Abstract
Duodenal lymphangitis carcinomatosa has been sporadically described, and little attention has been paid so far. To our knowledge, no data on radiological findings for this rare entity has been published. We report a case of duodenal lymphangitis carcinomatosa secondary to gallbladder mass in a 44-year-old Indian man to focus on the radiological diagnosis, which was further confirmed by endoscopic-guided biopsy and immunohistochemical analysis.
Introduction
Lymphangitis carcinomatosa is a diffuse infiltration of the lymphatic channels by malignant or metastatic cells and is common in lung malignancy (1). Pulmonary lymphangitic carcinomatosis occurs in 6–8% of patients with pulmonary metastases (2). Although virtually any metastatic neoplasm can cause lymphangitic carcinomatosis, the common locations of the primary tumor are the breasts, stomach, lungs, pancreas, and prostate. The incidence of duodenal lymphangitic carcinomatosa secondary to gallbladder mass has not been documented as yet.
Case report
A 44-year-old male patient presented with persistent chronic epigastric pain and constipation for 6 months. He had a history of significant weight loss of 7 kilograms over six months and loss of appetite with intermittent vomiting. He also had a history of smoking and alcoholism for 20 years. Baseline investigations showed leukocystosis and elevated bilirubin, SGOT, SGPT, and alkaline phosphatase levels.
In view of the epigastric pain, contrast-enhanced computed tomography (CECT) of the abdomen was advised. It was performed with a GE 64-slice VCT Light speed, and images were acquired before and after administration of the contrast agent. CECT images showed an enhancing, irregular, infiltrating mass lesion within the gallbladder (Fig. 1). No evidence of pericholecystic fluid/fat stranding was seen. In addition to the gallbladder mass, the second and third part of the duodenum showed a long segment of circumferential wall thickening with loss of mural stratification, mural enhancement, and periserosal fat stranding (Fig. 2A). Multiple peripherally enhancing enlarged necrotic lymph nodes with an average size 10–15 mm were noted in the periduodenal region and at the root of the mesentery (Fig. 2B).
Figure 1.

Axial, contrast-enhanced CT of abdomen in the portal venous phase demonstrates an asymmetrical, enhancing, infiltrating gallbladder mass lesion (arrow).
Figure 2.
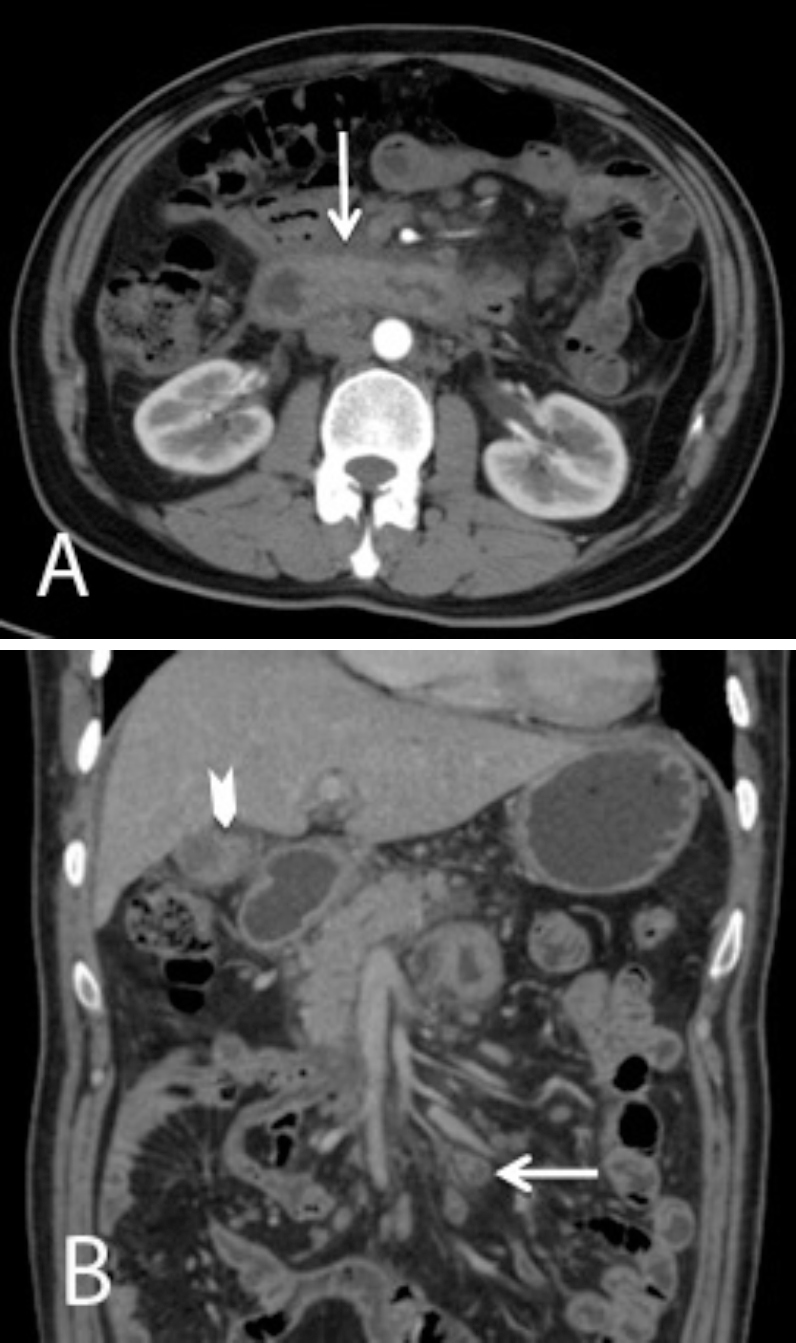
A. Axial section of abdomen with contrast in arterial phase shows long-segment circumferential wall thickening, loss of mural stratification, mural hyperenhancement, and periserosal fat stranding noted in the second and third part of duodenum (arrow). B. CT coronal section of abdomen with contrast in portal venous phase shows multiple enlarged necrotic paraduodenal and mesenteric lymph nodes (arrow). Also seen is a mass lesion involving the gallbladder (arrowhead).
Initially, the above imaging findings raised the possibilities of inflammatory etiology or a synchronous malignancy. UGI scopy showed multiple white polypoid granular lesions involving the second and third part of duodenum (Figs. 3A and B). An endoscopic-guided biopsy of the granular lesions in the duodenum was sent for immunohistochemical analysis. Microscopic examination revealed the presence of nests of tumor cells within the dilated lymphatics (Fig. 4), which suggested metastatic lymphatic spread of the malignancy. In view of the following:
-
*
An infiltrating mass lesion in the gallbladder
-
*
Diffuse, circumferential, long-segment duodenal wall thickening with adjacent lymphadenopathy
-
*
Immunohistochemical evidence of tumor cells within dilated lymphatics
Figure 3.

Upper gastrointestinal endoscopy of the second and third parts of the duodenum shows diffuse, nonulcerative, white, granular mucosal plaques (arrow) consistent with lymphangitis carcinomatosa.
Figure 4.

A. High-power (×400) view showing the tumor cell within the dilated lymphatics. B. Dilated lymphatics in the duodenal mucosa filled with tumor cells (H & E ×100).
We diagnosed duodenal lymphangitis carcinomatosa with primary gallbladder malignancy. The patient succumbed in 6 months due to advanced metastatic malignancy.
Discussion
Duodenal lymphangitis carcinomatosa has been sporadically described in the recent past. To our knowledge, no published data is available on the incidence of this rare entity. By definition, lymphangitis carcinomatosa is a diffuse infiltration of the lymphatic channels by malignant metastatic cells and is commonly encountered in lung malignancy (1). The other common malignancies that can metastasize to the intestine include end-stage adenocarcinomas of the pancreas, stomach, colon, and cervix (3). Malignant melanoma is the most common extragastrointestinal primary carcinom that can metastasize to the small bowel (4).
The etiology of lymphangitis carcinomatosa remains unclear; however, two possible mechanisms have been suggested. One hypothesis is that hematogenous tumor emboli first cause endarteritis obliterans; subsequently, an egress of tumor cells extends through the vascular walls into the perivascular lymphatics. Another theory states that there is diffuse retrograde lymphatic permeation and embolization of malignant cells. It is thought that the former is the main mode of the spread, but both mechanisms might be involved simultaneously (5).
The imaging features of duodenal neoplasm or any malignant mass lesion involving the gastrointestinal tract include focal or diffuse wall thickening of the involved bowel loop, loss of mural stratification, mural hyperenhancement, periserosal fat stranding, and adjacent lymphadenopathy (6).The imaging findings in our patient with involvement of the duodenum agreed with this.
Endoscopically, metastatic lesions to the duodenum have shown various appearances, with no single endoscopic appearance characteristic for any specific cancer or metastatic pattern (7). However, a study done by Masahiko et al showed that endoscopic findings of duodenal lymphangitis carcinomatosa are unique: multiple polypoid lesions along the Kerckring's folds covered by characteristic white, granular, nonulcerated mucosa (7). Microscopically, the tumor cells were seen in the dilated lymphatics (7). The endoscopic findings and the microscopic findings were similarly observed in our patient.
In our patient, given the presence of an infiltrating mass lesion in the gallbladder and diffuse circumferential long-segment duodenal wall thickening with adjacent lymphadenopathy, we considered a diagnosis of synchronous malignancies. Endoscopic and immunohistochemical analysis confirmed the presence of duodenal lymphangitis carcinomatosa.
Duodenal lymphangitis carcinomatosa is rare and has an extremely poor prognosis. Knowledge of this entity is very important, and it should be distinguished from ordinary metastatic duodenal carcinoma. Imaging and endoscopy-guided biopsy is mandatory, plays an important role in diagnosis, and helps the clinician provide effective management and prevent further complications.
Footnotes
Published: April 30, 2014
References
- 1.Thomas Anish, Lenox Robert. Primary lymphangitic carcinomatosis as a primary manifestation of colon cancer in a young adult. CMAJ. 2008 August 12;179(4):338–340. doi: 10.1503/cmaj.080142. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bruce DM, Heys SD, Eremin O. Lymphangitis carcinomatosa: a literature review. J R Coll Surg Edinb. 1996;41:7–13. [PubMed] [PubMed] [Google Scholar]
- 3.Kanthan Rani, Senger Jenna-Lynn, Diudeal Dana, Kanthan Selliah. A review of duodenal metastases from squamous cell carcinoma of the cervix presenting as an upper gastrointestinal bleed. World Journal of Surgical Oncology. September 2011 doi: 10.1186/1477-7819-9-113. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kanthan R, Gomez D, Senger JL, Kanthan SC. Endoscopic biopsies of duodenal polyp/mass lesions: a surgical pathology review. J Clin Pathol. 2010;63:921–925. doi: 10.1136/jcp.2010.081000. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Murin Susan. Tumor microembolism and lymphangitic carcinomatosis. Clinical pulmonary medicine. Jan 1997;4:1. [Google Scholar]
- 6.Zissin R, Osadchy A, Gayer G. Pictorial review. CT of duodenal pathology. Br J Radiol. 2002 Jan;75(889):78–84. doi: 10.1259/bjr.75.889.750078. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Nakasono Masahiko, Hirokawa Mitsuyoshi, Mugurauma Noaki, Okamura Seisuke. Duodenal lymphangitis carcinomatosa: Endoscopic characteristics and clinical significance. Journal of Gastroenterology and Hepatology. 2006;21:79–83. doi: 10.1111/j.1440-1746.2005.04203.x. [PubMed] [DOI] [PubMed] [Google Scholar]


