Abstract
The estrogen receptor alpha (ERα) is highly expressed in both endometrial and breast cancers, and represents the most prevalent therapeutic target in breast cancer. However, anti-estrogen therapy has not been shown to be effective in endometrial cancer. Recently it has been shown that hormone-binding domain alterations of ERα in breast cancer contribute to acquired resistance to anti-estrogen therapy. In analyses of genomic data from The Cancer Genome Atlas (TCGA), we observe that endometrial carcinomas manifest recurrent ESR1 gene amplifications that truncate the hormone-binding domain encoding region of ESR1 and are associated with reduced mRNA expression of exons encoding the hormone-binding domain. These findings support a role for hormone-binding alterations of ERα in primary endometrial cancer, with potentially important therapeutic implications.
Endometrial cancer (EC) is the fourth most common malignancy of women and the most common pelvic gynecological malignancy in countries with advanced industrialization1,2. But approved targeted therapies are still not in use today3,4. ERα, encoded by the gene ESR1, is known to be an important driver of cell proliferation5 and has been identified as a risk locus in breast cancer6,7. Both breast as well as endometrial cancer are estrogen dependent and express the estrogen receptor alpha (ERα) to a similar extent8,9,10,11.
While ERα constitutes the most frequently inhibited therapeutic target in breast cancer9, anti-estrogen therapy has shown inconsistent results and mostly a very limited effect in endometrial cancers12,13,14,15,16,17,18. The estrogen antagonist Tamoxifen can even increase the risk of carcinogenesis19,20,21. Consequently anti-estrogen therapy does not constitute a component of standard therapy of EC3,4. Since mutations and alternative splicing of ESR1 that alter the hormone-binding domain have been shown to generate hormone independence or resistance to anti-estrogen therapy in breast and endometrial cancers22,23,24,25,26,27,28,29,30,31, related genetic alterations could play a role for therapy outcome in primary endometrial carcinoma.
Recent studies identified mutations of ESR1 in breast cancer that alter their hormone binding domain coding sequence, to be linked to endocrine therapy resistance in a metastatic setting26,27,28. One study by Li et al. even demonstrates an ESR1 fusion in endocrine treatment resistant breast cancer, truncating the hormone-binding domain coding exons28, while a later study by Veeraraghavan et al. identified evidence for another type of recurrent ERα-altering gene fusions in this tumor type32. However, structural genetic alterations of ESR1 have not been suggested to play a role in endometrial cancer carcinogenesis. Due to the potential importance of such ESR1 alterations in endometrial cancer, we analyzed an tumor test subset of 29 primary endometrial cancers for somatic gene copy-number alterations (SCNA) and explored The Cancer Genome Atlas (TCGA)33 for concerning SCNA and mRNA expression data of endometrial carcinoma.
Results
Across a cancer study subset of 29 primary endometrial carcinomas that had gone on to metastasize, we characterized the copy-number changes by GeneChips and validated amplifications of ESR1 in these cancers by fluorescence in-situ hybridization (FISH). The Pearson correlation of ESR1 GeneChip copy numbers with FISH determined absolute average ESR1 copy numbers per nucleus and average ESR1 to centromere 6 (CEN6) ratios were r = 0.743 (p < 0.001) and r = 0.774 (p < 0.001) respectively (Appendix A, Fig. 1, Supplementary Figures S1 and S2, Supplementary Optical Dataset S1).
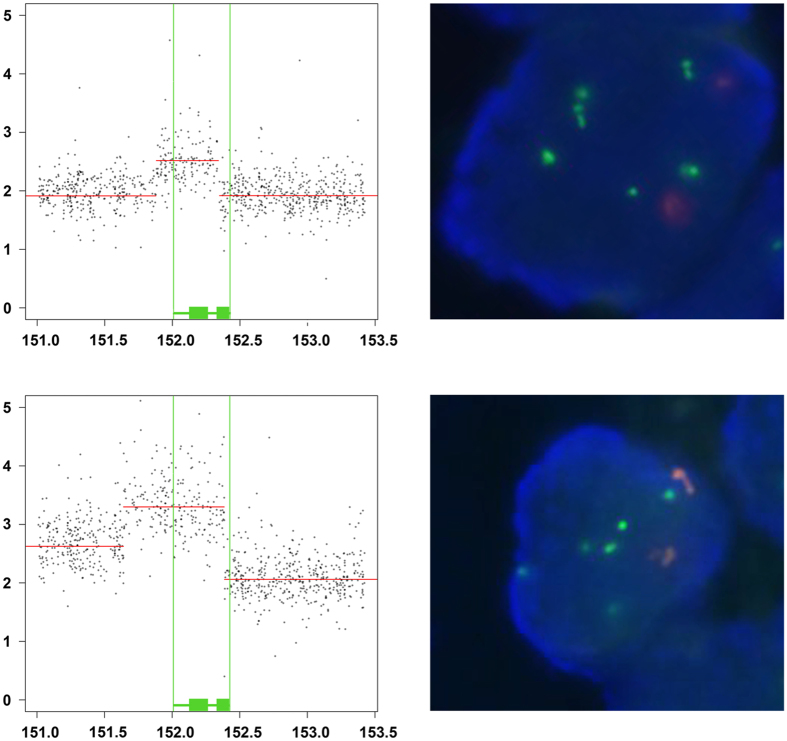
Figure 1. Truncated ESR1 amplifications in two metastatic endometrial carcinomas.
Dot plots of ESR1 copy-numbers (y-axis) determined by GeneChip measurements (grey dots) of two metastatic endometrial carcinomas (above: #4, below #2) are shown on the left. Horizontal red lines indicate the segmented copy-number level of chromosomal positions (mega base pairs) on chromosome 6 (x-axis). Position of full length ESR1 (vertical green lines) as well as ESR1 exons 1-4 and 5-8 are indicated as green rectangles (see also Figure 2). Regarding FISH signals of ESR1 (green) and centromere 6 (orange) within a tumor nucleus (blue) are shown on the right. FISH and regarding GeneChip copy-number data of 28 metastatic endometrial carcinoma are summarized in Appendix A. FISH analyses of these tumors are documented in Supplementary Optical Dataset S1.
Four of these tumors exhibited focal ESR1 amplification determined by GeneChips, of which two amplifications showed 3′ truncations of ESR1 (Δ exon 6–8 or 7–8) that would remove the hormone-binding domain (Appendix A, Fig. 1). We therefore explored the prevalence of ESR1-truncating amplifications across uterine corpus endometrial carcinoma within The Cancer Genome Atlas (TCGA)33.
Hormone-binding domain truncated ESR1 amplifications in primary endometrial cancers
In the TCGA data subset of 539 endometrial carcinomas analyzed, we identified 88 (16.3%) cases with amplifications encompassing or overlapping ESR1. 46.6% of these were histologically defined serous and 75.0% of the tumors with ESR1 amplification were clustered within the serous like copy-number high molecular subtype according to TCGA34. The ESR1 amplifications were focal (less than half a chromosome arm in length) in 36 cases (6.7%) of tumors, and had a significantly higher rate of amplification than the genome-wide average (q = 5.75 × 10−4). Mapping of the overlap between amplifications across tumors identified ESR1 only as the most likely gene target (see methods).
These amplifications appeared to truncate the hormone-binding domain encoding region in seven cases (1.3% of the entire dataset; and 19.4% of cases with focal ESR1 amplification) and to retain exons 1–4 or 1–3, encoding the n-terminal ESR1 transactivation domain (AF1) and DNA-binding domains. Another case without ESR1 amplification exhibited a heterozygous deletion of exons encoding the hormone-binding domain (Fig. 2), for a total apparent ESR1 truncation rate of 1.5% over all tumors. In one additional TCGA case, we detected a hormone-binding domain (exons 4–8) truncating ESR1-SYNE1 mRNA fusion (Appendix B). Eight of these nine tumors were molecularly classified as being in the serous like copy-number high subgroup (4.3% of this subgroup)35.
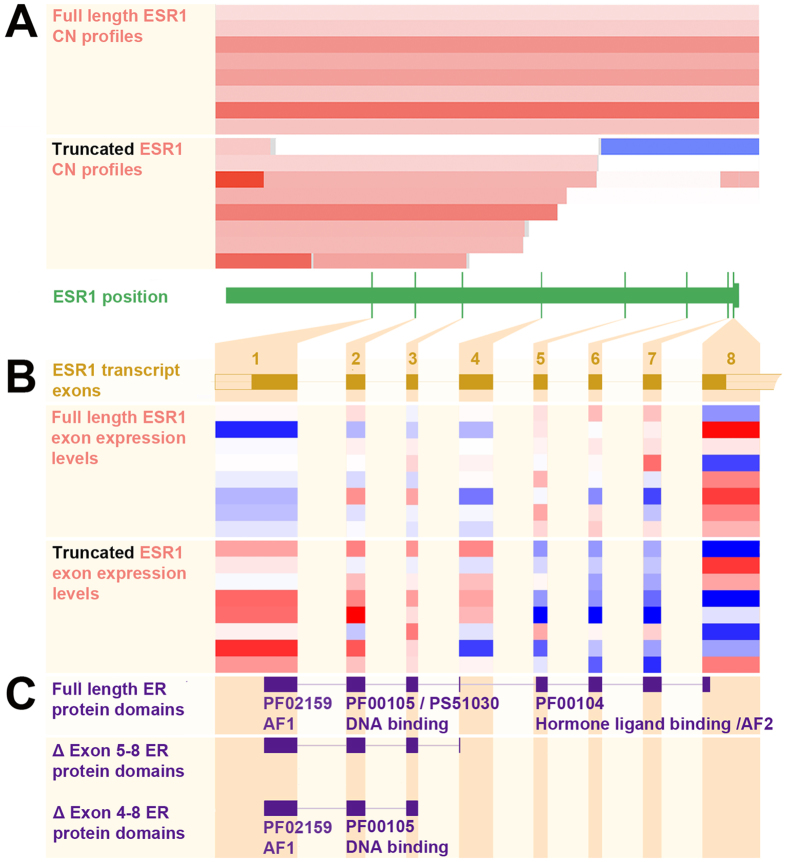
Figure 2. Truncated ESR1 amplifications in TCGA endometrial carcinomas.
Log2 ESR1 copy number ratios of eight uterine corpus endometrial carcinomas with ESR1 full-length amplification and eight carcinomas with ESR1 truncating copy-number alterations are shown in horizontal bars (increased: red, normal/neutral: white, decreased: blue) (A). The corresponding heatmap of exon expression is estimated from RNA-Seq data (normalized relative higher: red, neutral: white, lower: blue) (B). Corresponding ER protein domains according to PROSITE (PS) and Pfam (PF) databases (http://www.ebi.ac.uk/interpro/) are shown in panel C (see http://www.ensembl.orgfor ESR1 transcript variants).
Association of ESR1 exon copy numbers with mRNA expression
The ESR1 truncation events are associated with decreased mRNA expression of the truncated exons encoding the hormone-binding domain (exons 5–8) compared to the transactivation and DNA-binding domains (exons 1–4) (p < 0.001) (Fig. 2 and Appendix C). We compared the normalized ESR1 expression values estimated from RNA-Seq data for the eight tumors exhibiting amplified, truncated ESR1 to those from eight tumors selected on the basis of exhibiting similarly focal ESR1 amplifications that lack intragenic breakpoints. The average ratio between expression levels of exons 1–4 and 5–8 is 2.1-fold higher among truncated tumors relative to these controls (p = 0.003). We also confirmed this relation after replacing the eight ESR1-amplified controls with all 545 tumors profiled by TCGA. In this comparison, the ratio of expression levels between exons 1–4 and 5–8 is 2.2-fold higher in ESR1-truncated tumors (p < 0.001).
In contrast, TCGA breast cancers exhibit ESR1 truncations on DNA-level less than half as often (7 of 1080; 0.65%) as observed in endometrial cancer and had increased expression of exons 1–2, but not of the full DNA-binding domain (Appendix D). These data suggest that the amplified truncations and associated mRNA profiles we describe in endometrial cancer are not frequent in breast cancer.
Discussion
The gene truncations we report in endometrial carcinoma disrupt the hormone-binding domain encoding sequence of ESR1. Similarly, mRNA splice variants lacking one or more of exons 5–8, encoding the hormone-binding domain, have been described in normal35,36,37,38 and malignant22,23,35,36,37,39 breast as well as in normal22,40,41,42,43,44,45 and malignant42,43,44,45,46 endometrial tissue. Point mutations of the ligand binding domain encoding sequence of ESR1 have also been described to occur in both breast and endometrial cancers25,26,27,30,47,48.
Both splice variants and point mutations involving the ESR1 hormone-binding domain have been associated with hormone-independent ERα activity. The point mutations found in both breast and endometrial cancers have been shown to enable ligand-binding independent transcriptional activity26,30,48,49,50 and have been related to acquired resistance to anti-estrogen therapy in breast cancer26,27,28. Excisions of exons 5 and 7 by alternative splicing have also been shown to constitutively activate ERα22,23,30 and have been associated with hormone independent growth in both breast and endometrial cancer22,23,24,31. These findings raise the hypothesis that the ESR1 truncations we report may also generate hormone-independent ERα activity.
In breast cancer, point mutations in the ligand-binding domain occur in 20–50% of tumors that have acquired resistance to anti-estrogen therapy26,27 but only in 0.2% of primary cancers51. In endometrial cancer, however, point mutations and in-frame deletions altering the ligand binding domain occur in 2.8% of primary endometrial cancers26,51. Similarly the recurrent ESR1 truncations we report appear to be much more frequent in primary endometrial carcinoma than in primary breast cancers.
Anti-estrogen therapy with estrogen antagonists or aromatase inhibitors is standard first-line treatment for ERα-positive breast cancers, but has been associated with only a low rate (~10%) of overall response among endometrial cancers13,16,17,18 and is not a standard treatment for endometrial cancer3,4. In some cases, anti-estrogens such as Tamoxifen can even induce proliferation effect on endometrial cancer cells52,53 and normal endometrial tissue54 and increase the risk of endometrial carcinogenesis19,20,21. Splice variants of ESR1 that alter the hormone-binding domain have been associated with ERα activation by Tamoxifen in endometrial cancer cells24. The effect of estrogen antagonists on ERα encoded by the truncated forms of ESR1 that we have detected should also be tested, and all alterations of the ESR1 ligand-binding domain should be evaluated as potential biomarkers of anti-estrogen therapy resistance. Conversely, the absence of such alterations should be evaluated as a biomarker of anti-estrogen sensitivity, potentially opening up a new therapeutic option for a subset of patients with endometrial cancer.
Methods
GeneChip analysis
For our study subset of 29 primary endometrial tumors, gene copy-number data were determined by Affymetrix SNP 6.0 microarray analysis as described earlier55. GeneChip probe intensities are normalized across samples and circular binary segmentation is performed. Areas harboring germline CNVs are removed from the final segmented copy-number output. The range of birdseed call rates in this cohort was 92.6–99.3% with an average call rate of 97.1%. For TCGA copy-number data, level 3 segmented log2 copy-number data were used in analysis. For both datasets, log2 copy-number values are calculated as ratios relative to the genome wide average according to standard procedures56,57,58,59. These gene copy-number data were visualized using the IGV viewer software60. Linear gene level copy-number data were derived by GISTIC55,59. All TCGA DNA copy-number data (2015-06-01 stddata 2015-04-02 regular peel-off) can be accessed through the TCGA Copy Number Portal57.
RNA-Seq analysis
Reads per kilobase per million (RPKM)61 RNA exon expression quantification values were normalized and RPKM 0 was assigned 0.1 (Appendices C+D). Exons were compared using inverted log2 of normalized values. A two tailed Mann-Whitney-U-Test was applied to test for statistical significance of differences. P-values < 0.05 were considered statistically significant. Paired-end RNA-seq fusion transcript analysis of TCGA RNA-sequencing data from 295 tumors to detect mRNA fusions was performed using SnowShoes-FTD as described earlier62,63,64. Parameters used to define a fusion transcript of high confidence were at least two unique fusion junction spanning split reads within the dataset and at least five encompassing reads65. RNA-Seq data were taken from the TCGA database http://cancergenome.nih.gov
FISH analysis
FISH was performed without RNase treatment as described earlier66. Pearson correlation coefficients and regarding p-values (two sided t-test) were generated using SPSS (Statistical Package of Social Science) version 20.0.0 applying standard bootstrapping. P-values < 0.05 were considered statistically significant.
Tumor samples and DNA extraction
This study has been approved by the Norwegian Data Inspectorate (961478-2), the Norwegian Social Science Data Services (15501) and the local Institutional Review Board (REKIII nr. 052.01) and the BROAD institute, MA, USA and methods were carried out in accordance with these approved guidelines. The 29 metastatic high grade primary tumor samples were obtained with documented informed consent in a patient based setting (Sept 2002-Sept 2012) from the Department of Obstetrics and Gynaecology, Section of Gynaecological Cancer, Haukeland University Hospital, Bergen, Norway. Biopsies were snap frozen in nitrogen and stored at minus 80 °C until DNA extraction. Tumor purity was assessed based on histology sections obtained by microtome prior to DNA extraction. DNA extraction was performed using samples with estimated tumor purity ≥50% as previously described7.
Additional Information
How to cite this article: Holst, F. et al. Recurrent hormone-binding domain truncated ESR1 amplifications in primary endometrial cancers suggest their implication in hormone independent growth. Sci. Rep. 6, 25521; doi: 10.1038/srep25521 (2016).
Supplementary Material
Footnotes
Frederik Holst has royalty interest associated with intellectual property of ZytoVision GmbH concerning patent US8101352B2 “Detection of ESR1 Amplification in Breast Cancer” and according EU patent application. Mathew Meyerson and Andrew Cherniack receive research support from Bayer AG.
Author Contributions F.H. and A.D.C. designed and conducted the analyses, and prepared the manuscript, together with support from E.A.H., W.J.G., A.T., S.E.S., Y.W.A., P.G., J.T., B.M.N., E.A.T., M.M., R.B. and H.B.S.
References
- Parkin D. M., Bray F., Ferlay J. & Pisani P. Global cancer statistics, 2002. CA Cancer J Clin 55, 74–108 (2005). [DOI] [PubMed] [Google Scholar]
- Jemal A. et al. Global cancer statistics. CA Cancer J Clin 61, 69–90 (2011). [DOI] [PubMed] [Google Scholar]
- Salvesen H. B., Haldorsen I. S. & Trovik J. Markers for individualised therapy in endometrial carcinoma. Lancet Oncol 13, e353–e361 (2012). [DOI] [PubMed] [Google Scholar]
- Morice P., Leary A., Creutzberg C., Abu-Rustum N. & Darai E. Endometrial cancer. Lancet 387, 1094–1108 (2016). [DOI] [PubMed] [Google Scholar]
- Zabransky D. J. & Park B. H. Estrogen receptor and receptor tyrosine kinase signaling: use of combinatorial hormone and epidermal growth factor receptor/human epidermal growth factor receptor 2-targeted therapies for breast cancer. J Clin Oncol 32, 1084–1086 (2014). [DOI] [PubMed] [Google Scholar]
- Yue W., Yager J. D., Wang J. P., Jupe E. R. & Santen R. J. Estrogen receptor-dependent and independent mechanisms of breast cancer carcinogenesis. Steroids 78, 161–170 (2013). [DOI] [PubMed] [Google Scholar]
- Li Q. et al. Integrative eQTL-based analyses reveal the biology of breast cancer risk loci. Cell 152, 633–641 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jongen V. et al. Expression of estrogen receptor-alpha and -beta and progesterone receptor-A and -B in a large cohort of patients with endometrioid endometrial cancer. Gynecol Oncol 112, 537–542 (2009). [DOI] [PubMed] [Google Scholar]
- Burstein H. J. et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: american society of clinical oncology clinical practice guideline focused update. J Clin Oncol 32, 2255–2269 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wik E. et al. Lack of estrogen receptor-alpha is associated with epithelial-mesenchymal transition and PI3K alterations in endometrial carcinoma. Clin Cancer Res 19, 1094–1105 (2013). [DOI] [PubMed] [Google Scholar]
- Silverberg S. G. et al. Tumours of the uterine corpus: Epithelial tumors and related lesions. In Pathology and Genetics of Tumours of the Breast and Female Genital Organs (eds. Tavassoli F. A. & Devilee P.) 221–249 (IARC Press, Lyon, 2003). [Google Scholar]
- Rendina G. M., Donadio C., Fabri M., Mazzoni P. & Nazzicone P. Tamoxifen and medroxyprogesterone therapy for advanced endometrial carcinoma. Eur J Obstet Gynecol Reprod Biol 17, 285–291 (1984). [DOI] [PubMed] [Google Scholar]
- Thigpen T., Brady M. F., Homesley H. D., Soper J. T. & Bell J. Tamoxifen in the treatment of advanced or recurrent endometrial carcinoma: a Gynecologic Oncology Group study. J Clin Oncol 19, 364–367 (2001). [DOI] [PubMed] [Google Scholar]
- Pandya K. J. et al. Megestrol and tamoxifen in patients with advanced endometrial cancer: an Eastern Cooperative Oncology Group Study (E4882). Am J Clin Oncol 24, 43–46 (2001). [DOI] [PubMed] [Google Scholar]
- Kokka F., Brockbank E., Oram D., Gallagher C. & Bryant A. Hormonal therapy in advanced or recurrent endometrial cancer. Cochrane Database Syst Rev CD007926 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma B. B. et al. The activity of letrozole in patients with advanced or recurrent endometrial cancer and correlation with biological markers–a study of the National Cancer Institute of Canada Clinical Trials Group. Int J Gynecol Cancer 14, 650–658 (2004). [DOI] [PubMed] [Google Scholar]
- Rose P. G. et al. A phase II trial of anastrozole in advanced recurrent or persistent endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol 78, 212–216 (2000). [DOI] [PubMed] [Google Scholar]
- Lindemann K. et al. Examestane in advanced or recurrent endometrial carcinoma: a prospective phase II study by the Nordic Society of Gynecologic Oncology (NSGO). BMC Cancer 14, 68 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College of, O. & Gynecologists Committee on Gynecologic, P. ACOG committee opinion. No. 336: Tamoxifen and uterine cancer. Obstet Gynecol 107, 1475–8 (2006). [DOI] [PubMed]
- Fisher B. et al. Endometrial cancer in tamoxifen-treated breast cancer patients: findings from the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-14. J Natl Cancer Inst 86, 527–537 (1994). [DOI] [PubMed] [Google Scholar]
- Bernstein L. et al. Tamoxifen therapy for breast cancer and endometrial cancer risk. J Natl Cancer Inst 91, 1654–1662 (1999). [DOI] [PubMed] [Google Scholar]
- Fuqua S. A. et al. Variant human breast tumor estrogen receptor with constitutive transcriptional activity. Cancer Res 51, 105–109 (1991). [PubMed] [Google Scholar]
- Castles C. G., Fuqua S. A., Klotz D. M. & Hill S. M. Expression of a constitutively active estrogen receptor variant in the estrogen receptor-negative BT-20 human breast cancer cell line. Cancer Res 53, 5934–5939 (1993). [PubMed] [Google Scholar]
- Horvath G., Leser G., Helou K. & Henriksson M. Function of the exon 7 deletion variant estrogen receptor alpha protein in an estradiol-resistant, tamoxifen-sensitive human endometrial adenocarcinoma grown in nude mice. Gynecol Oncol 84, 271–279 (2002). [DOI] [PubMed] [Google Scholar]
- Herynk M. H. & Fuqua S. A. Estrogen receptor mutations in human disease. Endocr Rev 25, 869–898 (2004). [DOI] [PubMed] [Google Scholar]
- Robinson D. R. et al. Activating ESR1 mutations in hormone-resistant metastatic breast cancer. Nat Genet 45, 1446–1451 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toy W. et al. ESR1 ligand-binding domain mutations in hormone-resistant breast cancer. Nat Genet 45, 1439–1445 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S. et al. Endocrine-therapy-resistant ESR1 variants revealed by genomic characterization of breast-cancer-derived xenografts. Cell Rep 4, 1116–1130 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuqua S. A., Gu G. & Rechoum Y. Estrogen receptor (ER) alpha mutations in breast cancer: hidden in plain sight. Breast Cancer Res Treat 144, 11–19 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weis K. E., Ekena K., Thomas J. A., Lazennec G. & Katzenellenbogen B. S. Constitutively active human estrogen receptors containing amino acid substitutions for tyrosine 537 in the receptor protein. Mol Endocrinol 10, 1388–1398 (1996). [DOI] [PubMed] [Google Scholar]
- Lemieux P. & Fuqua S. The role of the estrogen receptor in tumor progression. J Steroid Biochem Mol Biol 56, 87–91 (1996). [DOI] [PubMed] [Google Scholar]
- Veeraraghavan J. et al. Recurrent ESR1-CCDC170 rearrangements in an aggressive subset of oestrogen receptor-positive breast cancers. Nat Commun 5, 4577 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- TCGA Research Network: The Cancer Genome Atlas (2010). http://cancergenome.nih.gov/ Date of access: 21/07/2015.
- Cancer Genome Atlas Research, N. et al. Integrated genomic characterization of endometrial carcinoma. Nature 497, 67–73 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poola I. & Speirs V. Expression of alternatively spliced estrogen receptor alpha mRNAs is increased in breast cancer tissues. J Steroid Biochem Mol Biol 78, 459–469 (2001). [DOI] [PubMed] [Google Scholar]
- Pfeffer U., Fecarotta E. & Vidali G. Coexpression of multiple estrogen receptor variant messenger RNAs in normal and neoplastic breast tissues and in MCF-7 cells. Cancer Res 55, 2158–2165 (1995). [PubMed] [Google Scholar]
- Leygue E. R., Watson P. H. & Murphy L. C. Estrogen receptor variants in normal human mammary tissue. J Natl Cancer Inst 88, 284–290 (1996). [DOI] [PubMed] [Google Scholar]
- Thomas C. & Gustafsson J. A. The different roles of ER subtypes in cancer biology and therapy. Nat Rev Cancer 11, 597–608 (2011). [DOI] [PubMed] [Google Scholar]
- Daffada A. A. et al. Exon 5 deletion variant estrogen receptor messenger RNA expression in relation to tamoxifen resistance and progesterone receptor/pS2 status in human breast cancer. Cancer Res 55, 288–293 (1995). [PubMed] [Google Scholar]
- Daffada A. A. & Dowsett M. Tissue-dependent expression of a novel splice variant of the human oestrogen receptor. J Steroid Biochem Mol Biol 55, 413–421 (1995). [DOI] [PubMed] [Google Scholar]
- Springwald A. et al. Identification of novel transcript variants of estrogen receptor alpha, beta and progesterone receptor gene in human endometrium. Endocrine 37, 415–424 (2010). [DOI] [PubMed] [Google Scholar]
- Skrzypczak M. et al. Molecular profiling of estrogen receptor alpha and progesterone receptor transcript variants in endometrial cancer. Steroids 104, 122–128 (2015). [DOI] [PubMed] [Google Scholar]
- Rice L. W., Jazaeri A. A. & Shupnik M. A. Estrogen receptor mRNA splice variants in pre- and postmenopausal human endometrium and endometrial carcinoma. Gynecol Oncol 65, 149–157 (1997). [DOI] [PubMed] [Google Scholar]
- Hu C., Hyder S. M., Needleman D. S. & Baker V. V. Expression of estrogen receptor variants in normal and neoplastic human uterus. Mol Cell Endocrinol 118, 173–179 (1996). [DOI] [PubMed] [Google Scholar]
- Hirata S. et al. Presence of alternatively spliced-estrogen receptor mRNA variants in normal human uterine endometrium and endometrial cancer. Endocr J 42, 289–293 (1995). [DOI] [PubMed] [Google Scholar]
- Jazaeri O., Shupnik M. A., Jazaeri A. A. & Rice L. W. Expression of estrogen receptor alpha mRNA and protein variants in human endometrial carcinoma. Gynecol Oncol 74, 38–47 (1999). [DOI] [PubMed] [Google Scholar]
- Assikis V. J., Bilimoria M. M., Muenzner H. D., Lurain J. R. & Jordan V. C. Mutations of the estrogen receptor in endometrial carcinoma: evidence of an association with high tumor grade. Gynecol Oncol 63, 192–199 (1996). [DOI] [PubMed] [Google Scholar]
- Zhang Q. X., Borg A., Wolf D. M., Oesterreich S. & Fuqua S. A. An estrogen receptor mutant with strong hormone-independent activity from a metastatic breast cancer. Cancer Res 57, 1244–1249 (1997). [PubMed] [Google Scholar]
- Thomas C. & Gustafsson J. A. Estrogen receptor mutations and functional consequences for breast cancer. Trends Endocrinol Metab 26, 467–476 (2015). [DOI] [PubMed] [Google Scholar]
- Skafar D. F. Formation of a powerful capping motif corresponding to start of “helix 12” in agonist-bound estrogen receptor-alpha contributes to increased constitutive activity of the protein. Cell Biochem Biophys 33, 53–62 (2000). [DOI] [PubMed] [Google Scholar]
- Gao J. et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal 6, pl1 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satyaswaroop P. G., Zaino R. J. & Mortel R. Estrogen-like effects of tamoxifen on human endometrial carcinoma transplanted into nude mice. Cancer Res 44, 4006–4010 (1984). [PubMed] [Google Scholar]
- Gottardis M. M., Robinson S. P., Satyaswaroop P. G. & Jordan V. C. Contrasting actions of tamoxifen on endometrial and breast tumor growth in the athymic mouse. Cancer Res 48, 812–815 (1988). [PubMed] [Google Scholar]
- Decensi A. et al. Effect of tamoxifen on endometrial proliferation. J Clin Oncol 14, 434–440 (1996). [DOI] [PubMed] [Google Scholar]
- Mermel C. H. et al. GISTIC2.0 facilitates sensitive and confident localization of the targets of focal somatic copy-number alteration in human cancers. Genome Biol 12, R41 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zack T. I. et al. Pan-cancer patterns of somatic copy number alteration. Nat Genet 45, 1134–1140 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- TCGA Research Network: TCGA Copy Number Portal (2010). http://www.broadinstitute.org/tcga/home Date of access: 21/07/2015.
- TCGA. Integrated genomic characterization of endometrial carcinoma. Nature 497, 67–73 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beroukhim R. et al. The landscape of somatic copy-number alteration across human cancers. Nature 463, 899–905 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson J. T. et al. Integrative genomics viewer. Nat Biotechnol 29, 24–26 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortazavi A., Williams B. A., McCue K., Schaeffer L. & Wold B. Mapping and quantifying mammalian transcriptomes by RNA-Seq. Nat Methods 5, 621–628 (2008). [DOI] [PubMed] [Google Scholar]
- Asmann Y. W. et al. A novel bioinformatics pipeline for identification and characterization of fusion transcripts in breast cancer and normal cell lines. Nucleic Acids Res 39, e100 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asmann Y. W. et al. Detection of redundant fusion transcripts as biomarkers or disease-specific therapeutic targets in breast cancer. Cancer Res 72, 1921–8 (2012). [DOI] [PubMed] [Google Scholar]
- Norton N. et al. Gene expression, single nucleotide variant and fusion transcript discovery in archival material from breast tumors. Plos One 8, e81925 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smallridge R. C. et al. RNA sequencing identifies multiple fusion transcripts, differentially expressed genes, and reduced expression of immune function genes in BRAF (V600E) mutant vs BRAF wild-type papillary thyroid carcinoma. J Clin Endocrinol Metab 99, E338–E347 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moelans C. B., Holst F., Hellwinkel O., Simon R. & van Diest P. J. ESR1 Amplification in Breast Cancer by Optimized RNase FISH: Frequent but Low-Level and Heterogeneous. Plos One 8, e84189 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.