SUMMARY
Point-of-care (POC) laboratories that deliver rapid diagnoses of infectious diseases were invented to balance the centralization of core laboratories. POC laboratories operate 24 h a day and 7 days a week to provide diagnoses within 2 h, largely based on immunochromatography and real-time PCR tests. In our experience, these tests are conveniently combined into syndrome-based kits that facilitate sampling, including self-sampling and test operations, as POC laboratories can be operated by trained operators who are not necessarily biologists. POC laboratories are a way of easily providing clinical microbiology testing for populations distant from laboratories in developing and developed countries and on ships. Modern Internet connections enable support from core laboratories. The cost-effectiveness of POC laboratories has been established for the rapid diagnosis of tuberculosis and sexually transmitted infections in both developed and developing countries.
INTRODUCTION
There are a number of conflicting problems that currently hamper diagnosis. First, the permanent increase in the number of biomarkers has led to the need for more laboratories that are equipped to perform as many diagnostic tests as possible. Second, there is a need to obtain biological test results during treatment in order to make rapid decisions in terms of patient management. In the field of microbiology, the most important issues are often the identification of a contagious disease that requires the patient to be isolated as well as the precise diagnosis of infection to identify the need for treatment and to select the treatment best suited to the situation. Third, it is important to detect infections that can be easily cured through ambulatory care and those which may compromise prognosis, requiring hospitalization.
The field of biology has evolved during recent years to take these issues into consideration (1). Very large laboratories (core laboratories) that reduce costs and operate 24 h a day and 7 days a week have emerged (2), but this raises the problem of the remoteness of care points. While the high speed of tests saves time, transport time can be a major drawback to the use of these rapid tests, which may in turn affect patient management. Conversely, doctor tests have been introduced, which are usually simple tests performed by a physician or a nurse. These tests can help optimize patient management. One of the first doctor tests to be introduced was the detection of Streptococcus pyogenes by throat swab, leading to the prescription of antibiotic treatment when the test was positive and no treatment when the test was negative.
Furthermore, for a long time, gynecologists performed tests to detect bacterial vaginosis (Nugent test) and used direct microscopic observation to detect the presence of Trichomonas vaginalis, Gram-negative bacteria, or gonococci (3).
The closure of a laboratory for which we were responsible in a Marseille hospital led us to question the way in which our laboratories are organized. The laboratory in question was located >10 km away from the core laboratory, and it was impossible to guarantee transport between the emergency unit of the hospital and the core laboratory within 2 h.
We thus installed an original point-of-care (POC) laboratory, which was equipped to rapidly test for syndromes and to provide results within 3 h, which was crucial for optimum patient management. This laboratory was located in the emergency room of a 1,100-bed teaching hospital. It has seen considerable success and has saved substantial labor time in comparison with core laboratories by consolidating all other tests on-site. The initiative has since been tested under more difficult conditions in Africa (4), and preliminary experiments have been carried out on boats (5). The objective of this review is to examine different issues which may help to develop care organization through POC laboratories.
METHODS
We screened the Medline database using “point-of-care,” “near-patient,” “rapid,” “POC infection,” and specific keywords related to each microorganism and disease. For the cost-effectiveness analysis, we further screened Medline, performing a literature search and identifying economic studies published between 2008 and 2015. We included all studies that compared POC tests (POCTs) with standard diagnosis strategies, including any analyses of cost-effectiveness. We focused the review on the cost-effectiveness of monitoring the following infectious diseases for which new POC tests (which may play a central role in the prevention and treatment of these diseases) have been developed, particularly in low-income countries: tuberculosis (TB), malaria, syphilis, and Chlamydia trachomatis infection. We excluded studies that had been conducted only on a specific population, such as coinfected patients, as this would have made it difficult to make comparisons between studies, as well as studies that did not compare both outcome and costs, enabling us to calculate incremental cost-effectiveness ratios (ICERs).
POC TESTS
In recent years, many definitions of POCTs have been proposed in the literature (6–8). We chose the following definition, which is the most widely used: POC tests are performed at the site of patient care. Three key features distinguish them from traditional laboratory tests: they do not need significant laboratory infrastructures or specialized staff in order to be performed, they are designed to be easy to use and interpret, and they are often able to deliver a rapid (i.e., within 1 h) diagnosis (5). Another key advantage of these new diagnostic tests is that because they require less specialized equipment and skills, they are potentially cheaper and could thus also be more cost-effective than conventional tests. Issues raised by their introduction may differ significantly depending on the setting. In low-income countries, which face a strong shortage of human resources and lack laboratory infrastructures, the availability of laboratory tests, including diagnostic tests, is very limited. When these tests are available, they are often too costly to be widely accessible to the patients and health care professionals who need them (9). In this setting, the introduction of POCTs, which require simpler procedures and fewer resources in order to be performed, may improve access to diagnostic tests and potentially generate significant health benefits by providing key information to guide therapeutic decisions (10). Conversely, in high-income countries, laboratory tests are widely available, and health care professionals have the choice between different laboratory techniques. In this setting, the main added value of POC tests compared with traditional techniques is the decrease of the time between sample collection and diagnosis, thus optimizing medical decisions made regarding the hospitalization, isolation, and treatment of patients diagnosed with infectious diseases (11).
Direct Detection of Pathogens by Antigen Detection Assays
Specific microorganism antigens can be rapidly detected from a clinical specimen through an immunochromatographic test (ICT). Lateral flow tests or strip tests rely on the binding of a microbial antigen present in the clinical sample to a primary antibody conjugated to gold or a fluorescent marker. The antibody-antigen complex then migrates either under the effect of a lysis buffer or by capillarity in a solid substrate. The antibody-antigen complex is then captured by a secondary antibody, leading to the appearance of an initial color band, while the excess primary antibody, conjugated to gold beads, continues migrating to a second point of capture with tertiary antibodies, leading to the appearance of a second color band. The test reading is taken within 15 min, and interpretation is based on visualization of the first band (present equals positive, and absent equals negative) and visualization of the second band (present equals an interpretable test result, and absent equals an uninterpretable test result). ICTs are available in several formats, the results of which can be read either visually or by using a compact and connectable reader, which is mandatory when labeling the primary antibody with a fluorescent marker. Currently, ICTs are available for diagnosis of infections by several bacteria, viruses, parasites, and fungi, and multiplexed strip tests are available to detect 3 to 14 pathogens, using the syndromic approach presented below. Together, these tests cover the more common pathogens (Table 1). The benefits of the ICT are its speed and the lack of instrumentation, making the test low cost; the fact that there is no need for a power source, maintenance, or training; and the fact that the test is easy to transport and store due to its small size and, in particular, its resistance to variations in temperature. The two main drawbacks of the ICT are its low sensitivity, usually between 60% and 95%, and the fact that visual interpretation of results is operator dependent, being based on a subjective interpretation of test positivity in weakly positive cases. This can lead to false-positive and false-negative results (12). The development of strip readers overcomes this drawback.
TABLE 1.
Menus for syndromic kits at the POCa
| Kit | Pathogen | Sample | Technique(s) |
|---|---|---|---|
| Diarrhea kit | Rotavirus | Stool | ICT |
| Adenovirus | Stool | ICT | |
| Clostridium difficile | Stool | ICT, RT-PCR | |
| Campylobacter spp. | Stool | ICT | |
| Pneumonia kit | Streptococcus pneumoniae | Urine | ICT |
| Legionella pneumophila | Urine | ICT | |
| Mycobacterium tuberculosis | Sputum | RT-PCR | |
| Staphylococcus aureus | Sputum | RT-PCR | |
| Influenza viruses | Nasal swab | RT-PCR, ICT | |
| Respiratory syncytial virus | Nasal swab | RT-PCR | |
| Procalcitonin | Blood | ICT | |
| Meningitis kit | Neisseria meningitidis | CSF | RT-PCR |
| Streptococcus pneumoniae | CSF | RT-PCR | |
| Enterovirus | CSF | RT-PCR | |
| Herpes simplex virus | CSF | RT-PCR | |
| Varicella-zoster virus | CSF | RT-PCR | |
| Sexually transmitted infection kit | Treponema pallidum | Genital swab | RT-PCR |
| Chlamydia trachomatis | Urine | RT-PCR | |
| Neisseria gonorrhoeae | Urine | RT-PCR | |
| Genital swab | ICT | ||
| Herpes simplex virus | Genital swab | ICT | |
| Vaginitis kit | Atopobium vaginae | Vaginal swab | RT-PCR |
| Gardnerella vaginalis | Vaginal swab | RT-PCR | |
| Trichomonas vaginalis | Vaginal swab | RT-PCR | |
| Candida spp. | Vaginal swab | RT-PCR | |
| Pharyngitis kit | Streptococcus pyogenes | Pharyngeal swab | ICT |
| Tropical fever kit | Plasmodium spp. | Blood | ICT |
| Borrelia spp. | Blood | RT-PCR | |
| Rickettsia felis | Blood | RT-PCR | |
| Rickettsia typhi | Blood | RT-PCR | |
| Dengue virus | Blood | ICT | |
| Yellow fever virus | Blood | ICT | |
| Ebola virus | Blood | RT-PCR, ICT |
Some panels may overlap commercially available multiplexed tests. ICT, immunochromatographic test; RT-PCR, real-time PCR; CSF, cerebrospinal fluid.
Direct Diagnosis by Nucleic Acid Amplification Tests
Nucleic acid amplification tests (NAATs) aim to detect one or more RNA or DNA sequences specific to a single pathogen and have revolutionized the diagnosis of infectious diseases (1). Two techniques are available for POC testing: PCR-based techniques and isothermal nucleic acid amplification techniques (13). Briefly, PCR incorporates 30 to 40 cycles of heating to 72°C, which requires specific equipment and electrical power, limiting the widespread use of PCR in resource-limited settings. Reactions take between 20 and 100 min, including reverse transcription for the detection of RNA. Real-time PCR (RT-PCR) is the variant used in POC testing, involving the hybridization of an appropriate fluorescent probe during each amplification cycle, thus increasing test sensitivity and specificity while reducing detection times. Results report the number of cycles (threshold cycle [CT] values) required to detect one positive specimen, by reference to a log2 scale. Loop-mediated isothermal amplification (LAMP) is a newer, alternative technique for amplifying DNA by means of a DNA polymerase, operating at a constant temperature of 60 to 65°C. Detection of amplification relies on the detection of magnesium pyrophosphate as a by-product. LAMP eliminates the need for a thermocycler, hence making NAATs cheap, energy-saving, and easy to perform in the POC laboratory (14). Current developments include the rapid diagnosis of malaria (15), tuberculosis, and Buruli ulcer (16). One of the advantages of NAATs is that they have greater sensitivity than the ICT, but they require a higher degree of technicality and training. Also, power shortages and the need to store some reagents at 4°C may limit the implementation of NAATs in POC laboratories in some resource-limited tropical countries.
Direct Diagnosis by Miscellaneous Tests
A few pathogens can be detected at the POC by hybridizing a specific fluorescent antibody. A commercially available test, which has not yet been approved by the FDA and the European Community (CE mark), offers 25-min multiplex detection of respiratory tract pathogens, including influenza virus, respiratory syncytial virus (RSV), adenovirus, coronavirus, and parainfluenza virus (17). Up to 26 tropical disease-causing pathogens can also be detected by using a technique for hybridizing DNA or RNA extracted from a clinical specimen, after amplification using the same format as the one used for hybridization (18). The performance of this technique was assessed on a retrospective collection of 170 blood samples. Pathogens were detected with 80% to 90% agreement with the reference method and 100% specificity for Plasmodium spp., chikungunya virus, and dengue virus (18). However, this new approach, which can be performed in ∼2 h using sophisticated instruments, has not yet been assessed under actual POC field conditions.
Non-Pathogen-Specific Diagnosis
Apart from hematology and biochemistry tests, there are some tests that can be incorporated into POC testing for the nonspecific diagnosis of infectious diseases. Urinary tract infection is caused by various bacteria, mainly Escherichia coli. In POC testing, the standard urine test strip features the nitrite test, which detects nitrate-reducing bacteria (E. coli and other enteric Gram-negative bacteria), marked by a pink dye, along with an esterase test, which detects leukocytes (detection limit of 10 to 25 leukocytes/μl), marked by a purple dye. Results are obtained within 5 min.
The monospot test detects heterophile antibodies in the course of mononucleosis syndrome due to Epstein-Barr virus with a sensitivity of 99% and a specificity >90% (19). False-positive results have been reported in the course of other acute infections due to cytomegalovirus (19) and dengue virus (20), among others.
Cell counts are performed at the POC for the laboratory diagnosis of meningitis. Cell counting by microscopic counting and reading is an operator-dependent technique. It could be replaced by an automated technique using an automatic and connectable counter. Most commercial readers have a limit of sensitivity that is higher than the limit of 10 cells/ml used for the biological definition of meningitis and a test sample of several hundred microliters, which is incompatible with the very low volume of cerebrospinal fluid (CSF) received at the POC. New instruments using innovative optical technologies are currently being evaluated (21).
Procalcitonin levels can be measured at the POC in order to assist medical decision-making regarding the prescription of antibiotics for respiratory tract infections (17, 22). Likewise, POC identification of whole-blood lactate has been used as a predictor of mortality in patients diagnosed with severe sepsis (23).
POC LABORATORIES AND SYNDROMIC APPROACHES
POC microbiology laboratories do not deliver a juxtaposition of POC tests but may adopt a syndromic approach in order to organize them and to speed up and optimize diagnosis. Most patients present with clinical signs and symptoms that are not pathognomonic of any particular infectious disease. However, clinical signs and symptoms are indicative of one particular diseased organ, potentially infected by one or several pathogens, or one particular circumstance that exposes the patient to one or more pathogens. It is therefore of medical interest to simultaneously test the multiple pathogens that may cause signs and symptoms in the patient at the POC. We named this approach “syndromic POC,” taking the form of syndromic POC kits incorporating several POC tests. The emergence of moderately complex multiplexed tests facilitates the syndromic approach.
Conventional clinical specimen sampling is a disease-based approach aimed at successively testing the pathogens that the doctor believes are potentially responsible for the infection, until a diagnosis is made. Because of the tremendous number of emerging pathogens, however, it is difficult for physicians to memorize the actual list of pathogens and the corresponding list of appropriate clinical samples. In contrast to this approach, clinical sampling can be standardized by syndrome in order to speed up the laboratory process and make it more efficient. Syndrome-based kits are contained in an appropriate format such as a plastic bag and contain prelabeled sampling tubes and containers along with summarized sampling instructions for doctors and nurses, prelabeled laboratory forms, and informed written consent to be signed by the patient, if required by local regulations (Fig. 1). The advantages of sampling kits over the usual disease-based sampling include the limited and nonrepetitive number of specimens collected from the patient, a simplified laboratory test prescription for the physician, a plannable workflow for the nurse and the doctor, and easily traceable samples for the laboratory. In the laboratory, clinical samples are tagged according to the particular sampling kit used to retrieve them, allowing specific laboratory protocols to be adopted. Syndromic kits are used to test most of the pathogens known to be responsible for one particular syndrome, such as endocarditis, pericarditis, diarrhea, osteitis, meningitis, encephalitis, uveitis, keratitis, or infections in one particular epidemiological group of individuals, such as febrile patients presenting to the emergency room, with a worsening of chronic respiratory tract infection in cystic fibrosis patients, fever in travelers, fever in pilgrims to Mecca, and fever in homeless patients and neonates, for whom a specific menu of pathogens has to be drawn up (Table 1). A syndrome-based kit is designed after reviewing the available literature regarding both the repertoire of pathogens responsible for the syndrome and the optimal methods of achieving direct and indirect diagnoses of infection by each one of these pathogens. Syndromic kits allow laboratories to constitute large clinical series and to preserve large collections of specimens in dedicated biological resource centers for retrospective testing using emerging pathogens.
FIG 1.
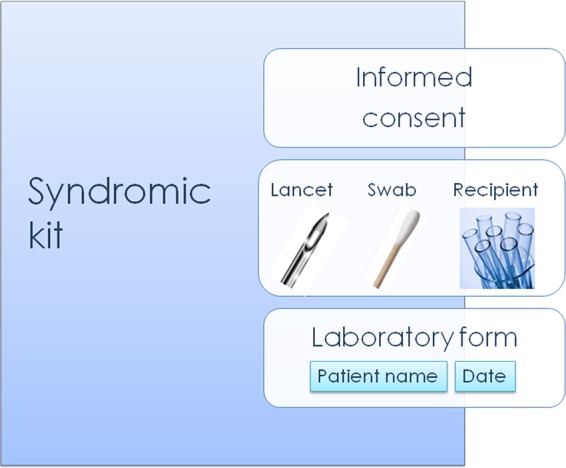
Syndromic kit for POC testing containing materials for clinical specimen collection, self-collection, and paperwork.
POC laboratory procedures have to specify supplementary tests to be performed in the core laboratory. These may include, for example, additional core laboratory NAATs to confirm negative results yielded by a lower-sensitivity POC ICT. Genotyping may also be conducted as a second-line test, the result of which will be incorporated into the laboratory epidemiology database. In any case, POC laboratory menus and procedures have to be conducted in agreement with the medical director of the core laboratory.
Syndromic Kit Menus
The menu of any given POC syndromic kit mixes deadly pathogens with 80% of the most frequent pathogens and highly contagious pathogens (Table 1). Such a mix aims to help doctors answer the following three basic questions concerning a patient potentially suffering from an infectious disease. (i) Is it a rapid, deadly infection requiring particular medical support, including hospitalization in an appropriate department? (ii) Is it a contagious infection requiring patient isolation under an appropriate isolation protocol? (iii) Is it an infection requiring any specific anti-infectious treatment?
Establishing the menu of any POC syndromic kit therefore relies on the prior establishment of the repertoire of pathogens responsible for syndromes in that particular geographic area (24). It must be emphasized, however, that interpretation must incorporate the study of control populations, which has not always been done (25). One corollary is that the menu of any POC syndromic kit must be reevaluated in a given geographic region, based on emerging pathogens. This is illustrated by the 2014-2015 Ebola virus epidemics in West African countries, which clearly led to the incorporation of appropriate POC tests in the fever POC syndromic kit (26). This also means that the menu of any POC syndromic kit may vary slightly from one geographic area to another, to take into account the most prevalent pathogens in that region. The repertoire can be established through the direct detection of pathogens circulating in one geographic area. As an example, we first had to establish the etiological agents responsible for fever in Senegal and Gabon, discovering that Rickettsia felis and Borrelia crocidurae were previously unrated frequent causes of fever (27), before establishing a tropical fever POC syndromic kit in the Dielmo POC in rural Senegal (4). Indirect diagnosis by serology can also be used to trace pathogens, and multiplexed formats facilitate such epidemiological surveys (28).
Tropical Fever
Fever is a nonspecific yet frequent sign in natives, expatriates, and travelers exposed to tropical regions (29), indicating an infection due to a ubiquitous pathogen or a pathogen specifically found in tropical countries. Fever can be the initial sign of, among other specific pathogens, deadly malaria and deadly Ebola virus infection and may signal other disabling infections that can be cured by specific anti-infectious treatments. Therefore, it is medically important to conduct rapid POC tests for some pathogens in patients exposed to tropical countries. Malaria continues to be a leading cause of fever in countries where the disease is endemic (30). The WHO now recommends that parasite-based diagnosis should be used in all cases of suspected malaria before treatment of patients (31). Rapid diagnostic POC tests include the BinaxNOW malaria test (Alere, Orlando, FL, USA), which is able to detect the four Plasmodium species infecting patients and is the only such FDA-approved test; the Parascreen Pan/Pf test (Zephyr Biomedical, Goa, India) and the OptiMAL test (Diamed AG, Cressier, Switzerland), which identify both Plasmodium falciparum and Plasmodium vivax; and the Paracheck Pf test (Orchid Biomedical Systems, Goa, India), which identifies only P. falciparum (31). Dengue virus can be tested by using a rapid diagnostic test (RDT), which detects either IgM and IgG antibodies or IgM antibodies and the NS1 protein (32). As with IgM detection, the sensitivity is 30 to 96% and the specificity is 86 to 92%, while for NS1 detection, the sensitivity is 38 to 71% and the specificity is 76 to 80% (32). Detection of the NS1 protein is particularly well suited to POC testing because of its higher sensitivity during the acute phase of infection and 92 to 99% reproducibility (32). Recurrent fevers due to various cross-reacting Borrelia species, typhus group and spotted fever group rickettsiae, and Bartonella spp. (more particularly Rickettsia felis and Rickettsia africae) are frequent causes of tropical fever. They can be detected by appropriate reported but noncommercialized RT-PCR assays (4, 33–35). A nanogold particle lateral flow assay was recently reported for POC diagnosis of dengue virus, yellow fever virus, and Ebola virus infections (23). These infections can also be diagnosed at the POC by using a commercially available RT-PCR assay (36) and a recently evaluated immunoassay detecting the Ebola virus VP40 antigenic protein (37).
Community-Acquired Respiratory Tract Infection
Community-acquired respiratory tract infections hold a major place in infectious pathology and, in the case of pneumonia, were responsible for 2.7 million deaths in 2013 (38). They are caused mainly by bacteria, viruses, and coinfections by influenza virus and, for example, Streptococcus pneumoniae and Staphylococcus aureus (39). These elements illustrate the importance of rapid diagnosis of S. pneumoniae pneumonia and Legionella pneumophila infection, which is performed by the ICT in 15 min with a specificity of 99% but a sensitivity of 74% for L. pneumophila (40) and a positive predictive value of 0.88 to 0.96 for S. pneumoniae (41). The detection of influenza virus in 30 min also has low sensitivity (<60%) but a specificity of almost 100% and a high positive predictive value (>98%) during the influenza season (42). ICTs are able to diagnose influenza virus and RSV infections. Recently, the sensitivity and specificity of real-time PCR (Xpert Flu/RSV XC; Cepheid) for the rapid diagnosis of the combination of influenza virus and RSV infections were measured at 97.8% and 100% for influenza virus, respectively, and at 97.9% and 100% for RSV, respectively (43, 44).
With 9 million estimated new cases and 1.5 million deaths in 2013 (45), tuberculosis (TB) currently remains one of the deadliest threats to public health. Its diagnosis in POC laboratories relies on real-time PCR, including the commercialized Xpert MTB/RIF assay (Cepheid, Sunnyvale, CA, USA), which provides accurate results within 2 h for detection of pulmonary TB disease. Xpert MTB/RIF can also identify resistance to rifampin, a critical first-line drug for treatment of the disease and a reliable surrogate marker of multidrug-resistant TB (MDR-TB) strains. Since 2010, the WHO has recommended the use of Xpert rather than smear microscopy for diagnosis of patients suspected of having TB (46). Finally, there is some interest in the semiquantitative measurement of procalcitonin levels of >0.5 mg/ml of blood in 1 h, to guide the prescription of antibiotics, including the diagnosis of bacterial coinfection with influenza virus (47).
Diagnosis of community-acquired pneumonia at the POC involves RT-PCR tests integrating nucleic acid extraction and amplification in a single cassette and in a multiplexed manner. The Respiratory Film Array Panel system (BioFire; bioMérieux) is FDA and EC approved and can detect 17 viruses and 3 types of bacteria within 1 h. Several other multiplex RT-PCR assays are commercially available. Their comparative evaluation specificity is >94% but with a 56 to 91.7% sensitivity, which is lower for bacteria (48). In addition to community-acquired pneumonia, the diagnosis of ventilator-associated pneumonia may also be conducted in a POC laboratory, including the rapid diagnosis of S. aureus pneumonia (49).
Digestive Tract Infection
Diarrhea is a leading cause of death worldwide (38) and a frequent reason for consulting a doctor. Coinfections are common (38, 50). Prognosis varies between a self-limited infection and fatal infection in the case of Clostridium difficile O27 enteritis (51). Several ICT techniques have been developed for the POC diagnosis of diarrhea, including the rapid (<30 min) agglutination-based detection of rotavirus and adenovirus as well as the detection of C. difficile toxins. The rapid detection of C. difficile toxins A and B should be routinely performed for both outpatients and hospitalized patients by using one of the commercially available ICTs, with a specificity of >99.5% and an average sensitivity of 90% (52). Alternatively, C. difficile, its toxin B, and an additional binary toxin can be detected within 90 min by using commercially available RT-PCR assays such as GeneXpert, with 98% agreement with reference testing in the core laboratory and higher sensitivity than ICTs (53, 54). The recent implementation of fecal transplant treatment has changed the prognosis of this infection, making early diagnosis even more important (51). A commercially available Campylobacter antigen detection kit has been favorably evaluated (55). A dipstick test for the rapid detection of Shigella is under evaluation (56, 57). Currently, several RT-PCR tests allow multiplexed detection of bacteria, including C. difficile and E. coli pathovars; parasites; and viruses, including norovirus 5, within 1 h (Table 1). Evaluation shows a sensitivity of >90% for the majority of pathogens and, interestingly, coinfection in 13 to 21% of samples tested, depending on the panels (50).
Genital Tract Infection
Genital tract infections are caused by pathogens transmitted during sexual intercourse. In infected women, they are one cause of infertility, and pathogens may infect other organs and systems. Because of the high contagiousness of these pathogens, rapid diagnosis is clearly important in terms of both treatment and prevention (58). Neisseria gonorrhoeae, Chlamydia trachomatis, and herpes simplex virus can all be detected by lateral flow assays in a POC laboratory and by RT-PCR assays, which have higher sensitivity. Maternal syphilis due to Treponema pallidum contributes to perinatal morbidity and mortality worldwide. If untreated, it may lead to complications and fetal infections. POC prenatal syphilis screening was developed to address the limitations of conventional rapid plasma reagin (RPR) tests, followed by a confirmatory Treponema pallidum hemagglutination assay (TPHA), which requires at least two visits, is usable only on serum, requires refrigeration, and is not easy to perform in facilities with personnel with low-level qualifications/technical skills. These new POCTs include immunochromatographic strip (ICS) and dual-POC tests to detect both treponemal and nontreponemal antibodies. While POC diagnosis of sexually transmitted infections (STIs) has been favorably evaluated (59, 60), the impact of POC syphilis diagnosis has not yet been evaluated (61).
C. trachomatis infection is the most frequent sexually transmitted infection in the world. Untreated infection can result in pelvic inflammatory disease (PID), infertility, and ectopic pregnancy in women and epididymitis and orchitis in men (62). C. trachomatis alone can be detected by using the ICT and NAAT in dual and multiplex RT-PCR assays.
In addition to being an STI, vaginosis has been associated with preterm birth (63). It can be diagnosed at the POC by using ion motility spectrometry (64) and the more widespread ICT and NAAT (63). These assays target mainly two bacteria, Atopobium vaginae and Gardnerella vaginalis.
Meningitis
Meningitis involves a broad spectrum of causative agents and related prognoses and medical management, highlighting the value of rapid POC diagnosis (11). Performing CSF cytology remains problematic, as microscopic observation and cell counting are operator-dependent techniques, and very few cell counters offer a 10-cell/mm3 resolution and a 10-μl assay mixture volume. We have nevertheless used such a cell counter, which performs well in terms of counting white cells but does not count red cells. Lens-free devices are under evaluation (65). In terms of the direct detection of pathogens, we created a POC meningitis menu that was systematically aimed at testing for enterovirus (NAAT), Streptococcus pneumoniae (NAAT), Neisseria meningitidis (NAAT), and herpesviruses, including herpes simplex and varicella-zoster viruses (NAAT), in cerebrospinal fluid collected from symptomatic patients clinically suspected of having meningitis (66). As for HIV-infected patients, an LFA detecting Cryptococcus neoformans polysaccharide capsule glucuronoxylomannan antigen performed adequately on CSF (67), plasma, serum, and urine samples (68), but tests on saliva were disappointing and should not be recommended (69). A few commercially available multiplexed NAATs currently under development would detect six bacteria, eight viruses, and two Cryptococcus species within 1 h.
Pharyngitis
Streptococcus pyogenes is one of the pathogens to be detected in the case of clinical pharyngitis (70). Specimens consist of a pharyngeal swab. The detection of S. pyogenes is most commonly achieved by using lateral flow assays, with sensitivity reported to be 86.1% and specificity reported to be 97.1% (70). The rapid POC measurement of C-reactive protein is not justified in assisting with medical decisions for adults, as levels have been measured within normal ranges in documented cases of S. pyogenes pharyngitis (71).
POC LABORATORY IMPLEMENTATION
Location and Space
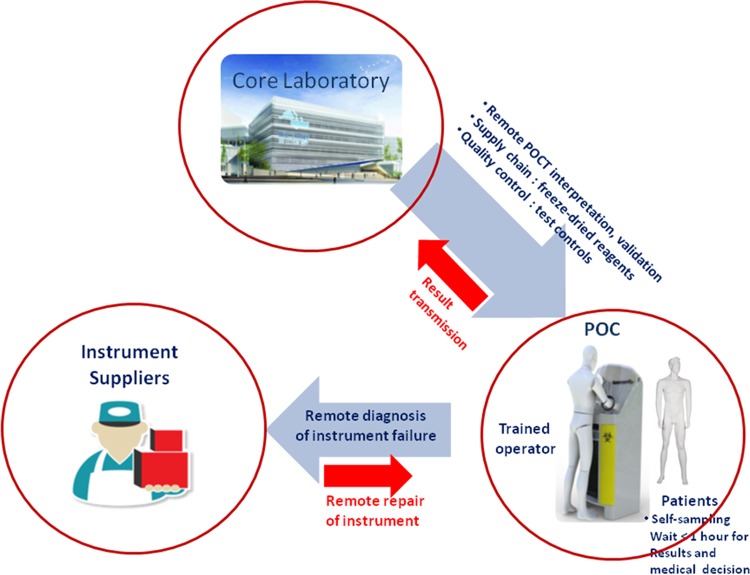
A decision may be made to set up a POC laboratory when the time of transport of clinical specimens to the core laboratory takes more than 1 h, the optimal time scale for POC tests in order to obtain a result within 2 h. In our experience, a POC laboratory can serve a minimum population of 500 to 1,000 people, corresponding to the population of patients in an emergency unit (66) or remote village (4) or a small population on board a ship (5) (Fig. 2). The POC could therefore be installed close to the emergency room of a large hospital in order to supplement the work of the core laboratory, by reducing the time of delivery of clinical specimens and filling a gap in the event of the core laboratory, the community-based pharmacy (72, 73), or any health care facility closing at night. In our experience, a POC laboratory can be installed in a 5- to 10-m2 air-conditioned room with the temperature regulated at 20°C ± 2°C and a power source (4, 5). An alternative is a mobile POC that can be quickly deployed in a civilian advanced nursing station at mass rallies, in areas of military conflict, or even onboard ships (5). The POC should accommodate one person in comfortable working conditions, including air-conditioning and sufficient natural daylight and artificial night light. POC laboratories must have room to store instruments, equipment, and some reagents at room temperature as well as room to store reagents at 4°C. POC laboratories must also accommodate potentially infectious waste. Complete computerization of POC management would restrict non-potentially infectious waste to reagent wraps. POC laboratories are in permanent contact with a supporting core laboratory. One major difference between a POC laboratory and self-diagnostic tests performed by patients is that self-diagnostic tests may guarantee quality-controlled design, manufacture, and performance but cannot guarantee the quality of implementation.
FIG 2.
The POC laboratory in its environment: patients, core laboratory and instruments, software, and reagent suppliers.
Instruments
The POC must contain a hood for handling class 2 clinical samples, storage at room temperature (controlled at 20°C ± 2°C), a refrigerator for storage at 4°C ± 1°C, a computer connected to the core laboratory, an automatic cell counter for the diagnosis of meningitis, a reader for immunochromatographic tests (optional), a nucleic acid extractor, and a thermocycler, with the latter two instruments optionally being combined into one, such as in the GeneXpert, BioFire, and Cobas Liat system formats (4, 5, 66). Other advantages of the Xpert system include the ability to use each machine module independently, allowing several samples to be screened simultaneously (74). In addition, the instrument is robust, portable, and easy to use and requires only minimal maintenance (75). Correct operation, however, requires a room temperature of between 15°C and 30°C, a constant power supply, and regular module maintenance and calibration. The LAMP technique has emerged due to the fact that the instrument uses little power and can even run on batteries if necessary (76, 77). Reagents can be delivered via the core laboratory, but reagent destocking and control are self-managed. Reagents must be stored at the appropriate temperature, and storage in a refrigerator at 4°C is possible. PCR mixes can be packaged and delivered in a lyophilized form, guaranteeing their stability and intrinsic qualities, as recently shown for the molecular diagnosis of Buruli ulcer (78).
Training
POC laboratories are operated by dedicated staff who have completed specific training. They do not need to be health care professionals, as has been shown in an onboard POC laboratory (5). Training and regular evaluation of personnel are very important (79). It has been shown that the sensitivity of the ICT for the detection of S. pyogenes in the throat was significantly higher when the test was carried out by a laboratory technician or, for nontechnical staff, following training, leading to a 34% increase in test sensitivity (80). We have established a training course split into two 4-h sessions, enabling anyone with or without a medical or biological background to manage a POC laboratory, from the collection of samples to reporting of the results (5). Training is fully recorded in the POC tablet and may be viewed at any time by the staff. Training comes in the form of a questionnaire comprising 20 simple questions with 3 possible answers (“right,” “wrong,” or “I do not know”). Each correct answer is worth 1 point, each incorrect answer deducts 1 point, and the “I do not know” answer is equal to 0 points. Competency assessment also includes observation of training by a qualified POC laboratory staff member. The staff and the POC laboratory itself are quality controlled and remain in permanent contact with a core laboratory and biologists.
Operation
The POC laboratory should operate 24 h a day and 7 days a week and be certified for one POC. A trained and certified operator is in charge of supervising specimen collection, testing, reporting of test results, and general maintenance of the POC, including quality assurance controls. Due to variable regulations in different countries, clinical specimens may be obtained by self-sampling. Self-sampling removes any responsibility for non-health care personnel and respects patients' privacy. Self-sampling has been reported to be effective for screening for STIs (81–83). Self-sampled specimens include blood obtained from a single finger prick, urine collected in a sterile container, and a pharyngeal swab. The operator must then choose the syndromic kit according to the instructions on the device and submit the results of the self-sampled report and interpretation to any competent medical doctor. Matching color-coded syndromic kits with color-coded reagents facilitate and secure the process. The operator is also responsible for the general maintenance of the POC, in particular to avoid shortages. Finally, the operator must conduct regular control assays of the quality assurance process.
Quality Control
In the United States, several POC tests are governed by the Clinical Laboratory Improvement Amendments (CLIA) text issued in 2009 (84). In general, a POC laboratory has to be operated under the supervision of a core laboratory. Unlike doctor tests, the POC has the advantage of being quality controlled in terms of the room, tools, reagents, personnel, and protocols. In Europe, COFRAC (the French quality control commission) recently approved two POC laboratories established in Marseille and operated by our core laboratory. Quality control covers certain critical elements, including refrigerator temperature, which should be maintained at 4°C ± 1°C, and room temperature, which must be kept at 20°C ± 2°C. Quality control also covers the presence of positive and negative internal controls in each test. Particularly in the case of self-sampling, testing must include a sample quality indicator. This may be a human gene detected by RT-PCR, for example, for cervical sampling (81). Finally, it includes regular external controls. Quality assurance includes maintenance of instruments as recommended by the supplier and traceability. Staff must update their certification on an annual basis. Finally, protocols should be reviewed by all operators. We and others are now implementing an external quality assurance program for these POC laboratories (85).
POC IN MICROBIOLOGY DESERTS
Reorganization of Clinical Microbiology
Microbiological POC is suitable whenever a population of >500 to 1,000 people is located more than an hour from the core laboratory. This situation is very common in developed countries, where core laboratories are centralized around technical platforms, thus creating medical deserts. In countries with low and intermediate levels of development, the laboratory network can be underdeveloped. In these countries, barriers to the implementation of POC laboratories in countries with weak and intermediate economies have been identified (86). Accordingly, we established a POC in Dakar, Senegal, as a backup POC for the one in the rural village of Dielmo (4) (Fig. 3).
FIG 3.
Remote POC testing in a rural village in Senegal. The POC test was run using its own source of electricity. (Reprinted from reference 4.)
In particular, the concentration of microbiological platforms in core laboratories limits the population's access to these facilities. In Marseille, we set up a POC in the emergency unit of a hospital serving 400,000 people situated within a 30- to 60-min drive of our core laboratory (66).
Ships
Ships, submarines, and off-shore platforms require access to tests for rapid diagnosis of infectious diseases. However, diagnostic uncertainty can lead to inappropriate, expensive deviations or inappropriate medical decisions, putting ship personnel and passengers at risk of contagion and delayed treatment. We therefore tested a POC laboratory onboard a cruise ship and a freight ship, with favorable results. Following a 4-h training course for nonmedical (freight ship) and medical (cruise ship) personnel, we observed that the POC laboratory enabled diagnosis to be reached exactly as in a conventional POC laboratory (5).
POC DEVELOPMENT
Cohorts
The syndrome-based approach in POC laboratories contributes to measuring the epidemiology of infectious diseases, abnormal events in real time, and the cost of diagnostic tests. We conduct weekly reviews of all POC data, including the total number of requests, the number of applications by syndrome, and the number of diagnoses by pathogen, taking into account the means ± 2 standard deviations over the previous 12 months to identify any abnormal events. This is easily achieved by using the EPIMIC program and a simple Excel database (87). It was shown that the installation of a rural POC in Africa helped to establish the epidemiology of infectious diseases in Africa (88).
Epidemiology and Infection Control
Computerized POC data can ensure real-time, local epidemiology, which in turn can be used to assist medical decision-making. As such, POC laboratories contribute to public health microbiology, assisting with the rapid detection of pathogens, including the threat of bioterrorism, and providing an appropriate response. It has been shown that the availability of real-time incidence data for S. pyogenes pharyngitis was effective in the accuracy of its clinical diagnosis (89). Likewise, the impact of some POC tests on the appropriate use of antibiotics in cases of urinary tract infections has also been favorably evaluated (90). The impact of POC tests on infection control was recently reviewed (79). In terms of infection control, one of the impacts of POC testing is to prevent the hospitalization of patients presenting at the emergency room with a contagious and benign infection such as enterovirus meningitis (91). A second impact is placing patients with the same epidemic and contagious infection into the same cohort; this is illustrated by the cohorting of respiratory syncytial virus-infected children in pediatric emergency rooms (79).
COST-EFFECTIVENESS
While several POC tests have been evaluated, we focused on four diseases and syndromes. Using WHO guidelines (92), we considered that an intervention was considered to be very cost-effective if its ICER was below the annual gross domestic product (GDP) per capita of the study country and was cost-effective if its ICER was less than three times the country's annual GDP per capita (92) (Table 2).
TABLE 2.
Cost-effectiveness analyses of POCTs for screening for infectious diseasesa
| Disease and reference | Setting(s) | Method | Cost(s) assessed (currency) | Effectiveness measure(s) | Time horizon, discountinge | Strategies assessed | ICER(s)b | Conclusion(s) |
|---|---|---|---|---|---|---|---|---|
| Tuberculosis | ||||||||
| 93 | India, South Africa, Uganda | Decision analytic model | Diagnostic and treatment costs (US$) | DALYs | <1 yr, discounted at 3% | S0, smear microscopy and clinical diagnosis (referencec); S1, Xpert in addition to S0; S2, Xpert replacing S0 | S1 vs S0, US$41–110; S2 vs S0, US$52–138; S2 vs S1, US$343–650 | S1 and S2 increase case findings; S1 and S2 are cost-effective, except for S2 in Uganda |
| 94 | Botswana, Lesotho, Namibia, South Africa, Swaziland | Dynamic mathematical model | Diagnostic, treatment, and transmission costs (US$) | DALYs, life years saved | 10–20 yr, from 2012, discounted at 3% | S0, smear microscopy (reference); S1, Xpert | S1 vs S0 over 10 yr, US$792–1,257; S1 vs S0 over 20 yr, US$536–1,060 | S1 is cost-effective |
| 95 | Tanzania | Integrated model | Investment costs and running costs (US$) | DALYs | 10 yr, discounted at 3% | S0, smear microscopy (reference); S1, LED fluorescence microscopy; S2, Xpert | S1 vs S0, US$29; S2 vs S0, US$169 | S2 is the most cost-effective |
| 96 | Former Soviet Union | Dynamic transmission model | Diagnosis, treatment, hospitalization, capital, supplies, labor, and administrative overhead costs (US$) | QALYs | 10 yr, discounted at 3% | S0, MMR (reference); S1, MMR + sputum PCR; S2, MMR + symptom screening; S3, sputum PCR; S4, no screening; S5, symptom screening; S6, MMR + symptom screening + sputum PCR; S7, symptom screening + sputum PCR | S1 vs S0, dominatedd; S2 vs S0, extended dominance; S3 vs S0, US$543; S4 vs S0, dominated; S5 vs S0, dominated; S6 vs S0, dominated; S7 vs S0, dominated | S3 is the most cost-effective |
| 97 | USA | Decision analytic model | Diagnosis, staff, consumable, and equipment costs (US$) | QALYs | Lifetime, discounted at 3% | S0, smear microscopy; S1, smear microscopy + MTD test if smear is positive (reference); S2, smear microscopy + MTD; S3, smear microscopy + Xpert if smear is positive; S4, smear microscopy + Xpert | S0, always dominated; S2 vs S1, US$47,914; S3 vs S1, US$23,111; S4 vs S1, US$39,992 (WTP threshold, US$50,000 per QALY) | S2, S3, and S4 are all CE compared with S1; with a WTP of US$50,000, S2 is recommended |
| Malaria | ||||||||
| 99 | Ethiopia | Decision analytic model | Diagnostic and treatment costs (US$) | Correctly treated cases | Not specified | S0, Paracheck RDT + treatment (reference); S1, Parascreen RDT + treatment; S2, presumptive treatment | S1 vs S0, US$0.59; S2 vs S0, dominated; S2 vs S1, dominated | S1 is highly cost-effective |
| 100 | Uganda | Decision analytic model | Diagnostic and treatment costs (US$) | Cases correctly diagnosed and treated | <1 yr, discounted at 3% | S0, presumptive treatment (reference); S1, microscopy; S2, Paracheck RDT | S1 vs S0, US$9.61; S2 vs S0, US$5.00; S1 vs S2, dominated | S1 and S2 are CE compared with S0; S2 should be preferred |
| 101 | Zambia | Cohort data | Capital and recurrent costs (US$) | Proportion of patients correctly diagnosed | <1 yr, discounted at 5% | S0, clinical diagnosis (reference); S1, microscopy; S2, Paracheck RDT | S1 vs S0, US$9.60; S2 vs S0, US$2.60; S2 vs S1, dominated | S1 and S2 are CE compared with S0; S1 should be preferred |
| 102 | Ghana | Decision analytic model | Health sector perspective (US$) | Proportion of patients correctly treated | Lifetime, discounted at 5% | S1, microscopy diagnosis; S2, optimal RDT; S3, presumptive diagnosis | S2 vs S1, US$4.60; S2 vs S3, US$10.50 | S2 should be preferred |
| 103 | Brazilian Amazon | Decision analytic model | Direct medical and nonmedical costs (US$) | No. of adequately diagnosed cases | From fever to diagnostic, discounted at 5% | S0, optimal RDT (reference); S1, smear microscopy | S1 vs S0, US$549.92 | S1 is cost-effective |
| 105 | Sub-Saharan Africa | Decision analytic model | Direct medical care costs and variable costs (US$) | DALYs | Not specified | S0, presumptive treatment (reference); S1, field standard microscopy; S2, RDT | Cost-effectiveness of RDTs depends on malaria prevalence; when prevalence is <81%, the probability that the RDT is CE is 50%; when prevalence is <62%, the probability that the RDT is CE is 95%; when prevalence is <58%, the RDT is cost-saving with a probability of 50% | |
| 106 | Nigeria | Decision analytic model | Consumer and provider costs (US$) | No. of deaths averted | Not specified | S0, presumptive treatment (reference); S1, microscopy; S2, RDT | S1 vs S0, US$257; S2 vs S0, US$221 | S1 is CE; S2 allows savings compared to S0 |
| 107 | Zanzibar | Nonrandomized clinical trial | Consumer and provider costs (US$) | Prescription of ACT, antibiotic prescription, reattendance | 14 days | S0, clinical diagnosis (reference); S1, clinical diagnosis + RDT | S1 is associated with lower rates of prescription of antimalarial treatment, higher rates of prescription of antibiotics, and lower reattendance due to perceived unsuccessful clinical cure for a similar avg cost per patient; S1 should be the preferred strategy | |
| 108 | Kenya | Decision analytic model | Medical care costs (US$) | Cost per 1,000 patients | Not specified | S0, clinical diagnosis (reference); S1, clinical diagnosis + RDT; S2, clinical diagnosis + RDT + revised treatment | S1 vs S0, high prevalence at −US$13, low prevalence at +US$241; S2 vs S0, high prevalence at −US$220, low prevalence at +US$109 | RDT use would improve malaria treatment by reducing treatment errors at a lower cost |
| Syphilis | ||||||||
| 109 | Sub-Saharan Africa | Cohort data | Diagnostic, supply, labor, direct medical, treatment, and pregnancy outcome costs (US$) | Cost per 1,000 women | Life expectancy | S0, no screening (reference); S1, standard screening of RPR + TPHA testing; S2, RPR screening; S3, rapid ICS screening | S1 vs S0, −US$110,220; S2 vs S0, −US$161,310; S3 vs S0, −US$170,030 | S3 is the most cost-saving and the most effective; S3 dominates |
| 110 | Sub-Saharan Africa | Cohort decision analytic model | Counseling, patient, test, and treatment costs (US$) | DALYs averted per 1,000 women | Life expectancy, discounted at 3% | S0, no screening, presumptive treatment (reference); S1, RPR + TPPA testing; S2, RPR testing; S3, dual-POC testing; S4, ICS test | S1 vs S0, 234 DALYs averted with US$20,000 saved; S2 vs S0, 247 DALYs averted with US$22,000 saved; S3 vs S0, 299 DALYs averted with US$27,000 saved; S4 vs S0, 326 DALYs averted with US$30,000 saved | S4 is less costly and the most effective; S4 dominates |
| 111 | Sub-Saharan Africa | Cohort decision analytic model | Direct medical costs (US$) | DALYs averted | Life expectancy, discounted at 3% | S0, no testing + no treatment (reference) S1, ICS testing + treatment | S1 vs S0, US$11 | S1 is cost-effective |
| Chlamydia | ||||||||
| 112 | Baltimore, MD | Decision analytic model | Diagnostic, treatment, and medical costs (US$) | Cases of PID averted | 2–10 yr, discounted at 3% | S0, vaginal swab NAAT (reference); S1, vaginal swab POC tests | S1 vs S0, US$5,050 | S1 is cost-effective |
| 113 | England | Decision analytic model | Diagnostic and treatment costs (£) | Cases correctly identified and treated | <1 yr | S0, PCR current practice (reference); S1, Clearview POC test; S2, Chlamydia Rapid Test at POC | S1 vs S0, −£18.20; S2 vs S0, £61.80 | S1 and S2 are more expensive and less effective than S0; both strategies are rejected |
| 62 | England | Decision tree model | Diagnostic and treatment costs (£) | QALYs | 28 days | S0, standard laboratory NAAT (reference); S1, POC NAAT | S1 vs S0, 46 QALYs gained with £11,754,015 saved | S1 is cost-saving |
ACT, artemisinin-based combination therapy; CE, cost-effective; DALYs, disability-adjusted life years; ICER, incremental cost-effectiveness ratio; ICS, immunochromatographic strip; LED, light-emitting diode; MMR, mass miniature radiography; MTD, Mycobacterium tuberculosis Direct; NAAT, nucleic acid amplification test; PID, pelvic inflammatory disease; POC, point of care; QALYs, quality-adjusted life years; RDT, rapid diagnostic test; RPR, rapid plasma reagin; S0, reference strategy; S1 to S7, strategies 1 to 7, respectively; TPHA, Treponema pallidum hemagglutination assay; TPPA, Treponema pallidum agglutination assay; WTP, willingness-to-pay ratio (that is, the maximum cost-effectiveness ratio that decision-makers are willing to pay to obtain an additional unit of effectiveness).
Values in italics are the minimal and maximal ICERs obtained in the study country.
The reference is the comparator (generally the standard strategy recommended in guidelines or the strategy used routinely), the strategy to which the new strategies are compared.
A strategy is dominated by another when it is more costly and less effective.
It is a common practice in economic evaluations to “discount” future costs using a discount rate. Discounting makes current costs and benefits worth more than those occurring in the future because there is an opportunity cost to spending money now, and there is a desire to enjoy benefits now rather than in the future.
Tuberculosis
In 2011, a cost-effectiveness analysis using a decision analytic model simulating costs and health gains for a cohort of 10,000 individuals suspected of having TB in India, South Africa, and Uganda compared three different diagnostic strategies: (i) smear microscopy alone, defined as two sputum microscopy examinations followed by clinical diagnosis for smear-negative individuals with suspected TB (base case); (ii) use of the Xpert system after two smear-negative examinations (“in addition to”); and (iii) use of Xpert instead of smear microscopy with one single sputum specimen tested (“as replacement for”) (93). ICERs computed for the use of Xpert in addition to smear microscopy compared with the base case were US$55, US$110, and US$41 per disability-adjusted life year (DALY) averted in India, South Africa, and Uganda, respectively. When using Xpert as a replacement for smear microscopy, compared with the base case, ICERs were US$68, US$138, and US$52 per DALY in each of the study countries, respectively. Finally, the ICERs for the use of Xpert as a replacement for smear microscopy compared with the use of Xpert in addition to smear microscopy were US$343 (India), US$582 (South Africa), and US$650 (Uganda) per DALY. These results suggest that both strategies incorporating Xpert were cost-effective in the study countries, except for the replacement of smear microscopy with Xpert in Uganda. Sensitivity analyses based on Monte Carlo simulations confirmed the results.
Another study compared Xpert and smear microscopy in Botswana, Lesotho, Namibia, South Africa, and Swaziland, where TB and HIV prevalences are high (94). The cost-effectiveness analysis was based on a dynamic mathematical model taking into account transmission-related effects over a long-term, 10- to 20-year time scale. Assuming a cost of US$30 per test over a 10-year time period, ICERs were US$1,257, US$1,011, US$878, US$958, and US$792 per DALY averted in each country, respectively. Over 20 years, ICERs dropped to US$1,060, US$536, US$663, US$779, and US$743 per DALY averted, respectively. The model took into account the diagnosis, treatment, and transmission of TB as well as interactions with HIV infection and HIV treatments, which could explain the higher ICERs than those found in the previous study. In almost all cases, ICERs were found to be below the standard benchmarks for cost-effectiveness recommended by the WHO, suggesting that Xpert is a cost-effective strategy within the context of these southern African countries. Conclusions were robust in sensitivity analyses.
The cost-effectiveness of eight different algorithms involving Xpert, light-emitting diode (LED) fluorescence microscopy, and smear microscopy for adult tuberculosis cases in Tanzania was studied by using an integrated model incorporated into and linked with a detailed operational component with a transmission component (95). The authors of that study computed the ICER per DALY from the Tanzanian health system perspective by comparing one option with the next least effective option. Options for the targeted use of Xpert were dominated by strategies based on LED fluorescence microscopy and the Xpert full rollout, which produced DALY gains at a higher incremental cost. Three strategies were identified as cost-effective: the Xpert full rollout, with an ICER of US$169 per DALY averted, followed by two LED fluorescence microscopy-based strategies (the first using two sputum samples collected on the same day, with an ICER of US$45, and the second using two sputum samples collected on different days, with an ICER of US$29). The main results did not change in sensitivity analyses. Those authors conclude that the government should consider full Xpert scale-up if the health-related budget in Tanzania can afford a health intervention, with a cost-effectiveness ratio of US$599 per DALY.
Winetsky et al. developed a dynamic transmission model to evaluate the relative effectiveness and cost-effectiveness of alternative strategies for active TB screening in prisons in the former Soviet Union, where a significant proportion of TB cases are MDR-TB cases (96). Those authors assessed eight strategies involving, either alone or in combination, self-referral, symptom screening, mass miniature radiography (MMR), and sputum PCR with probes for rifampin resistance (Xpert MTB/RIF). Sputum PCR was used either as a standalone screening test for active pulmonary TB or in combination with other case-finding strategies as a preliminary test for multidrug resistance among those cases found to have evidence of active TB upon screening. Results showed that the addition of sputum PCR to the currently used strategy of annual MMR screening was cost-saving over 10 years compared to MMR screening alone but produced only a modest reduction in MDR-TB prevalence (from 0.74% to 0.69%) and had a minimal effect on the overall TB prevalence (from 2.78% to 2.74%). However, the most effective strategy for reducing overall TB prevalence (from 2.78% to 2.31%) and MDR-TB prevalence (from 0.74% to 0.63%) involved the use of sputum PCR as an annual primary screening tool. This strategy was also the most cost-effective, with an ICER of US$543 per quality-adjusted life year (QALY), compared to the previous next least costly and nondominated strategy (MMR with sputum PCR reserved for rapid detection). Probabilistic sensitivity analysis showed that sputum PCR was cost-effective in >95% of simulations. Those authors concluded that sputum PCR for case finding and rapid MDR-TB detection was the best strategy for interrupting the cycle of transmission in prisons where TB is prevalent and MDR-TB strains are concentrated.
Choi et al. evaluated the cost-effectiveness of incorporating Xpert into TB diagnostic algorithms compared to current approaches in the United States, where TB prevalence is low (97). The analysis was conducted from a health system perspective using a decision tree model. It compared five strategies with and without the incorporation of molecular testing: (i) smear microscopy alone, (ii) smear microscopy plus an Amplified MTD (Mycobacterium tuberculosis Direct) 5gENpROBE test if the smear was positive, (iii) smear microscopy plus MTD testing regardless of smear microscopy results, (iv) smear microscopy plus Xpert if the smear was positive (“selective Xpert”), and (v) smear microscopy plus Xpert regardless of smear microscopy results (“intensive Xpert”). ICERs were computed over patients' life expectancies as the cost per QALY gained. The first strategy using smear microscopy alone was dominated by all others strategies. In addition, replacement of MTD with Xpert, using either a selective or an intensive strategy, was found to be cost-effective compared to existing molecular assays. Those authors concluded that, despite the availability of mycobacterial cultures, the addition of Xpert for TB diagnosis would be beneficial and cost-effective compared to current approaches in the low-prevalence setting of the United States. Conclusions were robust in probabilistic sensitivity analyses.
Finally, in a recent review of mathematical modeling to evaluate the cost-effectiveness and epidemiological impact of novel diagnostic strategies for active TB (98), the authors highlighted the fact that no study had reported taking a societal perspective. Those authors stated the need for increased efforts to include patient-level costs of TB diagnosis as well as indirect costs that can have a significant impact on cost-effectiveness results.
Available cost-effectiveness studies show that the use of algorithms involving Xpert to diagnose TB infection is a beneficial and cost-effective strategy in resource-limited settings where TB and HIV prevalences are high. In these settings, such a strategy can potentially reduce TB incidence and mortality over the long term, and thus, health benefits overtake additional costs associated with testing, MDR-TB treatment, and HIV care (94). However, although strategies relying on Xpert are cost-effective, it should be noted that they are not necessarily sustainable, as their implementation at the health system level implies an increase in the health budget, which may not always be possible in highly resource-constrained setting. Evidence of the cost-effectiveness of Xpert is also more limited in northern countries where TB prevalence is low. Indeed, critical parameters identified in sensitivity analyses as impacting cost-effectiveness results are related to TB prevalence (as greater health benefits are obtained in countries with high TB prevalence) and the cost of diagnosis and treatment. Only two studies have taken the effects of TB transmission into account (94, 95), but all these studies take into account the uncertainty of parameters and assumptions made by the model structure, using multiway probabilistic sensitivity analysis. Despite some limitations, the studies were, overall, robust in sensitivity analyses.
Malaria
In Ethiopia, a study that enrolled 2,422 patients suspected of having malaria compared a presumptive treatment strategy with two strategies based on rapid diagnostic tests (RDTs) followed by treatment of identified malaria cases: the first using the Parascreen Pan/Pf test and the second using the Paracheck Pf test (99). The authors of that study estimated the number of correctly treated cases (CTCs) and computed incremental cost-effectiveness ratios per CTC. The presumptive treatment strategy dominated, as it was more expensive and less effective than the two RDT strategies. The Parascreen-based strategy was more effective and costlier than the Paracheck-based strategy, with an ICER of US$0.59 per CTC. Given the very low ICER of Parascreen compared to that of the Paracheck-based strategy, those authors concluded that the Parascreen test (100–103) should not been recommended for assessing strategies involving RDTs for malaria diagnosis in the settings of Uganda, Ghana, Zambia, and Brazil. These studies compared the three following strategies: presumptive treatment, field standard microscopy, and RDTs. All studies defined “effectiveness” as the number of cases correctly diagnosed and treated, with the exception of the last one, which considered only the number of cases correctly diagnosed (and thus did not consider treatment costs in the analysis). The first two studies found that microscopy was dominated by the RDT and that the RDT was very cost-effective (ICERs of “RDT” versus “presumptive” treatment were US$5.00 per case correctly diagnosed and treated in the first study and US$2.60 in the second) (100, 102). The third study, by Ansah et al., however, suggested that there was no advantage to replacing microscopy with the RDT, as the costs and health benefits of the two strategies were similar, but when the studies were compared in a setting without microscopy (i.e., relying on the presumptive strategy), the RDT was associated with a significantly increased proportion of patients being correctly treated and an ICER of US$8.30. In the last study, conducted in remote areas of Brazil, those authors compared only microscopy with the RDT and found that microscopy was costlier and more effective, with an incremental cost estimated at US$549.90 per adequately diagnosed case (103) when high sensitivity (92 to 95%) and specificity (100%) were maintained. Sensitivity analysis, however, highlighted that when the accuracy of microscopy was lower (i.e., sensitivity of 90 to 98% and specificity of 83%), the RDT was more cost-effective than microscopy. These results indicate that very high levels of microscopy accuracy are needed for microscopy to be more cost-effective than the RDT.
Moreover, a review of cost-effectiveness studies conducted between 2006 and 2010 to assess new malaria RDTs in the setting of sub-Saharan countries was reported (104). In this paper, we briefly report the main results of the studies included in that review. Using a decision tree model and probabilistic sensitivity analysis, Shillcutt et al. showed that RDTs have the potential to be cost-effective compared to both presumptive treatment and microscopy in most countries in sub-Saharan Africa (105). Uzochukwu et al. found similar results: they showed in Nigeria that microscopy was an inferior strategy and that RDTs were cost-effective compared to presumptive treatment, with an ICER of US$221 per death averted (106). Msellem et al. demonstrated that the RDT led to a 2-fold reduction in antimalarial drug prescription, but overall costs were similar in the POC and clinical diagnosis groups (107). Finally, the impact of malaria prevalence on the effectiveness and cost-effectiveness of RDT was assessed by Zurovac et al., who highlighted that RDTs led to a notable reduction in treatment errors, with lower costs in areas with a high rate of malaria transmission (30% to 40%), while in areas with a low prevalence of malaria, they yielded only minor reductions in overprescription, with higher costs (108).
Available studies suggest that RDTs are very cost-effective in comparison with the presumptive strategy, as they reduce costs related to ineffectual treatments due to the very poor specificity of presumptive treatment (100–103, 105). In settings where microscopy is available, the cost-effectiveness of POC testing depends on microscopy accuracy, which varies depending on the setting. In sub-Saharan Africa, where microscopy accuracy was low, Batwala et al. and Chanda et al. (100, 101) demonstrated that the RDT was cost-effective compared to microscopy, in contrast to a setting such as Brazil, where microscopy was associated with high sensitivity and specificity (102). Another key factor impacting the cost-effectiveness results of RDTs is the prevalence of malaria, because in high-prevalence settings, the health benefits provided by POC testing are greater at a lower cost than in settings with a low prevalence (105, 106, 108). This review showed that the cost-effectiveness results for RDTs were consistent across studies, suggesting that decision-makers should consider the use of RDTs, especially when malaria prevalence is high and microscopy accuracy is not low. Future studies are needed to assess the long-term benefits of RDTs in terms of the development of antimalarial resistance and improved antibiotic drug prescription.
Syphilis
The cost-effectiveness of different diagnostic strategies was estimated by studying 1,000 pregnant women in sub-Saharan Africa in 2008 (109). Using a computer-based model simulating health outcomes and costs over the life expectancy of a cohort of 1,000 women, the authors of that study compared four strategies: no screening, RPR tests with results confirmed by TPHA tests (standard strategy), single-visit RPR tests, and single-visit rapid ICS tests. The ICS test was the most effective and least costly strategy: compared to no screening, it averted 178 cases of congenital syphilis, 43 cases of low birth weight, and 37 prenatal deaths and saved US$170,030 per 1,000 women over their lifetime. However, results were highly sensitive to test kit, labor, and supply costs. Sensitivity analyses showed that when the cost of the ICS test more than doubled or when the ICS test sensitivity fell to below 88%, the RPR test was preferred.
In 2011, Owusu-Edusei et al. compared the same four strategies as those used by Rydzak and Goldie in the setting of sub-Saharan Africa but included an additional screening strategy using dual-POC testing (110). Costs and DALYs related to miscarriage, stillbirth, congenital syphilis, low birth weight, and neonatal death were estimated for each strategy over the life expectancy of a cohort of 1,000 pregnant women. Compared with no screening, the ICS test averted 326 DALYs per 1,000 women and 180 DALYs per 1,000 pregnancies. It also saved US$30,000, while the dual-POC strategy averted 299 and 162 DALYs (for 1,000 women and 1,000 pregnancies, respectively) at a cost savings of US$27,000. The ICS test was the preferred strategy, but sensitivity analysis showed that an increase in the RPR sensitivity from 60% to 98% implied that RPR testing would become more cost-effective than the dual-POC test.
Another cost-effectiveness analysis used a decision analytic model to assess the introduction of an ICS test followed by treatment compared to current practice (i.e., no screening and no treatment) in the setting of national antenatal care programs in 43 countries in sub-Saharan Africa (111). The authors of that study estimated DALYs, costs, and costs per DALY averted over the life expectancy of a hypothetical cohort of 10,000 pregnant women. The ICERs of ICS testing compared to no screening ranged between US$2 (Liberia) and US$48 (Botswana), with a population-weighted average of US$11 per DALY averted. As all ICERs were lower than the GDP per capita, those authors concluded that the ICS test was very cost-effective in the setting of sub-Saharan Africa. Moreover, findings were robust to variations of inputs in one-way sensitivity analyses.
The POC cost-effectiveness results for syphilis diagnosis were consistent across studies: POCTs were very cost-effective compared to no screening in the setting of sub-Saharan Africa, as their use was associated with significant health benefits for both women and children as well as with significant savings due to the lower need for future treatment in this population. Compared with different screening alternatives, ICS tests were found to be the least costly and most effective strategy. However, this finding was dictated by ICS price along with RPR and ICS sensitivity. These results strongly support the use of POCTs in sub-Saharan Africa, where the prevalence of syphilis is high. Among the main limitations of those studies, it should be noted that none took into account transmission to partners, which would probably improve the cost-effectiveness of screening, and only one assessed the long-term benefits of incidence reduction (111).
Chlamydia trachomatis
The cost-effectiveness of a vaginal swab POC test using the Chlamydia Rapid Test (CRT) versus a standard vaginal swab NAAT was measured by using a decision tree model (112). Model parameters were based on primary data derived from a sample of 154 eligible women recruited in sexually transmitted disease (STD) clinics in Baltimore, MD, between April 2010 and February 2011, supplemented with reported data and unpublished results. In the base case analysis (POC sensitivity of 92.9%, 47.5% of patients willing to wait 40 min for results, and test cost of US$33.48), POC testing was more effective and less costly than NAAT (ICER of −US$5,050 per case of PID averted). Threshold analysis also demonstrated that the POC strategy dominated the NAAT strategy when the POC test cost <US$41.52 or when sensitivity was ≥87.1%. Probabilistic sensitivity analyses, however, showed that in nearly half the simulations, POC testing would save money but avert fewer PID cases. The authors of that study concluded that if future POCT improvements were able to reduce waiting time while maintaining sensitivity, the use of POC testing would prevent more PIDs and become more cost-effective. A further systematic review aimed at establishing the incremental cost-effectiveness of two POC tests based on antibody/antigen (Clearview Chlamydia test and CRT) compared with standard laboratory NAATs (113). For a hypothetical cohort of 1,000 people, both POCTs were more expensive and less effective than the standard laboratory NAAT: routine PCR would result in 12.63 tested people being correctly treated and having their sexual partners contacted, at a cost of £7,070 (for the whole cohort), while for the CRT, 10.98 people would be tested at a cost of £7,180. For the Clearview Chlamydia test, 7.14 people would be tested at a cost of £7,170. These results were robust in terms of sensitivity analyses.
A recent study developed a decision analytic model simulating patient pathways to estimate the costs and benefits of implementing standard care pathways (off-site NAAT laboratory) and POC pathways, including a chlamydia/gonorrhea POC NAAT using the Cepheid Xpert CT/NG test (62). The authors of that study modeled a cohort of 1.2 million index patients to simulate the annual number of STI screenings performed at genitourinary medicine clinics in England. Compared with standard laboratory tests, the POC NAAT enabled 46 additional QALYs to be obtained and saved ∼£11.7 million. Even making pessimistic assumptions that the POC test will not prevent any overtreatment, complications, or transmissions, the POC pathway was superior. Same-day diagnosis and treatment could prevent >95,000 unnecessary treatments per year. Those authors concluded that replacing standard laboratory tests for chlamydia and gonorrhea with a POC NAAT could reduce costs, and patients would benefit from more accurate diagnosis and less unnecessary treatment.
All studies were conducted in European countries, and the first two studies assessed RDTs by screening the antigen, while Turner et al. studied a POCT based on PCR (62). A study conducted by Hislop et al. presented a short-term horizon (<1 year) and thus failed to consider any long-term health impacts (113). Turner et al. did not consider patient costs, effects due to the clinic demands for POC tests, or indirect PID complications such as epididymitis (62). Studies based on antigen screening tests (110, 114) appeared to be less accurate than the PCR method, implying that POCTs were not a cost-effective strategy (109). Those studies presented some uncertainty regarding estimates of variables and the incidence of PID in untreated women. They did not take into account indirect complications of PID or its transmission to partners, and the results were dependent upon POCT price and Chlamydia prevalence.
Conclusion
Despite different issues, POCTs appear to be cost-effective for the diagnosis of tuberculosis, malaria, and syphilis in comparison with current diagnostic strategies in both southern and northern countries, leading to cost savings in some situations. It is worth noting that very few cost-effectiveness studies were conducted in northern countries, and these studies mainly concerned infectious disease caused by Chlamydia. POCTs increased the number of correct diagnoses in resource-limited settings, provided rapid test results, and enabled physicians to make decisions regarding patient treatment, notably at the time of care. Their rapidity and ease of use influenced their deployment worldwide. Moreover, the use of POCTs allows exploration by syndrome. Cost-effectiveness depends on the sensitivity of diagnostic tests and their prices. Improvements of these parameters would make these tests even more cost-effective and would enable health interventions to promote the use of POCTs for improving patient care.
FUTURE DIRECTIONS
It is clear that a radical change has been made in diagnostic microbiology during the 21st century (1). Indeed, it is now possible to reach a diagnosis at the time of care using the latest molecular techniques with lower production costs. The level of technology training for test performance is very low, and it is likely that technical training for persons with no biological background will be extremely fast and simple. Validation will soon be performed remotely over the Internet or via direct data transmission. In terms of a more speculative future, three-dimensional (3D) printer technology and remote fault diagnosis will repair some failures using a small stock of materials, including versatile components (115). The development of microfluidic PCR will allow dozens of microorganisms to be rapidly tested at low cost (116). Smartphone-operated enzyme-linked immunosorbent assays (ELISAs) have already been reported (117). The connection of all real-time data will enable epidemiological surveillance, the significance of which is difficult to imagine at this time. The key elements of the global development strategy of outsourced points of care will be based on a first-stage repertoire. Indeed, epidemiological situations lead to variations in pathogenic microorganisms depending on geographic location and time. Therefore, there will always be a need for highly equipped laboratories in order to identify the repertoire of microorganisms as well as their sensitivity to antimicrobial agents. However, it is likely that these sites will be limited in number and will provide regional poles of reference and infectious agent repertoire monitoring. At other sites, once the repertoire has been established and detection tools are in place, very simple molecular tools may be sufficient to allow medical staff to answer simple questions. Accordingly, the rapid detection of antimicrobial resistance, currently limited to a few antibiotics, will be expanded to assist doctors in reaching treatment decisions (118). Test organization will likely be a syndromic approach, validation will be performed remotely, and it is easy to imagine that this could be connected to the therapeutic management system.
The combination of a repertoire of geographic infections, the syndromic approach, and the versatility of microorganism testing and remote validation are the steps in this clinical microbiological revolution.
ACKNOWLEDGMENTS
D.R. and M.D. are cofounders and shareholders of POCRAMé, a startup devoted to the design, development, and sale of POC solutions for clinical microbiology. POCRAMé tested POC onboard a CMA-CGM maritime company vessel.
Biographies

Michel Drancourt is Professor of Microbiology at Aix Marseille University and Head of the Microbiology Laboratory at the Marseille public hospital. His research topics include mycobacteria, neglected organisms, and paleomicrobiology, and he participated in the promotion of point-of-care testing in clinical microbiology.

Audrey Michel-Lepage received her Ph.D. in health economics at Aix Marseille University. Her research focuses on antibiotic prescriptions, medical behaviors, physician payments, and health systems. She was involved in studying the cost-effectiveness of the point-of-care strategy in clinical microbiology.

Sylvie Boyer is Associate Professor in Health Economics at Aix Marseille University. Her research activities include social and economic science as well as psychological and social epidemiology of cancer, aging, and infectious diseases. She is currently involved in several multidisciplinary research programs implemented in sub-Saharan Africa and coordinates the socioeconomic aspects of these programs. Her current research interests include the economic evaluation of innovative treatment strategies, health systems, and health care service performance; risky behaviors in the field of infectious diseases; and the socioeconomic impacts of disease.

Didier Raoult is Professor of Microbiology at Aix Marseille University and Head of the Méditerranée Infection Institute. He has authored and coauthored more than 2,100 papers covering numerous fields in microbiology, infections, and tropical diseases. Professor Raoult has promoted several revolutions in clinical microbiology, including the invention and the development of point-of-care systems.
REFERENCES
- 1.Fournier PE, Drancourt M, Colson P, Rolain JM, La Scola B, Raoult D. 2013. Modern clinical microbiology: new challenges and solutions. Nat Rev Microbiol 11:574–585. doi: 10.1038/nrmicro3068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bossuyt X, Verweire K, Blanckaert N. 2007. Laboratory medicine: challenges and opportunities. Clin Chem 53:1730–1733. doi: 10.1373/clinchem.2007.093989. [DOI] [PubMed] [Google Scholar]
- 3.Nugent RP, Krohn MA, Hillier SL. 1991. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol 29:297–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sokhna C, Mediannikov O, Fenollar F, Bassene H, Diatta G, Tall A, Trape JF, Drancourt M, Raoult D. 2013. Point-of-care laboratory of pathogen diagnosis in rural Senegal. PLoS Negl Trop Dis 7:e1999. doi: 10.1371/journal.pntd.0001999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bouricha M, Samad MA, Levy PY, Raoult D, Drancourt M. 2014. Point-of-care syndrome-based, rapid diagnosis of infections on commercial ships. J Travel Med 21:12–16. doi: 10.1111/jtm.12090. [DOI] [PubMed] [Google Scholar]
- 6.Schito M, Peter TF, Cavanaugh S, Piatek AS, Young GJ, Alexander H, Coggin W, Domingo GJ, Ellenberger D, Ermantraut E, Jani IV, Katamba A, Palamountain KM, Essajee S, Dowdy DW. 2012. Opportunities and challenges for cost-efficient implementation of new point-of-care diagnostics for HIV and tuberculosis. J Infect Dis 205(Suppl 2):S169–S180. doi: 10.1093/infdis/jis044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kost GJ. 2002. Principles and practice of point-of-care testing, 1st ed Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- 8.Price CP. 2001. Point of care testing. BMJ 322:1285–1288. doi: 10.1136/bmj.322.7297.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reid A. 2012. Bringing the lab to the patient: developing point-of-care diagnostics for resource limited settings. American Academy of Microbiology, Washington, DC. [PubMed] [Google Scholar]
- 10.Peeling RW, Mabey D. 2010. Point-of-care tests for diagnosing infections in the developing world. Clin Microbiol Infect 16:1062–1069. doi: 10.1111/j.1469-0691.2010.03279.x. [DOI] [PubMed] [Google Scholar]
- 11.Ninove L, Gazin C, Gould EA, Nougairede A, Flahault A, Charrel RN, Zandotti C, de Lamballerie X. 2010. Impact of diagnostic procedures on patient management and hospitalization cost during the 2000 and 2005 enterovirus epidemics in Marseilles, France. Clin Microbiol Infect 16:651–656. doi: 10.1111/j.1469-0691.2009.02915.x. [DOI] [PubMed] [Google Scholar]
- 12.Rashid H, Shafi S, Haworth E, El Bashir H, Ali KA, Memish ZA, Booy R. 2007. Value of rapid testing for influenza among Hajj pilgrims. Travel Med Infect Dis 5:310–313. doi: 10.1016/j.tmaid.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 13.Nie S, Roth RB, Stiles J, Mikhlina A, Lu X, Tang YW, Babady NE. 2014. Evaluation of Alere i Influenza A&B for rapid detection of influenza viruses A and B. J Clin Microbiol 52:3339–3344. doi: 10.1128/JCM.01132-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Francois P, Tangomo M, Hibbs J, Bonetti EJ, Boehme CC, Notomi T, Perkins MD, Schrenzel J. 2011. Robustness of a loop-mediated isothermal amplification reaction for diagnostic applications. FEMS Immunol Med Microbiol 62:41–48. doi: 10.1111/j.1574-695X.2011.00785.x. [DOI] [PubMed] [Google Scholar]
- 15.Sattabongkot J, Tsuboi T, Han ET, Bantuchai S, Buates S. 2014. Loop-mediated isothermal amplification assay for rapid diagnosis of malaria infections in an area of endemicity in Thailand. J Clin Microbiol 52:1471–1477. doi: 10.1128/JCM.03313-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beissner M, Phillips RO, Battke F, Bauer M, Badziklou K, Sarfo FS, Maman I, Rhomberg A, Piten E, Frimpong M, Huber KL, Symank D, Jansson M, Wiedemann FX, Banla Kere A, Herbinger KH, Löscher T, Bretzel G. 2015. Loop-mediated isothermal amplification for laboratory confirmation of Buruli ulcer disease—towards a point-of-care test. PLoS Negl Trop Dis 9:e0004219. doi: 10.1371/journal.pntd.0004219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Drancourt M, Gaydos CA, Summersgill JT, Raoult D. 2013. Point-of-care testing for community-acquired pneumonia. Lancet Infect Dis 13:647–649. doi: 10.1016/S1473-3099(13)70165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tan JJ, Capozzoli M, Sato M, Watthanaworawit W, Ling CL, Mauduit M, Malleret B, Grüner AC, Tan R, Nosten FH, Snounou G, Rénia L, Ng LF. 2014. An integrated lab-on-chip for rapid identification and simultaneous differentiation of tropical pathogens. PLoS Negl Trop Dis 8:e3043. doi: 10.1371/journal.pntd.0003043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thamcharoen N, Sornprom S, Permpalung N, Hyman CL. 2015. False positivity of monospot test in an immunocompetent elderly woman with acute cytomegalovirus infection. Am J Emerg Med 33:1544.e1–1544.e2. doi: 10.1016/j.ajem.2015.07.028. [DOI] [PubMed] [Google Scholar]
- 20.Cunha BA, Munoz-Gomez S. 2014. Dengue fever in a returning traveller from El Salvador: another cause of a false positive monospot test. Travel Med Infect Dis 12:293–295. doi: 10.1016/j.tmaid.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 21.Kesavan SV, Momey F, Cioni O, David-Watine B, Dubrulle N, Shorte S, Sulpice E, Freida D, Chalmond B, Dinten JM, Gidrol X, Allier C. 2014. High-throughput monitoring of major cell functions by means of lensfree video microscopy. Sci Rep 4:5942. doi: 10.1038/srep05942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cooke J, Butler C, Hopstaken R, Dryden MS, McNulty C, Hurding S, Moore M, Livermore DM. 2015. Narrative review of primary care point-of-care testing (POCT) and antibacterial use in respiratory tract infection (RTI). BMJ Open Respir Res 2:e000086. doi: 10.1136/bmjresp-2015-000086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moore CC, Jacob ST, Pinkerton R, Meya DB, Mayanja-Kizza H, Reynolds SJ, Scheld WM. 2008. Point-of-care lactate testing predicts mortality of severe sepsis in a predominantly HIV type 1-infected patient population in Uganda. Clin Infect Dis 46:215–222. doi: 10.1086/524665. [DOI] [PubMed] [Google Scholar]
- 24.D'Acremont V, Kilowoko M, Kyungu E, Philipina S, Sangu W, Kahama-Maro J, Lengeler C, Cherpillod P, Kaiser L, Genton B. 2014. Beyond malaria—causes of fever in outpatient Tanzanian children. N Engl J Med 370:809–817. doi: 10.1056/NEJMoa1214482. [DOI] [PubMed] [Google Scholar]
- 25.Dubourg G, Fenollar F. 2015. Epidemiologic studies need asymptomatic controls. Clin Microbiol Infect 21:e51–e52. doi: 10.1016/j.cmi.2015.04.020. [DOI] [PubMed] [Google Scholar]
- 26.Yen CW, de Puig H, Tam JO, Gómez-Márquez J, Bosch I, Hamad-Schifferli K, Gehrke L. 2015. Multicolored silver nanoparticles for multiplexed disease diagnostics: distinguishing dengue, yellow fever, and Ebola viruses. Lab Chip 15:1638–1641. doi: 10.1039/C5LC00055F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mourembou G, Fenollar F, Socolovschi C, Lemamy GJ, Nzoughe H, Kouna LC, Toure-Ndouo F, Million M, Mbiguino AN, Lekana-Douki JB, Raoult D. 2015. Molecular detection of fastidious and common bacteria as well as Plasmodium spp. in febrile and afebrile children in Franceville, Gabon. Am J Trop Med Hyg 92:926–932. doi: 10.4269/ajtmh.14-0699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fujii Y, Kaneko S, Nzou SM, Mwau M, Njenga SM, Tanigawa C, Kimotho J, Mwangi AW, Kiche I, Matsumoto S, Niki M, Osada-Oka M, Ichinose Y, Inoue M, Itoh M, Tachibana H, Ishii K, Tsuboi T, Yoshida LM, Mondal D, Haque R, Hamano S, Changoma M, Hoshi T, Kamo K, Karama M, Miura M, Hirayama K. 2014. Serological surveillance development for tropical infectious diseases using simultaneous microsphere-based multiplex assays and finite mixture models. PLoS Negl Trop Dis 8:e3040. doi: 10.1371/journal.pntd.0003040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mueller Y, D'Acremont V, Ambresin AE, Rossi I, Martin O, Burnand B, Genton B. 2014. Feasibility and clinical outcomes when using practice guidelines for evaluation of fever in returning travelers and migrants: a validation study. J Travel Med 21:169–182. doi: 10.1111/jtm.12099. [DOI] [PubMed] [Google Scholar]
- 30.Otten M, Aregawi M, Were W, Karema C, Medin A, Bekele W, Jima D, Gausi K, Komatsu R, Korenromp E, Low-Beer D, Grabowsky M. 2009. Initial evidence of reduction of malaria cases and deaths in Rwanda and Ethiopia due to rapid scale-up of malaria prevention and treatment. Malar J 8:14. doi: 10.1186/1475-2875-8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.WHO. 2013. Malaria rapid diagnostic test performance. Results of WHO product testing of malaria RDTs: round 5 (2013). World Health Organization, Geneva, Switzerland. [Google Scholar]
- 32.Hunsperger EA, Yoksan S, Buchy P, Nguyen VC, Sekaran SD, Enria DA, Vazquez S, Cartozian E, Pelegrino JL, Artsob H, Guzman MG, Olliaro P, Zwang J, Guillerm M, Kliks S, Halstead S, Peeling RW, Margolis HS. 2014. Evaluation of commercially available diagnostic tests for the detection of dengue virus NS1 antigen and anti-dengue virus IgM antibody. PLoS Negl Trop Dis 8:e3171. doi: 10.1371/journal.pntd.0003171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mediannikov O, Socolovschi C, Million M, Sokhna C, Bassene H, Diatta G, Fenollar F, Raoult D. 2014. Molecular identification of pathogenic bacteria in eschars from acute febrile patients, Senegal. Am J Trop Med Hyg 91:1015–1019. doi: 10.4269/ajtmh.13-0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mediannikov O, Socolovschi C, Bassene H, Diatta G, Ratmanov P, Fenollar F, Sokhna C, Raoult D. 2014. Borrelia crocidurae infection in acutely febrile patients, Senegal. Emerg Infect Dis 20:1335–1338. doi: 10.3201/eid2008.130550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mediannikov O, Socolovschi C, Edouard S, Fenollar F, Mouffok N, Bassene H, Diatta G, Tall A, Niangaly H, Doumbo O, Lekana-Douki JB, Znazen A, Sarih M, Ratmanov P, Richet H, Ndiath MO, Sokhna C, Parola P, Raoult D. 2013. Common epidemiology of Rickettsia felis infection and malaria, Africa. Emerg Infect Dis 19:1775–1783. doi: 10.3201/eid1911.130361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Strecker T, Palyi B, Ellerbrok H, Jonckheere S, de Clerck H, Bore JA, Gabriel M, Stoecker K, Eickmann M, van Herp M, Formenty P, Di Caro A, Becker S. 2015. Field evaluation of capillary blood samples as a collection specimen for the rapid diagnosis of Ebola virus infection during an outbreak emergency. Clin Infect Dis 61:669–675. doi: 10.1093/cid/civ397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Broadhurst MJ, Kelly JD, Miller A, Semper A, Bailey D, Groppelli E, Simpson A, Brooks T, Hula S, Nyoni W, Sankoh AB, Kanu S, Jalloh A, Ton Q, Sarchet N, George P, Perkins MD, Wonderly B, Murray M, Pollock NR. 2015. ReEBOV Antigen Rapid Test kit for point-of-care and laboratory-based testing for Ebola virus disease: a field validation study. Lancet 386:867–874. doi: 10.1016/S0140-6736(15)61042-X. [DOI] [PubMed] [Google Scholar]
- 38.GBD 2013 Mortality and Causes of Death Collaborators. 2015. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 385:117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhou H, Haber M, Ray S, Farley MM, Panozzo CA, Klugman KP. 2012. Invasive pneumococcal pneumonia and respiratory virus co-infections. Emerg Infect Dis 18:294–297. doi: 10.3201/eid1802.102025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shimada T, Noguchi Y, Jackson JL, Miyashita J, Hayashino Y, Kamiya T, Yamazaki S, Matsumura T, Fukuhara S. 2009. Systematic review and metaanalysis: urinary antigen tests for legionellosis. Chest 136:1576–1585. doi: 10.1378/chest.08-2602. [DOI] [PubMed] [Google Scholar]
- 41.Sordé R, Falcó V, Lowak M, Domingo E, Ferrer A, Burgos J, Puig M, Cabral E, Len O, Pahissa A. 2011. Current and potential usefulness of pneumococcal urinary antigen detection in hospitalized patients with community-acquired pneumonia to guide antimicrobial therapy. Arch Intern Med 171:166–172. doi: 10.1001/archinternmed.2010.347. [DOI] [PubMed] [Google Scholar]
- 42.Cho CH, Woo MK, Kim JY, Cheong S, Lee CK, An SA, Lim CS, Kim WJ. 2013. Evaluation of five rapid diagnostic kits for influenza A/B virus. J Virol Methods 187:51–56. doi: 10.1016/j.jviromet.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 43.Salez N, Nougairede A, Ninove L, Zandotti C, de Lamballerie X, Charrel RN. 2014. Xpert Flu for point-of-care diagnosis of human influenza in industrialized countries. Expert Rev Mol Diagn 14:411–418. doi: 10.1586/14737159.2014.901152. [DOI] [PubMed] [Google Scholar]
- 44.Salez N, Nougairede A, Ninove L, Zandotti C, de Lamballerie X, Charrel RN. 2015. Prospective and retrospective evaluation of the Cepheid Xpert Flu/RSV XC assay for rapid detection of influenza A, influenza B, and respiratory syncytial virus. Diagn Microbiol Infect Dis 81:256–258. doi: 10.1016/j.diagmicrobio.2015.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.World Health Organization. 2014. Global tuberculosis report. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 46.World Health Organization. 2014. TB diagnostics and laboratory strengthening. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 47.Berg P, Lindhardt BØ. 2012. The role of procalcitonin in adult patients with community-acquired pneumonia—a systematic review. Dan Med J 59:A4357. [PubMed] [Google Scholar]
- 48.Pillet S, Lardeux M, Dina J, Grattard F, Verhoeven P, Le Goff J, Vabret A, Pozzetto B. 2013. Comparative evaluation of six commercialized multiplex PCR kits for the diagnosis of respiratory infections. PLoS One 8:e72174. doi: 10.1371/journal.pone.0072174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Leone M, Malavieille F, Papazian L, Meyssignac B, Cassir N, Textoris J, Antonini F, La Scola B, Martin C, Allaouchiche B, Hraiech S, AzuRea Network . 2013. Routine use of Staphylococcus aureus rapid diagnostic test in patients with suspected ventilator-associated pneumonia. Crit Care 17:R170. doi: 10.1186/cc12849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Khare R, Espy MJ, Cebelinski E, Boxrud D, Sloan LM, Cunningham SA, Pritt BS, Patel R, Binnicker MJ. 2014. Comparative evaluation of two commercial multiplex panels for detection of gastrointestinal pathogens by use of clinical stool specimens. J Clin Microbiol 52:3667–3673. doi: 10.1128/JCM.01637-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lagier JC, Delord M, Million M, Parola P, Stein A, Brouqui P, Raoult D. 2015. Dramatic reduction in Clostridium difficile ribotype 027-associated mortality with early fecal transplantation by the nasogastric route: a preliminary report. Eur J Clin Microbiol Infect Dis 34:1597–1601. doi: 10.1007/s10096-015-2394-x. [DOI] [PubMed] [Google Scholar]
- 52.Orellana-Miguel MA, Alcolea-Medina A, Barrado-Blanco L, Rodriguez-Otero J, Chaves-Sánchez F. 2013. Algorithm proposal based on the C. Diff Quik Chek Complete ICT device for detecting Clostridium difficile infection. Enferm Infecc Microbiol Clin 31:97–99. doi: 10.1016/j.eimc.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 53.Goldenberg SD, Bisnauthsing KN, Patel A, Postulka A, Wyncoll D, Schiff R, French GL. 2014. Point-of-care testing for Clostridium difficile infection: a real-world feasibility study of a rapid molecular test in two hospital settings. Infect Dis Ther 3:295–306. doi: 10.1007/s40121-014-0038-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Eckert C, Emirian A, Le Monnier A, Cathala L, De Montclos H, Goret J, Berger P, Petit A, De Chevigny A, Jean-Pierre H, Nebbad B, Camiade S, Meckenstock R, Lalande V, Marchandin H, Barbut F. 2014. Prevalence and pathogenicity of binary toxin-positive Clostridium difficile strains that do not produce toxins A and B. New Microbes New Infect 3:12–17. doi: 10.1016/j.nmni.2014.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dediste A, Vandenberg O, Vlaes L, Ebraert A, Douat N, Bahwere P, Butzler JP. 2003. Evaluation of the ProSpecT microplate assay for detection of Campylobacter: a routine laboratory perspective. Clin Microbiol Infect 9:1085–1090. doi: 10.1046/j.1469-0691.2003.00705.x. [DOI] [PubMed] [Google Scholar]
- 56.Taneja N, Nato F, Dartevelle S, Sire JM, Garin B, Thi Phuong LN, Diep TT, Shako JC, Bimet F, Filliol I, Muyembe JJ, Ungeheuer MN, Ottone C, Sansonetti P, Germani Y. 2011. Dipstick test for rapid diagnosis of Shigella dysenteriae 1 in bacterial cultures and its potential use on stool samples. PLoS One 6:e24830. doi: 10.1371/journal.pone.0024830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Duran C, Nato F, Dartevelle S, Thi Phuong LN, Taneja N, Ungeheuer MN, Soza G, Anderson L, Benadof D, Zamorano A, Diep TT, Nguyen TQ, Nguyen VH, Ottone C, Bégaud E, Pahil S, Prado V, Sansonetti P, Germani Y. 2013. Rapid diagnosis of diarrhea caused by Shigella sonnei using dipsticks; comparison of rectal swabs, direct stool and stool culture. PLoS One 8:e80267. doi: 10.1371/journal.pone.0080267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Smith L, Angarone MP. 2015. Sexually transmitted infections. Urol Clin North Am 42:507–518. doi: 10.1016/j.ucl.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 59.Huppert JS, Taylor RG, St Cyr S, Hesse EA, Reed JL. 2013. Point-of-care testing improves accuracy of STI care in an emergency department. Sex Transm Infect 89:489–494. doi: 10.1136/sextrans-2012-050994. [DOI] [PubMed] [Google Scholar]
- 60.Tucker JD, Bien CH, Peeling RW. 2013. Point-of-care testing for sexually transmitted infections: recent advances and implications for disease control. Curr Opin Infect Dis 26:73–79. doi: 10.1097/QCO.0b013e32835c21b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jafari Y, Johri M, Joseph L, Vadnais C, Pant Pai N. 2014. Poor reporting of outcomes beyond accuracy in point-of-care tests for syphilis: a call for a framework. AIDS Res Treat 2014:465932. doi: 10.1155/2014/465932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Turner KM, Round J, Horner P, Macleod J, Goldenberg S, Deol A, Adams EJ. 2014. An early evaluation of clinical and economic costs and benefits of implementing point of care NAAT tests for Chlamydia trachomatis and Neisseria gonorrhoeae in genitourinary medicine clinics in England. Sex Transm Infect 90:104–111. doi: 10.1136/sextrans-2013-051147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bretelle F, Rozenberg P, Pascal A, Favre R, Bohec C, Loundou A, Senat MV, Aissi G, Lesavre N, Brunet J, Heckenroth H, Luton D, Raoult D, Fenollar F, Groupe de Recherche en Obstetrique Gynecologie . 2015. High Atopobium vaginae and Gardnerella vaginalis vaginal loads are associated with preterm birth. Clin Infect Dis 60:860–867. doi: 10.1093/cid/ciu966. [DOI] [PubMed] [Google Scholar]
- 64.Blankenstein T, Lytton SD, Leidl B, Atweh E, Friese K, Mylonas I. 2015. Point-of-care (POC) diagnosis of bacterial vaginosis (BV) using VGTest ion mobility spectrometry (IMS) in a routine ambulatory care gynecology clinic. Arch Gynecol Obstet 292:355–362. doi: 10.1007/s00404-014-3613-x. [DOI] [PubMed] [Google Scholar]
- 65.Allier CP, Hiernard G, Poher V, Dinten JM. 2010. Bacteria detection with thin wetting film lensless imaging. Biomed Opt Express 1:762–770. doi: 10.1364/BOE.1.000762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cohen-Bacrie S, Ninove L, Nougairède A, Charrel R, Richet H, Minodier P, Badiaga S, Noël G, La Scola B, de Lamballerie X, Drancourt M, Raoult D. 2011. Revolutionizing clinical microbiology laboratory organization in hospitals with in situ point-of-care. PLoS One 6:e22403. doi: 10.1371/journal.pone.0022403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Boulware DR, Rolfes MA, Rajasingham R, von Hohenberg M, Qin Z, Taseera K, Schutz C, Kwizera R, Butler EK, Meintjes G, Muzoora C, Bischof JC, Meya DB. 2014. Multisite validation of cryptococcal antigen lateral flow assay and quantification by laser thermal contrast. Emerg Infect Dis 20:45–53. doi: 10.3201/eid2001.130906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jarvis JN, Percival A, Bauman S, Pelfrey J, Meintjes G, Williams GN, Longley N, Harrison TS, Kozel TR. 2011. Evaluation of a novel point-of-care cryptococcal antigen test on serum, plasma, and urine from patients with HIV-associated cryptococcal meningitis. Clin Infect Dis 53:1019–1023. doi: 10.1093/cid/cir613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kwizera R, Nguna J, Kiragga A, Nakavuma J, Rajasingham R, Boulware DR, Meya DB. 2014. Performance of cryptococcal antigen lateral flow assay using saliva in Ugandans with CD4 <100. PLoS One 9:e103156. doi: 10.1371/journal.pone.0103156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chapin KC, Blake P, Wilson CD. 2002. Performance characteristics and utilization of rapid antigen test, DNA probe, and culture for detection of group A streptococci in an acute care clinic. J Clin Microbiol 40:4207–4210. doi: 10.1128/JCM.40.11.4207-4210.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Calviño O, Llor C, Gómez F, González E, Sarvisé C, Hernández S. 2014. Association between C-reactive protein rapid test and group A streptococcus infection in acute pharyngitis. J Am Board Fam Med 27:424–426. doi: 10.3122/jabfm.2014.03.130315. [DOI] [PubMed] [Google Scholar]
- 72.Weber NC, Klepser ME, Akers JM, Klepser DG, Adams AJ. 2016. Use of CLIA-waived point-of-care tests for infectious diseases in community pharmacies in the United States. Expert Rev Mol Diagn 16:253–264. doi: 10.1586/14737159.2015.1116388. [DOI] [PubMed] [Google Scholar]
- 73.Swain GR, McDonald RA, Pfister JR, Gradus MS, Sedmak GV, Singh A. 2004. Decision analysis: point-of-care chlamydia testing vs. laboratory-based methods. Clin Med Res 2:29–35. doi: 10.3121/cmr.2.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nicol MP, Whitelaw A, Wendy S. 2013. Using Xpert MTB/RIF. Curr Respir Med Rev 9:187–192. doi: 10.2174/1573398X113099990015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Boehme CC, Nicol MP, Nabeta P, Michael JS, Gotuzzo E, Tahirli R, Gler MT, Blakemore R, Worodria W, Gray C, Huang L, Caceres T, Mehdiyev R, Raymond L, Whitelaw A, Sagadevan K, Alexander H, Albert H, Cobelens F, Cox H, Alland D, Perkins MD. 2011. Feasibility, diagnostic accuracy, and effectiveness of decentralised use of the Xpert MTB/RIF test for diagnosis of tuberculosis and multidrug resistance: a multicentre implementation study. Lancet 377:1495–1505. doi: 10.1016/S0140-6736(11)60438-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Patel JC, Lucchi NW, Srivastava P, Lin JT, Sug-Aram R, Aruncharus S, Bharti PK, Shukla MM, Congpuong K, Satimai W, Singh N, Udhayakumar V, Meshnick SR. 2014. Field evaluation of a real-time fluorescence loop-mediated isothermal amplification assay, RealAmp, for the diagnosis of malaria in Thailand and India. J Infect Dis 210:1180–1187. doi: 10.1093/infdis/jiu252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Goyal A, Kaur H, Sehgal A, Sehgal R. 2015. RealAmp loop-mediated isothermal amplification as a point-of-care test for diagnosis of malaria: neither too close nor too far. J Infect Dis 211:1686. doi: 10.1093/infdis/jiu810. [DOI] [PubMed] [Google Scholar]
- 78.Babonneau J, Bernard C, Marion E, Chauty A, Kempf M, Robert R, Marsollier L, Franco-Beninese Buruli Research Group . 2015. Development of a dry-reagent-based qPCR to facilitate the diagnosis of Mycobacterium ulcerans infection in endemic countries. PLoS Negl Trop Dis 9:e0003606. doi: 10.1371/journal.pntd.0003606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Moore C. 2013. Point-of-care tests for infection control: should rapid testing be in the laboratory or at the front line? J Hosp Infect 85:1–7. doi: 10.1016/j.jhin.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 80.Fox JW, Cohen DM, Marcon MJ, Cotton WH, Bonsu BK. 2006. Performance of rapid streptococcal antigen testing varies by personnel. J Clin Microbiol 44:3918–3922. doi: 10.1128/JCM.01399-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Menard JP, Fenollar F, Raoult D, Boubli L, Bretelle F. 2012. Self-collected vaginal swabs for the quantitative real-time polymerase chain reaction assay of Atopobium vaginae and Gardnerella vaginalis and the diagnosis of bacterial vaginosis. Eur J Clin Microbiol Infect Dis 31:513–518. doi: 10.1007/s10096-011-1341-8. [DOI] [PubMed] [Google Scholar]
- 82.Tamalet C, Le Retraite L, Leandri FX, Heid P, Sancho Garnier H, Piana L. 2013. Vaginal self-sampling is an adequate means of screening HR-HPV types in women not participating in regular cervical cancer screening. Clin Microbiol Infect 19:E44–E50. doi: 10.1111/1469-0691.12063. [DOI] [PubMed] [Google Scholar]
- 83.Paudyal P, Llewellyn C, Lau J, Mahmud M, Smith H. 2015. Obtaining self-samples to diagnose curable sexually transmitted infections: a systematic review of patients' experiences. PLoS One 10:e0124310. doi: 10.1371/journal.pone.0124310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Anonymous. 2009. Clinical laboratory improvement amendments (CLIA). US Department of Health and Human Services, Washington, DC. [Google Scholar]
- 85.Smit PW, Mabey D, van der Vlis T, Korporaal H, Mngara J, Changalucha J, Todd J, Peeling RW. 2013. The implementation of an external quality assurance method for point-of-care tests for HIV and syphilis in Tanzania. BMC Infect Dis 13:530. doi: 10.1186/1471-2334-13-530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pai NP, Vadnais C, Denkinger C, Engel N, Pai M. 2012. Point-of-care testing for infectious diseases: diversity, complexity, and barriers in low- and middle-income countries. PLoS Med 9:e1001306. doi: 10.1371/journal.pmed.1001306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Abat C, Chaudet H, Colson P, Rolain JM, Raoult D. 2015. Real-time microbiology laboratory surveillance system to detect abnormal events and emerging infections, Marseille, France. Emerg Infect Dis 21:1302–1310. doi: 10.3201/eid2108.141419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Angelakis E, Mediannikov O, Socolovschi C, Mouffok N, Bassene H, Tall A, Niangaly H, Doumbo O, Znazen A, Sarih M, Sokhna C, Raoult D. 2014. Coxiella burnetii-positive PCR in febrile patients in rural and urban Africa. Int J Infect Dis 28:107–110. doi: 10.1016/j.ijid.2014.05.029. [DOI] [PubMed] [Google Scholar]
- 89.Fine AM, Nizet V, Mandl KD. 2011. Improved diagnostic accuracy of group A streptococcal pharyngitis with use of real-time biosurveillance. Ann Intern Med 155:345–352. doi: 10.7326/0003-4819-155-6-201109200-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Holm A, Cordoba G, Sørensen TM, Jessen LR, Siersma V, Bjerrum L. 2015. Point of care susceptibility testing in primary care—does it lead to a more appropriate prescription of antibiotics in patients with uncomplicated urinary tract infections? Protocol for a randomized controlled trial. BMC Fam Pract 16:106. doi: 10.1186/s12875-015-0322-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ninove L, Nougairede A, Gazin C, Zandotti C, Drancourt M, de Lamballerie X, Charrel RN. 2011. Comparative detection of enterovirus RNA in cerebrospinal fluid: GeneXpert system vs. real-time RT-PCR assay. Clin Microbiol Infect 17:1890–1894. doi: 10.1111/j.1469-0691.2011.03487.x. [DOI] [PubMed] [Google Scholar]
- 92.WHO. 2015. Cost-effectiveness thresholds. WHO, Geneva, Switzerland. [Google Scholar]
- 93.Vassall A, van Kampen S, Sohn H, Michael JS, John KR, den Boon S, Davis JL, Whitelaw A, Nicol MP, Gler MT, Khaliqov A, Zamudio C, Perkins MD, Boehme CC, Cobelens F. 2011. Rapid diagnosis of tuberculosis with the Xpert MTB/RIF assay in high burden countries: a cost-effectiveness analysis. PLoS Med 8:e1001120. doi: 10.1371/journal.pmed.1001120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Menzies NA, Cohen T, Lin H-H, Murray M, Salomon JA. 2012. Population health impact and cost-effectiveness of tuberculosis diagnosis with Xpert MTB/RIF: a dynamic simulation and economic evaluation. PLoS Med 9:e1001347. doi: 10.1371/journal.pmed.1001347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Langley I, Lin HH, Egwaga S, Doulla B, Ku CC, Murray M, Cohen T, Squire SB. 2014. Assessment of the patient, health system, and population effects of Xpert MTB/RIF and alternative diagnostics for tuberculosis in Tanzania: an integrated modeling approach. Lancet Glob Health 2:e581–e591. doi: 10.1016/S2214-109X(14)70291-8. [DOI] [PubMed] [Google Scholar]
- 96.Winetsky DE, Negoescu DM, DeMarchis EH, Almukhamedova O, Dooronbekova A, Pulatov D, Vezhnina N, Owens DK, Goldhaber-Fiebert JD. 2012. Screening and rapid molecular diagnosis of tuberculosis in prisons in Russia and Eastern Europe: a cost-effectiveness analysis. PLoS Med 9:e1001348. doi: 10.1371/journal.pmed.1001348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Choi HW, Miele K, Dowdy D, Shah M. 2013. Cost-effectiveness of Xpert MTB/RIF for diagnosing pulmonary tuberculosis in the United States. Int J Tuberc Lung Dis 17:1328–1335. doi: 10.5588/ijtld.13.0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zwerling A, White RG, Vassall A, Cohen T, Dowdy DW, Houben RM. 2014. Modeling of novel diagnostic strategies for active tuberculosis—a systematic review: current practices and recommendations. PLoS One 9:e110558. doi: 10.1371/journal.pone.0110558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lemma H, Sebastian MS, Löfgren C, Barnabas G. 2011. Cost-effectiveness of three malaria treatment strategies in rural Tigray, Ethiopia where both Plasmodium falciparum and Plasmodium vivax co-dominate. Cost Eff Resour Alloc 9:2. doi: 10.1186/1478-7547-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Batwala V, Magnussen P, Hansen KS, Nuwaha F. 2011. Cost-effectiveness of malaria microscopy and rapid diagnostic tests versus presumptive diagnosis: implications for malaria control in Uganda. Malar J 10:372. doi: 10.1186/1475-2875-10-372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chanda P, Castillo-Riquelme M, Masiye F. 2009. Cost-effectiveness analysis of the available strategies for diagnosing malaria in outpatient clinics in Zambia. Cost Eff Resour Alloc 7:5. doi: 10.1186/1478-7547-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ansah EK, Epokor M, Whitty CJM, Yeung S, Hansen KS. 2013. Cost-effectiveness analysis of introducing RDTs for malaria diagnosis as compared to microscopy and presumptive diagnosis in central and peripheral public health facilities in Ghana. Am J Trop Med Hyg 89:724–736. doi: 10.4269/ajtmh.13-0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.De Oliveira MRF, de Castro Gomes A, Toscano CM. 2010. Cost effectiveness of OptiMal rapid diagnostic test for malaria in remote areas of the Amazon Region, Brazil. Malar J 9:277. doi: 10.1186/1475-2875-9-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Loubiere S, Moatti JP. 2010. Economic evaluation of point-of-care diagnostic technologies for infectious diseases. Clin Microbiol Infect 16:1070–1076. doi: 10.1111/j.1469-0691.2010.03280.x. [DOI] [PubMed] [Google Scholar]
- 105.Shillcutt S, Morel C, Goodman C, Coleman P, Bell D, Whitty CJ, Mills A. 2008. Cost-effectiveness of malaria diagnostic methods in sub-Saharan Africa in an era of combination therapy. Bull World Health Organ 86:101–110. doi: 10.2471/BLT.07.042259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Uzochukwu BS, Obikeze EN, Onwujekwe OE, Onoka CA, Griffiths UK. 2009. Cost-effectiveness analysis of rapid diagnostic test, microscopy and syndromic approach in the diagnosis of malaria in Nigeria: implications for scaling-up deployment of ACT. Malar J 8:265. doi: 10.1186/1475-2875-8-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Msellem MI, Mårtensson A, Rotllant G, Bhattarai A, Strömberg J, Kahigwa E, Garcia M, Petzold M, Olumese P, Ali A, Björkman A. 2009. Influence of rapid malaria diagnostic tests on treatment and health outcome in fever patients, Zanzibar—a crossover validation study. PLoS Med 6:e1000070. doi: 10.1371/journal.pmed.1000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zurovac D, Larson BA, Skarbinski J, Slutsker L, Snow RW, Hamel MJ. 2008. Modeling the financial and clinical implications of malaria rapid diagnostic tests in the case-management of older children and adults in Kenya. Am J Trop Med Hyg 78:884–891. [PMC free article] [PubMed] [Google Scholar]
- 109.Rydzak CE, Goldie SJ. 2008. Cost-effectiveness of rapid point-of-care prenatal syphilis screening in sub-Saharan Africa. Sex Transm Dis 35:775–784. doi: 10.1097/OLQ.0b013e318176196d. [DOI] [PubMed] [Google Scholar]
- 110.Owusu-Edusei K, Gift TL, Ballard RC. 2011. Cost-effectiveness of a dual non-treponemal/treponemal syphilis point-of-care test to prevent adverse pregnancy outcomes in sub-Saharan Africa. Sex Transm Dis 38:997–1003. doi: 10.1097/OLQ.0b013e3182260987. [DOI] [PubMed] [Google Scholar]
- 111.Kuznik A, Lamorde M, Nyabigambo A, Manabe YC. 2013. Antenatal syphilis screening using point-of-care testing in sub-Saharan African countries: a cost-effectiveness analysis. PLoS Med 10:e1001545. doi: 10.1371/journal.pmed.1001545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Huang W, Gaydos CA, Barnes MR, Jett-Goheen M, Blake DR. 2013. Comparative effectiveness of a rapid point-of-care test for detection of Chlamydia trachomatis among women in a clinical setting. Sex Transm Infect 89:108–114. doi: 10.1136/sextrans-2011-050355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hislop J, Quayyum Z, Flett G, Boachie C, Fraser C, Mowatt G. 2010. Systematic review of the clinical effectiveness and cost-effectiveness of rapid point-of-care tests for the detection of genital chlamydia infection in women and men. Health Technol Assess 14:1–97. doi: 10.3310/hta14290. [DOI] [PubMed] [Google Scholar]
- 114.Watson-Jones D, Changalucha J, Gumodoka B, Weiss H, Rusizoka M, Ndeki L, Whitehouse A, Balira R, Todd J, Ngeleja D, Ross D, Buvé A, Hayes R, Mabey D. 2002. Syphilis in pregnancy in Tanzania. I. Impact of maternal syphilis on outcome of pregnancy. J Infect Dis 186:940–947. doi: 10.1086/342952. [DOI] [PubMed] [Google Scholar]
- 115.Baden T, Chagas AM, Gage GJ, Marzullo TC, Prieto-Godino LL, Euler T. 2015. Open Labware: 3-D printing your own lab equipment. PLoS Biol 13:e1002086. doi: 10.1371/journal.pbio.1002086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Chin CD, Laksanasopin T, Cheung YK, Steinmiller D, Linder V, Parsa H, Wang J, Moore H, Rouse R, Umviligihozo G, Karita E, Mwambarangwe L, Braunstein SL, van de Wijgert J, Sahabo R, Justman JE, El-Sadr W, Sia SK. 2011. Microfluidics-based diagnostics of infectious diseases in the developing world. Nat Med 17:1015–1019. doi: 10.1038/nm.2408. [DOI] [PubMed] [Google Scholar]
- 117.Laksanasopin T, Guo TW, Nayak S, Sridhara AA, Xie S, Olowookere OO, Cadinu P, Meng F, Chee NH, Kim J, Chin CD, Munyazesa E, Mugwaneza P, Rai AJ, Mugisha V, Castro AR, Steinmiller D, Linder V, Justman JE, Nsanzimana S, Sia SK. 2015. A smartphone dongle for diagnosis of infectious diseases at the point of care. Sci Transl Med 7:273re1. doi: 10.1126/scitranslmed.aaa0056. [DOI] [PubMed] [Google Scholar]
- 118.Huang JM, Henihan G, Macdonald D, Michalowski A, Templeton K, Gibb AP, Schulze H, Bachmann TT. 2015. Rapid electrochemical detection of New Delhi metallo-beta-lactamase genes to enable point-of-care testing of carbapenem-resistant Enterobacteriaceae. Anal Chem 87:7738–7745. doi: 10.1021/acs.analchem.5b01270. [DOI] [PubMed] [Google Scholar]