Abstract
Tuberculous peritonitis is a serious condition with rising prevalence in recent years. It is especially common in those patients with risk factors such as an immunocompromised state, chronic kidney disease, or cirrhosis/liver disease. Spread is typically hematogenous from pulmonary foci. We report on a 34-year-old man who presented with initial complaints of cough, low-grade fevers, abdominal pain, and nausea/vomiting. Chest x-ray showed a cluster of nodular opacities on the right upper lobe, and a CT scan showed diffuse thickening and nodularity of the omentum with prominent mesenteric lymph nodes, consistent with tuberculous peritonitis.
Introduction
Tuberculous peritonitis was first described in 1843 (1), but its prevalence had previously been declining with the advent of antituberculosis therapy and improvements in sanitation. Recently, however, its prevalence has again been rising, thought in large part to be due to the higher number of HIV-positive individuals. The peritoneum is the sixth most common extrapulmonary site in the United States; it is seen in up to 3.5% of cases of pulmonary tuberculosis (TB) and 31-58% of abdominal TB (with the remaining cases of abdominal TB involving either the gastrointestinal tract or mesenteric lymph nodes, with some overlap) (2). Other factors, such as chronic kidney disease requiring continuous ambulatory peritoneal dialysis (CAPD) (3) and cirrhosis/liver disease secondary to alcohol usage, have also been shown to be important risk factors (2). Typically, the spread of the tubercles occurs hematogenously from the pulmonary foci. Three forms have been identified: wet-ascites, fibrotic-fixed, and dry-plastic. These forms may coexist with one another.
Diagnosing this condition is difficult, given the subacute nature of the disease and its nonspecific and variable complaints (2, 4). Additionally, comorbid conditions (for example, cirrhosis) and/or age may mask the symptoms or lead to an atypical presentation. Most commonly, patients present with ascites (93%), abdominal pain (73%), and fever (58%). In addition, many patients present with distended, tender abdomens, but otherwise physical examination signs are typically nonspecific. Diagnosis is typically via ascitic fluid analysis with SAAG calculation, microbiological tests (mycobacterial culture growth), peritoneal biopsy, laparoscopy, or minilaparotomy.
Chest x-ray may show old evidence of pulmonary tuberculosis but is relative nonspecific; 38% of chest x-rays showed some abnormality, and only 14% showed active pulmonary disease (2). Other radiographic studies found in the literature show evidence of ultrasound (US) and computed tomography (CT) usefulness in peritoneal involvement (5, 6, 7, 8, 9, 10, 11, 12, 13, 14). CT imaging has been shown to be much more useful than x-ray, especially if combined with US; CT demonstrates the ascitic fluid to have higher attenuation values, a thickened peritoneum diffusely, and omental changes (such as irregular soft-tissue densities [9]). Mesenteric lymph nodes may be evident as well. CT can also help distinguish between this condition and peritoneal carcinomatosis, which typically has more nodular implants and a more irregular peritoneal thickening pattern (7, 10). US is better at revealing the multiple small septations in the peritoneum (2). Additionally, US usually shows findings of a mesenteric thickness of >15mm, an increase in mesenteric echogenicity, and mesenteric lymphadenopathy (6). Another study concluded that both CT and US should be used together for an accurate diagnosis, with CT showing omental thickening more accurately and US showing the fine, mobile septations in the peritoneum more accurately (12).
Case report
A 34-year-old man presented to our institution with complaints of cough, low-grade fevers, abdominal pain, nausea/vomiting, and a 2-week history of weight loss. His past medical history included rheumatoid arthritis with concomitant long-term use of infliximab and a PPD conversion, during which the patient underwent 11 months of isoniazid therapy. Physical examination was unremarkable. Laboratory tests showed a mild leukocytosis of 12.5 × 103 cells/mL (normal 3.8–10.6). ESR was elevated at 108 mm/hr (normal, 0-20). CRP was 16.6 mg/dL (normal 0-0.9). A chest x-ray showed a left pleural effusion and a cluster of nodular opacities in the right upper lobe. A 7-day course of moxifloxacin resulted only in mild symptom relief.
A later CT scan with contrast showed diffuse thickening and nodularity of the omentum, infiltration of the mesentery, and a small amount of hemoperitoneum. Additionally, there were multiple prominent mesenteric lymph nodes and diffuse thickening of the small bowel. In the pelvis, there was a small volume of ascites in the rectovesicle space and enhancement of the peritoneal reflections due to peritonitis (Fig. 1). During a laparascopic biopsy done two days after the CT, extensive adhesions and infiltration of the peritoneum with thickened adhesions were noted between the omentum, bowel, and abdominal wall. The small bowel was covered with micronodular inflammatory nodules typical of a miliary spread of infection (Fig 1D). An omental biopsy showed omental fat with caseating and noncaseating granulomatous inflammation with acidfast organisms, consistent with tuberculosis. Treatment began with a multidrug protocol: rifampin, ethambutol, and moxifloxacin. The patient was discharged to home after two weeks of continued medical therapy. A CXR and CT of the chest of this patient demonstrating right-upper-lobe airspace opacities can be seen in Figure 2.
Figure 1.
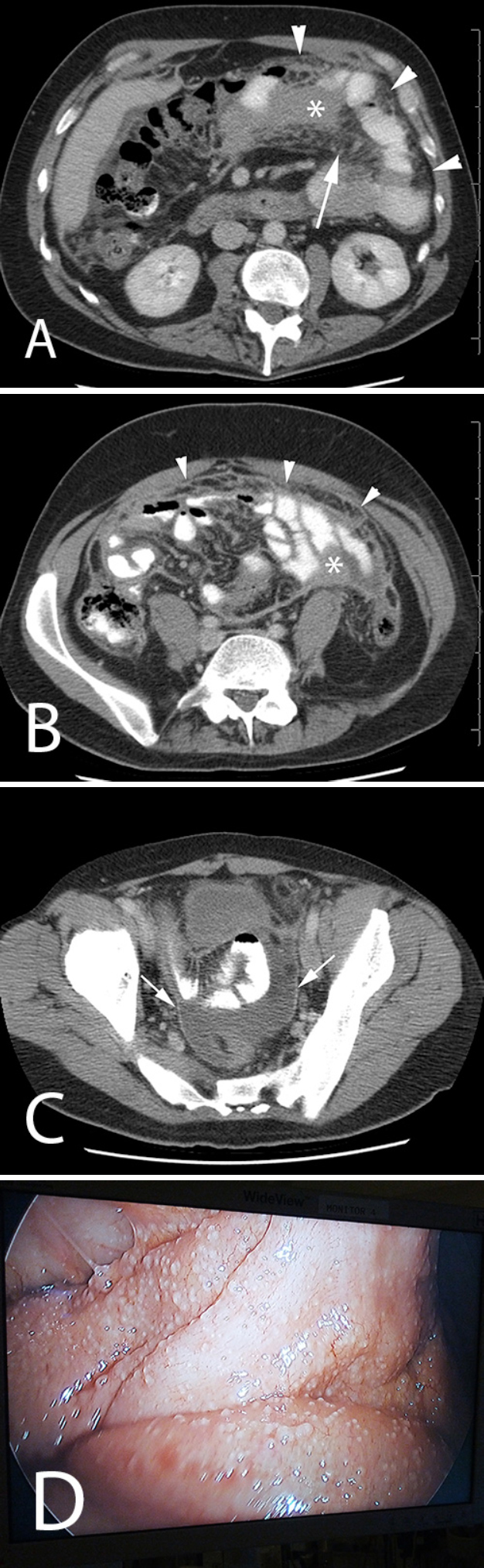
Postcontrast CT at the level of the kidneys shows diffuse thickening and nodularity of the omentum (arrowheads in A, B), infiltration of the mesentery (arrow), and a small amount of hemoperitoneum (asterisks in A, B). In B, more inferiorly, note multiple prominent mesenteric lymph nodes and diffuse thickening of the small bowel. In C, in the pelvis, note a small volume of ascites in the rectovesicle space and enhancement of the peritoneal reflections due to peritonitis. D, a photograph taken during laparoscopic biopsy, that shows the innumerable micronodules covering the surface of the small bowel. Histologically, these micronodules were found to have caseating and noncaseating granulomatous inflammation with acidfast organisms, consistent with tuberculosis.
Figure 2.
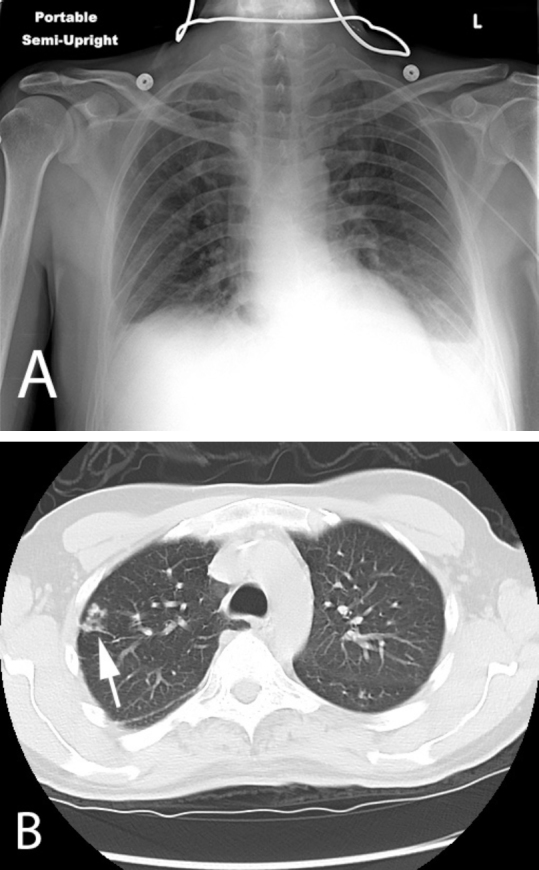
A) Portable chest radiograph and B) CT showing a subtle cluster of airspace opacities in the right upper lobe (arrow).
Discussion
Tuberculous peritonitis is difficult to diagnose, primarily due to its insidious onset and variability in radiographic findings. CT can show nonspecific findings, leading to confusion of tuberculous peritonitis with other peritoneal abnormalities, such as carcinomatosis. In these cases, clinical history becomes highly important, with quicker onset more suggestive of an infectious process.
In this patient, the initial presentation was largely consistent with reported symptoms of tuberculous peritonitis: fever, abdominal pain, and nausea/vomiting. Interestingly, the initial chest x-ray showed nodular opacities in the right upper lobe, likely of tuberculoid origin. These are consistent with theories in the literature that tuberculous peritonitis is usually secondary to a hematogenous spread from a pulmonary focus. CT findings in this patient also mirrored what has been observed in the literature: thickening/nodularity of the omentum, some ascitic fluid, infiltration of the mesentery, and involvement of the mesenteric lymph nodes. Given the time course, the history of a positive PPD in this patient, and his long-term use of infliximab, CT was fairly supportive of the diagnosis of tuberculous peritonitis, and this reflects what has been said in the literature. Regardless, a laparascopic biopsy confirmed the diagnosis.
As was seen in this case, CT is an excellent way to diagnose and view the extent of tuberculous peritonitis. Treatment for this condition is largely similar to treatment for tuberculosis elsewhere, and a multidrug protocol is used. Most importantly, clinicians must keep a high degree of suspicion of tuberculosis peritonitis in patients who present with insidious abdominal signs, and especially in patients who would otherwise be predisposed to it (immunosuppressed/immunocompromised, cirrhotic patients, prior history of tuberculosis). In addition, CT is an excellent tool to evaluate for this possibility, as well as to gauge the extent of the spread. Together with clinical history, radiographic findings can help quickly point the diagnosis towards tuberculous peritonitis.
Footnotes
Published: July 11, 2014
References
- 1.Dineeen P, Homan WP, Grafe WR. Tuberculous peritonitis: 43 years' expereince in diagnosis and treatment. Annals of surgery. Dec 1976;184(6):717–722. doi: 10.1097/00000658-197612000-00010. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sanai FM, Bzeizi KI. Systematic review: tuberculous peritonitis–presenting features, diagnostic strategies and treatment. Alimentary pharmacology & therapeutics. Oct 15 2005;22(8):685–700. doi: 10.1111/j.1365-2036.2005.02645.x. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Ram R, Swarnalatha G, Akpolat T, Dakshinamurty KV. Mycobacterium tuberculous peritonitis in CAPD patients: a report of 11 patients and review of literature. International urology and nephrology. Aug 2013;45(4):1129–1135. doi: 10.1007/s11255-012-0311-0. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Mamo JP, Brij SO, Enoch DA. Abdominal tuberculosis: a retrospective review of cases presenting to a UK district hospital. QJM : monthly journal of the Association of Physicians. Apr 2013;106(4):347–354. doi: 10.1093/qjmed/hct003. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Akhan O, Pringot J. Imaging of abdominal tuberculosis. European radiology. Feb 2002;12(2):312–323. doi: 10.1007/s003300100994. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Jain R, Sawhney S, Bhargava DK, Berry M. Diagnosis of abdominal tuberculosis: sonographic findings in patients with early disease. AJR. American journal of roentgenology. Dec 1995;165(6):1391–1395. doi: 10.2214/ajr.165.6.7484572. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Ha HK, Jung JI, Lee MS. CT differentiation of tuberculous peritonitis and peritoneal carcinomatosis. AJR. American journal of roentgenology. Sep 1996;167(3):743–748. doi: 10.2214/ajr.167.3.8751693. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Lundstedt C, Nyman R, Brismar J, Hugosson C, Kagevi I. Imaging of tuberculosis. II. Abdominal manifestations in 112 patients. Acta Radiol. Jul 1996;37(4):489–495. doi: 10.1177/02841851960373P213. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Epstein BM, Mann JH. CT of abdominal tuberculosis. AJR. American journal of roentgenology. Nov 1982;139(5):861–866. doi: 10.2214/ajr.139.5.861. [PubMed] [DOI] [PubMed] [Google Scholar]
- 10.Rodriguez E, Pombo F. Peritoneal tuberculosis versus peritoneal carcinomatosis: distinction based on CT findings. Journal of computer assisted tomography. Mar-Apr 1996;20(2):269–272. doi: 10.1097/00004728-199603000-00018. [PubMed] [DOI] [PubMed] [Google Scholar]
- 11.Sheikh M, Abu-Zidan F, al-Hilaly M, Behbehani A. Abdominal tuberculosis: comparison of sonography and computed tomography. Journal of clinical ultrasound : JCU. Sep 1995;23(7):413–417. doi: 10.1002/jcu.1870230704. [PubMed] [DOI] [PubMed] [Google Scholar]
- 12.Demirkazik FB, Akhan O, Ozmen MN, Akata D. US and CT findings in the diagnosis of tuberculous peritonitis. Acta Radiol. Jul 1996;37(4):517–520. doi: 10.1177/02841851960373P217. [PubMed] [DOI] [PubMed] [Google Scholar]
- 13.Denton T, Hossain J. A radiological study of abdominal tuberculosis in a Saudi population, with special reference to ultrasound and computed tomography. Clinical radiology. Jun 1993;47(6):409–414. doi: 10.1016/s0009-9260(05)81062-1. [PubMed] [DOI] [PubMed] [Google Scholar]
- 14.Lee DH, Lim JH, Ko YT, Yoon Y. Sonographic findings in tuberculous peritonitis of wet-ascitic type. Clinical radiology. Nov 1991;44(5):306–310. doi: 10.1016/s0009-9260(05)81264-4. [PubMed] [DOI] [PubMed] [Google Scholar]


