Abstract
Background
The genus Bartonella is comprised of a rapidly increasing number of pathogenic species that induce a seemingly diverse spectrum of neurological symptoms. During the 12 year period that followed the initial onset of neurological and gastrointestinal symptoms, an 11 year-old girl experienced a spectrum of neurological complaints including frequent headaches, visual and auditory hallucinations, anxiety, vision loss involving the lower left quadrant of both eyes, episodic bouts of generalized paralysis, facial palsy, chronic insomnia, seizures, dizziness, cognitive dysfunction, and memory loss. PCR assays targeting Bartonella spp. were used to test formalin-fixed, paraffin embedded brain tissue, patient blood specimens and Bartonella alpha Proteobacteria growth medium (BAPGM) enrichment blood cultures. PCR positive amplicons were sequenced directly and compared to GenBank sequences. Bartonella spp. serology was performed by indirect fluorescent antibody testing and confocal laser scanning microscopy was used to visualize B. henselae organisms in resected brain.
Results
Bartonella henselae DNA was independently PCR amplified and sequenced from the girl’s right parietal lobe, surgically resected in 2000 and from a blood specimen collected in 2012. Although causation cannot be established by a case report, prior diagnostic testing resulted in findings that were either inconclusive or within normal reference ranges and no etiological diagnosis had been obtained to explain the patient’s initial or progressive neurological symptoms.
Conclusions
As intravascular, intra-erythrocytic and endotheliotropic bacteria, it is possible that B. henselae initially induced a vasculitis, resulting in secondary cerebral infarction, tissue necrosis and surgical resection. Bartonella bacteremia, potentially spanning a 12-year time frame, in conjunction with the therapeutic administration of immunosuppressive drugs may have resulted in a progression and potentiation of the neurological disease that was partially reversible following antibiotic administration.
Keywords: Neurobartonellosis, Bartonella henselae San Antonio 2 vasculitis
Background
As recently reviewed, an increasing number of Bartonella species have been identified as zoonotic pathogens that are transmitted by animal bites or scratches, needle sticks, blood transfusions, or by arthropods [1–4]. Potentially, because Bartonella spp. can infect erythrocytes, endothelial cells, pericytes, and various macrophage-type cells, vascular pathology may be much more diverse than is currently appreciated [5–7]. Due to current limitations associated with diagnostic testing for bartonellosis, a high index of suspicion is required, particularly in patients with occult, persistent bacteremia, small vessel disease, or non-specific symptoms, such as fatigue, insomnia and memory loss [6, 8, 9]. Because of the rapid discovery of new, pathogenic Bartonella spp., the expanding number of arthropods proven or suspected in transmission, the large numbers of infected animal reservoir hosts in nature, and the broad spectrum of neurological abnormalities reported in recent years, neurobartonellosis may be a much more prevalent disease in both immunocompetent and immunocompromised patients throughout the world than is currently recognized [6].
Case report
In March 2000, an 11-year-old girl residing in Ottawa, Canada developed sudden-onset, headaches, difficulty walking, left sided paresis and an ataxic gait. The family resided in a rural environment and their home backed onto an extensive ravine. Shortly before the onset of neurological symptoms, a feral dog was adopted from the local humane society. Historically, the owner did not observe fleas or ticks and the dog did not bite the child. However, shortly after adoption, the dog developed a large abscess with purulent discharge in the neck region, which the child cleaned daily. A few weeks later, the girl developed flu-like symptoms followed by progressive neurological abnormalities. Concurrently, she reported gastrointestinal symptoms, including abdominal pain, bloating and constipation, which persisted throughout the patient’s subsequent illness. A Magnetic resonance imaging (MRI) scan identified a large, focal, demyelinating mass lesion located in the right parietal lobe. Based upon the MRI and examination of frozen brain tissue sections obtained at surgery, the mass was presumptively diagnosed by a neuropathologist as a glioblastoma. The mass and a portion of the right parietal lobe were surgically resected. Based upon formalin-fixed paraffin embedded (FFPE) tissue histopathology, the diagnosis was revised to a reactive inflammatory process consistent with vasculitis, secondary cerebral infarction, and tissue necrosis. The histopathological examination revealed abrupt demarcations between necrotic areas, with accompanying destruction of axons and myelin. Adjacent brain tissue contained wide-spread perivascular lymphoplasmacytic infiltration with extension into the vessel wall, resulting in intimal proliferation and sparse hemosiderin deposition in both venules and small arteries. There was no evidence of selective perivascular demyelination. The majority of the perivascular lymphocytes were T cells, with a few scattered B cells. Mindbomb E3 ubiquitin protein ligase 1(MIB1) staining was minimal, except among lymphocytes, and the tissue was immunonegative for Epstein-Barr virus (EBV). During the next 3 years, the patient was intermittently treated for a presumptive autoimmune neurological disease with high dose intravenous corticosteroids. Her diagnoses included idiopathic vasculitis, Guillain-Barre syndrome, multiple sclerosis, and acute disseminated encephalomyelitis (ADEM).
In 2003, the patient experienced frequent headaches, chest pain, visual and auditory hallucinations, anxiety, ocular floaters, severe depression, and fatigue. Additional episodes of partial paralysis occurred in 2004 and 2009. A few weeks prior to each of the three episodes, the patient experienced a non-febrile respiratory illness. In July 2004, after returning home from a sailing camp, the girl developed neurocognitive abnormalities, after which there was rapid deterioration in muscle strength with left sided paralysis, homonymous hemianopia, seizures, dysphagia, laryngitis, and severe confusion. After initiation of intravenous immunoglobulin (IVIG) the patient slowly recovered; however, it was several months before she became ambulatory, and her gait never normalized. During this time, the patient reportedly developed severe allergic reactions when ingesting gluten, corn, lactose or pork.
In March 2009, the patient again developed progressive paresis that was treated with low dose IVIG for 3 days. Despite initial improvement in neurological status, she developed generalized seizures and status epilepticus a few days later, requiring plasma exchange and pharmacological-induction of a coma, lasting for 10 days. After awakening from the coma, the patient exhibited tetraplegia, dysphasia, and marked facial palsy. During hospitalization, treatment consisted of IVIG and fluconazole (Diflucan) for oral Candidiasis. Serum IgA, IgM and IgG levels were consistently low, and based upon repeated testing had never normalized. Due to her unusual clinical presentation and disease progression, a diagnosis of tumefactive multiple sclerosis was rendered at this time. Shortly following this hospitalization, the family physician suspected Lyme disease, with equivocal Western immunoblot results (IgM positive, IgG negative), the patient was treated with penicillin. Combination therapy with fluconazole, penicillin and IVIG appeared to facilitate rapid improvement in neurological status, including improved ambulation, decreased headaches, and improved cognitive function.
Overall, there was a cumulative deterioration in neurological status following each of the three distinct paralysis episodes (2000, 2004, 2009); however, there was no observable disease progression between these episodes. After 2009, the patient’s neurological disabilities resulted in limited daily activities and required physical support and full-time care. In October of 2011, based upon the patient’s historical symptoms, a physician in Vancouver clinically suspected co-infections consisting of Lyme disease, babesiosis and neurobartonellosis. Because of a history of night sweats (starting in 2000), the patient was treated with atovaquone (Mepron) 1 tsp. twice daily, azithromycin (Zithromax) 500 mg, intravenously once daily and ceftriaxone (Rocephin®) 2 g intravenously 5 days each week for 8 weeks. After initiation of this treatment regimen, the patient experienced dramatic improvement, including partial resolution of facial palsy within 2 weeks, resolution of severe jaw and chest pain, cessation of night sweats, clearer thinking and speech, and a decrease in the frequency of floaters; all historical problems reported since illness onset. On February 14, 2012, the mother contacted the corresponding author by email and requested that her daughter be entered into an Institutional Review Board (North Carolina State University, College of Veterinary Medicine, IRB #164-08-05, NCSU-CVM IRB) approved research study.
Methods
Serology
For this study, all serum samples were tested by indirect fluorescent antibody (IFA) assays using a panel of Bartonella antigens. Briefly, antibody responses to Bartonella henselae strain Houston I, B. henselae strain San Antonio 2 (SA2 strain type), B. vinsonii subspecies berkhoffii genotype I, B. vinsonii subspecies berkhoffii genotype II, B. vinsonii subspecies berkhoffii genotype III, and B. koehlerae were tested by IFA as previously described [4–6]. Seropositive samples were defined as having endpoint titers ≥1:64 using a twofold dilution scale of 1:16 – 1:8192.
Molecular testing
Bartonella testing was performed using the Bartonella alpha proteobacteria growth medium (BAPGM) platform, as previously described [4–8]. The primer sequences targeting Bartonella genus specific 16-23S intergenic transcribed spacer (ITS) and B. koehlerae species specific 16-23S ITS were used [4–8]. BAPGM cultures were processed in a biosafety cabinet with HEPA filtration in a limited access Biosafety Level II laboratory. To assess for potential contamination during blood sample processing into BAPGM, an un-inoculated BAPGM culture flask was processed simultaneously and in an identical manner with each batch of patient blood and serum samples tested.
DNA extraction from formalin fixed paraffin-embedded (FFPE) brain tissues were tested by PCR for the presence of Bartonella spp. DNA. Multiple 30μm sections of FFPE brain tissue was excised using a microtome. Previously, we described Bartonella spp. DNA carryover, during animal necropsy and during the subsequent processing of tissue samples [10]. Hence, special precautions were taken in our laboratory when sampling paraffin blocks to minimize the DNA cross contamination. A negative control paraffin block, containing no tissue, was cut in between each tissue block and processed in an identical manner as samples to determine if any DNA carryover was occurring through the use of the microtome. Tissues were processed in small batches and the work surface was thoroughly cleaned using ethanol and DNAse between each tissue block tested, to avoid Bartonella spp. DNA carry over between the samples. DNA was extracted using QIAamp FFPE Tissue Kit (Qiagen, Valencia, CA) following manufacturer’s instructions. Elution buffer was used as a reagent control with each set of DNA extractions. DNA concentrations and purity were determined using a spectrophotometer (Nanodrop, Wilmington, DE). Extracted DNA was stored at -20 °C.
Laser confocal immunohistochemistry
To visualize B. henselae, brain tissue sections were processed using immunostaining as described previously [11]. Briefly, 20μm paraffin-embedded brain tissue sections were incubated with monoclonal Bartonella henselae antibody (Abcam Cambridge, MA) at 1:100 dilution followed by donkey anti-mouse IgG conjugated to Alexa Fluor 594 (Jackson ImmunoResearch West Grove, PA) at 1:400 dilution. Secondary antibody control includes buffer and donkey anti-mouse IgG conjugated to Alexa Fluor 594 (1:400 dilution) only.
Results and discussion
By IFA testing using previously described antigens and techniques, the patient was not seroreactive to B. henselae (Houston 1 strain type), B. henselae (SA2 strain type), B.vinsonii subsp. berkhoffii genotypes I, II and III and B. koehlerae. Using a triple draw approach [12] and previously described PCR assays targeting Bartonella genus specific 16-23S ITS and B. koehlerae species specific 16-23S ITS elements, B. henselae (376/380 base pairs, 99 %) DNA was amplified and sequenced from one of three of the patient’s blood specimens. At the time of sample collection, the patient was being treated with azithromycin and ceftriaxone. BAPGM enrichment blood cultures were PCR negative following 7 and 14 day incubation periods and no subculture isolate was obtained. Subsequently, B. henselae (448/448 base pairs, 100 %) was amplified from the surgically obtained, April 2000 FFPE brain tissue. Intracellular localization of B. henselae in surgically resected FFPE brain tissue was visualized by confocal laser scanning microscopy (Fig. 1).
Fig. 1.
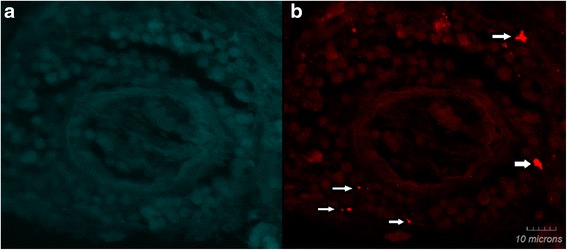
Bartonella henselae immunoreactivity detected in brain tissue biopsy using laser scanning confocal microscopy. Panel a shows no immunoreactivity (secondary antibody control). Panel b (arrows) shows immunoreactive B. henselae. Stained samples were imaged using laser scanning confocal microscopy. Z-stack projections for both images are in-focus projections of 17 0.43μm optical sections for a total thickness of 7 μm. (Olympus PlanApo 63×/1.40 oil objective)
When BAPGM enrichment PCR testing was performed in March, 2012, the girl was still experiencing severe cognitive problems, essential tremors and had musculoskeletal pain and weakness. Based on amplification of B. henselae from blood and brain tissue, her family physician initiated antibiotic treatment with intravenous ceftriaxone (2g intravenously daily), metronidazole (Flagyl, 250 mg twice daily), and azithromycin (500 mg daily) for 9 weeks. During the first 2 weeks of therapy, the patient experienced worsening symptoms, including cognitive decline, seizures, generalized muscle and joint pain, after which there was gradual improvement in overall cognitive function. By August 2012, muscle tone, visual stress and memory had improved dramatically. By October 2012, the patient’s mother reported continued improvement in neurological status. Subsequently, the patient developed a flu-like illness; however, unlike the three previous respiratory episodes and for the first time in 12 years she developed a fever (104 °F), and did not subsequently develop paralysis.
In October 2012, the patient was retested in conjunction with the NCSU-CVM IRB study. Prior to sample collection, the patient was not receiving antibiotics. Based upon repeated IFA testing, she was not seroreactive against B. henselae (Houston 1 strain type) B. henselae (SA2 strain type), B. vinsonii subsp. berkhoffii genotypes I, II and III and B. koehlerae antigens. Using the triple draw approach (3 samples sets pulled every other day) [12], B. henselae DNA was not amplified from blood, serum, and post-enrichment 7 and 14 day BAPGM enrichment blood cultures. No subculture isolates were obtained. Due to the chronicity and complexity of the patient’s illness and because based upon prior instances of rapid neurological deterioration, she refused additional treatment with immunosuppressive drugs. On follow up, facial palsy has resolved, neurocognitive function and physical movement have marginally improved, and her thought processes, (i.e. memory and ability to plan and follow complex operations) have remained stable. MRIs performed in 2015 and 2016 showed frontal lobe disintegration without evidence of progressive pathology in other portions of the brain.
Since 2000, when this patient was initially examined, there has been a substantial increase in the body of clinical literature describing a spectrum of symptoms in patients infected with B. henselae. Despite progress, Bartonella species in general, and B. henselae in particular, remain incompletely understood in the context of cellular and vascular tropism, neuropathogenesis, and the role that persistent intravascular infection plays in disease expression [6]. During the 12 year period following the initial onset of neurological and gastrointestinal symptoms, this patient experienced a wide spectrum of neurological abnormalities including frequent headaches, visual and auditory hallucinations, anxiety, vision loss involving the lower left quadrant of both eyes, episodic bouts of generalized paralysis, facial palsy, chronic insomnia, seizures, dizziness, cognitive dysfunction, and memory loss. During this time frame, differential neurological diagnoses included gliobastoma (initial mass lesion), vasculitis of undetermined etiology, Guillain-Barre syndrome, acute disseminated encephalomyelitis (ADEM), and multiple sclerosis. Based upon retrospective testing of the parietal lobe mass lesion that was surgically resected in 2000, a diagnosis of neurobartonellosis seems justified in this patient. Based upon DNA sequence comparison, B. henselae was successfully PCR amplified from the FFPE brain tissue and from a blood specimen obtained in 2012. Using a previously described technique [11], B. henselae organisms could be visualized in FFPE surgical brain tissue by laser scanning confocal microscopy. Additional indirect support for a diagnosis of neurobartonellosis was provided by the historical deterioration in neurological status that followed administration of immune suppressive drugs, as compared to gradual improvement in neurological status after the initiation of antimicrobial therapy.
The extent to which repeated, corticosteroid-induced suppression of immune function contributed to additional or progressive neurological damage is unknown. However, there are case reports in which patients treated with immunosuppressive drugs based upon a “positive” autoimmune disease test result subsequently developed B. henselae endocarditis [13, 14]. There are also recent case reports that describe the medical complexities associated with differentiating occult, intravascular infection with a Bartonella sp. from autoimmune diseases [15]. The extent to which repeated administration of IVIG prevents or enhances disease progression in patients with occult infection also deserves critical consideration. IVIG administration to a child with Guillain-Barre syndrome did not halt the progressive paralysis prior to an apparent reversal in the disease process after initiation of antibiotic therapy [16].
It is also unclear whether persistent intravascular, microglial, or cerebrospinal fluid (CSF) infection contributed to the various neurological symptoms or to the three paresis/paralysis episodes experienced by this patient between 2000 and 2009. Based upon in vitro and in vivo evidence, B. henselae is an intraerythrocytic and endotheliotropic bacteria [17]. However, no studies have addressed the potential localization of the bacterium within the vasculature versus brain parenchymal tissues or CSF of human patients. Unfortunately, despite substantial efforts on the part of several research groups, a pathologically relevant rodent model for bartonellosis or neurobartonellosis has not been established. Thus, prospective patient studies are needed to document intravascular and/or CSF infection with B. henselae, in conjunction with direct therapies to eliminate the infection and determine subsequent patient outcomes.
Combined utilization of molecular-based diagnostic testing, in conjunction with conventional microbiological approaches, are increasingly used in the clinical setting for the detection of fastidious and non-fastidious pathogens. While the location of Bartonella during the nonbacteremic phase of infection is currently unknown, endothelial cells and bone marrow have been hypothesized as primary niches in both incidental and reservoir hosts [18, 19]. Negative BAPGM enrichment blood culture is often attributed to history of antibiotic treatment before sampling as reported in this patient. A cross-sectional study by Maggi et al. [20] found that 75 % of Bartonella-infected humans did not have IFA antibodies to the infecting Bartonella species or genotype. Although unproven, chronic intravascular infection with Bartonella spp. may induce a degree of immunological anergy, resulting in an undetectable level of organism-specific antibodies in naturally-infected human patients or other mechanisms may contribute to seronegativity.
The source of B. henselae infection was not established for this patient. Although cats are most often implicated in the transmission of B. henselae to humans (Cat Scratch Disease), dogs have been infrequently reported as a source of infection. Shortly before the onset of a flu-like illness, this child did participate in cleaning purulent material from an abscess in the dog’s neck region, which could have potentially contained viable bacteria. Bartonella henselae can be isolated from the lymph nodes of dogs and humans with granulomatous lymphadenitis [21] Recently, French investigators implicated B. henselae and three Bartonella spp. not previously isolated from humans, as a cause of undifferentiated chronic illness, potentially transmitted by ticks [22]. The numerous modes of transmission in conjunction with the increasingly large number of animals in which B. henselae bacteremia has been confirmed supports a more overarching disease designation (bartonellosis), rather than the historical designation of B. henselae-induced Cat Scratch Disease.
Conclusion
If B. henselae contributed to the onset and progression of this patient’s illness, a delay in diagnosis and administration of immunosuppressive drugs may have resulted in a progression and potentiation of the neurological disease, which might have been more effectively managed pre-surgically by directed antimicrobial therapy. In a 2004 Nature publication by Merrell & Falkow [23], Helicobacter pylori and B. henselae were used to exemplify the role of “stealth pathogens” in chronic disease causation. Stealth pathogens are characterized by slow bacterial replication time (approximately 22h for B. henselae), a long incubation period (potentially months to years), induction of chronic symptomatology, a non-sterilizing immune response, indirect modes of transmission (all Bartonella spp. are known or thought to be transmitted by one or more arthropod vector), and a persistently infected “carrier state”. Based upon evolving evidence, B. henselae appears to fulfill all criteria for a stealth, intravascular, and endotheliotropic pathogen that can induce a chronic neurological symptoms.
Consent
Written informed consent was obtained from the patient for publication of this report and the accompanying images.
Acknowledgements
The authors would like to thank Julie Bradley for technical assistance and Barbara Hegarty for careful review of the manuscript. This case study was supported in part by the State of North Carolina and donations to the Vector Borne Disease Research Fund, North Carolina State University Veterinary Medical Foundation. Publication of this manuscript was sponsored by Bayer Animal Health in the framework of the 11th CVBD World Forum Symposium
Footnotes
Competing interests
In conjunction with Dr. Sushama Sontakke and North Carolina State University, Dr. Breitschwerdt holds U.S. Patent No. 7,115,385; Media and Methods for cultivation of microorganisms, which was issued October 3, 2006. He is the chief scientific officer for Galaxy Diagnostics, a company that provides advanced diagnostic testing for the detection of Bartonella species infection in animals.
Authors’ contributions
NB and RM performed the BAPGM enrichment blood culture, PCR testing of the patient’s blood and tissue specimens, DNA sequencing and alignments, and helped generate the first draft of the manuscript. ME performed the confocal immunohistochemistry. EBB coordinated various aspects of the investigation and drafted the final manuscript. All authors read and approved the manuscript.
References
- 1.Chomel BB, Boulouis HJ, Breitschwerdt EB, Kasten RW, Vayssier-Taussat M, Birtles RJ, et al. Ecological fitness and strategies of adaptation of Bartonella species to their hosts and vectors. Vet Res. 2009;40(2):29. doi: 10.1051/vetres/2009011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pulliainen AT, Dehio C. Persistence of Bartonella spp. stealth pathogens: from subclinical infections to vasoproliferative tumor formation. FEMS Microbiol Rev. 2012;36(3):563–99. doi: 10.1111/j.1574-6976.2012.00324.x. [DOI] [PubMed] [Google Scholar]
- 3.Ben-Tekaya H, Gorvel J-P, Dehio C. Bartonella and Brucella- weapons and strategies for stealth attack. Cold Spring Harb Perspect Med. 2013;3(8):1–20. doi: 10.1101/cshperspect.a010231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Breitschwerdt EB. Bartonellosis: one health perspectives for an emerging infectious disease. ILAR J. 2014;55:46–58. doi: 10.1093/ilar/ilu015. [DOI] [PubMed] [Google Scholar]
- 5.Breitschwerdt EB, Linder KL, Day MJ, Maggi RG, Chomel BB, Kempf VAJ. Koch’s postulates and the pathogenesis of comparative infectious disease causation associated with Bartonella species. J Comp Pathol. 2013;148(2–3):115–25. doi: 10.1016/j.jcpa.2012.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Breitschwerdt EB, Sontakke S, Hopkins S. Neurological manifestations of Bartonellosis in immunocompetent patients: a composite of reports from 2005–2012. Journal of Neuroparasitology. 2012;3:1–15. doi: 10.4303/jnp/235640. [DOI] [Google Scholar]
- 7.Breitschwerdt EB, Kordick DL. Bartonella species and vascular pathology (Chapter 6) In: Gavins FNE, Stokes KY, editors. Vascular response to pathogens. New York: Academic Press; 2016. [Google Scholar]
- 8.Breitschwerdt EB, Maggi RG, Nicholson WL, Cherry NA, Woods CW. Bartonella sp. bacteremia in patients with neurological and neurocognitive dysfunction. J Clin Microbiol. 2008;46(9):2856–61. doi: 10.1128/JCM.00832-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maggi RG, Mozayeni BR, Pultorak EL, Hegarty BC, Bradley JM, Correa M, et al. Bartonella spp. bacteremia and rheumatic symptoms in patients from Lyme disease-endemic region. Emerg Infect Dis. 2012;18(11):783–91. doi: 10.3201/eid1811.121226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Varanat M, Maggi RG, Linder KE, Horton S, Breitschwerdt EB. Cross-contamination in the molecular detection of Bartonella from paraffin-embedded tissues. Vet Pathol. 2009;46(5):940–4. doi: 10.1354/vp.08-VP-0259-B-BC. [DOI] [PubMed] [Google Scholar]
- 11.Maggi RG, Ericson M, Mascarelli PE, Bradley JM, Breitschwerdt EB. Bartonella henselae bacteremia in a mother and son potentially associated with tick exposure. Parasit Vectors. 2013;15(6):101. doi: 10.1186/1756-3305-6-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pultorak EL, Maggi RG, Mascarelli PE, Breitschwerdt EB. Serial testing from a 3-day collection period by use of the Bartonella Alphaproteobacteria growth medium platform may enhance the sensitivity of Bartonella species detection in bacteremic human patients. J Clin Microbiol. 2013;51(6):1673–7. doi: 10.1128/JCM.00123-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Turner JW, Pien BC, Ardoin SA, Anderson AM, Shieh WJ, Zaki SR, et al. A man with chest pain and glomerulonephritis. Lancet. 2005;365(9476):2062. doi: 10.1016/S0140-6736(05)66701-3. [DOI] [PubMed] [Google Scholar]
- 14.Vikram HR, Bacani AK, DeValeria PA, Cunningham SA, Cockerill FR., 3rd Bivalvular Bartonella henselae prosthetic valve endocarditis. J Clin Microbiol. 2007;45(12):4081–4. doi: 10.1128/JCM.01095-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maritsi DN, Zarganis D, Metaxa Z, Papaioannou G, Vartzelis G. Bartonella henselae infection: an uncommon mimicker of autoimmune disease. Case Rep Pediatr. 2013;1–4. [DOI] [PMC free article] [PubMed]
- 16.Mascarelli PE, Maggi RG, Hopkins S, Mozayeni BR, Trull CL, Bradley JM, et al. Bartonella henselae infection in a family experiencing neurological and neurocognitive abnormalities after woodlouse hunter spider bites. Parasit Vectors. 2013;15:98. doi: 10.1186/1756-3305-6-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harms A, Dehio C. Intruders below the radar: molecular pathogenesis of Bartonella spp. Clin Microbiol Rev. 2012;25(1):42–78. doi: 10.1128/CMR.05009-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mändle T, Einsele H, Schaller M, Neumann D, Vogel W, Autenrieth IB, et al. Infection of human CD34+ progenitor cells with Bartonella henselae results in intraerythrocytic presence of B. henselae. Blood. 2005;106(4):1215–22. doi: 10.1182/blood-2004-12-4670. [DOI] [PubMed] [Google Scholar]
- 19.Balakrishnan N, Cherry NA, Linder KE, Pierce E, Sontakke N, Hegarty BC, et al. Experimental infection of dogs with Bartonella henselae and Bartonella vinsonii subsp. berkhoffii. Vet Immunol Immunopathol. 2013;156(1–2):153–8. doi: 10.1016/j.vetimm.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 20.Maggi RG, Mascarelli PE, Pultorak EL, Hegarty BC, Bradley JM, Mozayeni BR, et al. Bartonella spp. bacteremia in high-risk immunocompetent patients. Diagn Microbiol Infect Dis. 2011;71(4):430–7. doi: 10.1016/j.diagmicrobio.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 21.Duncan AW, Marr HS, Birkenheuer AJ, Maggi RG, Williams LE, Correa MT, et al. Bartonella DNA in the blood and lymph nodes of Golden Retrievers with lymphoma and in healthy controls. J Vet Intern Med. 2008;22(1):89–95. doi: 10.1111/j.1939-1676.2007.0018.x. [DOI] [PubMed] [Google Scholar]
- 22.Vayssier-Taussat M, Moutailler S, Féménia F, Raymond P, Croce O, La Scola B, et al. Identification of novel zoonotic activity of Bartonella spp., France. Emerg Infect Dis. 2016;22(3):457–62. doi: 10.3201/eid2203.150269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Merrell DS, Falkow S. Frontal and stealth attack strategies in microbial pathogenesis. Nature. 2004;430(6996):250–6. doi: 10.1038/nature02760. [DOI] [PubMed] [Google Scholar]


