition to experiencing increased internalizing symptoms due to the social, physical, and psychological consequences incurred by ED behaviors.
A longitudinal relationship also emerged for affect reactivity, which predicted ED attitude increases. This predictive effect of affect reactivity is consistent with other studies that found that increases in negative affect in response to stressors predict subsequent disordered eating behaviors (e.g. Goldschmidt et al. (2014)) and is the first evidence that affect reactivity predicts the later development, or worsening, of ED-attitudes. Affect reactivity in response to a challenging task, such as the BIRD, may be associated with latent trait perfectionisms within the dimension of evaluative concern (i.e., self-criticism and concern about others' criticism). Adolescents may have experienced greater changes in affect due to greater self-criticism throughout the task, and such concerns over making mistakes have been found to predict later ED cognitive symptoms (including body dissatisfaction and a drive for thinness) both prospectively (Wade, Wilksch, Paxton, Byrne, & Austin, 2015) and retrospectively (Bulik et al., 2014). It is possible that increased affect reactivity may encourage greater reactivity to thoughts or feelings about body shape or weight, therefore increasing ED-attitudes over time. Although the COEDS only measures ED-attitudes and not specific ED symptoms, it is possible that increased affect reactivity may eventually lead youth to seek maladaptive ways to regulate their emotions (e.g., through the use of ED behaviors). This finding would be consistent with previous research implicating affect lability and deficits in emotion regulation in ED pathology (Lavender, Wonderlich, et al., 2015).
Strengths and Limitations
The current study features several strengths. First, the study used a longitudinal dataset with a large sample of adolescents. The study also used a behavioral measure of distress intolerance, which measures an individual's ability to tolerate distress as opposed to their perception of that ability as normally assessed with self-report measures (Leyro, Zvolensky, & Bernstein, 2010). Finally, this work examines distress intolerance from a developmental perspective, which has largely been investigated in adult populations.
The study also has limitations that should be noted for future research. We were not able to include a measure of ED-behaviors, which in addition to our measure of ED-attitudes, would have provided us with a more comprehensive examination of the development of ED vulnerability over adolescence. Second, the study relied on self-report measures of negative affect, which are subjective ratings (although perceived negative affect may be a key component of affect reactivity). Additionally, it is possible that our time period of analyses (approximately age 13 at baseline) was too late to capture the development of some of our constructs of interest. Finally, our behavioral measure of distress intolerance did not assess tolerance for specific types of stress that may be more frequently associated with ED behavior. However, the predictive ability of affect reactivity across a general stressor may suggest an underlying process that is susceptible to more specific mood states.
Conclusions and Future Directions
The current study is the first to assess the individual and combined predictive ability of several constructs related to negative affect in the development of ED attitudes during adolescence. Our results suggest that affect reactivity alone and the combined effect of high internalizing symptoms and high distress intolerance during early adolescence are risk factors for the later development of ED-attitudes. Future research is needed to replicate and extend these findings. For example, the use of momentary assessments with adolescents could allow researchers to assess affective variable and ED behavior in a momentary manner. Physiological indices of negative affect could also provide additional data related to affect reactivity. Should our findings be replicated using clinical samples and additional methods of measurement, future efforts at ED treatment development and prevention could be directed towards modifying Dialectical Behavior Therapy (DBT; Linehan, 1993), an empirically-supported treatment approach that targets emotion regulation deficits (such as affect lability and distress intolerance), for youth with eating pathology. However, more research is necessary to provide a more precise direction for treatment development and prevention efforts for EDs in youth and adolescence.
Acknowledgments
The current study was funded by a grant from the National Institute of Drug Abuse (R01DA18647) to Dr. Lejuez, and funding from the National Institutes of Mental Health to Dr. Juarascio (K23MH105680) and Ms. Manasse (F31MH108279)
Abbreviations
- ED
Eating disorder
- BIRD
Behavioral Indicator of Resiliency to Distress
- COEDS
College Eating Disorders Screen
- PANAS-C
Positive and Negative Affect Schedule for Children
- RCADS
Revised Children's Anxiety and Depression Scale
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Bakalar JL, Shank LM, Vannucci A, Radin RM, Tanofsky-Kraff M. Recent Advances in Developmental and Risk Factor Research on Eating Disorders. Current Psychiatry Reports. 2015;17(6):1–10. doi: 10.1007/s11920-015-0585-x. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Tozzi F, Anderson C, Mazzeo SE, Aggen S, Sullivan PF. The relation between eating disorders and components of perfectionism. American Journal of Psychiatry. 2014;160(2):366e368. doi: 10.1176/appi.ajp.160.2.366. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour research and therapy. 2000;38(8):835–855. doi: 10.1016/s0005-7967(99)00130-8. [DOI] [PubMed] [Google Scholar]
- Corstorphine E, Mountford V, Tomlinson S, Waller G, Meyer C. Distress tolerance in the eating disorders. Eating behaviors. 2007;8(1):91–97. doi: 10.1016/j.eatbeh.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Danielson CK, Ruggiero KJ, Daughters SB, Lejuez CW. Distress tolerance, risk-taking propensity, and PTSD symptoms in trauma-exposed youth: Pilot study. The Behavior Therapist. 2010;33:28–34. [Google Scholar]
- Dir AL, Karyadi K, Cyders MA. The uniqueness of negative urgency as a common risk factor for self-harm behaviors, alcohol consumption, and eating problems. Addictive behaviors. 2013;38(5):2158–2162. doi: 10.1016/j.addbeh.2013.01.025. [DOI] [PubMed] [Google Scholar]
- Fairburn CG. Cognitive behaviour therapy and eating disorders. Guilford Press; New York: 2008. [Google Scholar]
- Goldschmidt AB, Wonderlich SA, Crosby RD, Engel SG, Lavender JM, Peterson CB, Mitchell JE. Ecological momentary assessment of stressful events and negative affect in bulimia nervosa. Journal of consulting and clinical psychology. 2014;82(1):30. doi: 10.1037/a0034974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hambrook D, Oldershaw A, Rimes K, Schmidt U, Tchanturia K, Treasure J, Chalder T. Emotional expression, self-silencing, and distress tolerance in anorexia nervosa andchronic fatigue syndrome. British Journal of Clinical Psychology. 2011;50(3):310–325. doi: 10.1348/014466510X519215. [DOI] [PubMed] [Google Scholar]
- Holm-Denoma JM, Hankin BL, Young JF. Developmental trends of eating disorder symptoms and comorbid internalizing symptoms in children and adolescents. Eating Behaviors. 2014;15(2):275–279. doi: 10.1016/j.eatbeh.2014.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keshaviah A, Edkins K, Hastings ER, Krishna M, Franko DL, Herzog DB, Eddy KT. Re-examining premature mortality in anorexia nervosa: A meta-analysis redux. Comprehensive Psychiatry. 2014;55(8):1773–1784. doi: 10.1016/j.comppsych.2014.07.017. [DOI] [PubMed] [Google Scholar]
- Killen JD, Taylor CB, Hayward C, Wilson DM, Haydel KF, Hammer LD, Kraemer H. Pursuit of thinness and onset of eating disorder symptoms in a community sample of adolescent girls: a three-year prospective analysis. International Journal of Eating Disorders. 1994;16(3):227–238. doi: 10.1002/1098-108x(199411)16:3<227::aid-eat2260160303>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Kotler LA, Cohen P, Davies M, Pine DS, Walsh BT. Longitudinal relationships between childhood, adolescent, and adult eating disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(12):1434–1440. doi: 10.1097/00004583-200112000-00014. [DOI] [PubMed] [Google Scholar]
- Laurent J, Catanzaro SJ, Joiner TE, Jr, Rudolph KD, Potter KI, Lambert S, Gathright T. A measure of positive and negative affect for children: scale development and preliminary validation. Psychological Assessment. 1999;11(3):326. [Google Scholar]
- Lavender JM, Happel K, Anestis MD, Tull MT, Gratz KL. The interactive role of distress tolerance and eating expectancies in bulimic symptoms among substance abusers. Eating Behaviors. 2015;16:88–91. doi: 10.1016/j.eatbeh.2014.10.006. [DOI] [PubMed] [Google Scholar]
- Lavender JM, Wonderlich SA, Engel SG, Gordon KH, Kaye WH, Mitchell JE. Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: A conceptual review of the empirical literature. Clinical Psychology Review. 2015;40:111–122. doi: 10.1016/j.cpr.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez CW, Daughters SB, Danielson CW, Ruggiero K. The behavioral indicator of resiliency to distress (BIRD) 2006 [Unpublished manual] [Google Scholar]
- Leon GR, Fulkerson JA, Perry CL, Keel PK, Klump KL. Three to four year prospective evaluation of personality and behavioral risk factors for later disordered eating in adolescent girls and boys. Journal of Youth and Adolescence. 1999;28(2):181–196. [Google Scholar]
- Lewinsohn PM, Striegel-Moore RH, Seeley JR. Epidemiology and natural course of eating disorders in young women from adolescence to young adulthood. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(10):1284–1292. doi: 10.1097/00004583-200010000-00016. [DOI] [PubMed] [Google Scholar]
- Linehan M. Cognitive-behavioral treatment of borderline personality disorder. Guilford Press; 1993. [Google Scholar]
- Lingswiler VM, Crowther JH, Stephens MAP. Emotional reactivity and eating in binge eating and obesity. Journal of Behavioral Medicine. 1987;10(3):287–299. doi: 10.1007/BF00846542. [DOI] [PubMed] [Google Scholar]
- Little RJ. A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association. 1988;83(404):1198–1202. [Google Scholar]
- Little RJ, Rubin DB. The analysis of social science data with missing values. Sociological Methods & Research. 1989;18(2-3):292–326. [Google Scholar]
- Little RJA. The Bayesian approach to sample survey inference. Analysis of Survey Data. 2003:49–57. [Google Scholar]
- Measelle JR, Stice E, Hogansen JM. Developmental trajectories of co-occurring depressive, eating, antisocial, and substance abuse problems in female adolescents. Journal of Abnormal Psychology. 2006;115(3):524. doi: 10.1037/0021-843X.115.3.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus (version 6) Los Angeles, CA: Muthén & Muthén; 2010. [Google Scholar]
- Nowak JA, Roberson-Nay R, Strong DR, Bucceri J, Lejuez CW. Using item response theory in the development and validation of the College-Oriented Eating Disorders Screen. Eating Behaviors. 2003;4(4):345–361. doi: 10.1016/S1471-0153(03)00054-0. [DOI] [PubMed] [Google Scholar]
- Pearson CM, Guller L, McPherson L, Lejuez CW, Smith GT. Validation of an existing measure of eating disorder risk for use with early adolescents. Eating Behaviors. 2013;14(2):113–118. doi: 10.1016/j.eatbeh.2013.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine SE, Keel PK, Burt SA, Sisk CL, Neale M, Boker S, Klump KL. Exploring the relationship between negative urgency and dysregulated eating: Etiologic associations and the role of negative affect. Journal of Abnormal Psychology. 2013;122(2):433. doi: 10.1037/a0031250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweizer K. Some guidelines concerning the modeling of traits and abilities in test construction. European Journal of Psychological Assessment. 2010;26:1–2. [Google Scholar]
- Simons JS, Gaher RM. The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29(2):83–102. [Google Scholar]
- Stice E. Modeling of eating pathology and social reinforcement of the thin-ideal predict onset of bulimic symptoms. Behaviour Research and Therapy. 1998;36:931–944. doi: 10.1016/s0005-7967(98)00074-6. [DOI] [PubMed] [Google Scholar]
- Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents: Results from the national comorbidity survey replication adolescent supplement. Archives of General Psychiatry. 2011;68(7):714–723. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, Engel SG. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology. 2007;75(4):629. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Steiger JH. Structural model evaluation and modification: An interval estimation approach. Multivariate Behavioral Research. 1990;25(2):173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38(1):1–10. [Google Scholar]
- Wade TD, Wilksch SM, Paxton SJ, Byrne SM, Austin SB. How perfectionism and ineffectiveness influence growth of eating disorder risk in young adolescent girls. Behaviour Research and Therapy. 2015;66:56–63. doi: 10.1016/j.brat.2015.01.007. [DOI] [PubMed] [Google Scholar]


